Abstract
Aim: This study aims to investigate the effects of comprehensive nursing intervention on the negative emotions, quality of life, and nursing satisfaction in intracerebral hemorrhage patients (ICH). Methods: We recruited 72 ICH patients admitted to our hospital from February 2017 to March 2019 for this study, among whom 35 patients underwent conventional nursing (the control group, CG) and the other 37 patients underwent comprehensive nursing (the research group, RG). The Self-perceived Burden Scale (SPBS), Hamilton Depression Scale (HAMD), Pittsburgh Sleep Quality Index (PSQI), Fugl-Meyer Assessment (FAM), and Barthel index (BI) scores of all the patients were recorded. The patients returned to the hospital 6 months after the discharge to check if any complications had occurred. The Generic Quality of Life Inventory-74 (GQOL-74) scores and the Nursing Satisfaction Questionnaire scores, a questionnaire made by our hospital, were also recorded. Results: After the nursing, the RG had significantly lower SPBS, HAMD, and PSQI scores and significantly higher FAM, BI, and GQOL-74 scores than the CG (all P<0.05). The patient satisfaction levels with the nursing were significantly higher in the RG than in the CG (97.30% vs. 77.14%, P<0.05). Complications occurred in both groups within 6 months after the discharge. The total incidence of complications was significantly lower in the RG than in the CG (2.70% vs. 22.86%, P<0.05). Conclusion: Comprehensive nursing can relieve the negative emotions of ICH patients, enhance their self-management abilities, reduce the occurrence of complications, and improve their sleep quality and quality of life.
Keywords: Intracerebral hemorrhage, comprehensive nursing, quality of life, negative emotions
Introduction
Intracerebral hemorrhage (ICH) is a prevalent cerebrovascular disease in middle-aged and elderly people [1]. People affected by ICH have tended to be younger in recent years, with an increasing number of cases under 40 years of age [2,3]. ICH, with a quick onset and a rapid deterioration, damages the central nervous system and impairs the patients’ body functions [4,5]. Therefore, the treatment of ICH has always been a major clinical research priority. More and more in-depth studies at home and abroad have shown that effective nursing interventions are the key to improving the prognoses of ICH patients [6-8]. Nursing quality management is the process of planning, controlling, and organizing the elements of nursing to achieve the goals of nursing and meet the requirements of patients [9]. Enhanced nursing quality can improve the prognoses of many diseases [10-12]. In recent years, our hospital has been endeavoring to improve nursing quality and has achieved positive results in many departments.
In this modernized society, ICH patients and their families have increasingly high requirements and expectations for the treatment process and quality of care after admission [13]. The conventional nursing model cannot satisfy the needs and expectations of most patients for nursing due to its ineffective information transmission and poor nursing quality [14]. A previous study suggests that the conventional nursing model needs to be improved [15]. The clinical manifestations of acute ICH are closely related to the speed and amount of bleeding, including cerebral edema, intracranial hypertension, high fever, brain herniation, impaired limb and language functions, suppressed respiratory and heartbeat, shock, and even death. Survivors of ICH may suffer from a variety of complications, which affect patients and their families. ICH patients are confronted with a high disability rate and an even higher mortality rate. Reliable clinical practice, proper nursing care, effective medication, and careful rehabilitation management can greatly enhance the treatment response rate in patients and improve their prognoses. Comprehensive nursing intervention is an interdisciplinary, deeply integrated, and programmed modern nursing model, which focuses on the stratification before admission and the comprehensive improvement of the general nursing plan [16,17].
Materials and methods
Basic participant data
We recruited 72 ICH patients admitted to the Affiliated Hospital of Inner Mongolia University for Nationalities from February 2017 to March 2019. Among them, 35 patients undergoing conventional nursing were assigned to the control group (CG), including 19 males and 16 females, ranging in age from 60 to 85 years old, with an average age of 68.1 ± 3.2 years; the other 37 cases undergoing comprehensive nursing were assigned to the research group (RG), including 21 males and 16 females, ranging in age from 61 to 85 years old, with an average age of 68.2 ± 3.3 years. This study obtained ethical approval from the Ethics Committee of our hospital.
Inclusion and exclusion criteria
The inclusion criteria were as follows: patients diagnosed with ICH clinically, conscious patients able to complete the questionnaires independently, patients ranging in age from 60 to 85 years old, patients with complete clinical general information, patients willing to cooperate with the medical staff in our hospital to complete the investigation. All the patients or their immediate family members signed the written informed consent.
