Abstract
Objective: To determine the effect of respiration-related guidance and nursing on the respiratory function and living ability in elderly patients with chronic obstructive pulmonary disease (COPD). Methods: A total of 157 elderly patients with COPD admitted to our hospital between June 2016 and November 2019 were enrolled, and assigned into two groups according to difference nursing intervention methods. Among them, 72 cases were intervened by routine nursing as a control group (con group) and the rest 85 intervened by respiration-related guidance and nursing as a research group (res group). The two groups were compared in pulmonary and respiratory function indexes, and dyspnea, activities of daily living (ADL), Pittsburgh sleep quality index (PSQI), and MOS 36-Item Short-Form Health Survey (SF-36) scores before and after intervention as well as the nursing satisfaction after intervention. Results: After nursing intervention, compared with the con group, the res group showed significantly higher pulmonary function indexes (forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC) and greatly improved respiratory function indexes (arterial carbondioxide partial pressure (PaCO2), arterial partial pressure of oxygen (PaO2), and blood oxygen saturation (SaO2)), with significantly lower MMRC and PSQI scores and significantly higher SF-36 score, and nursing satisfaction. Conclusion: For elderly patients with COPD, respiration-related guidance and nursing can enhance their pulmonary function and respiratory function, relieve their dyspnea and sleep disorder, and improve their daily living ability, life quality and nursing satisfaction.
Keywords: Chronic obstructive pulmonary disease, respiration-related guidance and nursing, respiratory function, living ability
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic bronchitis and/or emphysema and a common preventable and treatable respiratory disease [1]. It is mainly characterized by persistent respiratory symptoms and airflow limitation caused by abnormal airway and/or alveoli, and obvious exposure to toxic particles or gases is the main cause of abnormal airway and/or alveoli [2]. COPD is mainly manifested by chronic bronchitis and emphysema in pathological changes [3]. People face a higher prevalence rate of COPD as they grow older, and the disease, with high disability rate and mortality rate, is highly common in the elderly, especially elderly smoking men, [4]. In recent years, with the change of people’s lifestyle and the aging of the population, the prevalence rate of COPD is growing annually [5]. The disease is mainly manifested by shortness of breath, dyspnea, chronic cough or expectoration, wheezing and chest tightness, and weight loss, and may even develop into cor pulmonale and respiratory failure in severe cases [6,7]. It is mainly diagnosed based on the comprehensive analysis of the history of smoking and other high-risk factors, clinical symptoms, signs and pulmonary function tests [8]. Long-term symptoms of cough, expectoration, and dyspnea and repeated hospitalization seriously impact the physical and mental health of patients with COPD, because it compromises their life quality and ability to work, study and daily activities, and increases their financial burden [9]. COPD develops in a progressive way, and is still incurable currently. It is mainly treated by drug therapy and non-drug therapy in clinical practice [10]. Drug therapy can alleviate patients’ symptoms, delay disease progression and reduce patients’ readmission rate, but non-drug therapy has captured increasing attention in recent years [11,12]. In addition to effective medical treatment, effective nursing intervention is also of great value in the rehabilitation of patients [13].
Respiration-related guidance and nursing is a novel nursing intervention mode, which is mainly to enhance patients’ respiratory function and achieve pulmonary rehabilitation by comprehensive nursing measures such as breathing training and guidance [14]. Measures of pulmonary rehabilitation is a primary intervention measure in the treatment of COPD and the cornerstone of its non-drug therapy, which can improve patients’ exercise ability, daily living ability, and self-efficacy, strengthen their muscle strength and relieve their dyspnea [15]. As living standards improve, people have increasingly higher awareness of health care and also make increasingly higher demand on nursing [16]. Currently, for elderly patients with COPD, conventional nursing cannot achieve the therapeutic effect well, and performs not well in restoring the respiratory function and life quality of patients [17]. At present, studies on the application of respiration-related guidance and nursing in elderly patients with COPD are rare.
Therefore, this study implemented respiration-related guidance and nursing for elderly patients with COPD to determine its effect on the respiratory function and living ability of such patients.
Materials and methods
General materials
A total of 157 elderly patients with COPD admitted to Jiangsu Province Hospital between June 2016 and November 2019 were enrolled, and assigned to two groups according to difference nursing intervention methods. Among them, 72 cases were intervened by routine nursing as a control group (con group) (52 males and 20 females between 60 and 80 years old, with a mean age of (68.53±9.53) years), and the rest 85 by respiration-related guidance and nursing as a research group (res group) (64 males and 21 females between 61 and 83 years old, with a mean age of (69.11±10.16) years).
