Abstract
Objective: To observe the efficacy of intrauterine Bakri balloon tamponade (IBBT) combined with ascending uterine artery ligation (AUAL) in the treatment of postpartum hemorrhage (PPH) due to uterine inertia after cesarean section. Methods: A total of 92 patients with PPH due to uterine inertia after cesarean section were divided into a study group (n=46) and a control group (n=46) in accordance with the random number table. The control group was treated with IBBT alone, while the study group was treated with IBBT combined with AUAL. The clinical efficacies, hemorrhage, surgical duration, hospital stay, hemorrhage rate after removal of tamponade, recurrence rate of PPH, changes in coagulation function and quality of life were compared between the two groups. Results: The overall response rate (ORR) in the study group was 95.65%, remarkably higher than that of 80.43% in the control group (P < 0.05). The study group had a lesser amount of hemorrhage at 2 h and 24 h after surgery, a longer surgical duration, a shorter hospital stay, and lower hemorrhage rate after removal of tamponade and recurrence rate of PPH than the control group (P < 0.05). After treatment, prothrombin time, activated partial thromboplastin time and fibrinogen in the study group were markedly higher than those in the control group (P < 0.05). Compared with those before treatment, the scores of quality of life in the two groups were elevated at 3 months after treatment (P < 0.05), and the scores of quality of life in the study group were higher than those in the control group at 3 months after treatment (P < 0.05). Conclusion: IBBT combined with AUAL can effectively alleviate hemorrhage and improve coagulation function and quality of life of patients with PPH due to uterine inertia after cesarean section, exhibiting a definite efficacy and a high safety profile.
Keywords: Postpartum hemorrhage, uterine inertia, intrauterine Bakri balloon tamponade, ligation of the ascending uterine artery
Introduction
Postpartum hemorrhage (PPH) refers to blood loss exceeding 500 ml within 24 h after vaginal delivery, with more than 80% of the hemorrhage concentrated within 2 h after delivery, which is the main cause of maternal death [1]. The causes of PPH include uterine inertia, soft birth canal injury, placental factors and coagulation dysfunction. Among them, uterine inertia is the main inducing factor, and more than 70% of PPH is caused by uterine inertia [2]. Previously, conservative treatment was mostly used in patients with PPH due to uterine inertia after cesarean section. However, if conservative treatment was ineffective, intrauterine Bakri balloon tamponade (IBBT) was usually performed. IBBT has multiple advantages, such as convenient operations, satisfactory hemostatic effects and short indwelling time [3,4]. The long-term clinical practices suggest that some patients still have PPH after the removal of Bakri balloon tamponade, affecting the therapeutic effects [5,6]. Therefore, how to effectively treat PPH caused by uterine inertia after cesarean section is a tough issue facing clinical gynecologists at present.
Recently, the ascending uterine artery ligation (AUAL) has been gradually applied in the treatment of PPH due to uterine inertia after cesarean section, with definite efficacy, effective improvement of uterine ischemia, promotion of uterine contraction, and relief of hemorrhage [7,8]. At present, there are few clinical reports on IBBT combined with AUAL in the treatment of PPH due to uterine inertia after cesarean section. In view of this, IBBT combined with AUAL was used in the treatment of 46 patients with PPH due to uterine inertia after cesarean section, aiming to provide more valuable references for the clinical treatment of such PPH.
Materials and methods
Clinical data
From July 2018 to February 2020, a total of 92 patients with PPH due to uterine inertia after cesarean section were divided into a study group (n=46) and a control group (n=46) in accordance with the random number table. Inclusion criteria: patients aged 20-40 years; singleton deliveries; > 500 mL of hemorrhage within 2 h after delivery; ineffective conservative massage and medication for promoting uterine contraction; voluntary signing of informed consent forms; PPH caused by uterine inertia during cesarean section. Exclusion criteria: those who were unable to tolerate surgery; complicated with pregnancy-induced hypertension syndrome, gestational diabetes mellitus, other types of obstetric complications and severe dysfunction of important organs; PPH caused by soft birth canal injury, uterine malformation and placenta previa; poor compliance; non-cooperation with the study. This study was reported to Tai’an City Central Hospital and approved by the Medical Ethics Committee.
