Abstract
Objective: To explore the effect of traditional Chinese medicine (TCM) nursing on postoperative patients with gastric cancer and its impact on quality of life. Methods: According to the random number table method, 103 patients with gastric cancer were divided into observation group (n=52, TCM nursing) and control group (n=51, routine nursing). The postoperative recovery of gastrointestinal function, the scores of mental states, inflammatory index, self-esteem scale (SES) and quality of life score (generic quality of life inventory-74 scale, GQOLI-74 scale) before and after intervention were compared between the two groups, and the adverse reactions were recorded. Results: Compared with the control group, the first postoperative exhaust time, the regression time of epigastric distension symptoms, the first defecation time and the time of returning to normal eating in the observation group were shorter than those in the control group (all P<0.05). After intervention, the scores of Hamilton Anxiety Scale (HAMA), Hamilton Depression Scale (HAMD) and the levels of serum TNF-α, CRP and IL-1β in the two groups were lower than those before intervention, and those in the observation group were lower than those in the control group (all P<0.05). After intervention, the scores of SES and GQOLI-74 in both groups were higher than those before intervention, and those in the observation group were higher than those in the control group (all P<0.05). During hospitalization, the total incidence of adverse reactions in the observation group was lower than that in the control group (P<0.05). Conclusion: Perioperative TCM nursing for patients with gastric cancer can more obviously improve postoperative gastrointestinal dysfunction, alleviate acute inflammation, improve postoperative unhealthy mental state, reduce the occurrence of postoperative complications, and finally improve the quality of life of postoperative patients, which is worthy of clinical application.
Keywords: Traditional Chinese medicine nursing, gastric cancer, mental state, inflammatory state, quality of life
Introduction
Gastric cancer is a malignant tumor with high incidence, and the 5-year survival rate is very low. For example, the 5-year survival rate of patients with stage III gastric cancer is about 30%, and that of the patients with stage IV is less than 10% [1]. At present, surgical resection is still the main treatment for non-metastatic gastric cancer. However, due to the influence of cancer, gastrointestinal function of patients with gastric cancer is mostly in a state of disorder, and surgery can cause body stress and even induce acute inflammation reaction, which is not conducive to the recovery of postoperative patients [2]. Therefore, postoperative high-quality nursing is particularly important in promoting the recovery of the postoperative patients. TCM nursing is a series of intervention measures implemented on the basis of TCM syndrome differentiation nursing theory, which is based on the principles of “treating the same disease with different nursing”, “treating the different disease with same nursing”, “treating both principal and secondary aspects of a disease promptly or slowly” and “determine the treatment based on differentiation of symptoms and signs”, combined with patients’ specific TCM symptoms [3]. At present, TCM nursing is mostly used in clinic care, such as after malignant tumor resection and percutaneous coronary intervention (PCI). Such studies have shown that TCM nursing can reduce the risk of recurrence of patients with malignant tumor resection, reduce the incidence of complications after PCI [4,5]. However, less attention was paid to patients’ psychology and postoperative body function, such as gastrointestinal function and sleep quality after operation of gastric cancer. Therefore, this study mainly evaluated the effect of TCM nursing on the recovery and quality of life of postoperative patients with gastric cancer from the aspects of postoperative inflammatory state, mental state and postoperative recovery of gastrointestinal function.
Materials and methods
The baseline data
For this prospective study, 103 postoperative patients with gastric cancer hospitalized and treated in our hospital from February 2019 to February 2020 were randomly divided into control group (n=51, routine nursing was given during the perioperative period) and observation group (n=52, TCM nursing was given on the basis of the control group). Inclusion criteria: (1) The patients were 45 to 70 years old. (2) Patients were confirmed by preoperative pathological examination as primary gastric cancer. (3) Patients who met the diagnostic criteria of “epigastric pain” in TCM [6]. (4) Patients undergoing elective radical gastrectomy after comprehensive evaluation of various indicators. (5) Patients who signed informed consent. Exclusion criteria: (1) Perioperative patients with acute and chronic infection. (2) Patients with the diseases of immune system and blood system, or blood coagulation disorders. (3) Patients with malignant tumors. (4) Patients who participated in other research projects at the same time, and so on. This study was reviewed and approved by the medical ethics committee of our hospital.