Inclusion and exclusion criteria
Inclusion criteria: Patients meeting the diagnostic criteria of COPD [18]; Patients with pulmonary function at grade II-III; Patients at ≥60 years old; Patients with detailed clinical data; This study was approved by the Ethics Committee of our hospital, and all participants and their families signed informed consent forms after being informed of the study.
Exclusion criteria: Patients with severe hypertension or cardiovascular diseases; Patients with severe liver or kidney dysfunction; Patients with cognitive, language, or hearing impairment; Patients with mental illness or a family history of mental illness; Patients with comorbid malignant tumor, active tuberculosis, or other parenchymal lung diseases.
Nursing methods
Patients in the two groups were all given the same clinical treatment methods, including aerosol inhalation, anti-infection with antibiotics, maintenance of water electrolyte balance, expectoration and nutritional support. Patients in the con group were given routine nursing, including health education and guidance on medication, diet, and smoking cessation. All patients were given nursing intervention for 3 months.
Patients in the res group were given respiration-related guidance and nursing specifically as follows:
Respiratory tract cleaning: The nursing staff were arranged to instruct each patient to cough effectively with the back patted and chest tapped to remove respiratory secretions to improve the effect of respiratory exercise before the exercise.
Lip-constriction breathing: Each patient was instructed to take a half-sitting or sitting position, first take a deep breath with his/her nose under the close of mouth, and then slowly exhale the exhaust gas with lips contracted, with a breathing ratio of 2:1-3:1, 2 times/d, and at least 5 min/time.
Abdominal breathing: Each patient was instructed to keep standing or a supine position, with hands placed on his/her chest and abdomen, respectively, and then the patient was instructed to inhale deeply with nose while keeping chest still and bulging the abdomen, and exhale the air slowly by contracting lips while tightening the abdomen and pressing it, with a breathing ratio of 2:1-3:1, 2 times/d, and at least 10 min/time.
Aerobic exercise: Each patient was required to properly carry out aerobic exercise mainly based on short-distance walking, with exercise time determined according to the patient’s physical condition and not exceeding 20 min.
Breathing training under artificial resistance: A three-ball spirometry training instrument was adopted for training under artificial resistance. Specifically, each patient was asked to hold a mouth piece with mouth, hold the training instrument with the left hand, put the right hand under the rib and upper abdomen, and then slowly exhale and inhale to make the ball of the training instrument rise. During this process, the patient was required to prolong the inhalation time to make the ball rise as much as possible, keep inhaling to try to make the ball rise to the highest point of the scale, and hold breath for 2-3 s. Afterwards, the patient was asked to let go of the mouth piece and exhale air slowly. The patient was required to adjust breathing and undertake the training again after each deep breath, and 10-15 times of such training could be carried out each time.
Breathing exercise-based training: The training included inhaling quietly in a standing position and exhaling with body leaning forward, inhaling with arms upward and exhaling with hands pressing the abdomen, inhaling with arms extending horizontally and exhaling with arms downward, inhaling with upper limbs stretching straight forward and exhaling with hands pressing the abdomen, inhaling with hands holding the head and exhaling with body rotating 30°, inhaling with the upper limb lifting in a standing position and exhaling with body squatting; Abdominal-type lip-contraction breathing was carried out at 3 times/d and 5 min/time.
Outcome measures
Primary outcome measures: (1) The pulmonary function indexes of the two groups were compared: A pulmonary function testing instrument was used for measuring the forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and FVC/FEV1 of patients before and after nursing. (2) The respiratory function indexes of the two groups were compared: An automatic blood gas analyzer was adopted for determining the partial pressure of carbon dioxide (PCO2), arterial partial pressure of oxygen (PaO2), and blood oxygen saturation (SaO2) of patients. The daily living ability of the two groups was compared: The activities of daily living (ADL) was adopted for evaluating the daily activities of the two groups [19], which covered 10 items, defecating, peeing, grooming, toilet use, eating, moving, activity, dressing, going up and down stairs, and bathing. It has a full score of 100 points, with a score <20 points for extremely serious functional defects and total dependence in terms of life, a score between 20 and 40 points for enormous requirement of help in terms of life, a score between 40 and 60 points for requirement of help in terms of life, and a score >60 points for basic self-care ability. A higher score indicates stronger daily living ability. (3) The life quality scores of the two groups were compared: A MOS 36-Item Short-Form Health Survey (SF-36) was adopted for evaluating the life quality of the two groups after nursing. SF-36 covers general health, physiological functioning, role physical, bodily pain, vitality, social functioning, role emotional, and mental health [20]. Each item is scored by 0-100 points, and a higher score indicates better life quality.
