Abstract
Objective: To investigate the implementation of evidence-based nursing model (EBNM) in health education and its influences on the therapeutic effects, degrees of pain, adverse emotions, postoperative complications and degrees of cognition of health knowledge of elderly fracture patients. Methods: A total of 75 elderly patients with hip fractures receiving surgery in the First People’s Hospital of Chuzhou from January 2019 to June 2020 were selected as the study subjects, and were divided into control group (n = 37) and experimental group (n = 38) in accordance with random number table method. The control group received conventional health education, while the experimental group received health education intervention based on EBNM. The changes in therapeutic effects, degrees of pain, complications, adverse emotional reactions and degrees of cognition of health knowledge were compared between the two groups. Results: After intervention, the hospital stay and fracture healing time in the experimental group were shorter than those in the control group (P < 0.05). Compared with those before intervention, the scores of Berg balance scale (BBS) and Fugl-Meyer assessment (FMA) were elevated, while numerical rating scale (NRS) score was decreased remarkably after intervention. After intervention, the experimental group showed remarkably higher scores of BBS and FMA and degrees of cognition of health knowledge and significantly lower scores of NRS and the overall risk of postoperative complications than the control group (P < 0.05). The scores of self-rating depression scale (SDS) and self-rating anxiety scale (SAS) in the two groups decreased after intervention (P < 0.05). Conclusion: Health education intervention based on EBNM can effectively improve patients’ understanding of the fracture, quality of prognosis, fracture healing time, the occurrence of adverse emotions and the incidence rate of complications of elderly fracture patients.
Keywords: Fracture, health education, evidence-based nursing
Introduction
The external forces can easily cause fractures of the elderly who usually have brittle bones and are most susceptible to hip fractures [1,2]. With the rise in age, there is a fall in The coordination and reaction abilities often decrease in the elderly, who are very likely to experience hip fractures when fall off. The conservative treatment and surgical options are primarily implemented to treat hip fractures [3]. Relevant statistics show that conservative treatment exhibits a high mortality rate. If there is no surgical contraindication, surgery should be performed as early as possible [4]. However, older adults suffering from underlying health conditions are easily susceptible to postoperative complications. In addition, degree of pain can affect the emotions, self-care abilities and quality of life, thereby affecting the prognosis [5,6]. Previous studies have demonstrated that proper health education and nursing interventions can improve the psychological state, quality of life, and the prognosis of elderly fracture patients [7].
Evidence-based nursing (EBN) is an important branch of evidence-based medicine. In 1991, Alba et al. first proposed the concept of EBN, which was continuously improved, promoted and extensively implemented by nursing specialists [8]. Based on EBN integrating internal and external evidence, nurses’ experience and patients’ actual conditions, the optimal nursing care plan can be formulated [9]. A study indicates that EBN can make up for the shortcomings of conventional nursing, elevate the ability of nurses, provide an excellent nursing care for patients, and improve the prognosis of patients [10].
The objective of this study is to analyze the nursing effects of EBN on elderly fracture patients through implementing EBNM in with health education, so as to provide a theoretical basis for the improvement of the prognosis, self-care abilities and quality of life of elderly fracture patients.
Materials and methods
General data
A total of 75 elderly patients with hip fractures admitted in the First People’s Hospital of Chuzhou from January 2019 to June 2020 were selected as the study subjects, including 43 males and 32 females.
Inclusion criteria: patients aged ≥ 65 years; patients who could walk independently before fractures; patients who were clinically diagnosed with hip fractures and required surgical treatment.
Exclusion criteria: aged < 65 years; unable to walk independently before fractures; pathological fractures; ASA Classifications: Class IV or V.
The 75 subjects were divided into a control group (n = 37) and an experimental group (n = 38) by random number table method. The control group included 20 males and 17 females, with a mean age of (74.50 ± 5.56) years, while the experimental group included 23 males and 15 females, with a mean age of (76.21 ± 5.87) years. There was no significant difference in the general data (e.g., gender, age and weight) between the two groups (P > 0.05), and the general data were comparable.