Methods
The control group was given routine nursing during the perioperative period, such as preoperative improvement of various examinations, active treatment of primary disease, active prevention of postoperative complications, daily nursing of drainage tube and catheter and other symptomatic treatment measures until the patient was discharged from hospital.
On this basis, the observation group was given TCM nursing until the patients were discharged: (1) TCM psychological care: The nursing staff communicated with patients face to face before operation, caring and comforting the patients with kind attitude and language, and telling the patients to use the methods of self-cultivation and emotional victory to eliminate the unhealthy mentality of tension and anxiety, and to welcome the operation with the best mentality [7]. After the operation, it was also necessary to communicate with the patients in time to comfort them. The targeted psychological counseling was given to patients in time for there were large mood fluctuations in them. The control measures of the self-cultivation method, emotional victory method and so on were explained to patients once again. (2) Syndrome differentiation nursing: As radiotherapy and chemotherapy were often needed for gastric cancer after operation, the immune function of the patients was decreased, and most of them were with deficiency [8]. Therefore, it is necessary to follow the principle of “treat the acute by incidental and treat the chronic by fundamentals”, and the measures of “treating the same disease with different nursing” were carried out according to the individual, time and local conditions. (3) Dietetic nursing: After the operation, patients were advised to eat more liquid and digestible food, with many meals but little food at each time. Food was chosen according to the principle of syndrome differentiation of TCM to achieve the coordination of cold and heat and the combination of five flavors. According to their postoperative recovery, a semi-liquid diet was transited, and a low-fat diet with high protein and vitamins was given. (4) Nursing of auricular-plaster therapy of TCM: The auricular points of spleen, stomach, sympathy, endocrine, large and small intestines were selected [9]. The auricular points such as spleen, stomach, sympathy, endocrine, large and small intestines were selected. After disinfection, the appropriate size adhesive plaster was selected with the cowherb seeds pressing on it. Then, the adhesive plaster with the cowherb seeds was placed on to the auricular points, and they were pressed with thumb and index finger for 2 to 3 min/times, 3 times a day.
Outcomes measurement
The main outcomes: (1) The recovery of gastrointestinal function was compared between the two groups, and the first postoperative exhaust time, the regression time of epigastric distension, the first defecation time and the recovery time of normal eating were recorded. (2) Hamilton anxiety and depression scales (HAMA and HAMD) were used to evaluate anxiety and depression before and after intervention. The higher the score, the more serious the degree of anxiety and depression [10,11].
The secondary outcomes: (1) About 3 mL of venous blood was collected from patients before and after intervention. After centrifugation, serum was separated, and the levels of tumor necrosis factor-α (TNF-α), C-reactive protein (CRP) and interleukin-1β (IL-1β) were detected by ELISA. (2) The SES scale was used to evaluate the patients’ self-esteem before and after the intervention [12]. The total score was 10-40, and the higher the score, the stronger the patients’ self-esteem. (3) GQOLI-74 scale was used to evaluate the quality of life before and after the intervention [13]. The total score was 76-380, and the higher the score, the better the quality of life. (4) The adverse reactions in patients between the two groups during hospitalization, such as dyspepsia, diarrhea, biliary vomiting, dysphagia, etc., the total incidence of adverse reactions = the number of adverse reactions/the total number of cases × 100% was calculated.
Statistical analysis
SPSS 20.0 was used to analyze the data. The enumeration data were expressed in n (%) and compared with the χ2 test. The measurement data were expressed in x̅ ± sd. Paired t test was used for comparison before and after intervention in the same group, and independent t test was used for comparison between the two groups. P<0.05 was considered that the difference was statistically significant.
Results
Comparison of the baseline data
There was no statistical difference in the baseline data between the two groups (all P>0.05), and they were comparable. The details were shown in Table 1.
Table 1.