Secondary outcome measures: (1) The dyspnea scores of the two groups were compared: The Modified British Medical Research Council Dyspnea Score (MMRC) was adopted to evaluate the dyspnea of each patient as follows [21]: Grade 0: Suffering from dyspnea only during strenuous exercise; grade 1: Shortness of breath when walking quickly on small slopes or flat ground; grade 2: Walking on flat ground slower than peers or requiring to stop for rest due to shortness of breath; grade 3; Requirement of taking a breath and having a rest after 100 min or several minutes of walking on flat ground; grade 4: Inability of leaving home due to severe dyspnea or suffering from dyspnea during wearing or taking off clothes. The four grades were recorded as 0-4 points correspondingly, and a high score indicates more serious dyspnea and lower life quality. (2) The sleep quality of the two groups was compared: Pittsburgh sleep quality index (PSQI) was adopted for evaluating the sleep quality of patients [22]. The index covers 7 categories (18 items). Each category is scored by 0-3 points, and the cumulative score is PSQI. With a total score between 0-21 points, PSQI indicates good sleep quality by 0-5 points, fine sleep quality by 6-10 points, moderate sleep quality by 11-15 points, and poor sleep quality by 16-21 points. (3) The nursing satisfaction of the two groups was compared: A self-made Nursing Satisfaction Questionnaire of our hospital was adopted for evaluating the nursing satisfaction of the two groups, which had a total of 20 questions, with 5 points for each question. Each patient was asked to score the content of our hospital according to the nursing content of our hospital. A total score less than 70 points indicated dissatisfaction; a total score between 70 and -89 points indicated satisfaction, and a total score of 90 points or more indicated high satisfaction. Satisfaction = (the number of patients with high satisfaction + that with satisfaction)/the total number of patients ×100%.
Statistical analyses
SPSS24.0 (IBM Corp, Armonk, NY, USA) was adopted for statistical analyses and GraphPad Prism 7 for drawing of corresponding figures. Enumeration data, expressed as [n (%)], were compare between groups by the chi-square test. Those with theoretical frequency in the chi-square test less than 5 were analyzed by the continuity correction chi square test. Measurement data, expressed as the (mean ± SD), were compared between groups by the independent-samples T test and within groups before and after intervention by the paired t test. P<0.05 suggests a notable difference.
Results
General materials
There was no notable difference between the two groups in general clinical baseline data such as sex, age, body mass index (BMI), course of disease, marriage, place of residence, educational background, smoking history, and hypertension history (all P>0.05) (Table 1).
Table 1.
Comparison between the two groups in general data [n (%)] (x̅ ± sd)
| Item | The research group (n=85) | The control group (n=72) | t/χ2 value | P-value |
|---|---|---|---|---|
| Sex | 0.190 | 0.662 | ||
| Male | 64 (75.29) | 52 (72.22) | ||
| Female | 21 (24.71) | 20 (27.78) | ||
| Age (Y) | 69.11±10.16 | 68.53±9.53 | 0.366 | 0.714 |
| BMI (kg/m2) | 22.58±3.36 | 21.86±3.02 | 1.40 | 0.163 |
| Course of disease (Y) | 10.28±2.83 | 10.86±3.06 | 1.233 | 0.2195 |
| Marriage | 0.016 | 0.897 | ||
| Married | 68 (80.00) | 57 (79.17) | ||
| Unmarried | 17 (20.00) | 15 (20.83) | ||
| Place of residence | 1.171 | 0.279 | ||
| Urban area | 52 (61.18) | 50 (69.44) | ||
| Rural area | 33 (38.82) | 22 (30.56) | ||
| Education background | 0.153 | 0.153 | ||
| ≥ senior high school | 27 (31.76) | 25 (34.72) | ||
| < senior high school | 58 (68.24) | 47 (65.28) | ||
| Smoking history | 0.797 | 0.371 | ||
| Yes | 60 (70.59) | 46 (63.89) | ||
| No | 25 (29.41) | 26 (36.11) | ||
| Hypertension history | 0.787 | 0.374 | ||
| Yes | 40 (47.06) | 39 (54.17) | ||
| No | 45 (52.94) | 33 (45.83) | ||
| Diabetes mellitus | 0.405 | 0.524 | ||
| Yes | 37 (43.53) | 35 (48.61) | ||
| No | 48 (56.47) | 37 (51.39) |
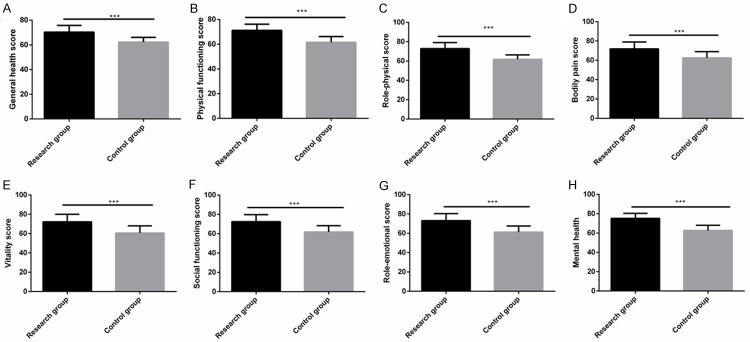
Comparison of pulmonary function
Before nursing, there was no significant difference between the two groups in FEV1, FVC and FEV1/FVC, while after nursing, these indexes of both groups increased greatly, and these indexes of the res group were significantly higher (all P<0.001) (Figure 1).
