Abstract
Objective: To explore the effects of PICCO on the Guidance of Goal-Directed Fluid Therapy for gastrointestinal function after cytoreductive surgery for ovarian cancer. Methods: A total of 98 patients who received cytoreductive surgery for ovarian cancer under general anesthesia in our hospital were stochastically divided into the observation group and control group, with 49 cases in each group. The observation group received PICCO guided goal-directed fluid therapy, while patients in the control group were treated with conventional fluid therapy. At last, the total amount of infusion, the time required for postoperative gastrointestinal function recovery and related recovery rating, the first time to get out of bed after the surgery and the total hospitalization time were observed and compared between the two groups. Results: The observation group had less time for gastrointestinal function recovery and had better functional recovery rating as well as other indicators than the control group. Besides, the observation group had less volume of infusion, needed shorter time to get out of bed and had a shorter length of hospital stay than the control group (all P<0.05). Conclusion: PICCO guided goal-directed liquid therapy can effectively improve the recovery of gastrointestinal function and reduce the length of stay in patients with ovarian cancer after cytoreductive surgery.
Keywords: Cytoreductive surgery for ovarian cancer, PICCO guided goal-directed, liquid therapy, recovery of gastrointestinal function
Introduction
Ovarian cancer is one of the most common cancers of the female reproductive system. It has does not have the highest incidence rate but it does have the highest mortality rate among female genital tract tumors, reported by an epidemiological survey. The main reason, we believe is due to the deep location of the ovary with in the pelvic cavity, and so no specific clinical manifestations are found in a timely manner in the early stages, which leads to delayed diagnosis and the missing of the best time for treatment [1-4]. Studies have shown that more than 70% of patients with ovarian cancer are already in advanced stage when diagnosed. Besides, with the characteristics of easily invasion of the uterus and pelvic cavity, ovarian cancer is not completely removed by surgery. However, active tumor resection is still of positive significance for the prognosis of patients [5-7]. At present, the combination of ovarian cancer cytoreductive surgery with peritoneal lavage and intravenous chemotherapy are preferred in clinical treatment, and have achieved certain results [8,9].
Due to the characteristics of a large amount of trauma, long operation time, large amount of blood loss and fluid loss, traditional open abdominal surgery for ovarian cancer slows down the recovery of gastrointestinal function and affects the overall prognosis of patients, so a large amount of fluid needs to be supplemented during the operation [10-12]. Previous studies have also gradually confirmed that intraoperative fluid management is of great significance for the recovery of postoperative functions of patients with ovarian cancer [13,14]. Previous fluid management was mainly conducted according to the clinical characteristics of patients (including temperature, heart rate, blood pressure, respiratory parameters, intraoperative central venous pressure changes, urine volume, blood loss, etc.), but these above measures were not necessarily accurate, and there may also be a risk of tissue damage caused by excessive or insufficient fluid infusion [15,16]. Therefore, more accurate fluid resuscitation management guidance may have important clinical significance for gynecological tumor patients.
As the latest liquid monitoring instrument, Pulse Indicating Continuous Cardiac Output (PICCO) has irreplaceable advantages in monitoring cardiac function indicators, arterial pressure, especially in volume indicators, compared with traditional monitoring indicators (such as central venous pressure and blood pressure) [17,18]. It has been confirmed that PICCO has achieved good effects in guiding the fluid infusion volume for patients with shock, but there is little research about its implementation in the effects of gynecologic tumor surgery on perioperative functional recovery [19]. Based on this, we explored the application of PICCO in the fluid treatment of patients with ovarian cancer undergoing open surgery, in order to provide more accurate guidance for the fluid management of ovarian cancer patients undergoing tumor cytoreductive surgery, and promote the postoperative recovery of patients.
Materials and methods
General materials
A total of 98 patients undergoing cytoreductive surgery for ovarian cancer in The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China from June 2019 to December 2020 were stochastically divided into the observation group and control group, with 49 cases in each group.