The exclusion criteria were as follows: patients who withdrew from this study midway, patients with comorbid malignancies, severe organ dysfunction, or infectious diseases, patients with poor treatment compliance, patients with physical disabilities, patients who were transferred to another hospital.
Nursing methods
The patients in the CG underwent conventional nursing
1. The patients’ conditions were closely monitored so that any abnormality was promptly reported to the attending doctor, who intervened. 2. The patient management was strengthened to prevent accidental risk events, such as falls and pressure sores. 3. The patients were given correct psychological guidance and counseling to reduce the risk of negative emotions occurring.
The patients in the RG underwent comprehensive nursing
1. A nursing team was assembled to analyze the advantages and disadvantages of conventional nursing and to initially design a comprehensive nursing plan based on the previous case data of ICH patients. 2. The members of the nursing team were trained on improved nursing philosophy to enhance their awareness of preventing pressure sores. The patients’ symptoms were recorded, discussed, and analyzed daily to optimize the nursing plan. 3. The probability of risk events in patients was graded according to their conditions. Patients of different risk grades were managed using different measures. For low-risk patients, the nurses kept the ground clean and dry, and hung anti-fall warning signs; for the high-risk patients, the nurses paid close attention to their medication and activities and assigned professional personnel to assist them in their physical activities.
Scoring criteria
Before the nursing and at one month after the nursing, the patients’ degrees of self-perceived burdens were assessed using Self-perceived Burden Scale (SPBS). The scale measures the patient burden from three dimensions: physical burdens (3 items), economic burdens (2 items), and emotional burdens (5 items), with 10 items in total. Each item is rated on a 5-point scale. Higher scores indicate greater self-perceived burdens. Before the nursing and at one month after the nursing, the patients depression levels were assessed using the 24-item version of the Hamilton Depression Scale (HAMD). Higher scores indicate more severe depression. Before and after the nursing, the patients’ sleep quality was assessed using Pittsburgh Sleep Quality Index (PSQI). It is a 21-point scale consisting of five questions rated by others and 19 self-rated questions. Higher scores indicate worse sleep quality. The performance in the patient’s activities of daily living was measured with the Barthel index (BI). Its scores range from 0 to 100, with higher scores indicating a greater living ability. The patients’ motor functions were assessed using Fugl-Meyer Assessment (FAM). It is a 100-point scale, with higher scores indicating stronger motor function. The patients’ quality of life was measured using Generic Quality of Life Inventory-74 (GQOL-74) from 4 dimensions. Each dimension is rated on a 100-point scale, with higher scores indicating a better quality of life. The patient satisfaction with the nursing was assessed using the Nursing Satisfaction Questionnaire, a questionnaire made by our hospital and comprised of 20 questions (5 points for each question). Scores of less than 70 points indicate dissatisfaction; scores ranging from 70 to 89 points denote moderate satisfaction; scores equal to or more than 90 points denote great satisfaction. Satisfaction rate = (number of cases with moderate satisfaction + great satisfaction)/total case number × 100%.
Outcome measures
The primary outcome measures were as follows: the SPBS, HAMD, PSQI, FAM, and BI scores.
The secondary outcome measures were as follows: the incidence of complications within 6 months after being discharged from the hospital; the GQOL-74 scores; the nursing satisfaction rate.
Statistical analysis
The collected data were statistically analyzed using SPSS 20.0 (IBM Corp, Armonk, NY, USA) and visualized using GraphPad 7. The distribution of the measurement data was analyzed using K-S tests. The measurement data following a normal distribution were represented as the mean ± standard deviation (mean ± SD). The comparisons between groups were analyzed using independent samples t-tests and the comparisons within a group were analyzed using paired t-tests. The count data were represented as the rate (%) and analyzed using chi-square tests, denoted as χ2. P<0.05 indicates that a difference is statistically significant.
Results
Basic patient data
The two groups were comparable because their differences in age, BMI, history of hypertension, smoking and drinking, place of residence, diet preferences, exercise habits, and course of the disease were not significant (P>0.05, Table 1).
Table 1.