Figure 1.
Comparison of pulmonary function between the two groups. A. Before nursing, there was no notable difference between the two groups in FEV1, while after nursing, FEV1 of both groups increased significantly, and FEV1 of the research group was significantly higher than that of the control group. B. Before nursing, there was no notable difference between the two groups in FVC, while after nursing, FVC of both groups increased significantly, and FVC of the research group was significantly higher than that of the control group. C. Before nursing, there was no notable difference between the two groups in FEV1/FVC, while after nursing, FEV1/FVC of both groups increased significantly, and FEV1/FVC of the research group was significantly higher than that of the control group. Note: *** indicates P<0.001.
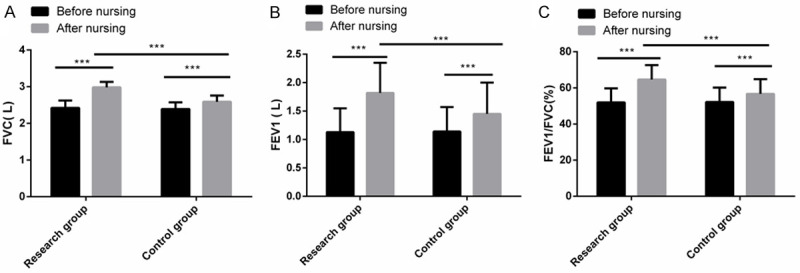
Comparison of respiratory function
Before nursing, there was no significant difference between the two groups in PaCO2, PaO2, and SaO2, while after nursing, PaCO2 of both groups decreased greatly, and PaCO2 of the res group was greatly lower; PaO2 and SaO2 of both groups increased significantly, and those of the res group were significantly higher (both P<0.001) (Figure 2).
Figure 2.
Comparison of respiratory function between the two groups. A. Before nursing, there was no notable difference between the two groups in PaCO2, while after nursing, PaCO2 of both groups decreased significantly, and PaCO2 of the research group was significantly lower than that of the control group. B. Before nursing, there was no notable difference between the two groups in PaO2, while after nursing, PaO2 of both groups increased significantly, and PaO2 of the research group was significantly higher than that of the control group. C. Before nursing, there was no notable difference between the two groups in SaO2, while after nursing, SaO2 of both groups increased significantly, and SaO2 of the research group was significantly higher than that of the control group. Note: *** indicates P<0.001.
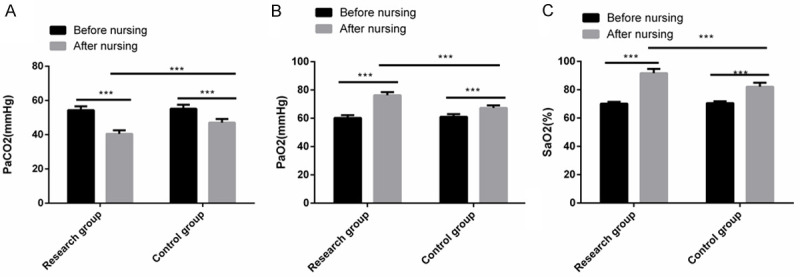
Comparison of MMRC score
Before nursing, there was no significant difference between the two group in MMRC score, while after nursing, MMRC score of both groups decreased greatly, and MMRC score of the res group was significantly lower (P<0.001) (Figure 3).
Figure 3.
Comparison of MMRC score between the two groups. After nursing, MMRC score of both groups decreased greatly, and MMRC score of the research group was significantly lower than that of the control group. Note: *** indicates P<0.001.
Comparison of ADL score
Before nursing, there was no significant difference between the two groups in ADL score, while after nursing, the ADL score of both groups increased greatly, and ADL score of the res group was significantly higher (P<0.001) (Figure 4).
Figure 4.