Inclusion Criteria: 1) ovarian cancer patients were diagnosed by preoperative cellular acupuncture or postoperative pathology, patients met the relevant diagnostic criteria [20]; 2) patients were aged between 20 to 70 years old; 3) patients without a history of surgery, radiotherapy and chemotherapy; 4) the expected survival time was more than half a year; 5) all patients were treated with cytoreductive surgery; 6) patients meeting the American Society of Anesthesiologists (ASA) grade I-II. Exclusion Criteria: 1) patients in clinical stage I-II; 2) patients accompanied with tumors in other tissues; 3) patients with Karnofsky (KPS) <60; 4) patients accompanied with major organ dysfunction such as in the heart, liver and kidney; 5) patients with previous immune system diseases; 6) patients with systemic infection or cachexia; 7) patients with contraindications or conditions which cannot meet the requirements of PICCO monitoring; 8) patients with blood system diseases such as abnormal coagulation function; 9) patients who were allergic to the liquid used in this study. All subjects had the nature of the study explained to them in detail and they signed the consent. The study was approved by the Ethics Committee of The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China.
Methods
Treatment methods
The two groups of patients both had cytoreductive surgery for ovarian cancer combined with postoperative chemotherapy. Paclitaxel intravenous chemotherapy combined with intraperitoneal hyperthermic perfusion of cisplatin were used for chemotherapy.
Cytoreductive surgery for ovarian cancer
The patients received cytoreductive surgery for ovarian cancer under general anesthesia. If there is a large amount of ascites in abdominal cavity, drainage was carried out in batches before the operation to ensure safety. The median or left lateral median incision was selected for the operation. The size of the incision was made based on the stomach, intestine and other tissues and organs in the operation field. Omental resection was performed according to the extent and degree of the tumor involved to expose the tumor. Then the pelvic tumor was resected (if the pelvic structure was intact, the whole uterus and double appendages were removed; otherwise, pelvic peritoneum was also be resected in addition to the above-mentioned surgical scope). Other tissues, such as the rectum, sigmoid colon, bladder and lymph node, were resected according to the corresponding operation. The tumor size <1.0 cm was taken as the resection standard [21].
Principles of intraoperative fluid management
The vital signs (heart rate, blood pressure, oxygen saturation) in both groups were closely detected. Sodium lactate Ringer’s solution (Baxter, USA) was used as the crystal and hydroxyethyl starch 130/0.4 sodium chloride injection (Fresenius, China) was used as the colloids (ratio of crystal to colloid was 2:1). At the same time, infusing human albumin was determined according to the albumin content before the operation (albumin <30 g/L needs to be infused). During the operation, hematocrit was adjusted according to blood gas analysis (HB<80 g/L); hematocrit was adjusted according to blood gas analysis during operation (Hb<80 g/L was infused with red cells suspension); because of the small amount of bleeding in patients with ovarian cancer (usually less than 300 mL), plasma was not routinely infused.
Rehydration principle
Rehydration principle of the control group
The volume of rehydration fluids was calculated according to the classical liquid calculation method: we took into account the body mass lost (cumulative loss + abdominal tissue loss + insensible evaporation) and physiological needs, including the central venous pressure (CVP <8 mmHg rehydration) and blood pressure (<80 mmHg rehydration), and fluid replacement was carried out according to the crystal gel ratio of 2:1.
Rehydration principle of the observation group
The patients in the observation group were monitored by PICCO hemodynamics. Cardiac index (CI), central venous pressure (CVP), global end diastolic volume index (GEDI), global ejection fraction (GEF), intrapleural blood volume index (ITBVI), and extravascular lung water index (EVLWI) were used as the evaluation index. The ratio of infusion was 1:2, with the end diastolic volume and cardiac index as the main indicator, and mean arterial pressure and central venous pressure as the auxiliary. The specific process is shown in Figure 1.
Figure 1.