Baseline data of the two groups of patients (n, x̅ ± sd)
| Indexes | Observation group (n=52) | Control group (n=51) | χ2/t | P |
|---|---|---|---|---|
| Gender (n) | 0.474 | 0.491 | ||
| Male | 28 | 24 | ||
| Female | 24 | 27 | ||
| Age (years) | 54.4±5.5 | 55.1±6.3 | 0.600 | 0.550 |
| Course of disease (years) | 2.18±1.02 | 2.23±1.10 | 0.239 | 0.812 |
| Tumor location (n) | 1.292 | 0.731 | ||
| Fundus of stomach | 16 | 18 | ||
| Cardia | 17 | 13 | ||
| Body of stomach | 10 | 8 | ||
| Gastric antrum | 9 | 12 | ||
| TNM staging (n) | 1.238 | 0.538 | ||
| Stage I | 20 | 17 | ||
| Stage II | 15 | 20 | ||
| Stage III | 17 | 14 | ||
| Postoperative pathology type (n) | 0.772 | 0.680 | ||
| Adenocarcinoma | 40 | 42 | ||
| Squamous cell carcinoma | 8 | 7 | ||
| Adeno-squamous carcinoma | 4 | 2 |
Recovery of gastrointestinal function after operation
Compared with the control group, the first postoperative exhaust time, the regression time of epigastric distension, the first defecation time and the time of returning to normal eating in the observation group were shorter than those in the control group (all P<0.05). The details were shown in Table 2.
Table 2.
Recovery of gastrointestinal function after operation in the two groups (x̅ ± sd)
| Groups | Observation group (n=52) | Control group (n=51) |
|---|---|---|
| The first exhaust time after operation (h) | 40.03±4.40# | 49.10±5.86 |
| The regression time of epigastric distension (d) | 7.44±2.22# | 10.09±2.03 |
| The first defecation time (h) | 60.09±6.66# | 68.85±6.49 |
| The time of returning to normal eating (d) | 8.88±2.03# | 11.84±2.36 |
Note: Compared with the control group;
P<0.05.
Mental state
After intervention, the scores of HAMA and HAMD in the two groups were lower than those before intervention, and those in the observation group were lower than those in the control group (all P<0.05). The details were shown in Table 3.
Table 3.
HAMA and HAMD scores of the two groups before and after intervention (x̅ ± sd, scores)
| Groups | HAMA score | HAMD score |
|---|---|---|
| Observation group (n=52) | ||
| Before intervention | 7.69±1.29 | 7.94±1.29 |
| After intervention | 5.90±1.23*,# | 6.08±1.07*,# |
| Control group (n=51) | ||
| Before intervention | 7.84±1.04 | 8.03±1.22 |
| After intervention | 6.80±1.11* | 7.02±1.05* |
Note: Compared with before intervention;
P<0.05.
Compared with the control group;
P<0.05.
HAMA: Hamilton Anxiety Scale; HAMD: Hamilton Depression Scale.
Levels of inflammatory factors
After intervention, the levels of serum TNF-α, CRP and IL-1β in the two groups were lower than those before intervention, and those in the observation group were lower than those in the control group (all P<0.05). The details were shown in Table 4.
Table 4.
The levels of inflammatory factors in the two groups before and after intervention (x̅ ± sd, scores)
| Groups | TNF-α (ng/mL) | CRP (mg/L) | IL-1β (pg/mL) |
|---|---|---|---|
| Observation group (n=52) | |||
| Before intervention | 29.97±5.40 | 87.59±10.03 | 98.27±10.02 |
| After intervention | 10.03±2.38*,# | 36.46±7.77*,# | 57.79±9.92*,# |
| Control group (n=51) | |||
| Before intervention | 29.65±4.99 | 88.20±12.27 | 97.70±12.28 |
| After intervention | 16.68±3.95* | 52.89±8.07* | 67.88±9.84* |
Note: Compared with before intervention;
P<0.05.
Compared with the control group;
P<0.05.
TNF-α: tumor necrosis factor-α; CRP: C-reactive protein; IL-1β: interleukin-1β.
The scores of SES and GQOLI-74
After intervention, the scores of SES and GQOLI-74 in the two groups were higher than those before intervention, and those in the observation group were higher than those in the control group (all P<0.05). The details were shown in Table 5.
Table 5.
SES and GQOLI-74 scores of the two groups before and after intervention (x̅ ± sd, scores)
| Groups | SES score | GQOLI-74 score |
|---|---|---|
| Observation group (n=52) | ||
| Before intervention | 25.50±3.33 | 264.49±20.20 |
| After intervention | 34.98±3.08*,# | 306.38±23.39*,# |
| Control group (n=51) | ||
| Before intervention | 24.78±3.89 | 262.88±18.94 |
| After intervention | 30.09±4.22* | 284.44±19.27* |
Note: Compared with before intervention;
P<0.05.