Basic clinical data [n (%)]
| Research group (n = 37) | Control group (n = 35) | χ2 or t | P | |
|---|---|---|---|---|
| Age (years) | 68.2 ± 3.3 | 68.1 ± 3.2 | 0.130 | 0.897 |
| Hypertension history | 0.172 | 0.679 | ||
| Yes | 26 (70.27) | 23 (65.71) | ||
| No | 11 (29.73) | 12 (34.29) | ||
| BMI | 22.05 ± 1.24 | 22.02 ± 1.17 | 0.106 | 0.916 |
| Smoking history | 0.002 | 0.963 | ||
| Yes | 15 (40.56) | 14 (40.00) | ||
| No | 22 (59.46) | 21 (60.00) | ||
| Drinking history | 0.007 | 0.995 | ||
| Yes | 18 (48.65) | 17 (48.57) | ||
| No | 19 (51.35) | 18 (51.43) | ||
| Place of residence | 0.695 | 0.405 | ||
| Urban area | 23 (62.16) | 25 (71.43) | ||
| Rural area | 14 (37.84) | 10 (28.57) | ||
| Dietary preference | 0.008 | 0.927 | ||
| Light diet | 12 (32.43) | 11 (31.43) | ||
| Spicy diet | 25 (67.57) | 24 (68.57) | ||
| Exercise habits | 0.188 | 0.664 | ||
| Yes | 23 (62.16) | 20 (57.14) | ||
| No | 14 (37.84) | 15 (42.86) | ||
| Course of disease (week) | 3.74 ± 1.04 | 3.92 ± 0.86 | 0.798 | 0.428 |
Comparison of the SPBS and HAMD scores
Our comparison of the SPBS and HAMD scores between the two groups before the nursing showed no significant differences (P>0.05). After the nursing, the scores were significantly lower in the RG than in the CG (P<0.05, Figure 1).
Figure 1.
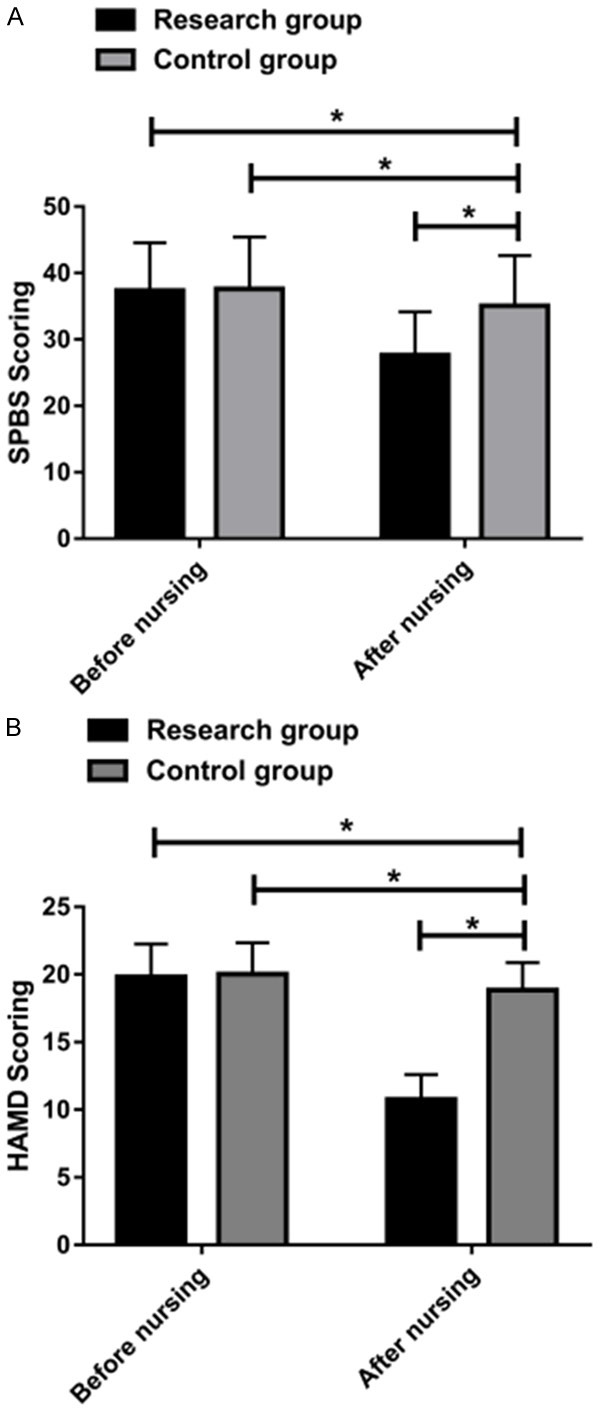
Comparison of the SPBS and HAMD scores. A. The SPBS scores decreased significantly in the RG after the nursing, lower than the scores in the CG. B. The HAMD scores decrease significantly in the RG after the nursing, lower than the scores in the CG. Note: The symbol “*” indicates a statistical difference between the two groups (P<0.05).