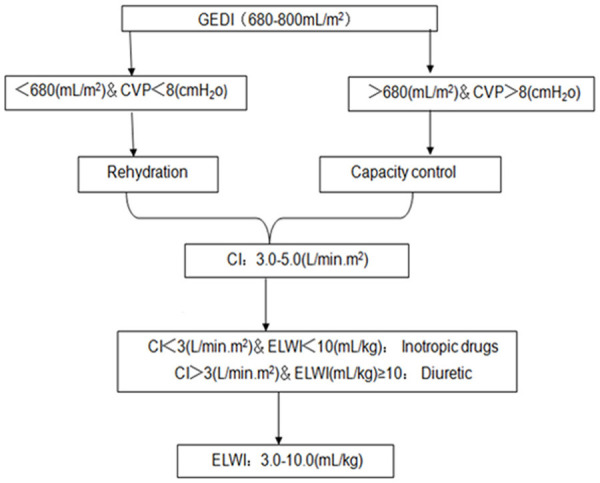
Capacity management process under PICCO monitoring. GEDI: global end diastolic volume index; CVP: central venous pressure; CI: cardiac index; ELWI: extravascular lung water index.
Outcome measures
Main outcome measures: The time needed for the recovery of gastrointestinal function (intestinal exhaust) and corresponding recovery grade (the recovery effect of gastrointestinal function is judged as excellent if the gastrointestinal function of patients was recovered within 24 h; judged as good if the time needed was within 24-36 h and judged as poor if the time needed was longer than 36 h) and the time needed to get out of bed after surgery.
Secondary outcome measures: The intraoperative conditions (blood loss, operation time, total fluid infusion) and total hospital stay of the two groups.
Statistical analysis of data
All data were analyzed by SPSS 22.0 software. The measurement data were expressed as mean ± SD, and the independent t test was used for comparison between groups; the enumeration data were expressed by the number of cases/percentage (n/%). χ2 test was used to compare the rates between groups for the enumeration data and α=0.05 was taken as the test standard. P<0.05 was statistically significant.
Results
Comparison of baseline data between the two groups
No significant difference existed in age, course of disease, clinical stage and tumor type between the two groups (all P>0.05). See Table 1 for details.
Table 1.
Comparison of baseline data between the two groups
| Groups | Control group (n=49) | Observation group (n=49) | t/χ2 | P |
|---|---|---|---|---|
| Age (years) | 49.5±8.7 | 52.0±7.4 | 1.532 | 0.129 |
| Hemoglobin content (g/L) | 135.9±18.7 | 134.2±17.0 | 0.471 | 0.639 |
| BMI (kg/m2) | 24.5±4.8 | 25.6±5.2 | 1.088 | 0.279 |
| Ascites/extraction (n) | 18/11 | 14/6 | 0.418/0.019 | 0.518/0.892 |
| Albumin (g/L) | 38.5±7.7 | 39.2±8.5 | 0.427 | 0.670 |
| Volume of ascites extracted (mL) | 230.72±25.80 | 241.53±26.94 | 1.653 | 0.102 |
| Malnutrition (n) | 8 | 12 | 0.565 | 0.452 |
| Course of disease (month) | 5.3±1.2 | 5.7±1.6 | 1.400 | 0.165 |
| Clinical stages | 0.164 | 0.686 | ||
| Stage III | 25 | 22 | ||
| Stage IV | 24 | 27 | ||
| Tumor type | 2.001 | 0.157 | ||
| Serous adenocarcinoma | 29 | 21 | ||
| Mucinous adenocarcinoma | 20 | 28 |
Note: BMI: body mass index.
Comparison of intraoperative data between the two groups
The results showed that there existed no significant difference in operation time, amount of bleeding, urine volume, mean arterial pressure and central venous pressure between the two groups (all P>0.05). However, the observation group had a lower mean amount of fluid infusion than the control group (P<0.001), indicating that PICCO reduced the total fluid infusion volume. See Table 2 for details.
Table 2.