The personal files of 75 patients enrolled were established, their information was registered, the informed consent forms were signed, and they voluntarily participated in this study. This study has been reviewed and approved by the Ethics Committee of The First People’s Hospital of Chuzhou.
Intervention methods
The two groups received surgery with neuraxial anesthesia.
The control group received conventional nursing combined with conventional health education. Publicity and education were performed at admission. The patients were instructed to conduct preoperative preparations, and the guidance on diet and medication was provided. Nursing manuals were distributed to the patients at the time of discharge.
The experimental group received conventional nursing combined with health education based on EBNM. Orthopedic nurses learned the knowledge associated with evidence-based medicine and EBN, and the head nurse and the director of orthopedics were responsible for the assessments. A professional EBN group was composed of orthopedic nurses who passed the assessments.
Collection of questions
The questionnaire was prepared, and the questions in the questionnaire included knowledge associated with hip fractures, postoperative psychological state, degrees of pain, diet, and functional exercise. One day after surgery, the patients were given questionnaires, and the questionnaires were collected immediately after being filled out.
The questionnaire results were collected, and the potential issues in daily nursing care were comprehensively analyzed based on patient admission assessment sheet. The major issues in the experimental group were summarized, namely, lack of relevant theoretical knowledge and effective self-care abilities after discharge, strong postoperative pain, poor emotions caused by inability to walk, and resistance to functional exercise.
Acquisition of evidence
Based on the issues of patients, PubMed, Embase, CBM and related books were consulted, and the health education methods for the collected issues were understood to work out specific health education plans.
Health education
Health education was conducted through distribution of brochures, lectures, WeChat official account and video teaching. The specific educational contents included the following aspects:
Theoretical publicity
The causes and theoretical knowledge of osteoporosis and hip fractures were explained, the surgical principle and method were informed, and the poor eating habits (e.g., reluctance to drink milk and have a vegetarian diet) were corrected. The patients were asked to increase the intake of vitamin D, have a balance portion of vegetables and meat, avoid excessive exercise, and exercise caution to prevent falling off.
Psychological counseling
The fracture patients experienced a strong pain and were unable to move freely, easily leading to emotional fluctuations. Older adults were concerned about a poor recovery after surgery, which may affect their self-care abilities and be left unattended in the future. Nurses paid attention to the emotional changes of the patients, and regularly organized the patients to attend the exchange meetings where the cured patients shared their therapeutic experiences to boost the confidence of other patients in treatment. Meanwhile, nurses vigorously communicated with the patients’ families, so that they could provide the patients with more care and eliminate the hidden worries of the patients.
Dietary guidance
The patients were instructed to have a regulated diet in their daily life, and have more foods with high calcium content (e.g., milk, beans, lean meat, animal liver, and marine fish). The patients were denied access to foods with a high content of oxalic and phytic acid (e.g., carbonated drinks, spinach, and bamboo shoots), so as to prevent affecting calcium absorption.
Guidance on functional exercise
During the recovery period of anesthesia, quadriceps femoris exercise was conducted, hip stretching exercise was performed within 72 h after surgery, and weight training was performed from 5 d after surgery. The patients and their families were informed the exercise time could be adjusted based on the patient’s physical conditions, so as to alternate work with rest and prevent secondary strain injury during exercise.
Pain management
The patients were instructed to play music, watch movies, and listen to operas in their daily life, so as to improve adverse emotions, distract the attention, and reduce degrees of pain of the patients. The patients’ families were informed of massage methods, so as to provide the patients with whole body and local massage, thereby alleviating postoperative pain and avoiding discomfort caused by long-term lying.
Nursing methods after discharge
The self-care methods and methods of care by others were explained to the patients and their families after discharge, and the patients were asked to exercise properly and conduct follow-up visits on schedule.
Observational indexes and assessment criteria
Therapeutic effects
The hospital stay in the two groups was recorded. After discharge, X-ray reexamination was performed regularly every month to check the healing condition at the fracture site.
