Abstract
Objective: This study explored and analyzed the effects of PDCA-based nursing intervention on the activities of daily living, neurological function and self-management of patients with acute cerebral stroke. Methods: A total of 137 patients with acute cerebral stroke who were hospitalized from March 2018 to March 2020 were enrolled and divided into the observation-group (n = 70) and the control-group (n = 67). The control-group was given routine care, while those subjects in the observation group were provided with nursing intervention under the optimization of PDCA cycling. The activities of daily living (ADL), NIHSS score, self-management ability and life quality were compared between these two groups. Results: ADL scores of the two groups after intervention were much higher than those without intervention (P<0.05), and the observation-group had apparently higher scores than the control-group (P<0.05). After intervention, the NIHSS scores of the two groups were much lower than before intervention (P<0.05), and the score of the observation-group was remarkably lower than the control-group (P<0.05). After intervention, the scores of each dimension of self-management behavior in both groups increased substantially compared to prior-intervention, and the score was higher in observation-group than in control-group (P<0.05). In addition, the two groups had increased scores in each dimension of life quality in post-intervention (P<0.05), and the observation-group had evidently higher scores than the control-group (P<0.05). Conclusion: PDCA-based nursing intervention can substantially enhance the daily living ability, neurological function, and self-management ability of patients, thus contributing to improve the clinical prognosis of patients and as such is worth popularizing.
Keywords: PDCA cycling, nursing intervention, acute stroke, activities of daily living, neurological function, self-management ability
Introduction
As a common cerebrovascular disease seen in clinical treatment, acute stroke has a high mortality and disability rate and imposes a great threat to patients’ life safety [1]. In recent years, with the changes of people’s lifestyles, diet structure and living habits, the incidence rate of acute stroke has increased remarkably, and the age of onset has gradually become younger [2,3]. The rapid development of modern medical technology has made great progress in the treatment of acute stroke, and the mortality rate of patients has been substantially reduced. However, lingering dysfunction is usually found in patients, which increases the suffering of patients and leads to a decrease in their quality of life. Therefore, it has become a clinical focus to promote the best possible recovery of neurological function and improve the quality of life [4,5]. PDCA cycle, which was firstly proposed by Dr. Deming in the United States, includes four stages of P (Plan), D (Do), C (Check) and A (Action). It is a standardized and scientific cycle system that is widely used in quality management, in which continuous learning and improvement are carried out [6]. In order to further promote the rehabilitation of patients, this study explored and analyzed the efficacy of PDCA-based nursing intervention on ADL, neurological function and self-management of patients with acute cerebral stroke. The report is as follows.
Data and methods
Clinical data
A total of 137 patients with acute cerebral stroke hospitalized from March 2018 to March 2020 were enrolled and randomly divided into the observation-group (n = 70) and the control-group (n = 67). This study was approved by the ethics department in our hospital.
Inclusion and exclusion standard
Inclusive Criteria: ① The patients met the diagnostic criteria of acute stroke and were confirmed by CT or MRI examination [7]; ② No prior history of stroke; ③ Patients that were accompanied by limb dysfunction and neurological deficits; ④ Patients and their families voluntarily signed the informed consent.
Exclusive Criteria: ① Patients with malignant tumor; ② Patients with history of mental disease or disturbance of consciousness; ③ Patients with immune system diseases or hematopoietic system diseases; ④ Those unable to cooperate; ⑤ Patients who received thrombolytic therapy within one week of onset; ⑥ Patients with severe disorders of the liver, kidney or heart function.
Method
The control-group was given routine nursing care, including the health training for patients and families upon admission, guidance on diet and life for patients, turn over support and rehabilitative training.
The observation-group received PDCA-based nursing intervention, with specific procedures as follows: ① Plan: set up the acute stroke management team. We retrospectively analyzed the previous nursing experience and discussed the problems that existed in rehabilitative nursing of patients to explore the causes and formulate corresponding improvement targets. In addition, we analyzed the possible problems and their influencing factors, organized corresponding plans for the key points of the problems, and put forward feasible and effective solutions. ② Do: The specialized staff adopted the PDCA management mode to collect the patient’s data. The responsible physician and nurses evaluated the patient’s condition, introduced the patient ot admission information and explained the necessity and function of nursing management, enabling the patients and their families to actively cooperate with the management. We instructed the patients to take balance movement training and daily living training. The nursing staff pasted the nursing plan in front of the patient’s bed, and informed the patients and their families of the matters needing attention in daily life. Nurses kept the patient’s skin clean and tidy, and cleaned the skin soaked with urine, sweat and drainage materials in time; and the nursing staff communicated with patients, to understand their concerns, and listened patiently and gave guidance to relieve the negative emotions of patients. The nurses communicated with patients to understand their concerns and alleviate their negative moods. ③ Check: The working group regularly reported on the progression of nursing work, conducted effective analysis of results, put forward the deficiencies and problems during nursing process, and listed them out for discussion. ④ Action: The quality control team visited patients and their families every day to understand their satisfaction and compliance with the nursing care, and ensured the project was implemented smoothly. In addition, the team put forward reasonable opinions, understood the rehabilitative situation of patients, made summary analysis, and formulated corresponding solutions, which were included in the nursing plan for the following week.
