Abstract
Objective: To explore the effect of individualized nursing intervention on autologous arteriovenous fistula (AVF) dysfunction and the risk factors leading to failures in maintenance hemodialysis (MHD) patients. Methods: A total of 196 patients undergoing MHD in our hospital from March 2017 to May 2019 were recruited as the study cohort and divided into two groups according to the nursing method each patient underwent. The patients who underwent individualized nursing intervention were placed in the research group (RG, n = 107), and the patients who underwent routine nursing intervention were placed in the control group (CG, n = 89). The proportion of patients with primary dysfunction in the use of AVF was recorded, and the patients’ psychological states, treatment compliance, and self-nursing abilities in the two groups before and after the nursing intervention were observed. The complications, the life treatment scores, and the patients’ nursing satisfaction were recorded after the nursing intervention. A logistic regression analysis was performed for the patients with initial AVF dysfunction. Results: Compared with the CG, the patients in the RG after the nursing intervention had statistically lower AVF dysfunction rates, notably lower SAS and SDS scores, remarkably higher total compliance rates and ESCA scores, and a dramatically lower total incidence of complications. AVF dysfunction occurred in 26 of 196 patients (13.4%) during the follow-up, with an increased risk of AVF loss in patients over 60 years old, lower blood pressure, higher hemoglobin concentrations, lower treatment compliance, self-care inability, and routine nursing interventions. After the nursing, the WHOQOL-BREF and nursing satisfaction scores in the RG were noticeably higher than they were in the CG. Conclusion: Autologous AVF dysfunction is the result of multiple risk factors, and personalized nursing can reduce the incidence of complications, improve patients’ treatment compliance and self-care abilities, and ameliorate their quality of life.
Keywords: Maintenance hemodialysis, autologous arteriovenous fistula dysfunction, risk factors, personalized nursing, efficacy analysis
Introduction
Chronic kidney disease leads to a decline of renal function in most patients and eventually develops into end-stage renal disease, thus requiring hemodialysis or peritoneal dialysis to remove toxins and excess fluid [1]. Hemodialysis is a process in which the blood from the patient’s body is fully introduced into a dialyzer and then diffused and filtered through special electrolytes [2]. Hemodialysis can filter heavy metals, impurities, and metabolic wastes in patients’ blood, improving the patients’ blood environment and reducing the metabolic load of the hepatorenal function [3]. Studies have shown that vascular access with a good hemodialysis function is paramount to ensuring dialysis treatment [4,5].
Clinically, vascular access as the lifeline of hemodialysis has attracted extensive attention [6]. An arteriovenous fistula (AVF) is currently the preferred vascular access point for permanent hemodialysis, for it has the advantages of a long service life and fewer complications, and it creates favorable conditions for hemodialysis treatment [7]. However, clinical studies have found that, affected by related factors, maintenance hemodialysis (MHD) patients are prone to early failure and other symptoms after AVF surgery, leading to limited hemodialysis treatment [8]. Therefore, this study adopted nursing intervention to observe the factors affecting AVF dysfunction. Among the various nursing modes, personalized nursing is one that starts from the perspective of the patients’ personal situation. While expressing care and concern for patients, it also pays attention to their psychological and physical health [9,10]. Evidence has shown that [11], due to the long treatment cycle and high cost, as well as their dislike of their own diseases, treatment methods and various catheterizations, hemodialysis patients are prone to negative emotions such as anxiety and depression. However, according to the patients’ cognitive levels, personalized nursing can explain the disease to the patients, strengthen communication with the patients, help them patiently face their doubts, ease them psychologically, and strengthen their confidence in the treatment [12,13]. For example, in the study of Liu YM et al. [14], nursing intervention for patients during hemodialysis improved their activity intolerance, invalidity, and weak health maintenance through exercise guidance, and bolstered their self-improvement ability to reduce their psychological states of depression and anxiety. Another study indicated [15] that patient-centered nursing intervention for AVF patients can improve patient comfort and intubation results.
In this study, the factors influencing AVF dysfunction in MHD patients were analyzed, and personalized nursing intervention was conducted to observe its effects on the patients’ self-management abilities and treatment efficacy.
Materials and methods
General information
According to the nursing method each patient received, 196 patients who underwent MHD in Chongqing People’s Hospital of Changshou District from March 2017 to May 2019 were divided into two groups: the patients who underwent individualized nursing intervention were selected as the research group (RG; n = 107), and the patients who underwent routine nursing intervention were included in the control group (CG; n = 89). Inclusion criteria: Patients ≥ 18 years old, patients treated with autologous AVF [16], patients with complete general information, clear thinking, and normal language abilities. This study was approved by the Medical Ethics Committee of Chongqing People’s Hospital of Changshou District, and the participants and their families were informed of the study and provided their written informed consent. Exclusion criteria: Patients with a history of thromboembolisms, heart or liver failure, coagulation and immune dysfunction or a previous history of mental illness, patients who withdrew from the experiment halfway were excluded, as well as patients lost to follow-up.