The balance abilities in the two groups were assessed by Berg Balance Scale (BBS) before intervention and 3 months after intervention. BBS comprises 14 items. A scoring system of 0-4 point(s) was adopted. A higher score indicated a better balance ability [11]. The patient’s motion coordination abilities were assessed by Fungl-Meyer assessment (FMA) scale. FMA scale consists of 17 items. A scoring system of 0-2 points was adopted. A higher score indicated a better motion coordination ability [12].
Degrees of pain
Numerical rating scale (NRS) was used to score patients’ degrees of pain before and after intervention. A scoring system of 0-10 point(s) was adopted. 0 point indicated painless, and 10 points indicated severe pain. A higher degree of pain indicated a higher score of NRS scale.
Complications
The postoperative complications (e.g., pressure sore, phlebothrombosis, nerve injury and pulmonary infection) were recorded in the two groups [13]. A lower incidence rate of postoperative complications indicated a better prognosis, exhibiting that the surgery was successfully completed and the perioperative nursing care was effective.
Adverse emotional reactions
Before and after intervention, the anxiety (Self-Rating Anxiety Scale, SAS) and depression (Self Rating Depression Scale, SDS) in the two groups were scored using Hamilton Anxiety Scale (HAMA) and Hamilton Depression Scale (HAMD) to assess the emotions of the patients. A higher score indicated a higher degree of anxiety and depression.
Degrees of recognition of health knowledge
According to Facts on Osteoporosis Quiz (FOOQ), a questionnaire on health knowledge of fracture was prepared, and the patients’ degrees of cognition of health knowledge were investigated. The questionnaire comprises disease knowledge, nursing precautions and rehabilitation operations. Based on the degrees of cognition of health knowledge, a scoring system of 0-4 points was adopted. There was a total score of 20 points for each item. A higher score indicated a higher degree of cognition of health knowledge [14].
Statistical method
SPSS 22.0 was adopted for statistical analysis. The measurement data were expressed using x̅ ± s. The comparison between groups was detected using the independent sample t test, and the comparison within groups was detected using the paired sample t test. The enumeration data were expressed using %, and detected using χ2 test. P < 0.05 indicated a statistically significant difference.
Results
Comparison of general clinical indexes between the two groups
The comparison suggested that there was no statistical significance in general clinical indexes (e.g., gender, age, weight, time of education, and course of disease) between the control group and the experimental group (P > 0.05), but the indexes were comparable (Table 1).
Table 1.
Comparison of general clinical indexes between the two groups (x̅ ± s)/[n (%)]
| General clinical data | Control group (n = 37) | Experimental group (n = 38) | t/X2 | P | |
|---|---|---|---|---|---|
| Gender | M | 20 | 23 | -0.200 | 0.874 |
| F | 17 | 15 | |||
| Mean age (years) | 74.50 ± 5.56 | 76.21 ± 5.87 | -1.089 | 0.296 | |
| Mean weight (kg) | 58.93 ± 6.90 | 60.71 ± 6.83 | -0.622 | 0.544 | |
| Time of education (years) | 10.39 ± 2.36 | 1.43 ± 2.17 | -0.880 | 0.379 | |
| BMI | 14.85 ± 2.37 | 15.42 ± 1.75 | -1.838 | 0.066 | |
| Course of disease | 2.53 ± 0.74 | 2.35 ± 0.64 | 0.792 | 0.276 | |
Analysis of changes in therapeutic effects before and after intervention
The comparison revealed that the hospital stay and fracture healing time in the experimental group were shorter than those in the control group (P < 0.05) (Table 2). The health education intervention based on EBNM was conducive to shortening the hospital stay of fracture patients and expediting the fracture healing.
Table 2.
Comparison of fracture healing time and hospital stay between the two groups (d, x̅ ± s)
| Control group | Experimental group | t/X2 | P | |
|---|---|---|---|---|
| Fracture healing time | 136.29 ± 11.35 | 98.93 ± 14.03 | 7.448 | 0.000 |
| Hospital stay | 12.07 ± 2.16 | 9.29 ± 1.27 | 4.358 | 0.001 |
The balance abilities and motion coordination abilities in the two groups were scored using BBS and FMA scale, respectively. There was no remarkable difference in the scores of BBS and FMA scale between the two groups before intervention (P > 0.05). 3 months after intervention, the scores of BBS and FMA scale in the two groups increased significantly, and the scores of BBS and FMA scale in the experimental group were higher than those in the control group (P < 0.05) (Figure 1). This exhibited that health education intervention based on EBNM could effectively improve the balance abilities and motion coordination abilities of the patients.