Compared with the control group;
P<0.05.
SES: self-esteem scale; GQOLI-74: generic quality of life inventory-74.
Adverse reactions
The total incidence of adverse reactions during hospitalization was 5.77% in the observation group (1 case of dyspepsia and 2 cases of dysphagia) and 19.61% in the control group (2 cases of dyspepsia, 3 cases of diarrhea, 1 case of biliary vomiting and 4 cases of dysphagia). During hospitalization, the total incidence of adverse reactions in the observation group was lower than that in the control group (P<0.05). The details were shown in Figure 1.
Figure 1.
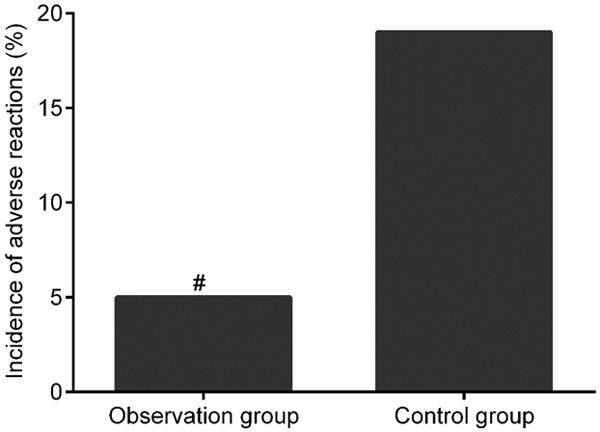
The incidence of adverse reactions in the two groups. Compared with the control group, #P<0.05.
Discussion
The postoperative recovery of gastric cancer is a chronic process. Patients are affected by many factors, such as disease, postoperative prognosis and economic pressure. And they are easy to have bad psychology such as anxiety, fear, and even depression [14]. Long-term anxiety and fear can lead to impede circulation of qi and blood, which is not conducive to the prognosis [15]. Studies of Zemla et al. have shown that timely and effective psychological counseling is very important for patients with poor perioperative mental state [16]. The results of this study showed that the scores of HAMA and HAMD in the observation group were lower than those in the control group after intervention, suggesting that the mental state of postoperative patients with gastric cancer could be improved more obviously by adding TMC nursing on the basis of routine nursing. The research of Ye et al. also pointed out that TCM psychological care is extremely effective in improving the unhealthy psychology of patients after operation, and its effect on relieving postoperative anxiety and tension is better than that of routine nursing mode [17].
Most patients with gastrointestinal tumors need to fast before operation, especially for patients with gastric cancer, and longer fasting can cause stomach discomfort. Some studies pointed out that fasting for more than 48 hours can cause gastrointestinal mucosal dysfunction and reduce the absorption of nutrients, which is not conducive to the recovery of patients after operation [18]. In this study, the first postoperative exhaust time, the regression time of epigastric distension symptoms, the first defecation time and the recovery time of normal eating in the observation group were shorter than those in the control group, suggesting that the addition of TCM nursing on the basis of routine nursing can significantly improve the gastrointestinal dysfunction of patients with gastric cancer after operation and promote the recovery of gastrointestinal function more quickly. The research of Liu et al. also showed that the nursing measures of TCM diet intervention have more obvious effect on the recovery of gastrointestinal function of patients with gastrointestinal tumor after operation, and the body has better nutrients absorption [19]. This is because in the aspect of diet, TCM can coordinate cold and heat and both the five flavors according to the food properties of tropism of nature and taste and cold and heat. It can not only ensure the nutrition of the food, but also balances the drug properties of the food, which is beneficial to the absorption of the body with less stimulation to the gastrointestinal tract, so it is more conducive to the recovery of gastrointestinal function [20].