Index observation
① Evaluation of ability of daily living (ADL) [8]: we evaluated the patients by Barthel Index (BI) before and after intervention. The scale scored 0-100 points, and the lower scores referred to a more severe dysfunction of patients.
② Evaluation by National Institutes of Health Stroke Scale (NIHSS) [9]: The neurological function of patients before and after intervention was evaluated by referring to the scoring points in Clinical Neurological Defect Scale of Stroke Patients and the National Institutes of Health Stroke Scale (NIHSS). The NIHSS included language, body movement, consciousness, cognition, etc. A higher score indicated a more severer deficit in neurological function of patients.
③ Evaluation of self-management behavior [10]: The patients’ self-management behavior were scored by the Self-management Behavior Scale for Stroke before and after intervention. The scale included 7 dimensions and 51 items of disease management, medication management, diet management, daily living management, emotional management, social function and interpersonal management, and rehabilitation management. The evaluation was carried out with a Liket5 score method, and the higher score referred to better self-management behavior of patients.
④ Evaluation of life quality [11]: the patients’ quality of life before and after intervention was evaluated by SF-36 health scale. The scale included eight dimensions: physiological functioning (PF), role-functioning (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE) and mental health (MH). The total score of dimensions was 100 points, and the higher score referred to the better quality of life of patients.
Statistical analysis
Data processing and analysis of the study were conducted by SPSS 25.0. The comparison of measurement data was by t-test and enumeration data was by χ 2 test. P<0.05 referred that the difference was statistically significant.
Results
Clinical data
There was no significant difference in the clinical data between the two groups (P>0.05), (Table 1).
Table 1.
Comparison of clinical data between the two groups
| Group | Number of cases | Gender | Age (years, ± sd) | Types of stroke | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Male | Female | Cerebral infarction | Cerebral hemorrhage | |||
| Observation group | 70 | 39 | 31 | 64.28±12.10 | 48 | 22 |
| Control group | 67 | 35 | 32 | 65.03±13.42 | 38 | 29 |
| t/χ 2 | - | 0.167 | 0.344 | 2.059 | ||
| P | - | 0.683 | 0.732 | 0.151 | ||
Evaluation of ADL
ADL scores of the two groups after intervention were much higher than those without intervention (P<0.05), and the observation-group had apparently higher scores than the control-group (P<0.05) (Table 2 and Figure 1).
Table 2.
Comparison of ADL scores between the two groups before and after intervention (points, x̅ ± sd)
| group | Number of cases | Before intervention | After intervention | t | P |
|---|---|---|---|---|---|
| Observation group | 70 | 78.64±13.10 | 52.15±9.72 | 13.587 | 0.000 |
| Control group | 67 | 79.03±12.66 | 61.02±10.25 | 9.117 | 0.000 |
| t | - | 0.178 | 5.217 | - | - |
| P | - | 0.859 | 0.000 | - | - |
Figure 1.