Comparison of intraoperative conditions between the two groups
| Groups | Control group (n=49) | Observation group (n=49) | t | P |
|---|---|---|---|---|
| Operation time (min) | 260.55±23.10 | 254.87±22.19 | 1.241 | 0.218 |
| Urine volume (mL) | 259.4±40.13 | 253.8±39.60 | 0.447 | 0.488 |
| MAP (mmHg)/CVP (cmH2O) | 83.8±10.6/5.4±1.4 | 84.1±9.9/5.3±1.8 | 0.145/0.307 | 0.885/0.760 |
| Amount of bleeding (mL) | 230.54±72.18 | 241.50±78.29 | 0.720 | 0.473 |
| Total liquid volume (mL) | ||||
| Crystal | 1879.35±219.07 | 1172.48±235.71 | 15.377 | 0.000 |
| Gel | 987.93±308.91 | 583.61±358.42 | 5.981 | 0.000 |
Note: MAP: mean arterial pressure; CVP: central venous pressure.
Comparison of time needed for postoperative gastrointestinal function recovery and getting out of bed between the two groups
The results of this study showed that the time needed for postoperative gastrointestinal function recovery (first exhaust time) and the time needed to get out of bed after surgery and the total hospitalization time of patients in the observation group were all much lower than those in the control group (P<0.05), which indicated that PICCO had certain effects on promoting the recovery of gastrointestinal function. See Figures 2, 3 and 4 for details.
Figure 2.
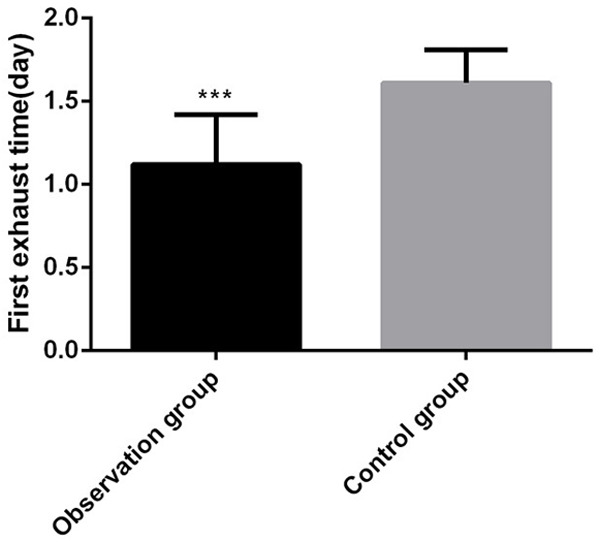
First exhaust time of two groups of patients. Compared with the control group, ***P<0.001.
Figure 3.
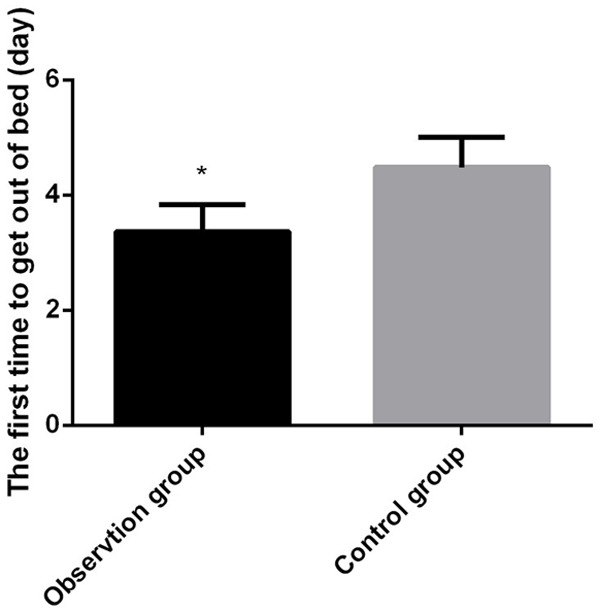
The first time to get out of bed after surgery. Compared with the control group, *P<0.05.
Figure 4.