Methods
(1) Prenatal and delivery treatment: the comprehensive assessment of high-risk factors for all patients was conducted before delivery; the calcium preparation was used to enhance the sensitivity of patients to drugs that promoted uterine contraction; after delivery, Carboprost Tromethamine injection was administrated to the patients with high-risk factors via an intramuscular injection. (2) Surgical method: the control group was treated with IBBT alone: when the PPH due to uterine inertia was diagnosed, a Bakri balloon tamponade (Cook Medical, USA) was immediately inserted into the uterine incision and then injected with 200-300 mL of NaCl solution (concentration: 0.9%), followed by the balloon tamponade handle to fix the leg of the patient. The study group was treated with IBBT combined with AUAL. The surgical method of IBBT was the same as that in the control group. When the AUAL was performed, the operation on the cesarean section incision of the patient was conducted. First, the needle was inserted at the avascular site, 1 cm below the top of the uterine incision and 1 cm above the bladder. Then, the needle was inserted from the uterine cavity, and the needle was inserted from the corresponding posterior wall of the uterus, followed by inserting the needle through bypassing the site of great vessels. Next, knotting was performed at the site of great vessels through the latum, and whether there was the oozing of blood at the needle eye was carefully detected. If there was oozing of blood, No.4 silk thread would be used to conduct sewing in the shape of “8” and stop bleeding. All surgical operations were performed in strict accordance with the principle of aseptic operations, and were completed by the same team of surgeons and nursing staff. After surgery, the two groups received conventional anti-infection treatment of the third generation cephalosporins via an intravenous drip, and those with an allergic constitution received azithromycin and clarithromycin via an intravenous drip for 3 d.
Observational indices
Clinical efficacy [9]
Marked response: after treatment, the amount of vaginal hemorrhage was less than 30 ml/h, the uterine contraction state was good, and the hemorrhage was stopped shortly. Moderate response: after treatment, the amount of vaginal hemorrhage was 30-50 ml/h, the uterine contraction state was good, and the amount of hemorrhage was gradually reduced. No response: after treatment, the amount of vaginal hemorrhage was more than 50 ml/h, and there was uterine inertia. The ORR is the sum of marked response rate and moderate response rate.
Hemorrhage
The amount of preoperative hemorrhage and the amount of hemorrhage at 2 h and 24 h after surgery were measured. The amount of PPH was measured using volumetric method combined with weighing method, and 1 g = 0.95 mL of blood.
Surgical duration and hospital stay
The surgical duration and hospital stay of the two groups were recorded.
Assessment on safety profile
The hemorrhage rate after removal of tamponade and recurrence rate of PPH in the two groups were calculated. The assessment criteria for recurrent PPH were as follows: after the delivery of the fetus or the removal of the balloon tamponade, there were still the symptoms of uterine hemorrhage, and the total amount of hemorrhage was more than > 1000 ml. Meanwhile, uterine massage and medication for promoting uterine contraction were ineffective.
Coagulation function
4 ml of venous blood was collected before and after treatment, and prothrombin time (PT), activated partial thromboplastin time (APTT) and fibrinogen (FIB) were measured using a fully automatic coagulometer.
Quality of life
Before treatment and at 3 months after treatment, QLQ-30 [10] was used to assess the quality of life in the two groups, including emotional and physical functions. A higher score indicates a higher quality of life.
Statistical analysis
SPSS 22.0 was adopted for statistical analysis. The measurement data were expressed as x̅ ± sd. The comparison between groups was detected using the independent sample t test, and the comparison within groups was detected using the paired sample t test. The enumeration data were expressed as [n (%)], and detected using χ2 test. P < 0.05 indicated a statistically significant difference.
Results
General data
There was no statistically significant difference in age, gestational weeks, type of parturient, and weight between the two groups (P > 0.05), which were comparable (Table 1).
Table 1.