Nursing methods
Patients in CG were treated with routine nursing intervention. The nursing staff gave routine examinations to the patients after admission, provided simple safety education, informed them of matters needing attention during the hemofiltration treatment, and daily protection guidance was carried out. Specific basic knowledge of the disease was also introduced according to each patient’s condition to improve their disease awareness, and successful treatment cases were shared to improve their confidence. Furthermore, a brief introduction to AVF dysfunction was given to the patients and their families before the treatment, and a good ward environment was made available to the patients.
The patients in RG were additionally treated with personalized nursing intervention: (1) Disease explanation and health education: The nursing staff strengthened the talk and communication with the patients after admission to get closer to them, and informed the patients of the disadvantages of negative psychological moods. In addition, the nursing staff cited successful cases of treatment to ease the patients’ psychological concerns, so as to encourage them to actively cooperate with this nursing intervention, and improve their confidence. Since patients may lack awareness of their own diseases after admission, so the nursing staff explained the disease to patients in detail, and patiently informed them and their families about the types of AVF complications and the nursing and defense measures, so as to enhance patients’ disease awareness and self-care abilities. (2) Drug guidance: The nursing staff explained the dosages and durations of the various drugs to the patients in detail, and informed them of the importance of correct medication for disease recovery, so as to enhance their treatment compliance. In addition, the nurses strictly abided by the doctor’s advice to administer drugs to the patients to improve their blood vessels and anticoagulation in order to avoid the occurrence of thrombosis. (3) Nursing of AVF and thrombus: The nursing staff explained arteriovenous internal flow in detail to the patients and their families according to their reception abilities, so as to improve their degree of cooperation. In addition, aseptic operations were carried before each puncture, and the puncture sites were regularly cleaned to avoid causing internal fistula stenosis. (4) Anti-infection nursing: The nursing staff regularly tested the patients’ vital signs, provided drainage and incision for those with local abscesses, and gave them appropriate antibiotics to avoid infections. Also, special attention was paid to avoid punctures on damaged skin to avoid cross infections.
Outcome measures
AVF dysfunction: AVF dysfunction was diagnosed when the extracorporeal blood flow was continuously less than 200 ml/min within 3 months after the first use of AVF, the diameter of the anastomotic vein was no more than 0.4 cm as measured by color Doppler ultrasound, or the dialysis blood flow basically disappeared.
Psychological state: The Self-Rating Depression Scale (SDS) and the Self-Rating Anxiety Scale (SAS) [17] were employed to assess the patients’ psychological states. There are 20 items in the SDS scale, and with a cut-off value of 53 points, 53-62 indicated mild depression, 62-72 indicated moderate depression, and 72 or above indicated severe depression. The SAS scale consists of 20 items, and with a cut-off value of 50 points, 50-59 points were considered mild anxiety, 60-69 points as moderate anxiety, and 70 points or above as severe anxiety.
Treatment compliance: The patient was rated as very compliant if he/she actively cooperated with the nursing staff to complete the operations and adhered to the medical regimens. The patient was rated as compliant if he/she can cooperate well with the treatment and nursing under the guidance of the nursing staff. On the other hand, a patient who still could not cooperate well with the treatment and nursing intervention under the guidance of the nursing staff was rated as non-compliant. Total compliance = (very compliant + compliant)/total number of cases × 100%.
Self-care ability: The Exercise of Self-Care Agency Scale (ESCA) [18] was adopted to evaluate the patients’ self-care abilities. The score had a maximum of 172 points covering 4 domains and 43 items, and the score was in direct proportion to the patients’ self-care abilities.
The complications occurring in the two groups after the nursing intervention were observed and recorded.
Quality of life: The World Health Organization Quality of Life Scale (WHOQOL-BREF) [19] was used to determine the patients’ quality of life. The scale was divided into physical, social, psychological, and environmental domains, with 100 points for each domain. The higher the score, the better the quality of life of the patients after the intervention.
Nursing satisfaction: The patients were given the self-made “Satisfaction Questionnaire” to score the nursing satisfaction. There were four items in the scale, namely, nursing process, nursing quality, nursing effect, and nursing service, and each item had a total possible score of 100 points. The higher the patient’s score, the higher the nursing effect.
Statistical methods
SPSS 25.0 (Beijing Easybio Technology Co., Ltd., Beijing, China) was used for the statistical analysis. The count data were expressed as the number of cases/percentage (n/%), and the inter-group comparisons were performed using Chi-square tests. When the theoretical frequency in a chi-square test was less than 5, a continuous correction Chi-square test was applied. The measurement data were expressed as the mean ± SD, the inter-group comparisons were conducted using independent sample t-tests, and the intra-group comparisons before and after the intervention were realized using paired t-tests. Logistic multivariate regression analyses were used to analyze the risk factors of AVF dysfunction. Significance was determined when probability (P) values were < 0.05.