Radical surgery for gastric cancer can cause great damage to the body, inducing strong stress response and acute inflammatory reaction after operation, which is not conducive to the recovery of various functions of the body after operation [21]. In addition to take medical measures to reduce the inflammatory reaction of the body, reasonable nursing intervention can also alleviate the symptoms of acute inflammation, and the reduction of inflammatory state is very beneficial to the recovery of patients after operation. In this study, the levels of serum TNF-α, CRP and IL-1β in the observation group were lower than those in the control group after intervention, suggesting that the addition of TCM nursing on the basis of routine nursing can obviously alleviate the acute inflammatory state of patients with gastric cancer after operation. Liao et al. also compared the effects of the nursing mode of conventional western medicine and combination of TCM with western medicine on postoperative inflammatory state of patients [22]. The results showed that the nursing mode of combination of TCM with western medicine was more effective in controlling postoperative inflammatory state. It is speculated that due to the rapid recovery of gastrointestinal function and the improvement of immune function under the nursing mode of TCM, the control of inflammation is more effective. However, the specific mechanism of relieving inflammation is not clear, and the further research is needed to confirm it in the later stage. Finally, this study found that the scores of SES and GQOLI-74 in the observation group were higher than those in the control group, and the total incidence of adverse reactions in the observation group was lower than that in the control group, suggesting that the addition of the TCM nursing on the basis of routine nursing can more effectively enhance patients’ postoperative self-esteem, reduce the occurrence of postoperative adverse reactions and improve their postoperative quality of life. However, this study is a single-center study, and the sample size is limited. In the later stage, a multi-center large sample study is still needed to confirm the effect of TCM nursing on the functional recovery of patients with gastric cancer after operation.
To sum up, perioperative TCM nursing care for patients with gastric cancer can more obviously improve postoperative gastrointestinal dysfunction, alleviate acute inflammation, improve postoperative poor mental state, reduce the occurrence of postoperative complications, and finally improve the quality of life of patients after operation, which is worthy of clinical application.
Disclosure of conflict of interest
None.
References
- 1.Morgan R, Cassidy M, DeGeus SWL, Tseng J, McAneny D, Sachs T. Presentation and survival of gastric cancer patients at an urban academic safety-net hospital. J Gastrointest Surg. 2019;23:239–246. doi: 10.1007/s11605-018-3898-3. [DOI] [PubMed] [Google Scholar]
- 2.Kanda M. Preoperative predictors of postoperative complications after gastric cancer resection. Surg Today. 2020;50:3–11. doi: 10.1007/s00595-019-01877-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cai Y, Boyd DL. Effect of a traditional Chinese medicine course for undergraduate nursing students: a pre-/post-test study. Nurse Educ Today. 2018;70:87–93. doi: 10.1016/j.nedt.2018.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Huang CH, Chang HP, Su SY, Chen WK, Chang YJ, Lee YC, Kuo YJ. Traditional Chinese medicine is associated with a decreased risk of heart failure in breast cancer patients receiving doxorubicin treatment. J Ethnopharmacol. 2019;229:15–21. doi: 10.1016/j.jep.2018.09.030. [DOI] [PubMed] [Google Scholar]
- 5.Liu Q, Qi B, Zhang L, Zhang M, Xiao L. Effect of continuous nursing intervention on psychological state and medication compliance of patients with acute myocardial infarction after PCI. Panminerva Med. 2020;10:237–246. doi: 10.23736/S0031-0808.20.04077-X. [DOI] [PubMed] [Google Scholar]
- 6.Vakil N, Vieth M, Wernersson B, Wissmar J, Dent J. Diagnosis of gastro-oesophageal reflux disease is enhanced by adding oesophageal histology and excluding epigastric pain. Aliment Pharmacol Ther. 2017;45:1350–1357. doi: 10.1111/apt.14028. [DOI] [PubMed] [Google Scholar]
- 7.Tan C, Chen W, Wu Y, Chen S. Chinese medicine for mental disorder and its applications in psychosomatic diseases. Altern Ther Health Med. 2013;19:59–69. [PubMed] [Google Scholar]