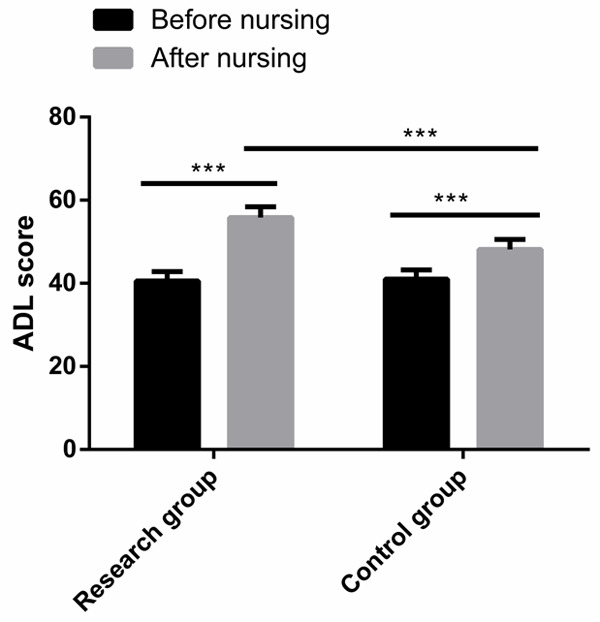
Comparison of ADL score between the two groups. After nursing, the ADL score of both groups increased greatly, and ADL score of the research group was significantly higher than that of the control group. Note: *** indicates P<0.001.
Comparison of PSQI score
Before nursing, there was no significant difference between the two group in PSQI score, while after nursing, the PSQI score of both groups decreased greatly, and PSQI score of the res group was significantly lower (P<0.001) (Figure 5).
Figure 5.
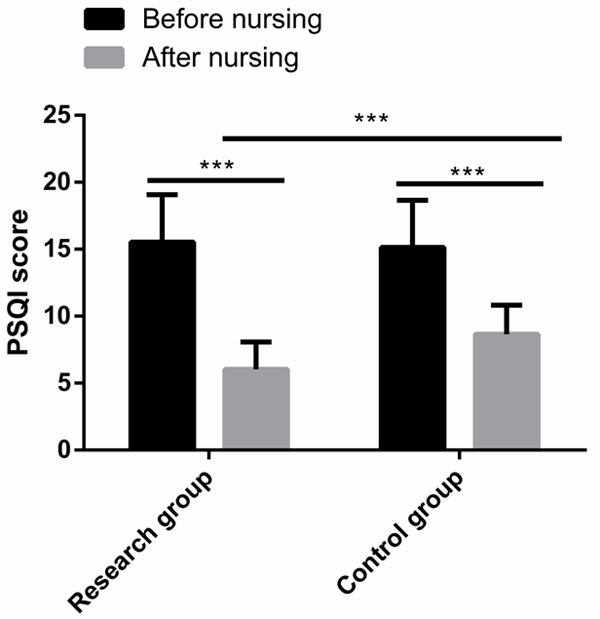
Comparison of PSQI score between the two groups. After nursing, the PSQI score of both groups decreased greatly, and PSQI score of the research group was significantly lower than that of the control group. Note: *** indicates P<0.001.
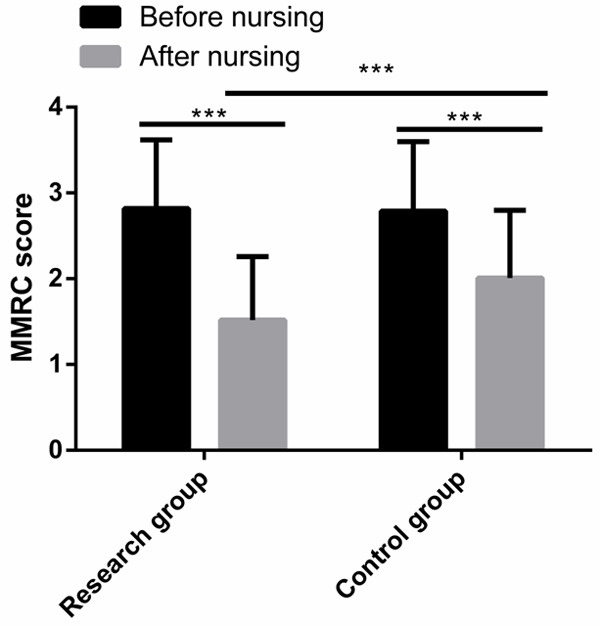
Comparison of life quality scores
After nursing, the res group got significantly higher scores of life quality than the con group in general health, physiological functioning, role physical, bodily pain, vitality, social functioning, role emotional, and mental health (all P<0.001) (Figure 6).
Figure 6.