Results
General information
There were no significant differences in terms of sex, average age, average course of the disease, body mass index (BMI), type of disease, hypotension, residence, ethnicity, educational background, smoking history, drinking history, or hemoglobin concentration between the RG and the CG (P > 0.05) (Table 1).
Table 1.
General data of the patients in the research group and the control group [n (%)] (Mean ± SD)
| Classification | Research group (n = 107) | Control group (n = 89) | t/χ2 value | P value |
|---|---|---|---|---|
| Sex | 0.092 | 0.761 | ||
| Male | 48 (44.86) | 38 (42.70) | ||
| Female | 59 (55.14) | 51 (57.30) | ||
| Average age (years old) | 48.68±3.43 | 49.05±3.49 | 0.746 | 0.457 |
| Average course of disease (years) | 4.42±1.03 | 4.56±1.05 | 0.939 | 0.348 |
| BMI (kg/m2) | 22.75±3.42 | 22.34±3.23 | 0.856 | 0.392 |
| Disease types | 0.789 | 0.673 | ||
| Diabetic nephropathy | 36 (33.64) | 25 (28.09) | ||
| Hypertensive nephropathy | 34 (31.78) | 29 (32.58) | ||
| Chronic nephritis nephropathy | 37 (34.58) | 35 (39.33) | ||
| Hypotension | 0.329 | 0.566 | ||
| Yes | 68 (63.55) | 53 (59.55) | ||
| No | 39 (36.45) | 36 (40.45) | ||
| Residence | 0.172 | 0.677 | ||
| Urban | 63 (58.88) | 55 (61.80) | ||
| Rural | 44 (41.12) | 34 (38.20) | ||
| Ethnicity | 1.084 | 0.297 | ||
| Han | 57 (53.27) | 54 (60.67) | ||
| Ethnic minorities | 50 (46.73) | 35 (39.33) | ||
| Educational background | 0.028 | 0.865 | ||
| ≥ High school | 48 (44.86) | 41 (46.07) | ||
| < High school | 59 (55.14) | 48 (53.93) | ||
| Smoking history | 0.406 | 0.523 | ||
| Yes | 65 (60.75) | 58 (65.17) | ||
| No | 42 (39.25) | 31 (34.83) | ||
| Drinking history | 0.213 | 0.643 | ||
| Yes | 59 (55.14) | 52 (58.43) | ||
| No | 48 (44.86) | 37 (41.57) | ||
| Hemoglobin concentration (g/L) | 113.70±15.32 | 114.05±15.37 | 0.159 | 0.873 |
Comparison of the AVF dysfunction between the two groups after nursing intervention
The AVF dysfunction rate after the nursing intervention was 5.61% in the CG and 22.47% in the CG. The results showed that the AVF dysfunction rate after the nursing intervention was significantly lower in the RG than in the CG (P < 0.05) (Table 2).
Table 2.
Comparison of the AVF dysfunction between the two groups after the nursing intervention [n (%)]
| Groups | n | AVF dysfunction rate (%) | |
|---|---|---|---|
|
| |||
| Failure | Normal | ||
| Research group | 107 | 6 (5.61) | 101 (94.39) |
| Control group | 89 | 20 (22.47) | 69 (77.53) |
| χ2 | - | 12.011 | 12.011 |
| P | - | 0.001 | 0.001 |
Comparison of the SAS and SDS scores between the two groups before and after the nursing intervention
The SAS and SDS scores did not differ significantly between the two groups before the nursing intervention (P > 0.05), but the scores improved notably after the nursing intervention (P < 0.05), and the scores were observably lower in the RG than they were in the CG after the intervention (P < 0.05) (Figure 1).
Figure 1.
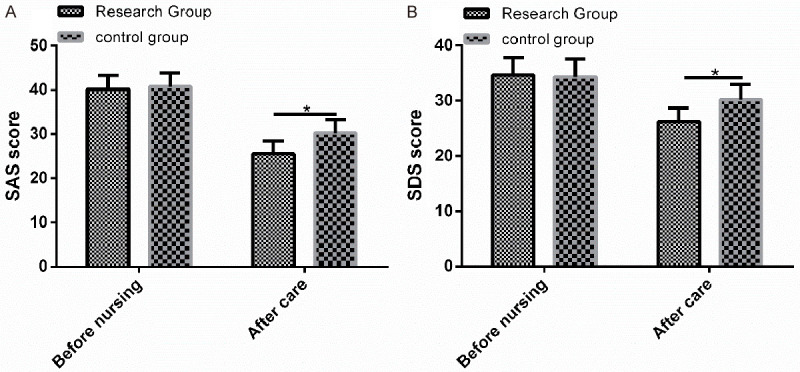
Comparison of the SAS and SDS scores between the two groups before and after the nursing intervention. A. There was no difference in the SAS scores between the two groups before the nursing, but the SAS score in the CG was significantly lower than it was in the CG after the nursing. B. There was no difference in the SDS scores between the two groups before the nursing, but the SDS score in the CG was significantly lower than it was in the CG after the nursing. Note: * indicates P < 0.05 compared between the two groups.