Comparison of the PSQI scores
Our comparison of the PSQI scores in the two groups before the nursing revealed no significant differences (P>0.05). After the nursing, the scores were significantly lower in the RG than in the CG (P<0.05, Figure 2).
Figure 2.
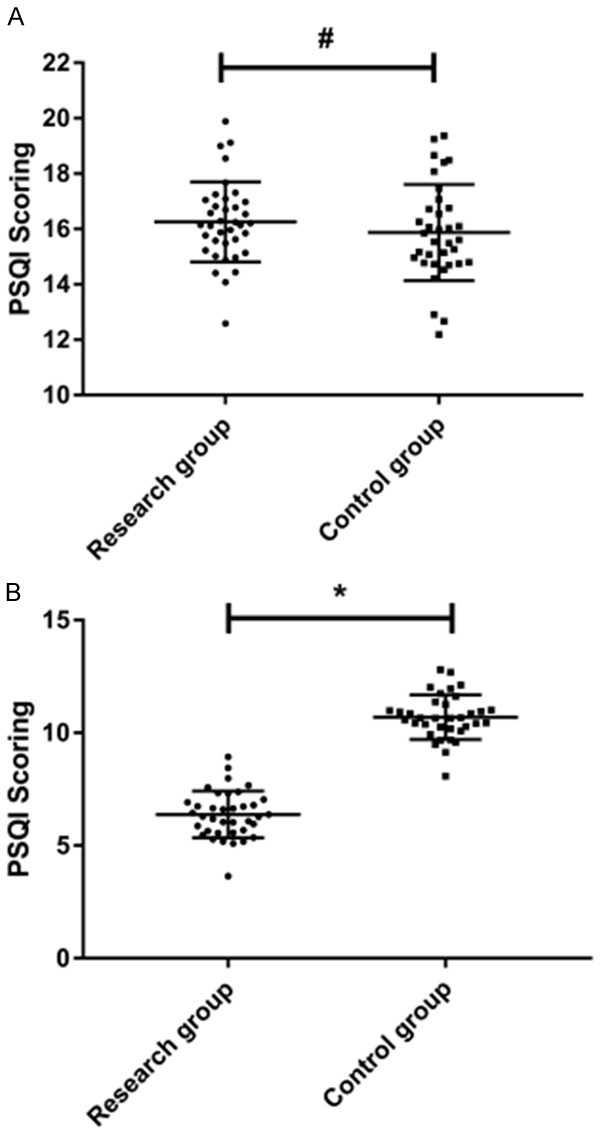
Comparison of the PSQI scores. A. Before the nursing, the PSQI scores in the two groups were not significantly different. B. After the nursing, the PSQI scores were significantly lower in the RG than in the CG. Note: The symbol “#” indicates no statistical difference between the two groups (P>0.05). The symbol “*” indicates a statistical difference between the two groups (P<0.05).
Comparison of the FAM and BI scores
The comparison of the FAM and BI scores between the two groups before the nursing revealed no statistical differences (P>0.05). After the nursing, the scores were significantly higher in the RG than in the CG (P<0.05, Figure 3).
Figure 3.