Figure 1.

Analysis of changes in the scores of BBS and FMA in the two groups before and after intervention. Note: # indicates the comparison before and after intervention (P < 0.05), * indicates the comparison between groups after intervention (P < 0.05).
Analysis of changes in degrees of pain before and after intervention
Before and after intervention, the degrees of pain in the two groups were assessed using NRS. Before intervention, there was no marked difference in NRS scores between the two groups (P > 0.05). After intervention, the NRS scores in the two groups were remarkably reduced, and the NRS scores in the experimental group were lower than those in the control group (P < 0.05) (Figure 2). This revealed that health education intervention based on EBNM could effectively reduce the degrees of pain of the patients.
Figure 2.
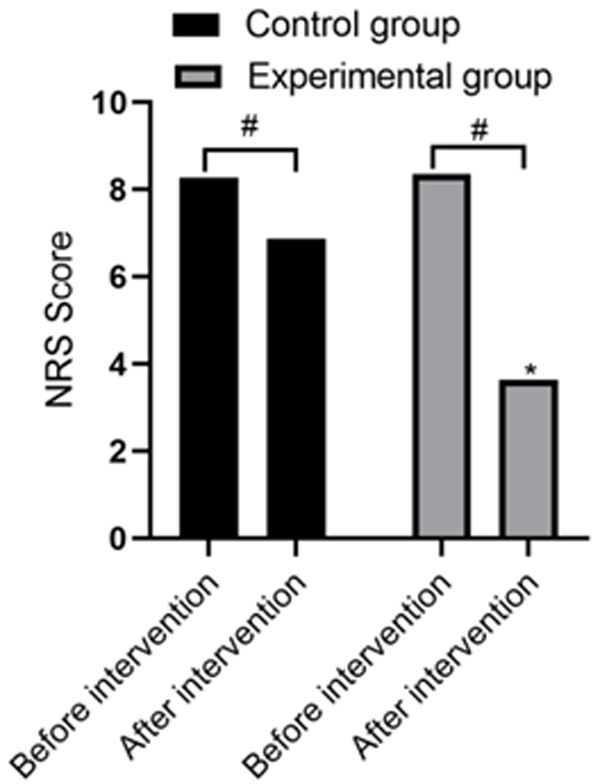
Analysis of changes in NRS scores in the two groups before and after intervention. Note: # indicates the comparison before and after intervention (P < 0.05), * indicates the comparison between groups after intervention (P < 0.05).
Incidence rate of complications after intervention
After intervention, the incidence rates of related complications (e.g., pressure sore, phlebothrombosis, nerve injury and pulmonary infection) in the experimental group were lower than those in the control group, and the overall incidence rate (7.89%) of complications in the experimental group was lower than that (35.14%) in the control group (P < 0.05) (Table 3). This indicated that the health education intervention based on EBNM led to a low risk of postoperative complications and a good prognosis.
Table 3.
Comparison of incidence of complications between the two groups after intervention [n (%)]
| Complications | Control group (n = 37) | Experimental group (n = 38) | t/X2 | P |
|---|---|---|---|---|
| Pressure of score | 4 (10.81) | 1 (2.63) | ||
| Venous thrombosis | 3 (8.11) | 0 (0) | ||
| Nerve injury | 3 (8.11) | 1 (2.63) | ||
| Pulmonary infection | 3 (8.11) | 1 (2.63) | ||
| Overall | 13 (35.14) | 3 (7.89) | 8.289 | 0.004 |
Analysis of changes of adverse emotions before and after intervention
The anxiety and depression in the two groups were scored by HAMA and SAS and HAMD and SDS, respectively. Before intervention, there was no remarkable difference in the scores between the two groups (P > 0.05). 3 months after intervention, the scores of SAS and SDS in the two groups decreased significantly, and the scores of SAS and SDS in the experimental group were lower than those in the control group (P < 0.05) (Figure 3). This demonstrated that health education intervention based on EBNM could effectively improve the adverse emotions of the patients.