Comparison of the treatment compliance between the two groups after the nursing intervention
The total patient compliance rate in the RG after the nursing intervention was 95.33%, and in the CG it was 76.40%. A comparison of the two groups showed that the total compliance rate of the patients in the RG after the nursing intervention was significantly higher than it was in the CG (P < 0.05) (Table 3).
Table 3.
Comparison of the treatment compliance between the two groups after the nursing intervention [n (%)]
| Groups | n | Complete compliance | Partial compliance | Non-compliance | Total compliance |
|---|---|---|---|---|---|
| Research group | 107 | 71 (66.36) | 31 (28.97) | 5 (4.67) | 102 (95.33) |
| Control group | 89 | 28 (31.46) | 40 (44.94) | 21 (23.60) | 68 (76.40) |
| χ2 | - | - | - | - | 15.121 |
| P | - | - | - | - | 0.001 |
Comparison of the ESCA scores between the two groups before and after the nursing intervention
There was no significant difference in the ESCA scores in the two groups before the nursing intervention (P > 0.05). After the nursing intervention, the ESCA scores were elevated noticeably in the two groups (P < 0.05), and the increase was more significant in the RG compared with the CG (P < 0.05) (Figure 2).
Figure 2.
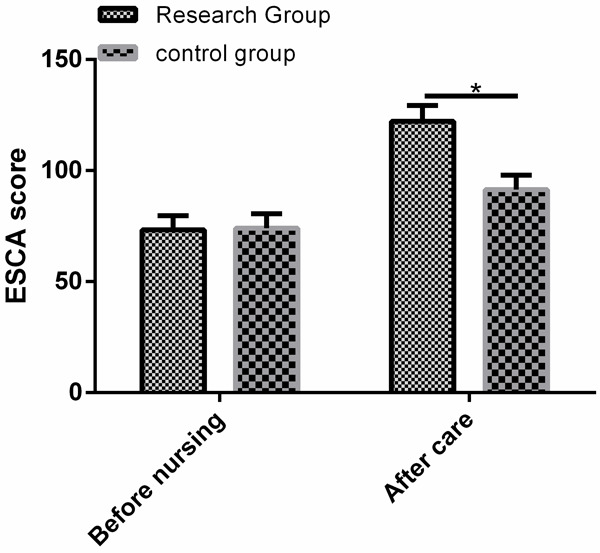
Comparison of the ESCA scores between the two groups before and after the nursing intervention. There was no difference in the ESCA score between the two groups before the nursing, but the ESCA score in the RG was significantly higher than it was in the CG after the nursing. Note: * indicates P < 0.05 compared between the two groups.
Comparison of the incidence of complications between the two groups after the nursing intervention
The total complication incidence rates in the RG and the CG were 5.61% and 25.84%, indicating that the patients who underwent personalized nursing had dramatically fewer complications than the patients treated with routine nursing (P < 0.05) (Table 4).
Table 4.
Comparison of the incidence of complications between the two groups [n (%)]
| Groups | n | Thrombus | Hemorrhage | Infection | Internal fistula stenosis | Subcutaneous hematomas | Total incidence |
|---|---|---|---|---|---|---|---|
| Research group | 107 | 1 (0.93) | 2 (1.87) | 1 (0.93) | 1 (0.93) | 1 (0.93) | 6 (5.61) |
| Control group | 89 | 3 (3.37) | 5 (5.62) | 6 (6.74) | 4 (4.49) | 5 (5.62) | 23 (25.84) |
| χ2 | - | 1.442 | 1.983 | 4.757 | 2.477 | 3.591 | 15.781 |
| P | - | 0.229 | 0.159 | 0.029 | 0.115 | 0.058 | < 0.001 |
Analysis of the risk factors affecting AVF dysfunction
After comparing the differences in the clinical parameters and the related indexes of the AVF patients after the nursing intervention, it was found that there were 26 patients in the AVF dysfunction group and 170 in the unobstructed group. The patient characteristics showed no significant differences in sex, disease type, smoking history, or alcohol consumption between the unobstructed group and the dysfunction group (P > 0.05). Conversely, significant differences were present in the patients’ ages, hypotension, hemoglobin concentrations, treatment compliance, lack of self-care abilities, and nursing modes (P < 0.05). A multivariate logistic regression analysis was conducted on the factors with differences. The results showed that age (P = 0.001), hypotension (P = 0.001), hemoglobin concentration (P = 0.018), treatment compliance (P = 0.021), self-care inability (P = 0.017) and nursing mode (P = 0.001) were independent risk factors for failure in AVF patients. Patients over 60, patients with low blood pressure, higher hemoglobin concentrations, a lower treatment compliance, patients lacking self-care abilities, and patients undergoing routine nursing intervention were at increased risk for AVF dysfunction (Tables 5, 6 and 7).