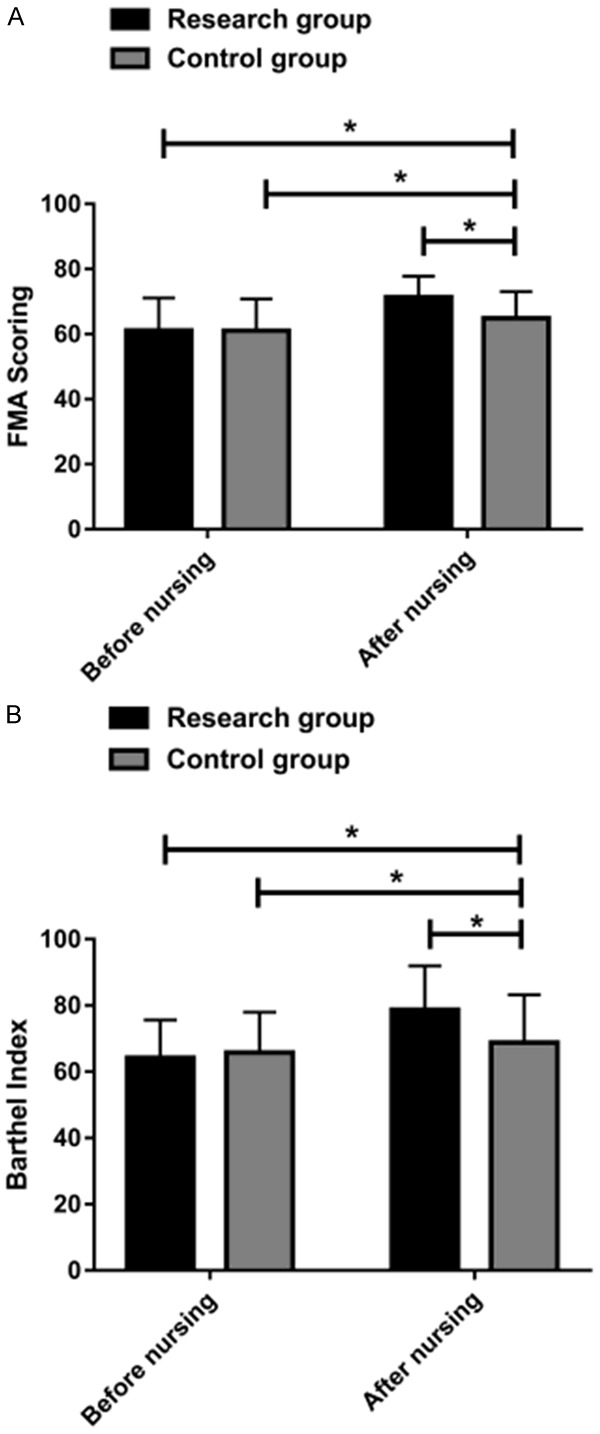
A comparison of the FAM and BI scores. A. The FAM scores increased significantly in the RG after the nursing, higher than the scores in the CG. B. The BI scores increased significantly in the RG after the nursing, higher than the scores in the CG. Note: The symbol “*” indicates a statistical difference between the two groups (P<0.05).
Comparison of the GQOL-74 scores
The GQOL-74 scores were totaled from the somatic function, psychological function, social function, and material life scores and were significantly higher in the RG than in the CG (P<0.05, Figure 4).
Figure 4.
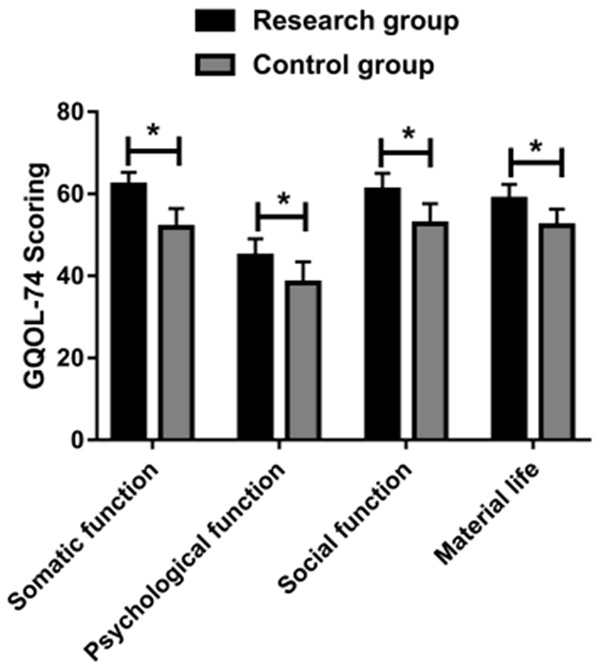
A comparison of the GQOL-74 scores. The GQOL-74 scores were significantly higher in the RG than in the CG. Note: The symbol “*” indicates a statistical difference between the two groups (P<0.05).
Comparison of the patient satisfaction with the nursing
The nursing satisfaction rate was significantly higher in the RG than in the CG (97.30% vs. 77.14%) (P<0.05, Table 2).
Table 2.
