Abstract
Objective: To evaluate the influence of evidence-based nursing (EBN) on psychological well-being, postoperative complications and quality of life (QOL) after breast cancer (BC) surgery. Methods: A total of 263 patients with BC who were surgically treated in Zhejiang Provincial People’s Hospital from May, 2018 to August, 2019 were as assigned to observation group (EBN, n=142) and control group (routine nursing care, n=121). Clinical indicators and any complications after intervention were recorded. And the exercise compliance in the affected limbs was evaluated. Barthel index (BI), self-rating anxiety scale (SAS) and self-rating depression scale (SDS), Pittsburgh Sleep Quality Index (PSQI) were employed for the assessment of self-care ability, psychological status, and sleep quality, respectively. In addition, we utilized the numerical rating scale (NRS) to evaluate postoperative pain, the functional assessment of cancer therapy-breast (FACT-B) scale to assesse the quality of life (QOL), and the self-made questionnaire to quantify patient satisfaction. Results: After intervention, the observation group presented greater improvement in symptoms, higher exercise compliance and BI scores, as well as lower SAS, SDS, and PSQI scores; the incidence of postoperative pain and complications decreased in observation group, and FACT-B scores and patient satisfaction increased. Conclusion: EBN is effective in relieving symptoms, reducing negative emotions and postoperative complications, as well as enhancing the QOL of patients undergoing BC surgery.
Keywords: Evidence-based nursing, breast cancer surgery, psychological well-being, postoperative complications, quality of life, influence
Introduction
Breast cancer (BC) is the most common cancer among women that threatens patients’ psychology and occupation and the society, and has a serious impact on their physical and mental health [1]. Surgical resection has been the preferred option for the treatment of BC [2]. However, patients who have undergone surgical resection usually suffer from complications and functional impairments induced by extensive trauma [3]. In addition, the defect of the secondary sexual characteristic causes severe physical and psychological damages; also, long-term chemotherapy may trigger a variety of adverse reactions, thereby resulting in negative emotions and a low quality of life (QOL) of most patients [4,5]. Therefore, it is essential to offer effective psychological counseling or nursing guidance to patients undergoing BC surgery.
Due to longterm radiotherapy and chemotherapy, and many other adversing factors, patients with BC usually display poor psychological status and self-image and low QOL [6]. There has been evidence that most surgically treated patients have increased stress, leading to emotional disorders and a decline in QOL [7]. Thus, improving the QOL of patients is important to reduce negative psychological symptoms [8]. The existing routine nursing cares are mostly disease-centered and focus on disease care, and ignore the actual needs of patients; besides, the functional exercise often lacks personalized guidance, which leads to the failure to achieve optimal efficacy [9]. Evidence-based nursing (EBN) is a patient-centered model that gives guidance to patients upon their admission, and performs targeted nursing measures and psychological counseling according to their disease, personality and psychological conditions, so as to relieve their negative emotions and enhance their confidence in healing [10,11]. A previous study reveals that EBN can restore swallowing disorders, oral health and QOL of patients with dysphagia [12]. In addition, for patients receiving BC surgery, health belief model, a kind of nursing model with door-to-door services and telephone reminders, is able to significantly prevent lymph node edema [13].
To provide a feasible nursing care for patients who had underwent BC surgery, EBN was performed, and the improvement of psychological status, postoperative complications and QOL was discussed.
Materials and methods
General data
A total of 263 patients with BC who were surgically treated in Zhejiang Provincial People’s Hospital from May, 2018 to August, 2019 were designated as observation group (EBN, n=142) and control group (routine nursing care, n=121). Inclusion criteria: Patients diagnosed with BC by MRI [14] and receiving radical mastectomy in our hospital; patients with complete general data, stable vital signs, clear consciousness, as well as those who were able to communicate normally with medical staff. No ethics rules were violated, the scheme was submitted to the hospital ethics committee, and the study was approved by the ethics committee. All participants were fully informed and signed the informed consent form. Exclusion criteria: patients with cognitive impairment, a history of mental illness or other malignant tumors, or diseases of the heart, brain, liver and other organs and blood systems; patients who were not willing to participate in and cooperate with the study, or those who had difficulties in understanding the questionnaires; pregnant and lactating women; patients quitting the study or having poor treatment compliance; lost to follow-up patients.
Nursing measures
Routine nursing care was implemented in control group: inform patients about the time of surgery, record the history of drug allergy, and guide the routine fasting and water deprivation before surgery. In addition, conduct basic health education before and after surgery. During hospitalization, closely monitor the disease, diet, rest and degree of pain, answer patients’ questions patiently, and pay attention to health promotion and education. Record the changes in vital signs, monitor the wound and drainage to remove necrotic flap in time and keep the drainage tube unobstructed. Next, assist patients raise their upper limbs and guide them to exercise properly.