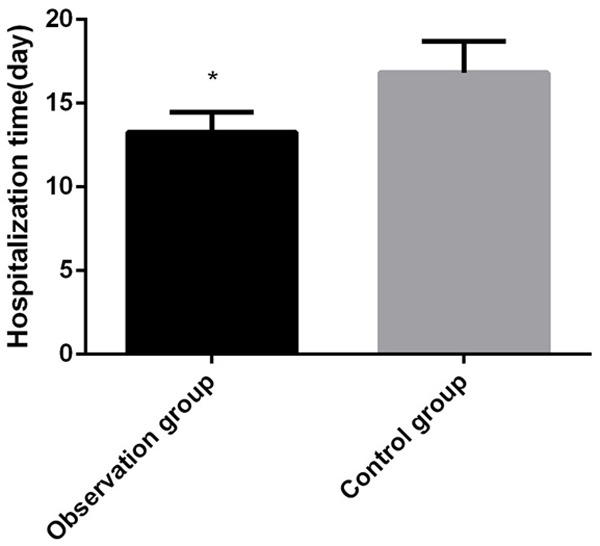
Comparison of total hospitalization time between the two groups. Compared with the control group, *P<0.05.
Comparison of gastrointestinal function grading between the two groups
The results of this study showed that the gastrointestinal recovery rating of the observation group was much better than that of the control group (P<0.01), which confirmed that PICCO improved the recovery rating of gastrointestinal function in patients with ovarian cancer after operation. See Table 3 for details.
Table 3.
Comparison of gastrointestinal function recovery rating between the two groups
| Groups | Gastrointestinal function recovery rating | Rate of excellent and good | ||
|---|---|---|---|---|
|
| ||||
| Excellent | Good | Poor | ||
| Control group (n=49) | 24 | 11 | 14 | 35/49 |
| Observation group (n=49) | 33 | 13 | 3 | 46/49 |
| χ2 | 8.584 | 7.117 | ||
| P | 0.014 | 0.008 | ||
Discussion
The routine preoperative gastrointestinal preparation and long-term diet restrictions in patients with ovarian cancer have led to the lack of blood volume before induction. At the same time, patients with ovarian cancer are often complicated with multiple system diseases, organ dysfunction and anterograde decline, which further lead to the decline of various regulatory capacities of the body. In addition, a large amount of fluid is lost during the operation. Thus, without effective correction for the low volume condition, organ perfusion insufficiency and organ function damage can be induced. Conversely, excessive infusion volume will lead to tissue edema, and it ultimately affects the recovery of patients [22]. Optimal fluid management maintains an effective circulation volume to ensure tissue perfusion and avoid tissue edema to promote good recovery in patients. Therefore, effective monitoring means are an important prerequisite for liquid management. At present, the related indexes of intraoperative anesthesia monitoring volume mainly include central venous pressure (CVP), blood pressure, heart rate, etc. However, central venous pressure is affected by the contractility of the body position and the volume of vessels, the heart rate is usually affected by anesthesia factors, and the current target level of mean arterial pressure is defined by this. Therefore, the above indicators lack a high level of accuracy, and have the characteristics of insensitivity and hysteresis. Thus, they do not necessarily reflect the volume state accurately and are unable to provide an accurate dose-response relationship for volume therapy. Excessive or insufficient fluid resuscitation in the process of clinical application easily induces a series of complications [23]. Urine volume pulmonary capillary wedge pressure (PCWP) was once considered as the gold standard for hemodynamic monitoring. However, in the actual process, the related operation procedure is very complex and the resulting complications are serious, such as cardiac arrest, pulmonary artery rupture, as well as pneumothorax and papillary muscle injury, etc. Through real-time monitoring of hemodynamic parameters and effective monitoring of cardiac pump function, volume load and lung water index, PICCO can assess in a timely manner the body’s demand for fluid with accurate guidance on the fluid resuscitation and rationalize a good rehydration plan, so as to maintain the necessary corresponding hemodynamic indexes in the average or above-average range. Thus, PICCO helps to maintain adequate organ perfusion, which ensures the balance of oxygen supply and demand, and improves tissue metabolism. Besides, PICCO has achieved good clinical effects in intestinal surgery for colon cancer, rectal cancer, and gastric cancer [24,25].