Comparison of the nursing satisfaction [n (%)]
| Groups | Case number | Great satisfaction | Moderate satisfaction | Dissatisfaction | Satisfaction rate (%) |
|---|---|---|---|---|---|
| Research group | 37 | 29 (78.38) | 7 (18.92) | 1 (2.70) | 36 (97.30) |
| Control group | 35 | 10 (28.57) | 17 (48.57) | 8 (22.86) | 27 (77.14) |
| t | 6.680 | ||||
| P | 0.010 |
Comparison of the incidences of complications within 6 months after the discharge
Complications occurred in both groups within 6 months after the discharge. The incidence of complications was significantly lower in the RG than in the CG (2.70% vs. 22.86%) (P<0.05, Table 3).
Table 3.
Comparison of the complications [n (%)]
| Complications | Research group (n = 37) | Control group (n = 35) | χ2 | P |
|---|---|---|---|---|
| Vomiting | 1 (2.70) | 2 (5.71) | ||
| Conscious disturbance | 0 (0.00) | 1 (2.86) | ||
| Pressure sores | 0 (0.00) | 2 (5.71) | ||
| Headache and dizziness | 0 (0.00) | 3 (8.57) | ||
| Total incidence | 1 (2.70) | 8 (22.86) | 6.680 | 0.010 |
Discussion
ICH patients, generally affected by dizziness, stroke, high blood pressure, and decreased muscle strength, have poor control over their own body and limited joint mobility, so they are vulnerable to risk events such as pressure sores and falls [18,19]. Moreover, drugs for treating ICH mainly act on the brain tissue and can induce side effects on the nerve center and the brain stem, which impairs ICH patients’ thinking abilities and limb coordination abilities [20]. Under the conventional nursing model, ICH patients are frequently affected by risk events due to inadequate attention from nurses and the lack of working initiative in some nurses [21]. Risk events may attenuate the effect of rehabilitation management, slow the recovery speed, aggravate the patient’s negative emotions, worsen the doctor-patient relationship, and greatly reduce the treatment coordination [22]. Therefore, it’s crucial to seek effective and comprehensive quality improvement in nursing. The wide application of comprehensive quality improvement in nursing in the medical field has achieved significantly positive results, and the great value of comprehensive quality improvement in nursing in multiple disciplines has been recognized by an increasing number of in-depth studies [23,24]. Especially for patients admitted to the department of neurology who have an impaired nerve center, a delicate, meticulous, and targeted nursing model is needed to improve their prognoses.
In this study, we provided comprehensive nursing intervention for ICH patients. The comparison of the SPBS and HAMD scores between the two groups before the nursing showed no statistical differences. After the nursing, the two scores were significantly lower in the RG than in the CG, indicating that comprehensive nursing can relieve patients’ self-perceived burdens and negative emotions. A previous study suggests that ICH patients are generally elderly, troubled by depression and poor sleep quality [25]. Here the sleep quality of patients was measured using PSQI. The comparison of the PSQI scores between the two groups before the nursing showed no significant differences. After the nursing, the scores were significantly lower in the RG than in the CG, suggesting that comprehensive nursing can improve sleep quality. ICH patients have weakened performance in daily living and impaired motor functions. Here we used BI to measure the performance in the activities of daily living and FAM to measure the patients’ motor functions. After the nursing, the BI and FAM scores were significantly increased in the RG and they were higher than the scores in the CG, indicating that comprehensive nursing can effectively improve patients’ performance in the activities of daily living and motor functions. We used the GQOL-74 to assess the patients’ quality of life from four dimensions (somatic function, psychological function, social function, and material life) and noted a much better quality of life in the RG than in the CG. According to the hospital review data of patients at 6 months after discharge, only 1 case of dysphagia occurred in the RG, but 2 cases of dysphagia occurred in the CG, along with 1 case of aspiration pneumonia, 2 cases of pressure sores, and 3 cases of falls. The total incidence of complications was lower in the RG than in the CG (2.70% vs. 22.86%). In this study, the nursing satisfaction rate was significantly higher in the RG than in the CG (97.30% vs. 77.14%), indicating that comprehensive nursing is more beneficial and has been unanimously recognized by patients and their families.
This study preliminarily revealed that comprehensive nursing can relieve the negative emotions of ICH patients, enhance their self-management abilities, facilitate their activities of daily living, and improve their sleep quality. However, this study is subject to certain limitations. For example, there are currently diverse nursing models in the clinic, but we only took conventional nursing as a control, making this study less comprehensive. We will include more nursing models in future research to supplement our results and make them more comprehensive.