Comparison of general data between the two groups
| Group | Mean age (years) | Mean gestational week (week) | Mean weight (kg) | Type of parturient | |
|---|---|---|---|---|---|
|
| |||||
| Primipara | Multipara | ||||
| Control group (n=46) | 29.35±3.77 | 38.65±1.73 | 73.15±6.80 | 34 | 12 |
| Study group (n=46) | 29.28±3.58 | 38.57±1.62 | 73.02±6.37 | 36 | 10 |
Clinical efficacy
The overall response rate (ORR) in the study group was 95.65%, markedly higher than that of 80.43% in the control group (P < 0.05). This exhibited that IBBT combined with AUAL was superior to IBBT in the treatment of PPH due to uterine inertia after cesarean section (Table 2).
Table 2.
Comparison of efficacies between the two groups [n (%)]
| Group | Marked response | Moderate response | No response | ORR |
|---|---|---|---|---|
| Control group (n=46) | 21 (45.65) | 16 (33.33) | 9 (19.57) | 37 (80.43) |
| Study group (n=46) | 29 (63.04) | 15 (32.61) | 2 (4.35) | 44 (95.65)# |
Note: compared with the control group;
P < 0.05.
Hemorrhage
There was no statistically significant difference in the amount of preoperative hemorrhage between the two groups (P > 0.05). The amount of hemorrhage at 2 h and 24 h after surgery in the study group was less than that in the control group (P < 0.05). This suggested that TIBBT combined with AUAL could markedly improve the hemorrhage of patients with PPH due to uterine inertia after cesarean section (Table 3).
Table 3.
Comparison of postpartum hemorrhage between the two groups (x̅ ± s, ml)
| Group | Amount of preoperative hemorrhage | Amount of hemorrhage at 2 h after surgery | Amount of hemorrhage at 24 h after surgery |
|---|---|---|---|
| Control group (n=46) | 653.80±75.33 | 63.35±11.60 | 436.68±85.90 |
| Study group (n=46) | 662.41±68.90 | 47.57±9.25### | 358.46±82.37### |
Note: compared with the control group;
P < 0.001.
Surgical duration and hospital stay
The study group had a longer surgical duration and a shorter hospital stay than the control group (P < 0.05). Although TIBBT combined with AUAL led to a longer surgical duration, it could effectively promote the recovery of patients and shorten the hospital stay (Figure 1).
Figure 1.
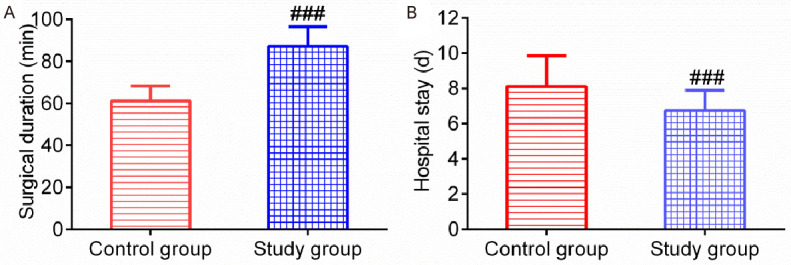
Comparison of surgical duration and hospital stay between the two groups. Note: (A) Surgical duration; (B) Hospital stay. Compared with the control group, ###P < 0.001.
Assessment on safety profile
The study group had lower hemorrhage rate after removal of tamponade and recurrence rate of PPH than the control group (P < 0.05). This revealed that TIBBT combined with AUAL exhibited a high safety profile (Table 4).
Table 4.
Comparison of hemorrhage rate after removal of tamponade and recurrence rate of PPH between the two groups [n (%)]
| Group | Hemorrhage rate after removal of tamponade | Recurrence rate of PPH |
|---|---|---|
| Control group (n=46) | 7 (15.22) | 6 (13.04) |
| Study group (n=46) | 0 (0.00)# | 0 (0.00)# |
Note: compared with the control group;
P < 0.05.
Coagulation function
There was no statistically significant difference in PT, APTT and FIB between the two groups before treatment (P > 0.05). Compared with those before treatment, PT, APTT and FIB increased in the two groups after treatment (P < 0.05), and PT, APTT and FIB in the study group were higher than those in the control group after treatment (P < 0.05). This demonstrated that TIBBT combined with AUAL could remarkably improve the coagulation function of patients with PPH due to uterine inertia after cesarean section (Figure 2).
Figure 2.