Table 5.
Univariate analysis of the AVF dysfunction [n (%)] (mean ± SD)
| Classification | n | Dysfunction group (n = 26) | Unobstructed group (n = 170) | t/χ2 value | P value |
|---|---|---|---|---|---|
| Sex | 2.323 | 0.127 | |||
| Male | 86 | 15 (17.44) | 71 (82.56) | ||
| Female | 110 | 11 (10.00) | 99 (90.00) | ||
| Age (years old) | 14.141 | 0.001 | |||
| 35-60 | 125 | 8 (6.40) | 117 (93.60) | ||
| > 60 | 71 | 18 (25.35) | 53 (74.65) | ||
| Disease type | 0.395 | 0.820 | |||
| Diabetic nephropathy | 61 | 9 (14.75) | 52 (85.25) | ||
| Hypertensive nephropathy | 63 | 7 (11.11) | 56 (88.89) | ||
| Chronic nephritis nephropathy | 72 | 10 (13.89) | 62 (86.11) | ||
| Hypotension | 4.598 | 0.032 | |||
| Yes | 121 | 21 (17.36) | 100 (82.64) | ||
| No | 75 | 5 (6.67) | 70 (93.33) | ||
| Smoking history | 0.088 | 0.765 | |||
| Yes | 123 | 17 (13.82) | 106 (86.18) | ||
| No | 73 | 9 (12.33) | 64 (87.67) | ||
| Drinking history | 1.973 | 0.164 | |||
| Yes | 111 | 18 (16.22) | 93 (83.78) | ||
| No | 85 | 8 (9.41) | 77 (90.59) | ||
| Hemoglobin concentration (g/L) | 110.43±15.22 | 92.47±15.03 | 5.665 | < 0.001 | |
| Treatment compliance | 118.710 | < 0.001 | |||
| High | 170 | 5 (2.94) | 165 (97.06) | ||
| Low | 26 | 21 (80.77) | 5 (19.23) | ||
| Inability to self-care | 80.771 | < 0.001 | |||
| Yes | 167 | 7 (4.19) | 160 (95.81) | ||
| No | 29 | 19 (65.52) | 10 (34.48) | ||
| Nursing mode | 18.591 | < 0.001 | |||
| Personalized nursing | 107 | 4 (3.74) | 103 (96.26) | ||
| Routine nursing | 89 | 22 (24.72) | 67 (75.28) |
Table 6.
Logistic multivariate regression analysis assignment
| Factors | Variables | Assignment |
|---|---|---|
| age > 60 years old | X1 | Yes = 0, no = 1 |
| Hypotension | X2 | Yes = 0, no = 1 |
| Hemoglobin concentration (g/L) | X3 | Continuous variable |
| Treatment compliance | X4 | High = 0, low = 1 |
| Inability to self-care | X5 | Yes = 0, no = 1 |
| Nursing mode | X6 | Personalized nursing = 0, routine nursing = 1 |
Table 7.
Multivariate Logistic regression analysis of the AVF dysfunction
| Variables | B | S.E | Wals | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| age > 60 years old | 0.518 | 0.204 | 2.438 | 0.001 | 1.679 | 0.839-3.358 |
| Hypotension | 0.509 | 0.334 | 8.012 | 0.001 | 1.684 | 0.842-3.368 |
| Hemoglobin concentration | 0.039 | 0.016 | 2.003 | 0.018 | 1.041 | 0.521-2.082 |
| Treatment compliance | 0.429 | 0.257 | 3.178 | 0.021 | 1.218 | 0.609-2.436 |
| Self-care inability | 0.615 | 0.346 | 7.873 | 0.017 | 1.852 | 0.926-3.704 |
| Nursing mode | 0.864 | 0.376 | 9.203 | 0.001 | 3.091 | 1.545-6.182 |
Comparison of the WHOQOL-BREF scores between the two groups after the nursing intervention
After the nursing, the WHOQOL-BREF scores of the patients in CG were significantly higher than those in CG in the psychological, social, physical, and environmental domains (Table 8).
Table 8.
Comparison of the WHOQOL-BREF scores between the two groups after the nursing intervention (mean ± SD)
| Groups | n | Psychological domain | Social domain | Physical domain | Environmental domain |
|---|---|---|---|---|---|
| Research group | 107 | 77.38±4.27 | 80.23±4.32 | 80.73±3.23 | 77.23±4.13 |
| Control group | 89 | 70.59±3.58 | 73.34±4.04 | 74.54±3.19 | 71.15±4.29 |
| t | - | 11.920 | 11.450 | 13.430 | 10.080 |
| P | - | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Comparison of the nursing satisfaction scores between the two groups after the nursing intervention
The nursing quality, nursing effect, nursing process, and nursing service ratings in the RG were significantly higher than the corresponding ratings in the CG (P < 0.05) (Table 9).
