Abstract
Objective: To study the application effect of comprehensive nursing combined with early activityactivity in patients with ventilator-associated pneumonia (VAP) and its influence on blood gas indexes of patients. Methods: 100 patients with VAP admitted to our hospital from February 2018 to November 2019 were randomly selected and divided into control group and experimental group, with 50 patients in each group. Patients in the control group received routine nursing intervention with early activity, and patients in the experimental group received comprehensive nursing intervention with early activity. The incidence of adverse reactions, length of hospital stay, blood gas index, nursing efficiency, and nursing satisfaction were compared between the two groups. Results: Compared with the control group, the incidence of adverse reactions, mental status scale in non-psychiatric settings (MSSNS) score and length of hospital stay in the experimental group were noticeably lower (P<0.05), while the partial arterial oxygen pressure (PaO2) and saturation of blood oxygen (SaO2) in the experimental group were higher (P<0.05), and the arterial partial pressure carbon dioxide (PaCO2) in the experimental group was significantly lower (P<0.05). Nursing efficiency in the experimental group was significantly higher than the control group (P<0.05). Experimental group exhibited higher satisfaction rate compared to the control group (P<0.05). Conclusion: Comprehensive nursing intervention combined with early activityactivity can significantly reduce the incidence of adverse reactions and hospital stay, improve the blood gas indicators of patients, and promote nursing efficiency.
Keywords: Comprehensive nursing, early activityactivity, ventilator-associated pneumonia, blood gas index, nursing effect
Introduction
Ventilator-associated pneumonia (VAP) is a disease in which infectious pneumonia occurs because of ventilators applied for mechanical ventilation. There is highly contaminated condensate in the ventilator, and when it flows into the human body, severe infectious pneumonia will occur. The ventilator and humidifier pipes also need to be replaced regularly, which may also induce serious pneumonia if timely replacement is not performed [1-3]. Blood gas indicators are commonly used clinically to determine the physical dissolved oxygen and carbon dioxide tension of the patient’s blood, including arterial oxygen partial pressure, arterial carbon dioxide partial pressure and arterial oxygen saturation [4-6]. Pneumonia is a common respiratory disease, andexhibits symptoms such as dyspnea, aggravated wheezing, cough and sputum, which can lead to death. For this, the care of patients with VAP is one of the key links in the treatment. Comprehensive nursing intervention refers to the comprehensive care applied for patients’ body and mind, giving patients a positive and good mindset [4,5,7]. During the treatment of pneumonia patients, appropriate activity and breathing exercises are required. Comprehensive nursing interventions combined with early activity are reported to alleviate the disease manifestations of pneumonia patients. In order to study the application of comprehensive nursing and early activity in patients with VAP, this paper takes patients with VAP as the research object, and provides them with different nursing care, and analyzes the hospitalization time, blood gas indicators, adverse response, and nursing efficacy.
Materials and methods
General information
We did a randomized controlled trial on 100 VAP patients admitted to our hospital from February 2018 to November 2019 who were enrolled into a control group and an experimental group, 50 each. The patients in the experimental group were 31-56 years old, and the patients in the control group were 33-60 years old.
Inclusion/exclusion criteria
Inclusion criteria
① In line with the clinical manifestations of VAP; ② Patient aged ≥18 years old; ③ No comorbid organic diseases; ④ No history of drug allergy, drug abuse, or bad habits; ⑤ This study is registered in our hospital ethics committee, and the patients or family members voluntarily participated in the study and signed an informed consent form.
Exclusion criteria
① With coagulopathy, or is taking anticoagulant drugs; ② With mental disorder and cannot cooperate with the research; ③ With serious cerebrovascular disease occurring recently.
Methods
The control group received routine care combined with early activity care. Nurses regularly check the patient’s vital signs and pay attention to whether the patient has abnormalities. If the patient shows an abnormal increase in body temperature, unexplained decrease in blood pressure, difficulty breathing, or decreased blood oxygen saturation, nurses should inform the attending doctor in time and implement relevant treatment. Nurses should formulate appropriate exercise goals, and ensure a certain amount of exercise every day in particular walking if allowed. Nursing staff need to instruct patients to perform breathing exercises, mainly abdominal breathing, with interesting activity such as blowing balloons.