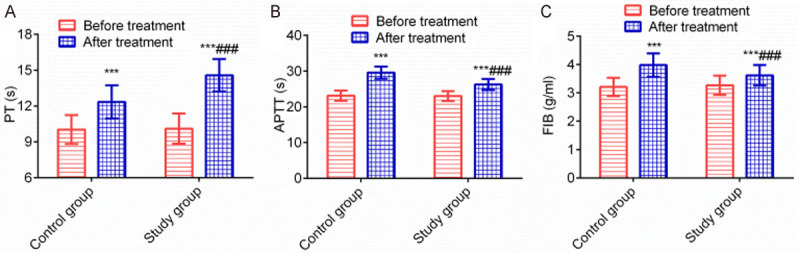
Comparison of coagulation functions between the two groups. Note: (A) PT; (B) APTT; (C) FIB. Compared with this group before treatment, ***P < 0.001; compared with the control group, ###P < 0.001.
Quality of life
There was no statistically significant difference in the scores of quality of life between the two groups before treatment (P > 0.05). Compared with those before treatment, the scores of quality of life increased in the two groups at 3 months after treatment (P < 0.05), and the scores of quality of life in the study group were higher than those in the control group (P < 0.05). This showed that TIBBT combined with AUAL could significantly improve the quality of life of patients with PPH due to uterine inertia after cesarean section (Figure 3).
Figure 3.
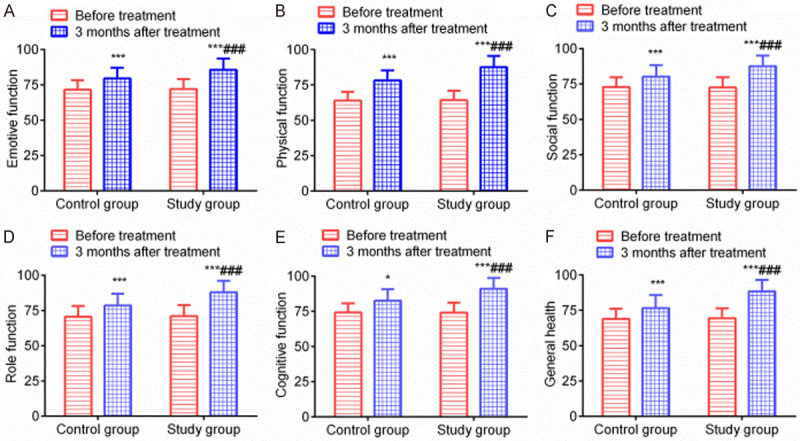
Comparison of quality of life between the two groups (points). Note: (A) Emotional function score; (B) Physical function score; (C) Social function score; (D) Role function score; (E) Cognitive function score; (F) Overall health score. Compared with this group before treatment, ***P < 0.001; compared with the control group, ###P < 0.001.
Discussion
The causes of PPH are uterine inertia, soft birth canal laceration, placental factors and coagulation dysfunction, which coexist or cause and have a cause-and-effect relationship [11]. Uterine inertia is the most common cause of PPH, and more than 70% of PPH is attributable to uterine inertia. This is mainly due to the reason that the contractile weakness of uterine muscle fibers in different directions after delivery of the fetus cannot effectively compress the blood vessels between muscle bundles, thus causing PPH [12]. It has been found in clinical practice that the incidence rate of PPH is 2.0-3.0%, mainly including a large amount of acute vaginal hemorrhage or a small amount of persistent vaginal hemorrhage, and in severe cases, it may lead to maternal hemorrhagic shock, posing a great threat to their health [13]. Therefore, the effective treatment of PPH is of great significance.