Current studies have confirmed that there are many gastrointestinal dysfunction related factors during abdominal surgery, including ischemia and hypoxia caused by intestinal mucosal hypo-perfusion due to insufficient volume or decreased cardiac output and mucosal edema caused by excessive fluid infusion. However, edema caused by excessive fluid infusion is primary, so the recovery of gastrointestinal function also reflects the level of intraoperative fluid management for ovarian cancer. The results of our present study showed that the first exhaust time of the observation group was much earlier than that of the control group, and the gastrointestinal function level was also much better than that of the control group. This may be related to the fact that patients in the observation group had minor intestinal edema due to less infusion volume and the optimized liquid treatment which improved the microcirculation of gastrointestinal tissue. The operation in the observation group effectively improved the tissue oxygen supply of the intestinal tract and promoted the recovery of gastrointestinal function, which were similar to previous research reports [26,27]. In addition, the urine volume of the observation group was less than that of the control group with no statistical significance. On the one hand, our results may be related to the small sample size of individuals in this research, on the other hand, urine volume is related to renal function, cardiac function and preoperative food and drinking of patients; so these results needs further study.
The time to first get out of bed after surgery and total length of hospital stay are important reference indexes to evaluate the recovery of patients. In this study, we explored the effects of PICCO guided fluid resuscitation on postoperative functional recovery from cytoreductive surgery for ovarian cancer patients. The results showed that the time to get out of bed after surgery was earlier and total length of hospital stay of patients in the observation group was shorter than those in the control group. It is possible that the fluid resuscitation scheme optimized by PICCO helps to reduce the stress response and tissue edema, promotes the recovery of patients, thus reducing the length of hospital stay and bed rest time, which also further verifies previous research reports [28,29]. However, the parameters of PICCO in this study refer to the normal ranges of the body, and the specified range is relatively large. Although certain clinical effects have been achieved, the precise indicators of PICCO for ovarian cancer surgery still need more evidence-based results.
In conclusion, during the process of guiding the fluid management, PICCO effectively optimizes the fluid supplement scheme, maintains the stability of the internal environment, and reduces the edema of the gastrointestinal tract and systemic tissues. In addition, PICCO can also be widely used in the clinic because it effectively promoted the rapid recovery of postoperative gastrointestinal function and shortened the total length of hospital stay. However, this study is a single center study with a small sample size, which needs a multi-center and larger sample population of study to further confirm the guiding effects of PICCO in fluid resuscitation during ovarian cancer reduction surgery. In addition, serological indicators are necessary to evaluate the guiding role of PICCO in fluid management during ovarian cancer surgery which may be used as important supplemental information for the improvement of PICCO research.
Acknowledgements
This work was supported by the Xiaoping Chen Foundation for the Development of Science and Technology of Hubei Province (CXPJJH118000017-02-03).
Disclosure of conflict of interest
None.