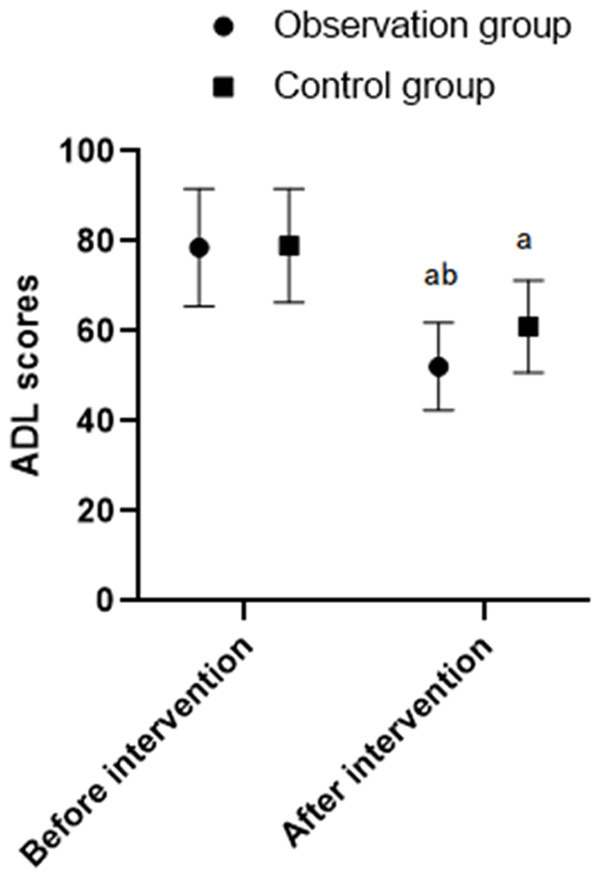
Comparison of ADL scores between the two groups before and after intervention. Note: Compared with before intervention, a P<0.05; compared with after intervention, b P<0.05.
Evaluation of NIHSS
After intervention, the NIHSS scores of the two groups were much lower than before intervention (P<0.05), and the scores of the observation-group were remarkably lower than the control-group (P<0.05) (Table 3 and Figure 2).
Table 3.
Comparison of NIHSS scores between the two groups before and after intervention (points, x̅ ± sd)
| Group | Number of cases | Before intervention | After intervention | t | P |
|---|---|---|---|---|---|
| Observation group | 70 | 30.82±7.83 | 15.73±4.28 | 14.148 | 0.000 |
| Control group | 67 | 31.05±8.22 | 19.21±5.21 | 9.958 | 0.000 |
| t | - | 0.168 | 4.280 | - | - |
| P | - | 0.867 | 0.000 | - | - |
Figure 2.
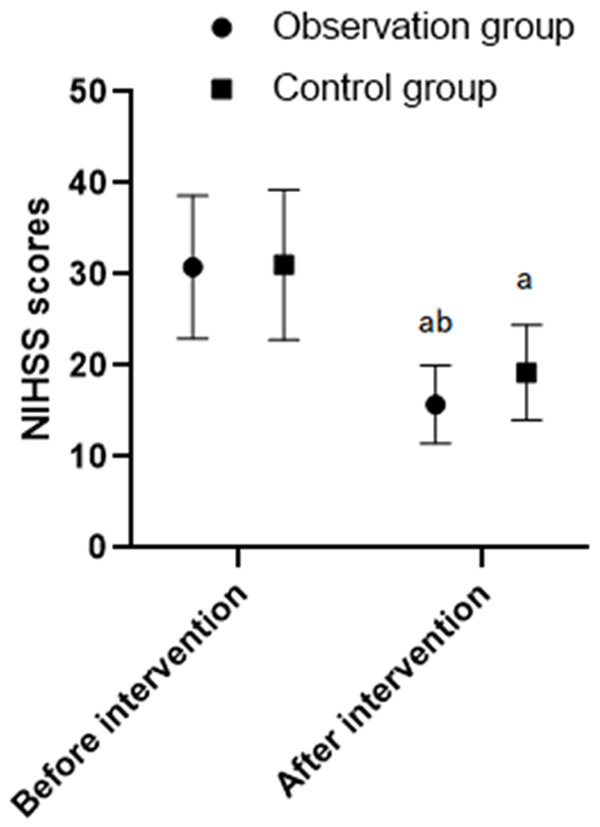
Comparison of NIHSS scores between the two groups before and after intervention. Note: Compared with before intervention, a P<0.05; compared with after intervention, b P<0.05.
Evaluation of self-management behavior
After intervention, the scores of each dimension of self-management behavior in two groups increased substantially compared to prior-intervention, and the score was higher in the observation-group than in the control-group (P<0.05) (Tables 4 and 5).
Table 4.
Scores of self-management ability between the two groups before and after intervention (score, x̅ ± sd)
| Group | Number of cases | Disease management | Medication management | Diet management | Daily life management |
|---|---|---|---|---|---|
| Observation group | 70 | 47.48±10.22 | 26.57±4.33 | 32.47±6.94 | 33.78±9.87 |
| Control group | 67 | 38.84±9.30 | 21.46±4.38 | 27.69±7.21 | 24.16±6.46 |
| t | - | 5.168 | 6.866 | 3.954 | 6.718 |
| P | - | 0.000 | 0.000 | 0.000 | 0.000 |
Table 5.