Table 9.
Comparison of the nursing satisfaction scores between the two groups after the nursing intervention [n (%)]
| Groups | n | Nursing quality | Nursing effect | Nursing process | Nursing service |
|---|---|---|---|---|---|
| Research group | 107 | 97.24±3.43 | 89.34±3.24 | 90.79±4.05 | 95.24±4.53 |
| Control group | 89 | 90.51±3.21 | 83.28±3.17 | 85.16±4.02 | 88.34±4.12 |
| χ2 | - | 14.080 | 13.170 | 9.722 | 11.060 |
| P | - | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Discussion
With the continuous improvement of medical science and technology, hemodialysis technology has also been significantly developed, giving it unique advantages in the treatment of some diseases, especially for patients with end-stage renal disease [20]. For patients needing MHD, maintaining the integrity and good function of vascular access is the key to dialysis treatment [21,22]. For AVF patients, nursing intervention is essential because internal fistula dysfunction and various complications can occur easily [23].
In the present study, we carried out personalized nursing intervention for MHD patients with AVF and found that the patients’ conditions were notably improved after the nursing intervention. Evidence has shown [24] that in hemodialysis patients, the body’s immune function is decreased, and when arteriovenous internal fistulas have contact with the outside world, secondary infections can occur due to decreased immunity, resulting in AVF dysfunction. In this study, we observed the AVF dysfunction of the two groups of patients after the nursing, and found that the total AVF dysfunction rate in the RG after the nursing intervention was markedly lower than it was in the CG, indicating that personalized nursing enhances patients’ awareness of hemodialysis treatment and improves their cooperation with AVF maintenance, thus reducing the occurrence of AVF dysfunction. Generally, the treatment cycle of MHD is long, and patients are susceptible to various adverse emotions, greatly reducing their treatment compliance and efficacy [25]. Therefore, we recorded the patients’ adverse psychological emotions. It was found that after the nursing intervention, the patients in the RG presented significantly lower SAS and SDS scores than the CG, suggesting that personalized nursing intervention improves the patients’ awareness of the disease and treatment, and effectively alleviates their anxiety and depression through psychological nursing. Studies have found that [26] chronic hemodialysis patients show low treatment compliance and reduced treatment efficacy, so the formulation and implementation of intervention measures can improve patients’ treatment compliance and reduce the use of health resources. By observing the treatment compliance of the patients in the two groups, we found that the total treatment compliance rate in the RG was significantly higher than it was in the CG, indicating that personalized nursing provides effective intervention measures for patients to improve their treatment compliance, thereby improving their treatment efficacy. Also, there is research showing that [27] improved self-management support can improve the drug compliance of patients with non-control hypertension hemodialysis and can better control their blood pressure. The results of this study indicate that the ESCA scores of the patients in RG was significantly higher than they were in the CG after the nursing intervention, which indicated that personalized nursing intervention bolstered the patients’ self-management and self-care abilities.
During the treatment of MHD patients, AVF dysfunction may trigger complications like bleeding and thrombosis [28]. Qin et al. [29] reported that professional fistula care can prolong the AVF use times in MHD patients, reduce the incidence of complications, and improve the quality of life of patients. The results of this study showed that the complication incidence rate in the RG was dramatically lower than it was in the CG, indicating that personalized nursing can help reduce the incidence of infections. The reason behind it may be due to the fact that the thrombus nursing implemented in the personalized nursing avoided blood viscosity and thrombosis induced by increased hemoglobin levels, and nursing care for bleeding and infections helped avoid cross infections. Moreover, compared with the CG, the WHOQOL-BREF scores of the patients in the CG after the nursing were observably higher, indicating that personalized nursing helped patients establish good and healthy living habits and kept patients in a healthy physiological state, thereby improving their quality of life. It has been reported [30] that AVF dysfunction in hemodialysis patients is related to sex, age, PLT count, hemoglobin level, and duration of temporary catheter indwelling. In this study, the risk factors for AVF dysfunction were analyzed, and the results showed that patients over 60 years old, patients with lower blood pressure, higher hemoglobin concentrations, lower treatment compliance, self-care inabilities, and routine nursing interventions had an increased risk of AVF dysfunction. Finally, we calculated the nursing satisfaction scores. The results showed that the nursing satisfaction of the patients in RG was significantly higher than it was in the CG, indicating that the patients highly appreciated the nursing intervention, which provides a strong reference for the subsequent clinical application.
Although this study confirmed that personalized nursing can reduce MHD-induced autogenous AVF dysfunction, there is still room for improvement. For example, we can further increase the number of research participants and observe the intervention effects of personalized nursing at different ages. In the future, we will gradually carry out supplementary studies from the above perspectives.