EBN was implemented in observation group: 1. Health education: Set up a nursing group composed of professional nursing staff to give health education according to patients’ age, personality, and family situations. Introduce disease-related knowledge and self-prevention of postoperative complications through brochures, videos and professional explanations. 2. Psychological intervention: due to postoperative anxiety, restlessness and panic, the preparation process of nursing care has always been hindered. Therefore, nursing staff should carry out targeted psychological intervention according to patients’ personality and psychological status. Moreover, they should sincerely help patients build confidence in recovery. At the same time, invite patients’ families to create a harmonious family atmosphere, so as to improve patients’ postoperative recovery. 3. Dietary intervention: make a diet plan (low-fat, low-salt, and digestible foods rich in vitamins and protein) based on the condition and eating habits of patients. Stop all health supplements during the treatment, and use tonic food to enhance the immunity. 4. Exercise intervention: After the surgery, use a soft pillow to raise the affected upper limb to 30°, so as to promote blood circulation and lymphatic return and prevent edema of the upper limb. Infusion, blood pressure measurement and blood sampling should be prohibited in the affected limb. Next, formulate step-by-step functional exercises. When using elastic bandages for pressure pressing, do not bandage too tightly to affect lymphatic and venous return. Centripetal massage can also be performed for the affected upper limbs. 5. Pain intervention: Record the location, degree and time of the pain to take corresponding analgesic measures. 6. Complication management: observe the occurrence of subcutaneous hydrops and hemorrhage, flap necrosis, upper limb edema. Moreover, instruct the patients and their families to focus on postoperative rehabilitation.
Outcome measures
1. Clinical indicators: the times to first ambulation, swelling regression, extubation by vacuum sealing drainage were recorded, as well as the hospital stay.
2. Exercise compliance: the self-made compliance questionnaire was used to evaluate exercise compliance. Full compliance: patients closely followed the postoperative exercise plan and were capable of full abduction; Partial compliance: patients could only follow part of the exercise plan, and had limited abduction; Non-compliance: patients entirely failed to follow the exercise plan, and were not capable of abduction. Total compliance rate = cases of (full compliance + partial compliance)/total cases × 100%.
3. Self-care ability: Barthel index (BI) was used for evaluation [15]. There were 10 items in the scale, with a total score of 100. A score of less than 40 (Grade I) indicated severe dependence of patients, a score of 41-60 (Grade II) indicated moderate dependence, a score of greater than 60 (Grade III) indicated low dependence.
4. Psychological well-being: Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) (with a total score of 100 for both scales) were employed [16]. After the intervention, patients scored 50-70 were considered mildly anxious, those scored 71-90 were considered moderately anxious, and scored >90 were considered severely anxious. The higher score indicated a higher level of the anxiety. The above classification criteria were also applicable to the SDS; the higher the score, the more severe the depression.
5. Sleep quality: Pittsburgh Sleep Quality Index (PSQI) [17] had 7 dimensions and scores ranging from 0 to 21. The higher score suggested the lower sleep quality of patients.
6. Pain evaluation: With a total score of 10, a numerical rating scale (NRS) [18] score of 0 indicated no pain, 1 to 4 indicated mild pain, 5 to 6 indicated moderate pain, and 7 to 10 indicated severe pain. The higher score suggested higher pain levels.
7. Complications: Any complications occurring in the nursing process were recorded.
8. Quality of life: The functional assessment of cancer therapy-breast (FACT-B) scale [19] included 5 domains (physical, social/family, emotional, functional well-being, additional concerns) and 36 items. Using a 5-level scoring method, forward items were scored from 0-4, the others were reverse scored, and the scores of 5 domains were added together; the higher the score, the better the QOL.
9. Patient satisfaction: The self-made satisfaction questionnaire consisted of five items, namely, timeliness of service delivery, management standardization, service attitude, hospital environment and comprehensive quality of nursing staff. The higher the score, the higher the satisfaction of patients with the service.
Statistical methods
SPSS22.0 (EasyBio Technology Co., Ltd., Beijing, China) was used for statistical analyses. The categorized data were summarized by number/percentage [n (%)], and intra-group comparisons were analyzed with chi-square test. When the expected frequency was less than 5, chi-square test was applied with continuity correction. The continuous data were expressed by mean ± standard deviation (mean ± SD); inter-group comparisons were conducted with independent samples t test, and intra-group comparisons were conducted with paired t test. A value of P < 0.05 was considered to be statistically significant.
Results
General data
There was no significant difference between the two groups in age, body mass index (BMI), marital status, nationality, employment, smoking history, history of alcoholism, history of breast disease, surgery type, tumor staging, cancer type and site (P>0.05) (Table 1).