In this study, IBBT combined with AUAL was applied in the treatment of PPH due to uterine inertia after cesarean section. The results showed that compared with the control group, the study group had a higher clinical efficacy, a lesser amount of hemorrhage at 2 h and 24 h after surgery, a longer surgical duration, a shorter hospital stay, and lower hemorrhage rate after removal of tamponade and recurrence rate of PPH. Liao et al. [14] indicated that compared with IBBT alone, IBBT combined with AUAL caused a lesser amount of postoperative hemorrhage, a shorter hospital stay and a lower incidence rate of complications, which was basically consistent with the results of this study. This showed that IBBT combined with AUAL could effectively alleviate hemorrhage, promote physical recovery and shorten the hospital stay of patients with PPH due to uterine inertia after cesarean section, exhibiting a definite efficacy. This may be due to the reason that IBBT can be performed through vaginal and cesarean section incisions. The incisions are simple, the operation is convenient, and the compression area is large. Additionally, the incisions do not negatively affect the reproductive function of the patients [15,16]. The hemostatic mechanism is as follows: ① After complete placenta detachment, PPH is easy to occur due to the uterine inertia and the wide opening of venous sinus, and the insertion of Bakri balloon tamponade and injection of normal saline can produce a hydrostatic pressure on the inner wall of the patient’s uterus. Since this hydrostatic pressure is higher than the intrauterine arterial pressure, it can help hemostasis by compression, activate the coagulation function of the patient’s body, and expedite local thrombosis, thus achieving hemostasis [17]; ② The insertion of Bakri balloon tamponade can compress uterine artery to a certain extent, so as to reduce the blood flow of uterine and intrauterine arteries. This can not only activate the coagulation function of patients to play a hemostatic role, but also increase the secretion of coagulation factors and prostaglandins (PGs), so as to promote local aggregation of platelets and contractions, thereby achieving hemostasis by compression, blocking uterine dissection surface, and achieving the packing of intrauterine venous sinus [18]; ③ Due to the design of double-lumen tube of Bakri balloon tamponade, the balloon tamponade can be compressed to a certain extent during uterine contraction, and the external capacity bag can monitor the intrauterine pressure. If the intrauterine pressure rises, it will properly release the liquid to prevent the uterus from rupturing, and the vulnerable parts of the scarred uterus from tearing. If the intrauterine pressure is insufficient, fluid will be injected properly, so as to achieve hemostasis by compression and packing hemostasis [19]. Although Bakri balloon tamponade has multiple advantages, some patients may have the risk of recurrent hemorrhage after removal of tamponade or recurrent PPH [20]. AUAL is a kind of invasive surgery, which can reduce the blood supply of myometrium to a certain extent, thus diminishing the blood flow of intrauterine vein and venous sinus, activating the coagulation function of the body, making local aggregation of platelets, and achieving the purpose of hemostasis [21]. Meanwhile, it can also exert longitudinal pressure on the uterus to compress the blood vessels between uterine walls, promote the closure of blood sinuses, diminish the blood flow velocity between uterine walls, thereby exerting the hemostatic effects [22,23]. Combined with IBBT, it can further enhance the hemostatic effects, reduce the amount of postoperative IBBT, and improve the recurrence rate of PPH, which are conducive to shortening the hospital stay of patients [24].
Clinical findings have shown that PPH can damage the coagulation function of patients, and even lead to deaths in severe cases. Therefore, the effective improvement of the coagulation function is of great significance to reduce the mortality and alleviate the conditions [25]. In this study, compared with those before treatment, PT, APTT and FIB increased in the two groups after treatment, and PT, APTT and FIB in the study group were higher than those in the control group after treatment. Lin et al. [26] used intrauterine balloon compression for hemostasis in women with placenta previa, and postoperative APTT, TT and PT were significantly lower than those in the control group received uterine gauze packing for hemostasis, which was similar to the results in this study. This exhibited that IBBT combined with AUAL could effectively improve the coagulation function, alleviate the conditions, and promote the recovery of patients with PPH due to uterine inertia after cesarean section. Quality of life is an important index to assess the prognosis of patients. In this study, compared with those before treatment, the scores of quality of life increased in the two groups at 3 months after treatment, and the scores of quality of life in the study group were higher than those in the control group at 3 months after treatment. This suggested that IBBT combined with AUAL could remarkably improve the quality of life and prognosis of patients with PPH due to uterine inertia after cesarean section.
In summary, IBBT combined with AUAL can effectively alleviate hemorrhage and improve coagulation function and quality of life of patients with PPH due to uterine inertia after cesarean section, exhibiting a definite efficacy and a high safety profile. However, it is worth noting that the study results may be biased to a certain extent as a result of insufficient cases collected in this study. Therefore, the future studies with a larger number of cases should be performed for further investigation.
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure of conflict of interest
None.