To sum up, autologous AVF dysfunction occurs due to multiple risk factors, and personalized nursing can reduce the incidence of complications, improve patients’ treatment compliance and self-care abilities, and ameliorate their quality of life.
Disclosure of conflict of interest
None.
References
- 1.Lu W, Ren C, Han X, Yang X, Cao Y, Huang B. The protective effect of different dialysis types on residual renal function in patients with maintenance hemodialysis: a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e12325. doi: 10.1097/MD.0000000000012325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kofler M, Lenninger M, Mayer G, Neuwirt H, Grimm M, Bechtold T. Multi-chamber electroosmosis using textile reinforced agar membranes--a promising concept for the future of hemodialysis. Carbohydr Polym. 2016;136:81–86. doi: 10.1016/j.carbpol.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 3.Khanna R. Solute and water transport in peritoneal dialysis: a case-based primer. Am J Kidney Dis. 2017;69:461–472. doi: 10.1053/j.ajkd.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Chen CF, Chen FA, Lee TL, Liao LF, Chen CY, Tan AC, Chan CH, Lin CC. Current status of dialysis and vascular access in Taiwan. J Vasc Access. 2019;20:368–373. doi: 10.1177/1129729818807336. [DOI] [PubMed] [Google Scholar]
- 5.Fukasawa M. Current status of vascular access in Japan-from dialysis access symposium 2017. J Vasc Access. 2019;20:38–44. doi: 10.1177/1129729818762982. [DOI] [PubMed] [Google Scholar]
- 6.Shroff R, Calder F, Bakkaloglu S, Nagler EV, Stuart S, Stronach L, Schmitt CP, Heckert KH, Bourquelot P, Wagner AM, Paglialonga F, Mitra S, Stefanidis CJ European Society for Paediatric Nephrology Dialysis Working Group. Vascular access in children requiring maintenance haemodialysis: a consensus document by the European Society for Paediatric Nephrology Dialysis Working Group. Nephrol Dial Transplant. 2019;34:1746–1765. doi: 10.1093/ndt/gfz011. [DOI] [PubMed] [Google Scholar]
- 7.Raji YR, Ajayi SO, Aminu O, Abiola B, Efuntoye O, Salako BL, Arije A, Kadiri S. Outcomes of tunneled internal jugular venous catheters for chronic haemodialysis at the University College Hospital, Ibadan, Nigeria. Pan Afr Med J. 2018;31:218. doi: 10.11604/pamj.2018.31.218.17525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abreo K, Amin BM, Abreo AP. Physical examination of the hemodialysis arteriovenous fistula to detect early dysfunction. J Vasc Access. 2019;20:7–11. doi: 10.1177/1129729818768183. [DOI] [PubMed] [Google Scholar]
- 9.Yang Y, Li H, Xiao LD, Zhang W, Xia M, Feng H. Resident and staff perspectives of person-centered climate in nursing homes: a cross-sectional study. BMC Geriatr. 2019;19:292. doi: 10.1186/s12877-019-1313-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamei T, Takahashi K, Omori J, Arimori N, Hishinuma M, Asahara K, Shimpuku Y, Ohashi K, Tashiro J. Toward advanced nursing practice along with people-centered care partnership model for sustainable universal health coverage and universal access to health. Rev Lat Am Enfermagem. 2017;25:e2839. doi: 10.1590/1518-8345.1657.2839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwan JR, Chong TT, Low GZ, Low GW, Htay H, Foo MW, Tan C. Outcomes following peritoneal dialysis catheter removal with reinsertion or permanent transfer to haemodialysis. J Vasc Access. 2019;20:60–64. doi: 10.1177/1129729818773984. [DOI] [PubMed] [Google Scholar]
- 12.Chan ZCY. A qualitative study on communication between nursing students and the family members of patients. Nurse Educ Today. 2017;59:33–37. doi: 10.1016/j.nedt.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 13.Harnischfeger N, Rath HM, Ullrich A, Alt-Epping B, Letsch A, Thuss-Patience P, Bokemeyer C, Oechsle K, Bergelt C. Evaluation of a communication skills training to facilitate addressing palliative care related topics in advanced cancer patients: study protocol of a multicenter randomized controlled trial (PALLI-KOM) BMC Palliat Care. 2020;19:67. doi: 10.1186/s12904-020-00568-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu YM, Yeh ML, Chung YC. Improving physiological and psychological status in a hemodialysis patient: a nursing experience using an exercise training program. Hu Li Za Zhi. 2013;60:104–110. doi: 10.6224/JN.60.5.104. [DOI] [PubMed] [Google Scholar]