Comparison of life quality between the two groups. A. The general health score of the research group was significantly higher than that of the control group. B. The physiological functioning score of the research group was significantly higher than that of the control group. C. The role physical score of the research group was significantly higher than that of the control group. D. The bodily pain score of the research group was significantly higher than that of the control group. E. The vitality score of the research group was significantly higher than that of the control group. F. The social functioning score of the research group was significantly higher than that of the control group. G. The emotional function score of the research group was significantly higher than that of the control group. H. The mental health score of the research group was significantly higher than that of the control group. Note: *** indicates P<0.001.
Comparison of nursing satisfaction
After nursing, the res group showed a significantly higher nursing satisfaction than the con group (97.65% vs. 83.33%) (Table 2).
Table 2.
Comparison of nursing satisfaction between the two groups [n (%)]
| Item | The research group (n=85) | The control group (n=72) | χ2 value | P-value |
|---|---|---|---|---|
| High satisfaction | 61 (71.76) | 18 (25.00) | - | - |
| Satisfaction | 20 (23.53) | 42 (58.33) | - | - |
| Dissatisfaction | 4 (4.71) | 12 (16.67) | - | - |
| Nursing satisfaction | 83 (97.65) | 60 (83.33) | 6.341 | 0.011 |
Discussion
COPD is a progressive respiratory disease that is not completely reversible, and it is usually accompanied by airway hyperreactive chronic inflammation [23]. Patients with this disease suffer from severe impact of repeated attacks and long-term illness [24]. COPD is an incurable disease of respiratory dysfunction, so improving their respiratory function will significantly improve the life quality of patients with this disease [25]. Therefore, it is of great significance to explore a nursing intervention model to enhance the respiratory function of patients while effectively treating them clinically.
In our study, we implemented respiration-related guidance and nursing for patients with COPD to determine its effect on the respiratory function and life quality of such patients. As a result, after nursing, the res group showed significantly improved pulmonary function indexes (FEV1, FVC, and FEV1/FVC) compared with the con group, indicating that respiration-related guidance and nursing can strongly improve the pulmonary function of patients and exert beneficial effect on their pulmonary rehabilitation. One study by Yang Y et al. [26] has found that for patients with COPD, eight-sectioned exercise can help improve their pulmonary function and life quality effectively, which is similar to the research results of our respiration-related guidance and nursing mode. One study by Wang X et al. [27] has come to the conclusion that for patients with both silicosis and COPD, nursing intervention about pulmonary function exercise can strongly improve their pulmonary function indexes (FEV1 and FVC) and respiratory mechanics index (PaO2). PaCO2, PaO2, and SaO2 are usually adopted to reflect the situation of patients with COPD. In our study, we also monitored the respiratory indexes of the two groups, finding that compared with the con group, the res group showed significantly lower PaCO2 and significantly higher PaO2 and SaO2. The results denote that respiration-related guidance and nursing can strongly improve the respiratory indexes and respiratory function of patients, which is similar to the research results obtained by Wang X et al. One study by Akor AA et al. [28] has pointed out that MMRC is a leading index to predict the condition of patients with COPD, and patients with the disease can get great amelioration of dyspnea after taking effective physical activities, thus having improved life quality. Moreover, one study by Chabowski M et al. [29] has revealed that over 60% of patients with COPD suffer sleep disorder, and intervention measures of effectively ameliorating the sleep disorder of patients can significantly improve the treatment compliance of patients and clinical efficacy on them. In our study, the res group got significantly lower MMRC and PSQI scores than the con group, indicating that respiration-related guidance and nursing can strongly alleviate dyspnea and sleep disorder of patients, thus enhancing their recovery and treatment outcomes, which is similar to the research results obtained Akor AA et al. and Chabowski M, etc. Life quality and daily living ability are crucial embodiment of the rehabilitation of patients with COPD. We evaluated the two aspects of the two groups, finding that the life quality and daily living ability scores of the res group were higher than those of the con group. The results suggested that respiration-related guidance and nursing greatly improved the daily living ability and life quality of patients, which may be due to the following reasons: Under the respiration-related guidance and nursing mode, patients learned skills of breathing training, which enhanced their recovery of respiratory function and pulmonary function and relieved their dyspnea and sleep disorder, and thus enhanced their life quality and daily living ability. One study by Chen KH et al. [30] has indicated that self-management nursing intervention for patients with COPD can greatly increase their life quality and daily living ability, which is similar to our research results. Additionally, according to one study by Yu YL et al. [31], continuing care can provide continuous health education and supervision for patients with COPD, and can effectively improve their compliance with oxygen therapy, self-care ability, daily living ability, and life quality, which is also similar to our research results. Finally, we compared the nursing satisfaction of the two groups, and found that the res group showed significantly higher nursing satisfaction than the con group. The results implied that patients were more willing to accept respiration-related guidance and nursing, which also suggested that this nursing mode was more advantageous for patients with COPD.