The experimental group performed comprehensive nursing care with early activity nursing. Psychological counseling was done for patients, to strengthen communication with patients or their families, and prevent patients from experiencing negative emotions such as depression and anxiety. We should popularize health education, so that patients can understand the treatment process of VAP and the existing treatment methods, and eliminate patients’ fear. We would conduct regular rounds and routine disinfection of wards.
Observation indicators
The outcome measures include incidence of adverse reactions, length of hospital stay, blood gas indicators, mental status scale in non-psychiatric settings (MSSNS), and nursing effectiveness.
Blood gas indicators mainly include arterial oxygen partial pressure (PaO2), partial pressure of arterial carbon dioxide (PaCO2), and arterial oxygen saturation (SaO2) [8-10].
The MSSNS score is graded into <60 points, 60-70 points and >70 points, which are defined as normal, mildly abnormal, and abnormal respectively.
Effectiveness of nursing care is appraised as three ratings. The patient has no other adverse reactions, and the symptoms of VAP basically disappear is considered as markedly effective; the patient has no other adverse reactions, and the symptoms of VAP disappeared obviously as effective; the symptoms of VAP do not disappear or aggravate as ineffective.
A self-made scale was used to conduct a nursing satisfaction survey on the quality of patient care, and the nursing satisfaction rate between the two groups was compared. The nursing satisfaction rate = [(satisfied + generally satisfied) number of cases/total number of cases] × 100%.
Statistical analysis
Mean ± SD was calculated for numeric variables. Frequency and rate were used to describe categorical data. The independent t-test and X2 test was used to compare 2 independent samples. All data were analyzed using IBM SPSS Statistics for Windows v.20 (IBM Corp., Armonk, NY), and all graphics were mapped using GraphPad Prism 7 (GraphPad Software, San Diego, USA). A P value of <0.05 was considered significant.
Results
Comparison of general data
The baseline information did not differ significantly between the two groups (P>0.05). See Table 1.
Table 1.
General data comparison (x̅ ± s)
| Group | Experimental group | Control group | t/X2 | P |
|---|---|---|---|---|
| Gender (male/female) | 23/27 | 25/25 | 0.16 | 0.69 |
| Age (years) | 45.67±3.38 | 45.29±3.61 | 0.54 | 0.59 |
| Height (cm) | 166.23±8.06 | 166.50±8.17 | 0.17 | 0.87 |
| Weight (kg) | 70.22±5.50 | 70.66±5.29 | 0.41 | 0.68 |
| History of smoking (years) | 6.64±1.20 | 6.57±1.48 | 0.26 | 0.80 |
| History of drinking (years) | 10.24±2.00 | 10.55±2.61 | 0.67 | 0.51 |
| Hypertension (n) | 5 | 7 | 0.38 | 0.54 |
| Diabetes (n) | 10 | 9 | 0.07 | 0.80 |
| Hyperlipidemia (n) | 6 | 4 | 0.44 | 0.51 |
| Cause of hospitalization | ||||
| coronary heart disease | 17 | 20 | 0.39 | 0.53 |
| severe pneumonia | 6 | 5 | 0.10 | 0.75 |
| shock | 17 | 16 | 0.05 | 0.83 |
| organ transplantation | 10 | 9 | 0.07 | 0.80 |
Incidence of adverse reactions
The adverse reactions during the nursing process of the treatment involved dyspnea, fever, and moist rales in the lungs. We examined the adverse reaction rate and found that the experimental group exhibited a significantly lower rate (10% vs 34%) (P<0.05, Table 2).
Table 2.
Comparison of the incidence of adverse reactions
| Groups | Difficulty breathing | Fever | Moist rale | Total incidence rate (%) |
|---|---|---|---|---|
| Experimental group | 2 | 0 | 3 | 10% |
| Control group | 6 | 2 | 9 | 34% |
| X2 | 8.39 | |||
| P | 0.004 |
Hospitalization time
We counted the hospitalization time of the two groups and the results demonstrated that the hospitalization time of the experimental group was shorter as compared to the control group (P<0.05). See Figure 1A.
Figure 1.