- 8.Li F, Du H, Li S, Liu J. The association between metabolic syndrome and gastric cancer in Chinese. Front Oncol. 2018;8:326. doi: 10.3389/fonc.2018.00326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu KC, Wei HT, Chang SC, Hsu CH. Efficacy of electroacupuncture combined with auricular point pressing in improving mental well-being among individuals with heroin use disorder: a randomized controlled crossover trial and pilot study. Evid Based Complement Alternat Med. 2020;2020:3748056. doi: 10.1155/2020/3748056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zimmerman M, Martin J, Clark H, McGonigal P, Harris L, Holst CG. Measuring anxiety in depressed patients: a comparison of the Hamilton anxiety rating scale and the DSM-5 anxious distress specifier interview. J Psychiatr Res. 2017;93:59–63. doi: 10.1016/j.jpsychires.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 11.Raimo S, Trojano L, Spitaleri D, Petretta V, Grossi D, Santangelo G. Psychometric properties of the hamilton depression rating scale in multiple sclerosis. Qual Life Res. 2015;24:1973–1980. doi: 10.1007/s11136-015-0940-8. [DOI] [PubMed] [Google Scholar]
- 12.Eberl C, Winkler I, Pawelczack S, Tröbitz E, Rinck M, Becker ES, Lindenmeyer J. Self-esteem consistency predicts the course of therapy in depressed patients. PLoS One. 2018;13:e0199957. doi: 10.1371/journal.pone.0199957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou Y, Zhou R, Li W, Lin Y, Yao J, Chen J, Shen T. Controlled trial of the effectiveness of community rehabilitation for patients with schizophrenia in Shanghai, China. Shanghai Arch Psychiatry. 2015;27:167–174. doi: 10.11919/j.issn.1002-0829.215026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hwang H, Lee KM, Son KL, Jung D, Kim WH, Lee JY, Kong SH, Suh YS, Lee HJ, Yang HK, Hahm BJ. Incidence and risk factors of subsyndromal delirium after curative resection of gastric cancer. BMC Cancer. 2018;18:765. doi: 10.1186/s12885-018-4681-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stamenkovic DM, Rancic NK, Latas MB, Neskovic V, Rondovic GM, Wu JD, Cattano D. Preoperative anxiety and implications on postoperative recovery: what can we do to change our history? Minerva Anestesiol. 2018;84:1307–1317. doi: 10.23736/S0375-9393.18.12520-X. [DOI] [PubMed] [Google Scholar]
- 16.Zemła AJ, Nowicka-Sauer K, Jarmoszewicz K, Wera K, Batkiewicz S, Pietrzykowska M. Measures of preoperative anxiety. Anaesthesiol Intensive Ther. 2019;51:64–69. doi: 10.5603/AIT.2019.0013. [DOI] [PubMed] [Google Scholar]
- 17.Ye J, Cai S, Cheung WM, Tsang HWH. An east meets west approach to the understanding of emotion dysregulation in depression: from perspective to scientific evidence. Front Psychol. 2019;10:574. doi: 10.3389/fpsyg.2019.00574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ismail S, Manaf RA, Mahmud A. Comparison of time-restricted feeding and Islamic fasting: a scoping review. East Mediterr Health J. 2019;25:239–245. doi: 10.26719/emhj.19.011. [DOI] [PubMed] [Google Scholar]
- 19.Liu Y, Gao X, Ding Y, Zhou Y, Liu X, Wang H, Wang Q, Ma B, Yao S. Effectiveness and safety of light vegetarian diet on functional constipation with gastrointestinal damp-heat pattern: an exploratory study protocol for randomized controlled trial. Medicine (Baltimore) 2019;98:e18325. doi: 10.1097/MD.0000000000018325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tao W, Luo X, Cui B, Liang D, Wang C, Duan Y, Li X, Zhou S, Zhao M, Li Y, He Y, Wang S, Kelley KW, Jiang P, Liu Q. Practice of traditional Chinese medicine for psycho-behavioral intervention improves quality of life in cancer patients: a systematic review and meta-analysis. Oncotarget. 2015;6:39725–39739. doi: 10.18632/oncotarget.5388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Long AJ, Burton PR, De Veer MJ, Ooi GJ, Laurie CP, Nottle PD, Watt MJ, Brown WA. Radical gastric cancer surgery results in widespread upregulation of pro-tumourigenic intraperitoneal cytokines. ANZ J Surg. 2018;88:e370–e376. doi: 10.1111/ans.14267. [DOI] [PubMed] [Google Scholar]
- 22.Liao YH, Chao YC, Sim BY, Lin HM, Chen MT, Chen CY. Rhodiola/cordyceps-based herbal supplement promotes endurance training-improved body composition but not oxidative stress and metabolic biomarkers: a preliminary randomized controlled study. Nutrients. 2019;11:2357. doi: 10.3390/nu11102357. [DOI] [PMC free article] [PubMed] [Google Scholar]