In summary, comprehensive nursing can relieve the negative emotions of ICH patients, enhance their self-management abilities, facilitate their activities of daily living, reduce their risks of complications, improve their sleep quality, and increase their nursing satisfaction.
Acknowledgements
Scientific Research Project of Inner Mongolia University for Nationalities: Evaluation of the effect of Mongolian medicine special nursing on patients with cerebral hemorrhage on constipation (No. NMDYB17133).
Disclosure of conflict of interest
None.
References
- 1.Frontera JA, Lewin JJ 3rd, Rabinstein AA, Aisiku IP, Alexandrov AW, Cook AM, del Zoppo GJ, Kumar MA, Peerschke EI, Stiefel MF, Teitelbaum JS, Wartenberg KE, Zerfoss CL. Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the neurocritical care society and society of critical care medicine. Neurocrit Care. 2016;24:6–46. doi: 10.1007/s12028-015-0222-x. [DOI] [PubMed] [Google Scholar]
- 2.Qureshi AI, Palesch YY, Barsan WG, Hanley DF, Hsu CY, Martin RL, Moy CS, Silbergleit R, Steiner T, Suarez JI, Toyoda K, Wang Y, Yamamoto H, Yoon BW ATACH-2 Trial Investigators and the Neurological Emergency Treatment Trials Network. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage. N Engl J Med. 2016;375:1033–1043. doi: 10.1056/NEJMoa1603460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsivgoulis G, Zand R, Katsanos AH, Turc G, Nolte CH, Jung S, Cordonnier C, Fiebach JB, Scheitz JF, Klinger-Gratz PP, Oppenheim C, Goyal N, Safouris A, Mattle HP, Alexandrov AW, Schellinger PD, Alexandrov AV. Risk of symptomatic intracerebral hemorrhage after intravenous thrombolysis in patients with acute ischemic stroke and high cerebral microbleed burden: a meta-analysis. JAMA Neurol. 2016;73:675–683. doi: 10.1001/jamaneurol.2016.0292. [DOI] [PubMed] [Google Scholar]
- 4.Boulouis G, Morotti A, Brouwers HB, Charidimou A, Jessel MJ, Auriel E, Pontes-Neto O, Ayres A, Vashkevich A, Schwab KM, Rosand J, Viswanathan A, Gurol ME, Greenberg SM, Goldstein JN. Association between hypodensities detected by computed tomography and hematoma expansion in patients with intracerebral hemorrhage. JAMA Neurol. 2016;73:961–968. doi: 10.1001/jamaneurol.2016.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang F, Hu S, Ding Y, Ju X, Wang L, Lu Q, Wu X. Neutrophil-to-lymphocyte ratio and 30-day mortality in patients with acute intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2016;25:182–187. doi: 10.1016/j.jstrokecerebrovasdis.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 6.Li W, Gao J, Wei S, Wang D. Application values of clinical nursing pathway in patients with acute cerebral hemorrhage. Exp Ther Med. 2016;11:490–494. doi: 10.3892/etm.2015.2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rutherford MA, Pennock JM, Dubowitz LM. Cranial ultrasound and magnetic resonance imaging in hypoxic-ischaemic encephalopathy: a comparison with outcome. Dev Med Child Neurol. 1994;36:813–825. doi: 10.1111/j.1469-8749.1994.tb08191.x. [DOI] [PubMed] [Google Scholar]
- 8.Bjerkreim AT, Thomassen L, Waje-Andreassen U, Selvik HA, Naess H. Hospital readmission after intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2016;25:157–162. doi: 10.1016/j.jstrokecerebrovasdis.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 9.Hong JH, Bang JS, Chung JH, Han MK. Protocol based real-time continuous electroencephalography for detecting vasospasm in subarachnoid hemorrhage. J Korean Neurosurg Soc. 2016;59:154–157. doi: 10.3340/jkns.2016.59.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Szczyglowska M, Piekarska A, Konieczka P, Namiesnik J. Use of brassica plants in the phytoremediation and biofumigation processes. Int J Mol Sci. 2011;12:7760–7771. doi: 10.3390/ijms12117760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walton MM, Barraclough BH, Van Staalduinen SA, Elliott SL. An educational approach to improving healthcare safety and quality. J Evid Based Med. 2009;2:136–142. doi: 10.1111/j.1756-5391.2009.01030.x. [DOI] [PubMed] [Google Scholar]