References
- 1.Evensen A, Anderson JM, Fontaine P. Postpartum hemorrhage: prevention and treatment. Am Fam Physician. 2017;95:442–449. [PubMed] [Google Scholar]
- 2.Waks A, Tabsh K, Tabsh K, Afshar Y. Balloon uterine tamponade device after peripartum hysterectomy for morbidly adherent placenta. Obstet Gynecol. 2018;132:643–646. doi: 10.1097/AOG.0000000000002792. [DOI] [PubMed] [Google Scholar]
- 3.Sentilhes L, Maillard F, Brun S, Madar H, Merlot B, Goffinet F, Deneux-Tharaux C. Risk factors for chronic post-traumatic stress disorder development one year after vaginal delivery: a prospective, observational study. Sci Rep. 2017;7:8724. doi: 10.1038/s41598-017-09314-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen H, Zou S, Yang J, Deng S, Cai J, Wang Z. Maternal and neonatal outcomes of pregnancy at 39 weeks and beyond with mild gestational diabetes mellitus. Ginekol Pol. 2017;88:366–371. doi: 10.5603/GP.a2017.0069. [DOI] [PubMed] [Google Scholar]
- 5.Li H, Liu H, Huang S, Pan C. Meta-analysis of efficacy and safety of intrauterine Bakri balloon tamponade and intrauterine gauze tamponade in the treatment of postpartum hemorrhage. Hainan Med J. 2020;31:388–394. [Google Scholar]
- 6.Woiski M, de Visser S, van Vugt H, Dijkman A, Schuitemaker N, van Meir C, Middeldorp J, Huisjes A, Mol BW, Molkenboer J, Moonen-Delarue D, Oudijk M, van Rheenen-Flach L, Rijnders R, Pernet P, Porath M, de Wit S, Grol R, Scheepers H, Hermens R. Evaluating adherence to guideline-based quality indicators for postpartum hemorrhage care in the netherlands using video analysis. Obstet Gynecol. 2018;132:656–667. doi: 10.1097/AOG.0000000000002781. [DOI] [PubMed] [Google Scholar]
- 7.Seow KM, Chen KH, Wang PH, Lin YH, Hwang JL. Carbetocin versus oxytocin for prevention of postpartum hemorrhage in infertile women with twin pregnancy undergoing elective cesarean delivery. Taiwan J Obstet Gynecol. 2017;56:273–275. doi: 10.1016/j.tjog.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Lan JZ, Liu JL. Application of bilateral uterine artery ascending branch ligation+modified uterine brace suture in intractable postpartum hemorrhage during cesarean delivery. J Hebei Med Univ. 2018;39:59–62. [Google Scholar]
- 9.Yu S, Liu P, Wang RY. Comparative analysis of bakri balloon tamponade and intrauterine gauze packing for postpartum hemor-rhage after c-section for central placenta previa. Clin Misdiagn Misther. 2020;33:86–90. [Google Scholar]
- 10.Zhang HZ, Liu H. Effect of misoprostol combined with oxytocin on postpartum hemorrhage and quality of life of patients with uterine atony postpartum hemorrhage. Drug Eval. 2018;15:52–54. 64. [Google Scholar]
- 11.Dai MJ, Jin GX, Lin JH, Zhang Y, Chen YY, Zhang XB. Pre-cesarean prophylactic balloon placement in the internal iliac artery to prevent postpartum hemorrhage among women with pernicious placenta previa. Int J Gynaecol Obstet. 2018;142:315–320. doi: 10.1002/ijgo.12559. [DOI] [PubMed] [Google Scholar]
- 12.Zafran N, Gerszman E, Garmi G, Zuarez-Easton S, Salim R. The impact of postpartum cervical tear on the occurrence of preterm birth in subsequent pregnancy. Arch Gynecol Obstet. 2017;296:199–204. doi: 10.1007/s00404-017-4410-0. [DOI] [PubMed] [Google Scholar]
- 13.Muraca GM, Sabr Y, Lisonkova S, Skoll A, Brant R, Cundiff GW, Joseph KS. Perinatal and maternal morbidity and mortality after attempted operative vaginal delivery at midpelvic station. CMAJ. 2017;189:E764–E772. doi: 10.1503/cmaj.161156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liao S, Luo Z, He X. Bakri balloon tamponade combined with ligation of ascending uterine artery for postpartum hemorrhage after cesarean section. Clin Med Eng. 2019;26:1605–1606. [Google Scholar]