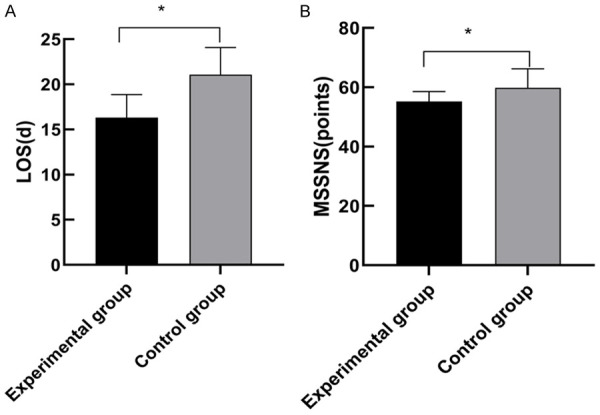
Comparison of hospital stays and MSSNS scores between the two groups. Note: A. The abscissa represents the experimental group and the control group from left to right, and the ordinate represents the hospital stay (LOS, d). *Indicates a comparison of hospital stay between the experimental group (16.33±2.54) d and the control group (21.08±3.00) d was statistically significant (t=8.54, P<0.05). B. The abscissa represents the experimental group and the control group from left to right, and the ordinate represents the MSSNS score (points). *Indicates the comparison of MSSNS score between the experimental group (55.21±3.37) and the control group (59.84±6.39) was statistically significant (t=4.53, P<0.05).
Blood gas indexes
We compared the blood gas index of the two groups, and it showed that PaO2 and SaO2 of the experimental group were notably higher, while the PaCO2 was significantly lower than that of the control group (P<0.05). See Table 3.
Table 3.
Comparison of blood gas indexes between the two groups (x̅ ± s)
| Group | PaO2 (mmHg) | PaCO2 (mmHg) | SaO2 (%) |
|---|---|---|---|
| Experimental group | 91.42±1.05 | 37.48±1.09 | 96.89±1.88 |
| Control group | 84.03±1.22 | 42.54±1.55 | 90.11±1.43 |
| t | 32.46 | 18.88 | 20.30 |
| P | <0.001 | <0.001 | <0.001 |
MSSNS scores
Regarding MSSNS score, the experimental group who applied comprehensive nursing intervention and early activity showed a lower score than that of the control group who underwent conventional nursing (P<0.05). See Figure 1B.
Nursing effectiveness
When considering effectiveness of nursing care, the effectiveness in the experimental group was significantly higher than that of the control group (P<0.05, Table 4).
Table 4.
Comparison of the effectiveness of nursing care between the two groups
| Group | Markedly effective | Effective | Ineffective | Total effective rate (%) |
|---|---|---|---|---|
| Experimental group | 35 | 9 | 6 | 88% |
| Control group | 14 | 21 | 15 | 60% |
| X2 | 4.88 | |||
| P | 0.03 |
Comparison of nursing satisfaction rate
The nursing satisfaction rate of experimental group was significantly higher than that of the control group (P<0.05, Table 5).
Table 5.
Comparison of the satisfaction rate between the two groups
| Groups | satisfied | generally satisfied | dissatisfied | total satisfaction rate (%) |
|---|---|---|---|---|
| Experimental group | 37 | 8 | 5 | 90% |
| Control group | 20 | 14 | 16 | 68% |
| X2 | 7.294 | |||
| P | 0.007 |
Discussion
A variety of instruments are needed in most patients in the intensive care unit to maintain their lives, of which the ventilator is a common breathing assistance device. When patients cannot breathe independently, they use the ventilator to assist in breathing. When using a ventilator for mechanical ventilation, the patient must remain supine, and ensure that there are no secretions or residues in the oral cavity or respiratory tract. After cleaning the patient’s mouth, the ventilator mask is placed on the patient’s mouth and nose to assist breathing [11-13]. Mechanically ventilated patients are prone to pulmonary infection and infectious pneumonia from 48 hours after ventilation to 48 hours after completion of ventilation, which is called VAP. Timely treatment should be provided after VAP, and if not, it may be life-threatening [14,15]. Although the common nursing mode is frequently applied in VAP, the outcome is not ideal, and the nursing efficiency is relatively low. As a consequence, seeking a more effective nursing method for VAP patients is an urgent problem. Comprehensive nursing intervention refers to the comprehensive care provided by nursing staff to patients, including physical and mental nursing, health knowledge education, and living habits training. Some studies have reported that comprehensive nursing intervention combined with early activity can significantly improve the onset of VAP in patients [16]. In this paper, we chose VAP patients and performed different nursing methods, with a purpose of analyzing the application effect of comprehensive nursing intervention and early activity in VAP.