- 12.Meehan A, Loose C, Bell J, Partridge J, Nelson J, Goates S. Health system quality improvement: impact of prompt nutrition care on patient outcomes and health care costs. J Nurs Care Qual. 2016;31:217–223. doi: 10.1097/NCQ.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 13.Head SJ, Davierwala PM, Serruys PW, Redwood SR, Colombo A, Mack MJ, Morice MC, Holmes DR Jr, Feldman TE, Stahle E, Underwood P, Dawkins KD, Kappetein AP, Mohr FW. Coronary artery bypass grafting vs. percutaneous coronary intervention for patients with three-vessel disease: final five-year follow-up of the SYNTAX trial. Eur Heart J. 2014;35:2821–2830. doi: 10.1093/eurheartj/ehu213. [DOI] [PubMed] [Google Scholar]
- 14.Brusco NK, Taylor NF, Watts JJ, Shields N. Economic evaluation of adult rehabilitation: a systematic review and meta-analysis of randomized controlled trials in a variety of settings. Arch Phys Med Rehabil. 2014;95:94–116. e114. doi: 10.1016/j.apmr.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 15.Loeb M, Carusone SC, Goeree R, Walter SD, Brazil K, Krueger P, Simor A, Moss L, Marrie T. Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006;295:2503–2510. doi: 10.1001/jama.295.21.2503. [DOI] [PubMed] [Google Scholar]
- 16.Yousef KM, Balzer JR, Bender CM, Hoffman LA, Poloyac SM, Ye F, Sherwood PR. Cerebral perfusion pressure and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Am J Crit Care. 2015;24:e65–71. doi: 10.4037/ajcc2015913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christensen MC, Mayer S, Ferran JM. Quality of life after intracerebral hemorrhage: results of the factor seven for acute hemorrhagic stroke (FAST) trial. Stroke. 2009;40:1677–1682. doi: 10.1161/STROKEAHA.108.538967. [DOI] [PubMed] [Google Scholar]
- 18.Muehlschlegel S, Rordorf G, Bodock M, Sims JR. Dantrolene mediates vasorelaxation in cerebral vasoconstriction: a case series. Neurocrit Care. 2009;10:116–121. doi: 10.1007/s12028-008-9132-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hu X, Tao C, Gan Q, Zheng J, Li H, You C. Oxidative stress in intracerebral hemorrhage: sources, mechanisms, and therapeutic targets. Oxid Med Cell Longev. 2016;2016:3215391. doi: 10.1155/2016/3215391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Francoeur CL, Mayer SA. Management of delayed cerebral ischemia after subarachnoid hemorrhage. Crit Care. 2016;20:277. doi: 10.1186/s13054-016-1447-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nielsen PB, Larsen TB, Skjoth F, Lip GY. Outcomes associated with resuming warfarin treatment after hemorrhagic stroke or traumatic intracranial hemorrhage in patients with atrial fibrillation. JAMA Intern Med. 2017;177:563–570. doi: 10.1001/jamainternmed.2016.9369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blume KG, Forman SJ, O’Donnell MR, Doroshow JH, Krance RA, Nademanee AP, Snyder DS, Schmidt GM, Fahey JL, Metter GE, et al. Total body irradiation and high-dose etoposide: a new preparatory regimen for bone marrow transplantation in patients with advanced hematologic malignancies. Blood. 1987;69:1015–1020. [PubMed] [Google Scholar]
- 23.Chagolla B, Bingham D, Wilson B, Scheich B. Perceptions of safety improvement among clinicians before and after participation in a multistate postpartum hemorrhage project. J Obstet Gynecol Neonatal Nurs. 2018;47:698–706. doi: 10.1016/j.jogn.2018.04.140. [DOI] [PubMed] [Google Scholar]
- 24.McFadden KL, Stock GN, Gowen CR 3rd. Leadership, safety climate, and continuous quality improvement: impact on process quality and patient safety. Health Care Manage Rev. 2015;40:24–34. doi: 10.1097/HMR.0000000000000006. [DOI] [PubMed] [Google Scholar]
- 25.Jeon H, Sohn MK, Jeon M, Jee S. Clinical characteristics of sleep-disordered breathing in subacute phase of stroke. Ann Rehabil Med. 2017;41:556–563. doi: 10.5535/arm.2017.41.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]