Scores of self-management ability between two groups before and after intervention-continued (score, x̅ ± sd)
| Group | Number of cases | Emotion management | Social function and interpersonal management | Recovery management |
|---|---|---|---|---|
| Observation group | 70 | 18.27±3.15 | 22.38±2.17 | 25.47±4.21 |
| Control group | 67 | 15.22±2.64 | 18.97±2.06 | 20.93±3.79 |
| t | - | 6.129 | 9.425 | 6.624 |
| P | - | 0.000 | 0.000 | 0.000 |
Evaluation of life quality
The two groups had increased scores in each dimension of life quality post-intervention (P<0.05), and the observation-group had evidently higher scores than the control-group (P<0.05) (Tables 6 and 7).
Table 6.
Scores of life quality between two groups before and after intervention (points, x̅ ± sd)
| Group | Time | PF | RP | BP | CH |
|---|---|---|---|---|---|
| Observation group (n = 70) | Before intervention | 56.49±6.47 | 58.93±5.94 | 55.96±6.17 | 54.85±6.92 |
| After intervention | 68.95±7.83a | 70.25±6.44a | 69.08±5.63a | 67.48±6.73a | |
| T | 10.263 | 10.810 | 13.142 | 10.947 | |
| P | 0.000 | 0.000 | 0.000 | 0.000 | |
| Control group (n = 67) | Before intervention | 56.17±7.22 | 58.20±6.07 | 55.73±6.48 | 55.07±6.34 |
| After intervention | 65.48±7.39 | 65.48±6.82 | 62.37±5.94 | 61.92±5.42 | |
| T | 7.376 | 6.527 | 6.183 | 6.722 | |
| P | 0.000 | 0.000 | 0.000 | 0.000 |
Note: Compared with the control group;
P<0.05.
Table 7.
Scores of life quality between two groups before and after intervention-continued (points, x̅ ± sd)
| Group | time | VT | SF | RE | MH |
|---|---|---|---|---|---|
| Observation group (n = 70) | Before intervention | 60.37±5.37 | 56.38±6.20 | 54.04±5.97 | 57.48±6.84 |
| After intervention | 73.85±7.20a | 68.39±6.84a | 67.21±7.03a | 66.94±7.05a | |
| t | 12.458 | 10.776 | 11.837 | 7.972 | |
| P | 0.000 | 0.000 | 0.000 | 0.000 | |
| Control group (n = 67) | Before intervention | 59.74±6.21 | 56.04±5.97 | 54.83±6.38 | 57.03±5.97 |
| After intervention | 67.43±6.02 | 62.64±6.48 | 61.46±6.58 | 62.31±7.39 | |
| t | 7.278 | 6.131 | 5.921 | 4.549 | |
| P | 0.000 | 0.000 | 0.000 | 0.000 |
Note: Compared with the control group;
P<0.05.
Discussion
Acute stroke is a common disorder of blood circulation seen in clinical work. The sudden onset and rapid progression of disease often lead to different degrees of limb dysfunction of patients, seriously affecting their quality of life [12]. In addition, patients with acute stroke often suffer from cognitive impairment with the main performance of poor memory, inattention, poor orientation, etc., seriously affecting the clinical prognosis of patients [13,14].
The PDCA cycling management mode is a new management mode proposed in the middle of the 20th century. In recent years, it has been widely used in clinical nursing management by domestic and foreign scholars, and it is a standardized and scientific circulation system. A large number of clinical studies have confirmed that PDCA cycling can effectively improve the quality of clinical nursing management [15-17]. Patients with acute stroke often suffer from lower ability of daily living due to limb dysfunction. The PDCA-based nursing management mode can effectively evaluate the patient’s condition. Under this mode, nursing staff develop personalized rehabilitative training programs, adjust the plan in time according to the actual situation of patients and apply it to the implementation of the next plan In the whole process, the nursing work is closely linked and the actual needs of patients are taken as the guidance, which greatly improves the work efficiency and enables the nursing quality to occur as a spiral rise [18,19].
This study explored and analyzed the efficacy of PDCA-based nursing intervention on ADL, neurological function and self-management of patients with acute cerebral stroke. According to the results, the ADL, neurological function, self-management ability and life quality in the observation-group had obvious post-intervention improvement compared to those in the control-group. The results are similar to those reported by other scholars [20,21], the PDCA-based nursing intervention can effectively improve ADL, neurological function, self-management behavior and quality of life in patients with acute stroke. Under the PDCA cycling management mode, nursing staff are actively involved in the nursing work of patients, they timely understand the patient’s condition and psychological changes. This not only enables timely adjustment of nursing measures, but also provides individualized nursing services for each patient. The improvement of patients’ compliance with treatment can promote the recovery of disease, and also promote the ability of patients to manage their conditions, thereby improving patients’ satisfaction with nursing services and clinical prognosis [22-24].