Figure 3.

Analysis of changes in the scores of SAS and SDS in the two groups before and after intervention. Note: # indicates the comparison before and after intervention (P < 0.05), * indicates the comparison between groups after intervention (P < 0.05).
Analysis of changes in degrees of cognition of health knowledge before and after intervention
The degrees of cognition of health knowledge in the two groups were assessed using the questionnaire on health knowledge of fracture. Before intervention, there was no marked difference in the scores between the two groups (P > 0.05). 3 months after intervention, the scores of disease knowledge, nursing precautions and rehabilitation operations in the two groups increased remarkably, and the scores in the experimental group were higher than those in the control group (P < 0.05) (Figure 4).
Figure 4.

Analysis of changes in the scores of degrees of cognition of health knowledge in the two groups after intervention. Note: # indicates the comparison before and after intervention (P < 0.05), * indicates the comparison between groups after intervention (P < 0.05).
Discussion
As population ages, there is a rising number of older adults, and there is a year-on-year increase in the number of hip fracture patients. The epidemiological investigation of hip fractures reveals that 50% of hip fracture patients globally are in Asia, and the number of the patients will hit 6.2 million in 2050 [15]. Elderly patients with hip fractures have multiple complications and a poor prognosis, with a mortality rate of 30% within one year. The patients who survive have a disability rate of 50% [16,17]. Recently, new technologies and methods have been implemented to treat hip fractures. However, there is a high mortality rate after surgery, and some even regard hip fractures as “the last fracture in older adults” [18]. Early patients with hip fractures produce negative emotions (e.g., fear and anxiety). The early patients who fear falling dare not to move and are reluctant to conduct rehabilitation exercises, which is not conducive to the recovery of elderly patients with hip fractures [19,20]. Previous studies revealed that effective nursing can obviously improve the quality of prognosis, eliminate fear, andimprove the quality of life of elderly patients with hip fractures [21-23]. However, the health education in conventional nursing is provided only through the guidance on medication and diet, which lacks individuation and concerns for the patients. Therefore, the education can hardly meet patients’ needs and thus reduce the nursing efficiency.
In this study, EBNM based on conventional nursing was implemented to conduct health education intervention. The results exhibited that after intervention, the scores of BBS and FMA scale in the two groups were remarkably improved compared with those before intervention, while the scores of NRS, SAS and SDS in the two groups were significantly reduced compared to those before intervention. The hospital stay and fracture healing time in the experimental group were shorter than those in the control group (P < 0.05). The scores of BBS and FMA in the experimental group were remarkably higher than those in the control group, while the scores of NRS, SAS and SDS and the overall incidence rate of complications were markedly lower than those in the control group (P < 0.05). The experiment proves that the conventional nursing combined with health education based on EBNM can shorten the rehabilitation time, improve the balance abilities and motion coordination abilities, reduce the incidence rate of postoperative complications, alleviate degrees of pain, eliminate adverse emotions, and elevate the quality of life of early patients with hip fractures. This is basically consistent with the study results obtained by March, Hohler, Christie, et al. [24-26].
In summary, the implementation of EBNM in health education can remarkably improve the degrees of cognition of health knowledge and prognosis, alleviate the adverse emotions, reduce the incidence rate of postoperative complications, shorten the therapeutic duration and fracture healing time, and improve the therapeutic efficiency of hip fracture patients. Therefore, it is worthy of clinical promotion and implementation. The innovation of this study lies in implementing EBN in health education, and determining the health education plan through collection of questions and acquisition of evidence.