Our study has verified that respiration-related guidance and nursing is more advantageous in nursing of patients with COPD. The innovation of our study lies in the fact that a series of new nursing measures were adopted, with the main goal of enhancing patients’ pulmonary function and respiratory function, and compared with conventional nursing mode, respiration-related guidance and nursing pays more attention to improving patients’ respiratory function and living ability. However, t there is still room for improvement in this study. For example, we can further follow up the patients to understand the long-term intervention effect, and analyze the influencing factors of treatment compliance of patients with COPD, so as to improve the curative effect on them and promote their stability and rehabilitation. We will gradually carry out supplementary research from the above perspective in the future.
To sum up, for patients with COPD, respiration-related guidance and nursing can enhance their pulmonary function and respiratory function, relieve their dyspnea and sleep disorder, and improve their daily living ability, life quality and nursing satisfaction.
Disclosure of conflict of interest
None.
References
- 1.Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet. 2017;389:1931–1940. doi: 10.1016/S0140-6736(17)31222-9. [DOI] [PubMed] [Google Scholar]
- 2.Hattab Y, Alhassan S, Balaan M, Lega M, Singh AC. Chronic obstructive pulmonary disease. Crit Care Nurs Q. 2016;39:124–130. doi: 10.1097/CNQ.0000000000000105. [DOI] [PubMed] [Google Scholar]
- 3.Dean E. Chronic obstructive pulmonary disease. Nurs Older People. 2017;29:12. doi: 10.7748/nop.29.4.12.s14. [DOI] [PubMed] [Google Scholar]
- 4.Duffy SP, Criner GJ. Chronic obstructive pulmonary disease: evaluation and management. Med Clin North Am. 2019;103:453–461. doi: 10.1016/j.mcna.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Long R, Stracy C, Oliver MC. Nutritional care in chronic obstructive pulmonary disease. Br J Community Nurs. 2018;23:S18–S26. doi: 10.12968/bjcn.2018.23.Sup7.S18. [DOI] [PubMed] [Google Scholar]
- 6.Segal LN, Martinez FJ. Chronic obstructive pulmonary disease subpopulations and phenotyping. J Allergy Clin Immunol. 2018;141:1961–1971. doi: 10.1016/j.jaci.2018.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faludi R. [Chronic obstructive pulmonary disease: a cardiologist’s point of view] . Orv Hetil. 2014;155:1480–1484. doi: 10.1556/OH.2014.29989. [DOI] [PubMed] [Google Scholar]
- 8.Leo F, Menger H. [Exacerbations of chronic obstructive pulmonary disease - diagnostic approach, management and follow-up care] . Dtsch Med Wochenschr. 2019;144:21–27. doi: 10.1055/a-0723-4172. [DOI] [PubMed] [Google Scholar]
- 9.Dunn B. Updated guidelines for chronic obstructive pulmonary disease. JAAPA. 2019;32:49–51. doi: 10.1097/01.JAA.0000550297.68348.78. [DOI] [PubMed] [Google Scholar]
- 10.Devillier P, Salvator H, Roche N, Grassin-Delyle S, Naline E, Dorocant S, Neveu H. [Long-term treatment strategy in chronic obstructive pulmonary disease: how to change the course of the disease] . Presse Med. 2014;43:1368–1380. doi: 10.1016/j.lpm.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Yawn BP, Kim V. Treatment options for stable chronic obstructive pulmonary disease: current recommendations and unmet needs. Cleve Clin J Med. 2018;85:S28–S37. doi: 10.3949/ccjm.85.s1.05. [DOI] [PubMed] [Google Scholar]
- 12.Lipworth B, Jabbal S. A pragmatic approach to simplify inhaler therapy for COPD. Lancet Respir Med. 2017;5:679–681. doi: 10.1016/S2213-2600(17)30264-3. [DOI] [PubMed] [Google Scholar]
- 13.Bal Ozkaptan B, Kapucu S. Home nursing care with the self-care model improves self-efficacy of patients with chronic obstructive pulmonary disease. Jpn J Nurs Sci. 2016;13:365–377. doi: 10.1111/jjns.12118. [DOI] [PubMed] [Google Scholar]