The adverse reactions in the nursing process of VAP patients include dyspnea, and fever. We examined the incidence of adverse reactions during the nursing process and found that the experimental group exhibited a lower rate (P<0.05). This shows that comprehensive nursing intervention combined with early activity can significantly reduce the adverse reactions in the nursing process of patients with VAP and reduce the suffering of patients. In addition, we compared hospitalization time and MSSNS mental status scores of the two groups of patients who underwent different nursing modes, and the results revealed that those indexes were significantly lower in the experimental group (P<0.05). Additionally, the experimental group showed a higher satisfaction rate compared to the control group, indicating that the experimental group patients can maintain relatively positive mindset during the nursing process, and further reduce the length of hospital stay.
If the PaCO2 is too high, respiratory acidosis may occur, and the pH of the breath will be unbalanced, which is extremely life-threatening to the patient. In this study, the PaO2 and SaO2 of the experimental group were significantly higher than those of the control group, while the PaCO2 was lower. To a certain extent, this shows that comprehensive nursing intervention combined with early activity can significantly stabilize the patient’s respiratory pH and keep the patient’s blood gas indicators in a relatively normal range. The above conclusion is in line with the results by Baowei [17], in which he proposed that the PaCO2 in patients with VAP in ICU under comprehensive care mode was significantly lower than that in patients with VAP under conventional care mode. This fully reinforces the scientific nature of the results of this study. A limitation was that it failed to assess the mobility, cardiopulmonary function, and quality of life of patients with VAP after discharge. In the future, the sample size will be expanded to further study the long-term quality of life and psychological conditions of patients.
In summary, comprehensive nursing intervention combined with early activity can significantly reduce the incidence of adverse reactions and length of stay in the hospital, improve patient blood gas indicators, and improve nursing efficiency. Therefore, comprehensive nursing intervention combined with early activity has high application value in patients with VAP, and is worthy of clinical promotion and application.
Disclosure of conflict of interest
None.
References
- 1.Alonso B, Fernández-Barat L, Di Domenico EG, Marín M, Cercenado E, Merino I, de Pablos M, Muñoz P, Guembe M. Characterization of the virulence of pseudomonas aeruginosa strains causing ventilator-associated pneumonia. BMC Infec Dis. 2020;20:909. doi: 10.1186/s12879-020-05534-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hussain K, Salat MS, Ambreen G, Mughal A, Idrees S, Sohail M, Iqbal J. Intravenous vs intravenous plus aerosolized colistin for treatment of ventilator-associated pneumonia - a matched case-control study in neonates. Expert Opin Drug Saf. 2020;19:1641–1649. doi: 10.1080/14740338.2020.1819980. [DOI] [PubMed] [Google Scholar]
- 3.Hou SY, Wu D, Feng XH. Polymyxin monotherapy versus polymyxin-based combination therapy against carbapenem-resistant klebsiella pneumoniae: a systematic review and meta-analysis. J Glob Antimicrob Resist. 2020;23:197–202. doi: 10.1016/j.jgar.2020.08.024. [DOI] [PubMed] [Google Scholar]
- 4.Jansson MM, Syrjälä HP, Ala-Kokko TI. Corrigendum to “association of nurse staffing and nursing workload with ventilator-associated pneumonia and mortality: a prospective, single-center cohort study” [journal of hospital infection 101 (2019) 257-263] . J Hosp Infect. 2020;106:839–840. doi: 10.1016/j.jhin.2020.10.009. [DOI] [PubMed] [Google Scholar]