However, due to the insufficient sample quantity included in this study, more larger sample data are required to analyze the effect of nursing strategies of patients with acute stroke.
In conclusion, the PDCA-based nursing intervention can substantially enhance the daily living ability, neurological function, and self-management ability of patients, thus contributing to improvement of the clinical prognosis of patients and is worth popularizing.
Disclosure of conflict of interest
None.
References
- 1.Muñoz Venturelli P, Robinson T, Lavados PM, Olavarría VV, Arima H, Billot L, Hackett ML, Lim JY, Middleton S, Pontes-Neto O, Peng B, Cui L, Song L, Mead G, Watkins C, Lin RT, Lee TH, Pandian J, de Silva HA, Anderson CS HeadPoST Investigators. Regional variation in acute stroke care organisation. J Neurol Sci. 2016;371:126–130. doi: 10.1016/j.jns.2016.10.026. [DOI] [PubMed] [Google Scholar]
- 2.Holmes DR Jr, Hopkins LN. Interventional cardiology and acute stroke care going forward: JACC review topic of the week. J Am Coll Cardiol. 2019;73:1483–1490. doi: 10.1016/j.jacc.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 3.Perry C, Papachristou I, Ramsay AIG, Boaden RJ, McKevitt C, Turner SJ, Wolfe CDA, Fulop NJ. Patient experience of centralized acute stroke care pathways. Health Expect. 2018;21:909–918. doi: 10.1111/hex.12685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boulanger JM, Lindsay MP, Gubitz G, Smith EE, Stotts G, Foley N, Bhogal S, Boyle K, Braun L, Goddard T, Heran M, Kanya-Forster N, Lang E, Lavoie P, McClelland M, O’Kelly C, Pageau P, Pettersen J, Purvis H, Shamy M, Tampieri D, vanAdel B, Verbeek R, Blacquiere D, Casaubon L, Ferguson D, Hegedus Y, Jacquin GJ, Kelly M, Kamal N, Linkewich B, Lum C, Mann B, Milot G, Newcommon N, Poirier P, Simpkin W, Snieder E, Trivedi A, Whelan R, Eustace M, Smitko E, Butcher K. Canadian stroke best practice recommendations for acute stroke management: prehospital, emergency department, and acute inpatient stroke care, 6th edition, update 2018. Int J Stroke. 2018;13:949–984. doi: 10.1177/1747493018786616. [DOI] [PubMed] [Google Scholar]
- 5.Raychev RI, Stradling D, Patel N, Gee JR, Lombardi DA, Moon JL, Brown DM, Pathak M, Yu W, Stratton SJ, Cramer SC. Evolution of a US county system for acute comprehensive stroke care. Stroke. 2018;49:1217–1222. doi: 10.1161/STROKEAHA.118.020620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adeoye O, Nyström KV, Yavagal DR, Luciano J, Nogueira RG, Zorowitz RD, Khalessi AA, Bushnell C, Barsan WG, Panagos P, Alberts MJ, Tiner AC, Schwamm LH, Jauch EC. Recommendations for the establishment of stroke systems of care: a 2019 update. Stroke. 2019;50:187–210. doi: 10.1161/STR.0000000000000173. [DOI] [PubMed] [Google Scholar]
- 7.Bornstädt D, Gertz K, Lagumersindez Denis N, Seners P, Baron JC, Endres M. Sensory stimulation in acute stroke therapy. J Cereb Blood Flow Metab. 2018;38:1682–1689. doi: 10.1177/0271678X18791073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chimatiro GL, Rhoda AJ. Scoping review of acute stroke care management and rehabilitation in low and middle-income countries. BMC Health Serv Res. 2019;19:789. doi: 10.1186/s12913-019-4654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akosile CO, Banjo TO, Okoye EC, Ibikunle PO, Odole AC. Informal caregiving burden and perceived social support in an acute stroke care facility. Health Qual Life Outcomes. 2018;16:57. doi: 10.1186/s12955-018-0885-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meisel KM, Thabet AM, Josephson SA. Acute care of ischemic stroke patients in the hospital. Semin Neurol. 2015;35:629–637. doi: 10.1055/s-0035-1564301. [DOI] [PubMed] [Google Scholar]