- 15.Wilson B, Harwood L. Reaching consensus on outcomes for successful cannulation of an arteriovenous fistula: patient and healthcare provider perspectives. Nephrol Nurs J. 2018;45:327–336. [PubMed] [Google Scholar]
- 16.Freitas LR, Pennafort VPDS, Mendonca AEO, Pinto FJM, Aguiar LL, Studart RMB. Guidebook for renal dialysis patients: care of central venous catheters and arteriovenous fistula. Rev Bras Enferm. 2019;72:896–902. doi: 10.1590/0034-7167-2018-0131. [DOI] [PubMed] [Google Scholar]
- 17.Hou Y, Li X, Yang L, Liu C, Wu H, Xu Y, Yang F, Du Y. Factors associated with depression and anxiety in patients with end-stage renal disease receiving maintenance hemodialysis. Int Urol Nephrol. 2014;46:1645–1649. doi: 10.1007/s11255-014-0685-2. [DOI] [PubMed] [Google Scholar]
- 18.Guo L, Soderhamn U, McCallum J, Ding X, Gao H, Guo Q, Liu K, Liu Y. Testing and comparing two self-care-related instruments among older Chinese adults. PLoS One. 2017;12:e0182792. doi: 10.1371/journal.pone.0182792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joshi U, Subedi R, Poudel P, Ghimire PR, Panta S, Sigdel MR. Assessment of quality of life in patients undergoing hemodialysis using WHOQOL-BREF questionnaire: a multicenter study. Int J Nephrol Renovasc Dis. 2017;10:195–203. doi: 10.2147/IJNRD.S136522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong CKH, Chen J, Fung SKS, Mok MMY, Cheng YL, Kong I, Lo WK, Lui SL, Chan TM, Lam CLK. Direct and indirect costs of end-stage renal disease patients in the first and second years after initiation of nocturnal home haemodialysis, hospital haemodialysis and peritoneal dialysis. Nephrol Dial Transplant. 2019;34:1565–1576. doi: 10.1093/ndt/gfy395. [DOI] [PubMed] [Google Scholar]
- 21.Richard CJ. Preservation of vascular access for hemodialysis in acute care settings. Crit Care Nurs Q. 2011;34:76–83. doi: 10.1097/CNQ.0b013e3182048ca4. [DOI] [PubMed] [Google Scholar]
- 22.Ayarragaray JE. Surgical treatment of hemodialysis-related central venous stenosis or occlusion: another option to maintain vascular access. J Vasc Surg. 2003;37:1043–1046. doi: 10.1067/mva.2003.215. [DOI] [PubMed] [Google Scholar]
- 23.Bai YL, Hung SY, Chiou CP. Vascular access management and education for hemodialysis patients. Hu Li Za Zhi. 2014;61:93–98. doi: 10.6224/JN.61.1.93. [DOI] [PubMed] [Google Scholar]
- 24.MacAskill MG, Watson DG, Ewart MA, Wadsworth R, Jackson A, Aitken E, MacKenzie G, Kingsmore D, Currie S, Coats P. Improving arteriovenous fistula patency: transdermal delivery of diclofenac reduces cannulation-dependent neointimal hyperplasia via AMPK activation. Vascul Pharmacol. 2015;71:108–115. doi: 10.1016/j.vph.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hou Y, Li X, Yang L, Liu C, Wu H, Xu Y, Yang F, Du Y. Factors associated with depression and anxiety in patients with end-stage renal disease receiving maintenance hemodialysis. Int Urol Nephrol. 2014;46:1645–1649. doi: 10.1007/s11255-014-0685-2. [DOI] [PubMed] [Google Scholar]
- 26.Tohme F, Mor MK, Pena-Polanco J, Green JA, Fine MJ, Palevsky PM, Weisbord SD. Predictors and outcomes of non-adherence in patients receiving maintenance hemodialysis. Int Urol Nephrol. 2017;49:1471–1479. doi: 10.1007/s11255-017-1600-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang B, Li Z, Wang Y, Xia J, Shi T, Jiang J, Nolan MT, Li X, Nigwekar SU, Chen L. Effectiveness of self-management support in maintenance haemodialysis patients with hypertension: a pilot cluster randomized controlled trial. Nephrology (Carlton) 2018;23:755–763. doi: 10.1111/nep.13098. [DOI] [PubMed] [Google Scholar]
- 28.Lee CH. Stent graft repair of iatrogenic femoral arteriovenous fistula with acute bleeding after hemodialysis catheter insertion. Hemodial Int. 2016;20:497–500. doi: 10.1111/hdi.12431. [DOI] [PubMed] [Google Scholar]
- 29.Qin HY, Jia P, Liu H. Nursing strategies for patients with chronic renal failure undergoing maintenance hemodialysis treatment by arteriovenous fistula. Iran J Public Health. 2016;45:1270–1275. [PMC free article] [PubMed] [Google Scholar]
- 30.Wen M, Li Z, Li J, Zhou W, Liu Y, Liu H, Chen G. Risk factors for primary arteriovenous fistula dysfunction in hemodialysis patients: a retrospective survival analysis in multiple medical centers. Blood Purif. 2019;48:276–282. doi: 10.1159/000500045. [DOI] [PubMed] [Google Scholar]