- 5.Vieira PC, de Oliveira RB, da Silva Mendonça TM. Should oral chlorhexidine remain in ventilator-associated pneumonia prevention bundles? Med Intensiva. 2020 doi: 10.1016/j.medin.2020.09.009. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Elhag M, Alaagib RM, Ahmed NM, Abubaker M, Haroun EM, Abd Albagi SO, Hassan MA. Design of epitope-based peptide vaccine against pseudomonas aeruginosa fructose bisphosphate aldolase protein using immunoinformatics. J Immunol Res. 2020;2020:9475058. doi: 10.1155/2020/9475058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang HC, Liao CC, Chu SM, Lai MY, Huang HR, Chiang MC, Fu RH, Hsu JF, Tsai MH. Impacts of multidrug-resistant pathogens and inappropriate initial antibiotic therapy on the outcomes of neonates with ventilator-associated pneumonia. Antibiotics (Basel) 2020;9:760. doi: 10.3390/antibiotics9110760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collins T, Plowright C, Gibson V, Stayt L, Clarke S, Caisley J, Watkins CH, Hodges E, Leaver G, Leyland S, McCready P, Millin S, Platten J, Scallon M, Tipene P, Wilcox G. British association of critical care nurses: evidence-based consensus paper for oral care within adult critical care units. Nurs Crit Care. 2020 doi: 10.1111/nicc.12570. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Barbeta E, Ceccato A, Artigas A, Ferrer M, Fernández L, López R, Bueno L, Motos A, Bassi GL, Mellado R, Ferrando C, Palomeque AC, Panigada M, Gabarrús A, de Mendoza D, Torres A. Characteristics and outcomes in patients with ventilator-associated pneumonia who do or do not develop acute respiratory distress syndrome. An observational study. J Clin Med. 2020;9:3508. doi: 10.3390/jcm9113508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yin MY, Liu MR. Effect of chronic obstructive pulmonary disease combined with ventilator-associated pneumonia on patient outcomes: a systematic review and meta-analysis. Exp Ther Med. 2020;20:273. doi: 10.3892/etm.2020.9403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Massart N, Dupin C, Mari A, Debarre M, Barbarot N, Legay F, Magalhaes E, Rieul G, Fillatre P. Clinician involvement for ventilator-associated pneumonia surveillance resulted in higher than expected incidence rate reported with implication for attributable mortality. Infect Dis (Lond) 2021;53:154–157. doi: 10.1080/23744235.2020.1839129. [DOI] [PubMed] [Google Scholar]
- 12.Howatt M, Klompas M, Kalil AC, Metersky ML, Muscedere J. Carbapenem antibiotics for the empiric treatment of nosocomial pneumonia: a systematic review and meta-analysis. Chest. 2021;159:1041–1054. doi: 10.1016/j.chest.2020.10.039. [DOI] [PubMed] [Google Scholar]
- 13.Carraway JS, Carraway MW 2nd, Truelove CA Jr. Nursing implementation of a validated agitation and sedation scale: an evaluation of its outcomes on ventilator days and ICU length of stay. Appl Nurs Res. 2021;57:151372. doi: 10.1016/j.apnr.2020.151372. [DOI] [PubMed] [Google Scholar]
- 14.Coelembier C, Venet F, Demaret J, Viel S, Lehot JJ, Dailler F, Monneret G, Lukaszewicz AC. Impact of ventilator-associated pneumonia on cerebrospinal fluid inflammation during immunosuppression after subarachnoid hemorrhage: a pilot study. J Neurosurg Anesthesiol. 2020 doi: 10.1097/ANA.0000000000000732. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Alessandri F, Pugliese F, Angeletti S, Ciccozzi M, Russo A, Mastroianni CM, d’Ettorre G, Venditti M, Ceccarelli G. Procalcitonin in the assessment of ventilator associated pneumonia: a systematic review. Adv Exp Med Biol. 2020;1323:103–114. doi: 10.1007/5584_2020_591. [DOI] [PubMed] [Google Scholar]
- 16.El Fawy DM, Ibrahim AY, Abdulmageed AMM, El Seddek EABakr. A comparative study between effect of combined intravenous and nebulized amikacin versus intravenous amikacin alone in mechanically ventilated patients with ventilator-associated pneumonia (VAP) Ain-Shams J Anesth. 2020:12. [Google Scholar]
- 17.Mo BW. Influence of comprehensive nursing care on occurrence of ventilators associated pneumonia in ICU. Continuing Medical Education. 2020;34:117–118. [Google Scholar]