- 14.Borge CR, Mengshoel AM, Omenaas E, Moum T, Ekman I, Lein MP, Mack U, Wahl AK. Effects of guided deep breathing on breathlessness and the breathing pattern in chronic obstructive pulmonary disease: a double-blind randomized control study. Patient Educ Couns. 2015;98:182–190. doi: 10.1016/j.pec.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 15.Cornelison SD, Pascual RM. Pulmonary rehabilitation in the management of chronic lung disease. Med Clin North Am. 2019;103:577–584. doi: 10.1016/j.mcna.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 16.Lenferink A, Brusse-Keizer M, van der Valk PD, Frith PA, Zwerink M, Monninkhof EM, van der Palen J, Effing TW. Self-management interventions including action plans for exacerbations versus usual care in patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017;8:CD011682. doi: 10.1002/14651858.CD011682.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aboumatar H, Naqibuddin M, Chung S, Chaudhry H, Kim SW, Saunders J, Bone L, Gurses AP, Knowlton A, Pronovost P, Putcha N, Rand C, Roter D, Sylvester C, Thompson C, Wolff JL, Hibbard J, Wise RA. Effect of a hospital-initiated program combining transitional care and long-term self-management support on outcomes of patients hospitalized with chronic obstructive pulmonary disease: a randomized clinical trial. JAMA. 2019;322:1371–1380. doi: 10.1001/jama.2019.11982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chinai B, Hunter K, Roy S. Outpatient management of chronic obstructive pulmonary disease: physician adherence to the 2017 global initiative for chronic obstructive lung disease guidelines and its effect on patient outcomes. J Clin Med Res. 2019;11:556–562. doi: 10.14740/jocmr3888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mlinac ME, Feng MC. Assessment of activities of daily living, self-care, and independence. Arch Clin Neuropsychol. 2016;31:506–516. doi: 10.1093/arclin/acw049. [DOI] [PubMed] [Google Scholar]
- 20.Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725. doi: 10.1177/2050312116671725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rhee CK, Kim JW, Hwang YI, Lee JH, Jung KS, Lee MG, Yoo KH, Lee SH, Shin KC, Yoon HK. Discrepancies between modified Medical Research Council dyspnea score and COPD assessment test score in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:1623–1631. doi: 10.2147/COPD.S87147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 23.Brandt NJ, Cook H. Chronic obstructive pulmonary disease in older adults: part I: case study. J Gerontol Nurs. 2018;44:10–14. doi: 10.3928/00989134-20180614-04. [DOI] [PubMed] [Google Scholar]
- 24.Riley CM, Sciurba FC. Diagnosis and outpatient management of chronic obstructive pulmonary disease: a review. JAMA. 2019;321:786–797. doi: 10.1001/jama.2019.0131. [DOI] [PubMed] [Google Scholar]
- 25.Wang J, Guo S, Zeng M, Yu P, Mo W. Observation of the curative effect of device-guided rehabilitation on respiratory function in stable patients with chronic obstructive pulmonary disease. Medicine (Baltimore) 2019;98:e14034. doi: 10.1097/MD.0000000000014034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang Y, Chen K, Tang W, Xie X, Xiao W, Xiao J, Luo X, Wang W. Influence of Baduanjin on lung function, exercise capacity, and quality of life in patients with mild chronic obstructive pulmonary disease. Medicine (Baltimore) 2020;99:e22134. doi: 10.1097/MD.0000000000022134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang X, Jiang H, Yu HT, Ju F. [Nursing intervention for respiratory function exercise in patients with silicosis complicated by stable chronic obstructive pulmonary disease] . Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2018;36:844–846. doi: 10.3760/cma.j.issn.1001-9391.2018.11.012. [DOI] [PubMed] [Google Scholar]
- 28.Akor AA, Bamidele A, Erhabor GE. Predictors of health-related quality of life (HRQOL) in patients with chronic obstructive pulmonary disease using the COPD Assessment Test (CAT) West Afr J Med. 2020;37:275–280. [PubMed] [Google Scholar]
- 29.Chabowski M, Luczak J, Dudek K, Jankowska-Polanska B. Sleep disorders and adherence to inhalation therapy in patients with chronic obstructive pulmonary disease. Adv Exp Med Biol. 2019;1160:43–52. doi: 10.1007/5584_2019_345. [DOI] [PubMed] [Google Scholar]
- 30.Chen KH, Liu CY, Shyu YI, Yeh SL. Living with chronic obstructive pulmonary disease: the process of self-managing chronic obstructive pulmonary disease. J Nurs Res. 2016;24:262–271. doi: 10.1097/jnr.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 31.Yu YL, Zheng XS, Han XX, Sun MJ. The application value of continuous nursing for home oxygen therapy of patients in the stable phase of chronic obstructive pulmonary disease. Eur Rev Med Pharmacol Sci. 2017;21:67–72. [PubMed] [Google Scholar]