References
- 1.Liu Y, He X, Chen Y, Cao D. Long non-coding RNA LINC00504 regulates the Warburg effect in ovarian cancer through inhibition of miR-1244. Mol Cell Biochem. 2020;464:39–50. doi: 10.1007/s11010-019-03647-z. [DOI] [PubMed] [Google Scholar]
- 2.Kratzer TB, Weinstein SJ, Albanes D, Mondul AM. Vitamin D binding protein and risk of renal cell carcinoma in the prostate, lung, colorectal and ovarian cancer screening trial. Int J Cancer. 2020;147:669–674. doi: 10.1002/ijc.32758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muller P, Woods L, Walters S. Temporal and geographic changes in stage at diagnosis in England during 2008-2013: a population-based study of colorectal, lung and ovarian cancers. Cancer Epidemiol. 2020;67:101743. doi: 10.1016/j.canep.2020.101743. [DOI] [PubMed] [Google Scholar]
- 4.Grundy A, Ho V, Abrahamowicz M, Parent M, Siemiatycki J, Arseneau J, Gilbert L, Gotlieb WH, Provencher DM, Koushik A. Lifetime recreational moderate-to-vigorous physical activity and ovarian cancer risk: a case-control study. Int J Cancer. 2020;146:1800–1809. doi: 10.1002/ijc.32513. [DOI] [PubMed] [Google Scholar]
- 5.González-Martín A, Pothuri B, Vergote I, DePont Christensen R, Graybill W, Mirza MR, McCormick C, Lorusso D, Hoskins P, Freyer G, Baumann K, Jardon K, Redondo A, Moore RG, Vulsteke C, O’Cearbhaill RE, Lund B, Backes F, Barretina-Ginesta P, Haggerty AF, Rubio-Pérez MJ, Shahin MS, Mangili G, Bradley WH, Bruchim I, Sun K, Malinowska IA, Li Y, Gupta D, Monk BJ. Niraparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med. 2019;381:2391–2402. doi: 10.1056/NEJMoa1910962. [DOI] [PubMed] [Google Scholar]
- 6.Lu YR, Zhen S. Comparison of clinical efficacy between laparoscopic and open surgery for early ovarian cancer. Systems Med. 2019 [Google Scholar]
- 7.Al Mutairi N, Le T. Does neoadjuvant chemotherapy impact prognosis in advanced-stage epithelial ovarian cancer optimally debulked at surgery? J Obstet Gynaecol Can. 2019;41:185–190. doi: 10.1016/j.jogc.2018.05.031. [DOI] [PubMed] [Google Scholar]
- 8.Xiao B, Yu GM, Sun QS. Efficacy of neoadjuvant chemotherapy combined with tumor cell reduction surgery in the treatment of III-IV ovarian cancer. The Pract J of Cancer. 2017 [Google Scholar]
- 9.Griffiths CT, Grogan RH, Hall TC. Advanced ovarian cancer: primary treatment with surgery, radiotherapy, and chemotherapy. Cancer. 1972;29:1–7. doi: 10.1002/1097-0142(197201)29:1<1::aid-cncr2820290102>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 10.Bergström BS. Lift-assisted laparoscopy in hysterectomy: a retrospective study of 32 consecutive cases. ISRN Minim Invasive Surg. 2015;2013:1–4. [Google Scholar]
- 11.Wei S, Yu-Han Z, Wei-Wei J, Hai Y. The effects of intravenous lidocaine on wound pain and gastrointestinal function recovery after laparoscopic colorectal surgery. Int Wound J. 2020;17:351–362. doi: 10.1111/iwj.13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qiang H, Sun YS. Effect of early enteral nutrition on laparoscopic common bile duct exploration with enhanced recovery after surgery protocols. Eur J Clin Nutr. 2020;74:666. doi: 10.1038/s41430-020-0565-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bounameaux H, Khabiri E, Huber O, Schneider PA, Didier D, de Moerloose P, Reber G. Value of liquid crystal contact thermography and plasma level of D-dimer for screening of deep venous thrombosis following general abdominal surgery. Thromb Haemost. 1992;67:603–606. [PubMed] [Google Scholar]
- 14.Teich N, Keim V. Hereditary chronic pancreatitis: diagnosis and management. Dis Pan. 2008 [Google Scholar]