The shortcomings of this study are as follows: (1) Insufficient samples lead to the lack of universality in the study results. (2) In the study, the functional assessments were performed only using the scales, and no comparative analysis was made on physicochemical indexes and imaging results. In view of the aforementioned shortcomings, the future studies with a larger sample size and more comprehensive assessment criteria should be performed, so as to provide a more detailed theoretical basis for the health education for early fracture patients.
Acknowledgements
This work was supported by Fund of Anhui Province’ Colleges and Universities “Natural Science Research” key Projects (NO. KJ2018A0957), Anhui Province’ Colleges and Universities “Quality Engineering” Projects: Nursing High-level Special Field of Study (NO. 2018ylzy168).
Disclosure of conflict of interest
None.
References
- 1.Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2004;16:S3–S7. doi: 10.1007/s00198-004-1702-6. [DOI] [PubMed] [Google Scholar]
- 2.Coburn M, Röhl AB, Knobe M, Stevanovic A, Stoppe C, Rossaint R. Anesthesiological management of elderly trauma patients. Anaesthesist. 2016;65:98–106. doi: 10.1007/s00101-016-0136-9. [DOI] [PubMed] [Google Scholar]
- 3.van de Ree CLP, De Jongh MAC, Peeters CMM, de Munter L, Roukema JA, Gosens T. Hip fractures in elderly people: surgery or no surgery? a systematic review and meta-analysis. Geriatr Orthop Surg Rehabil. 2017;8:173–180. doi: 10.1177/2151458517713821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoon BH, Baek JH, Kim MK, Lee YK, Ha YC, Koo KH. Poor prognosis in elderly patients who refused surgery because of economic burden and medical problem after hip fracture. J Korean Med Sci. 2013;28:1378–1381. doi: 10.3346/jkms.2013.28.9.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiménez-Mola S, Calvo-Lobo C, Idoate-Gil J, Seco-Calvo J. Functionality, comorbidity, complication & surgery of hip fracture in older adults by age distribution. Rev Assoc Med Bras (1992) 2018;64:420–427. doi: 10.1590/1806-9282.64.05.420. [DOI] [PubMed] [Google Scholar]
- 6.Zanker J, Duque G. Rapid geriatric assessment of hip fracture. Clin Geriatr Med. 2017;33:369–382. doi: 10.1016/j.cger.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Alexiou KI, Roushias A, Varitimidis SE, Malizos KN. Quality of life and psychological consequences in elderly patients after a hip fracture: a review. Clin Interv Aging. 2018;13:143–150. doi: 10.2147/CIA.S150067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pendharkar SA, Singh RG, Chand SK, Cervantes A, Petrov MS. Pro-inflammatory cytokines after an episode of acute pancreatitis: associations with fasting gut hormone profile. Inflamm Res. 2018;67:339–350. doi: 10.1007/s00011-017-1125-4. [DOI] [PubMed] [Google Scholar]
- 9.Spiva L, Hart PL, Patrick S, Waggoner J, Jackson C, Threatt JL. Effectiveness of an evidence-based practice nurse mentor training program. Worldviews Evid Based Nurs. 2017;14:183–191. doi: 10.1111/wvn.12219. [DOI] [PubMed] [Google Scholar]
- 10.Foo S, Majid S, Mokhtar IA, Zhang X, Luyt B, Chang YK, Theng YL. Nurses’ perception of evidence-based practice at the National University Hospital of Singapore. J Contin Educ Nurs. 2011;42:522–528. doi: 10.3928/00220124-20110516-04. [DOI] [PubMed] [Google Scholar]
- 11.Gialanella B, Santoro R, Prometti P, Giordano A, Monguzzi V, Comini L, Olivares A, Grioni G. Functional recovery in hip fracture patients: the role of pharmacotherapy. Aging Clin Exp Res. 2020;32:49–57. doi: 10.1007/s40520-019-01175-w. [DOI] [PubMed] [Google Scholar]