- 11.Molidor S, Overbaugh KJ, James D, White CL. Palliative care and stroke: an integrative review of the literature. J Hosp Palliat Nurs. 2018;20:358–367. doi: 10.1097/NJH.0000000000000450. [DOI] [PubMed] [Google Scholar]
- 12.Theofanidis D, Gibbon B. Nursing interventions in stroke care delivery: an evidence-based clinical review. J Vasc Nurs. 2016;34:144–151. doi: 10.1016/j.jvn.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 13.Wilkins SS, Akhtar N, Salam A, Bourke P, Joseph S, Santos M, Shuaib A. Acute post stroke depression at a Primary Stroke Center in the Middle East. PLoS One. 2018;13:e0208708. doi: 10.1371/journal.pone.0208708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ren L, Li C, Li W, Zeng Y, Ye S, Li Z, Feng H, Lei Z, Cai J, Hu S, Sui Y, Liu Q, Cheung BMY. Fast-tracking acute stroke care in China: Shenzhen stroke emergency map. Postgrad Med J. 2019;95:46–47. doi: 10.1136/postgradmedj-2018-136192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baatiema L, Otim ME, Mnatzaganian G, de-Graft Aikins A, Coombes J, Somerset S. Health professionals’ views on the barriers and enablers to evidence-based practice for acute stroke care: a systematic review. Implement Sci. 2017;12:74. doi: 10.1186/s13012-017-0599-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Josephson SA, Kamel H. The acute stroke care revolution: enhancing access to therapeutic advances. JAMA. 2018;320:1239–1240. doi: 10.1001/jama.2018.11122. [DOI] [PubMed] [Google Scholar]
- 17.Ng JC, Churojana A, Pongpech S, Vu LD, Sadikin C, Mahadevan J, Subramaniam J, Jocson VE, Lee W. Current state of acute stroke care in Southeast Asian countries. Interv Neuroradiol. 2019;25:291–296. doi: 10.1177/1591019918811804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suntrup-Krueger S, Minnerup J, Muhle P, Claus I, Schröder JB, Marian T, Warnecke T, Kalic M, Berger K, Dziewas R. The effect of improved dysphagia care on outcome in patients with acute stroke: trends from 8-year data of a large stroke register. Cerebrovasc Dis. 2018;45:101–108. doi: 10.1159/000487811. [DOI] [PubMed] [Google Scholar]
- 19.Lachkhem Y, Rican S, Minvielle É. Understanding delays in acute stroke care: a systematic review of reviews. Eur J Public Health. 2018;28:426–433. doi: 10.1093/eurpub/cky066. [DOI] [PubMed] [Google Scholar]
- 20.Matos Diaz I, Liang JW, Ostojic LV, Tansy AP. Acute stroke multimodal imaging: present and potential applications toward advancing care. Semin Neurol. 2017;37:558–565. doi: 10.1055/s-0037-1607355. [DOI] [PubMed] [Google Scholar]
- 21.Rudilosso S, Laredo C, Vera V, Vargas M, Renú A, Llull L, Obach V, Amaro S, Urra X, Torres F, Jiménez-Fàbrega FX, Chamorro Á. Acute stroke care is at risk in the era of covid-19: experience at a comprehensive stroke center in barcelona. Stroke. 2020;51:1991–1995. doi: 10.1161/STROKEAHA.120.030329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li Z, Zhang X, Wang K, Wen J. Effects of early mobilization after acute stroke: a meta-analysis of randomized control trials. J Stroke Cerebrovasc Dis. 2018;27:1326–1337. doi: 10.1016/j.jstrokecerebrovasdis.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 23.Puri I, Bhatia R, Vibha D, Singh MB, Padma MV, Aggarwal P, Prasad K. Stroke-related education to emergency department staff: an acute stroke care quality improvement initiative. Neurol India. 2019;67:129–133. doi: 10.4103/0028-3886.253636. [DOI] [PubMed] [Google Scholar]
- 24.Melnychuk M, Morris S, Black G, Ramsay AIG, Eng J, Rudd A, Baim-Lance A, Brown MM, Fulop NJ, Simister R. Variation in quality of acute stroke care by day and time of admission: prospective cohort study of weekday and weekend centralised hyperacute stroke unit care and non-centralised services. BMJ Open. 2019;9:25366. doi: 10.1136/bmjopen-2018-025366. [DOI] [PMC free article] [PubMed] [Google Scholar]