- 15.Erikitola OO, Siempis T, Foot B, Lockington D. The incidence and management of persistent cystoid macular oedema following uncomplicated cataract surgery-a Scottish Ophthalmological Surveillance Unit study. Eye (Lond) 2021;35:584–591. doi: 10.1038/s41433-020-0908-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Batista A, Vera J, Pozo D. Multi-objective admission planning problem: a two-stage stochastic approach. Health Care Manag Sci. 2020;23:51–65. doi: 10.1007/s10729-018-9464-4. [DOI] [PubMed] [Google Scholar]
- 17.Qin XD, Liu PF, Wang QL. Pulse indicating continuous cardiac output monitoring technique for patients with acute heart failure. Trauma Crit Care Med. 2018 [Google Scholar]
- 18.Duan J, Cong LH, Wang H, Zhang Y, Wu XJ, Li G. Iconography: clinical evaluation compared to the pulse indicator continuous cardiac output system in the hemodynamic assessment of critically ill patients. J Am Emerg Med. 2014;32:629–633. doi: 10.1016/j.ajem.2014.03.023. [DOI] [PubMed] [Google Scholar]
- 19.Yang YP, Li YQ, Long QF, Zhu M, Fan XX, Fang Y, Guo SW. Clinical significances of PICCO monitoring in the capacity management of patients with severe craniocerebral injury. Prog Mod Biomed. 2017 [Google Scholar]
- 20.Forstner R, Sala E, Kinkel K, Spencer JA. ESUR guidelines: ovarian cancer staging and follow-up. Eur Radiol. 2010;20:2773–2780. doi: 10.1007/s00330-010-1886-4. [DOI] [PubMed] [Google Scholar]
- 21.Thompson C, McCormick C, Kamran W, O’Riain C, Norris L, Gallagher D, Gleeson N. Risk reduction surgery (RRS) for tubo-ovarian cancer in an Irish gynaecological practice: an analysis of indications and outcomes. Ir J Med Sci. 2018;187:789–794. doi: 10.1007/s11845-017-1717-6. [DOI] [PubMed] [Google Scholar]
- 22.Wu Y, Ma YD, Wu SK. Clinical application of PICCO volume indexes in fluid resuscitation of septic shock. Mod J Integr Tradit Chin West Med. 2013 [Google Scholar]
- 23.Kikuchi G, Yamasaki Y, Takiguchi M, Yabuta Y, Kato H, Nakamura T, Kinefuchi Y, Amano M. Complication of CVP catheter--embolization and self-knotting. Masui. 1982;31:1147–1150. [PubMed] [Google Scholar]
- 24.Ersoy Z, Ozdemirkan A, Zeyneloglu P, Pirat A, Torgay A, Kayhan Z, Haberal M. PiCCO monitoring during liver transplantation for pediatric patients. Transplantation. 2018:102. [Google Scholar]
- 25.Horster S, Stemmler HJ, Strecker N, Brettner F, Hausmann A, Cnossen J, Parhofer KG, Nickel T, Geiger S. Cardiac output measurements in septic patients: comparing the accuracy of USCOM to PiCCO. Crit Care Res Pract. 2012;2012:270631. doi: 10.1155/2012/270631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wisén O, Johansson C. Gastrointestinal function in obesity: motility, secretion, and absorption following a liquid test meal. Metabolism. 1992;41:390–395. doi: 10.1016/0026-0495(92)90073-j. [DOI] [PubMed] [Google Scholar]
- 27.Aurora A, Roe JL, Umoh NA, Dubick M, Wenke JC, Walters TJ. Fresh whole blood resuscitation does not exacerbate skeletal muscle edema and long-term functional deficit after ischemic injury and hemorrhagic shock. J Trauma Acute Care Surg. 2018;84:786–794. doi: 10.1097/TA.0000000000001806. [DOI] [PubMed] [Google Scholar]
- 28.Bundgaard-Nielsen M, Holte K, Secher NH, Kehlet H. Monitoring of peri-operative fluid administration by individualized goal-directed therapy. Acta Anaesthesiol Scand. 2007;51:331–340. doi: 10.1111/j.1399-6576.2006.01221.x. [DOI] [PubMed] [Google Scholar]
- 29.Kushimoto S, Taira Y, Kitazawa Y, Okuchi K, Sakamoto T, Ishikura H Pulmonary ESG, Picco. Prospective multicenter study on quantitative pathophysiological assessment of acute pulmonary edema: results of intermediate analysis. Inj Int J Care Inj. 2011;42:1484–1490. [Google Scholar]