- 12.Dong Y, Wang P, Dai Z, Liu K, Jin Y, Li A, Wang S, Zheng J. Increased self-care activities and glycemic control rate in relation to health education via Wechat among diabetes patients: a randomized clinical trial. Medicine (Baltimore) 2018;97:e13632. doi: 10.1097/MD.0000000000013632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clare MP, Crawford WS. Managing complications of calcaneus fractures. Foot Ankle Clin. 2017;22:105–116. doi: 10.1016/j.fcl.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 14.Baek JH, Lee YK, Hong SW, Ha YC, Koo KH. Knowledge on osteoporosis in guardians of hip fracture patients. J Bone Miner Metab. 2013;31:481–484. doi: 10.1007/s00774-012-0420-y. [DOI] [PubMed] [Google Scholar]
- 15.Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 16.Guzon-Illescas O, Perez Fernandez E, Crespí Villarias N, Quirós Donate FJ, Peña M, Alonso-Blas C, García-Vadillo A, Mazzucchelli R. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res. 2019;14:203. doi: 10.1186/s13018-019-1226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Griffiths R, Alper J, Beckingsale A, Goldhill D, Heyburn G, Holloway J, Leaper E, Parker M, Ridgway S, White S, Wiese M, Wilson I. Management of proximal femoral fractures 2011: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2012;67:85–98. doi: 10.1111/j.1365-2044.2011.06957.x. [DOI] [PubMed] [Google Scholar]
- 18.Rosso F, Dettoni F, Bonasia DE, Olivero F, Mattei L, Bruzzone M, Marmotti A, Rossi R. Prognostic factors for mortality after hip fracture: operation within 48 hours is mandatory. Injury. 2016;47(Suppl 4):S91–S97. doi: 10.1016/j.injury.2016.07.055. [DOI] [PubMed] [Google Scholar]
- 19.Schmitz A, Lins S, Krüger C, Segmüller T, Adler K, Meyer G. “Who is glossary?”--Focus-group evaluation of an evidence-based consumer information brochure on risk of falling and fall prevention in the elderly. Pflege. 2010;23:267–274. doi: 10.1024/1012-5302/a000054. [DOI] [PubMed] [Google Scholar]
- 20.Scheffers-Barnhoorn MN, van Haastregt JC, Schols JM, Kempen GI, van Balen R, Visschedijk JH, van den Hout WB, Dumas EM, Achterberg WP, van Eijk M. A multi-component cognitive behavioural intervention for the treatment of fear of falling after hip fracture (FIT-HIP): protocol of a randomised controlled trial. BMC Geriatr. 2017;17:71. doi: 10.1186/s12877-017-0465-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Currie C. Hip fracture audit: creating a ‘critical mass of expertise and enthusiasm for hip fracture care’? Injury. 2018;49:1418–1423. doi: 10.1016/j.injury.2018.06.025. [DOI] [PubMed] [Google Scholar]
- 22.Erickson KLB. Innovations in care of the elderly hip fracture patient; a nightmare no more. Nurs Clin North Am. 2020;55:149–161. doi: 10.1016/j.cnur.2020.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Shyu YI, Chen MC, Liang J, Tseng MY. Trends in health outcomes for family caregivers of hip-fractured elders during the first 12 months after discharge. J Adv Nurs. 2012;68:658–666. doi: 10.1111/j.1365-2648.2011.05778.x. [DOI] [PubMed] [Google Scholar]
- 24.March LM, Cameron ID, Cumming RG, Chamberlain AC, Schwarz JM, Brnabic AJ, O’Meara P, Taylor TF, Riley S, Sambrook PN. Mortality and morbidity after hip fracture: can evidence based clinical pathways make a difference? J Rheumatol. 2000;27:2227–2231. [PubMed] [Google Scholar]
- 25.Hohler SE. Providing evidence-based practices for patients with hip fractures. Nursing. 2018;48:52–57. doi: 10.1097/01.NURSE.0000531895.31558.55. [DOI] [PubMed] [Google Scholar]
- 26.Christie J, Macmillan M, Currie C, Matthews-Smith G. Improving the experience of hip fracture care: a multidisciplinary collaborative approach to implementing evidence-based, person-centred practice. Int J Orthop Trauma Nurs. 2015;19:24–35. doi: 10.1016/j.ijotn.2014.03.003. [DOI] [PubMed] [Google Scholar]