- 15.Pan AJ, Yang TJ, Mei Q, Zhang L, Chen L, Wu DB, Liu B. [Retrospectively analysis on 95 postpartum hemorrhage women treated with obstetrics and gynecology in intensive care unit] . Zhonghua Yi Xue Za Zhi. 2017;97:2248–2252. doi: 10.3760/cma.j.issn.0376-2491.2017.29.003. [DOI] [PubMed] [Google Scholar]
- 16.Deffieux X, Vinchant M, Wigniolle I, Goffinet F, Sentilhes L. Maternal outcome after abdominal packing for uncontrolled postpartum hemorrhage despite peripartum hysterectomy. PLoS One. 2017;12:e0177092. doi: 10.1371/journal.pone.0177092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El Refaeey AEA, Abdelfattah H, Mosbah A, Gamal AM, Fayla E, Refaie W, Zaied A, Barakat RI, Seleem AK, Maher M. Is early intervention using Mansoura-VV uterine compression sutures an effective procedure in the management of primary atonic postpartum hemorrhage?: a prospective study. BMC Pregnancy Childbirth. 2017;17:160. doi: 10.1186/s12884-017-1349-x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 18.Ishibashi H, Miyamoto M, Soyama H, Shinmoto H, Murakami W, Nakatsuka M, Natsuyama T, Takano M, Yoshida M, Furuya K. Marginal sinus placenta previa is a different entity in placenta previa: a retrospective study using magnetic resonance imaging. Taiwan J Obstet Gynecol. 2018;57:532–535. doi: 10.1016/j.tjog.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Lio CF, Lee YH, Chan HY, Yu CC, Peng NJ, Chan HP. Posterior reversible encephalopathy syndrome in a postpartum hemorrhagic woman without hypertension: a case report. Medicine (Baltimore) 2017;96:e6690. doi: 10.1097/MD.0000000000006690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu CY, Zhu DM, Tan XY. Comparison of efficacies of gauze packing, Bakri balloon tamponade and modified B-Lynch suture in the treatment of refractory postpartum hemorrhage. J Chin Physician. 2019;21:920–922. [Google Scholar]
- 21.Salman L, Hiersch L, Shmueli A, Krispin E, Wiznitzer A, Gabbay-Benziv R. Complicated primary cesarean delivery increases the risk for uterine rupture at subsequent trial of labor after cesarean. Arch Gynecol Obstet. 2018;298:273–277. doi: 10.1007/s00404-018-4801-x. [DOI] [PubMed] [Google Scholar]
- 22.Fan XH. Effect of bilateral ascending uterine artery ligation on bleeding during cesarean section of central placenta previa. Matern Child Health Care China. 2017;32:2498–2499. [Google Scholar]
- 23.Zhang N, Lou WH, Zhang XB, Lin JH, Di W. Antepartum hemorrhage from previous-cesarean-sectioned uterus as a potential sign of uterine artery pseudoaneurysm. J Zhejiang Univ Sci B. 2017;18:441–444. doi: 10.1631/jzus.B1600528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang D, Xu S, Qiu X, Zhu C, Li Z, Wang Z, Hou H, Gao Y, Wang X, He P, Qin Y, Liu L. Early usage of Bakri postpartum balloon in the management of postpartum hemorrhage: a large prospective, observational multicenter clinical study in South China. J Perinat Med. 2018;46:649–656. doi: 10.1515/jpm-2017-0249. [DOI] [PubMed] [Google Scholar]
- 25.Zhang LY. Application of bilateral ascending uterine artery ligation combined with motherwort injection in treating hemorrhage due to uterine inertia after cesarean section and its effect on coagulation system and ovarian function. Modern J Integr Tradit Chin Western Med. 2017;26:2867–2870. [Google Scholar]
- 26.Lin QL, Huang LL, Lan JY. Effect of intrauterine balloon compression on placenta previa and oxidative stress. J Prevent Med Chin PLA. 2018;36:765–767. 774. [Google Scholar]