Table 1.
Comparison of general data [n (%)] (mean ± SD)
| Classification | Observation group (n=142) | Control group (n=121) | t/χ2 | P |
|---|---|---|---|---|
| Age (years) | 47.23±4.45 | 47.53±4.42 | 0.546 | 0.585 |
| BMI (kg/m2) | 22.37±2.64 | 22.68±2.54 | 0.335 | 0.965 |
| Marital status | 0.151 | 0.697 | ||
| Married | 75 (52.82) | 61 (50.41) | ||
| Unmarried, divorced and widowed | 67 (47.18) | 60 (49.59) | ||
| Nationality | 0.139 | 0.708 | ||
| Han nationality | 73 (51.41) | 65 (53.72) | ||
| Minority nationalities | 69 (48.59) | 56 (46.28) | ||
| Employment status | 0.338 | 0.561 | ||
| Employed | 56 (39.44) | 52 (42.98) | ||
| Laid-off or unemployed | 86 (60.56) | 69 (57.02) | ||
| Smoking history | 0.405 | 0.524 | ||
| Yes | 59 (41.55) | 55 (45.45) | ||
| No | 83 (58.45) | 66 (54.55) | ||
| History of drinking | 0.507 | 0.476 | ||
| Yes | 63 (44.37) | 59 (48.76) | ||
| No | 79 (55.63) | 62 (51.24) | ||
| History of breast disease | 0.581 | 0.445 | ||
| Yes | 91 (64.08) | 72 (59.50) | ||
| No | 51 (35.92) | 49 (40.50) | ||
| Surgery type | 0.102 | 0.905 | ||
| Modified radical mastectomy | 55 (38.73) | 49 (40.50) | ||
| Breast-conserving surgery | 45 (31.69) | 38 (31.40) | ||
| Prosthesis implantation following mastectomy | 42 (29.58) | 34 (28.10) | ||
| Tumor staging | 0.846 | 0.655 | ||
| I | 58 (56.86) | 46 (53.49) | ||
| II | 29 (28.43) | 23 (26.74) | ||
| III | 15 (14.71) | 17 (19.77) | ||
| Cancer type | 0.315 | 0.574 | ||
| Ductal carcinoma | 73 (51.41) | 58 (47.93) | ||
| Lobular carcinoma | 69 (48.59) | 63 (52.07) | ||
| Cancer site | 0.594 | 0.440 | ||
| Left | 83 (58.45) | 65 (53.72) | ||
| Right | 59 (41.55) | 56 (46.28) |
Comparison of clinical symptoms
Observing the clinical symptoms of patients after the intervention found that the observation group showed earlier time to first ambulation, swelling regression, extubation by vacuum sealing drainage than the control group, as well as shorter hospital stay (P < 0.05) (Table 2).
Table 2.
Comparison of clinical symptoms (mean ± SD)
| Group | n | Time to first ambulation (h) | Time to swelling regression (d) | Time to extubation by vacuum sealing drainage (d) | Hospital stay (d) |
|---|---|---|---|---|---|
| Observation group | 142 | 18.53±1.93 | 10.04±1.05 | 8.73±0.75 | 11.35±1.47 |
| Control group | 121 | 25.74±2.68 | 16.96±1.57 | 12.56±1.32 | 15.78±1.84 |
| t | - | 39.070 | 42.540 | 29.450 | 21.700 |
| P | - | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Comparison of exercise compliance
After intervention, the exercise compliance of patients in the observation group was 95.07%, remarkably higher than 74.38% in the control group (P < 0.05) (Table 3).
Table 3.
Comparison of exercise compliance [n (%)]
| Group | n | Full compliance | Partial compliance | Non-compliance | Total compliance rate |
|---|---|---|---|---|---|
| Observation group | 142 | 98 (69.01) | 37 (25.62) | 7 (4.93) | 135 (95.07) |
| Control group | 121 | 42 (34.71) | 48 (39.67) | 31 (25.62) | 90 (74.38) |
| χ2 | - | - | - | - | 22.631 |
| P | - | - | - | - | < 0.001 |
Comparison of BI scores
In the observation group, 3.52% of the patients had BI grade I after the intervention, 14.79% BI grade II, and 81.69% BI grade III; while those in the control group were 14.88%, 29.75%, and 55.37%, respectively. The comparison showed that there were more patients in grade lll and fewer patients in grade ll and lll in the observation group (Table 4).
Table 4.
Comparison of Barthel index [n (%)]
| Group | Cases (n) | Grade I | Grade II | Grade III |
|---|---|---|---|---|
| Observation group | 142 | 5 (3.52) | 21 (14.79) | 116 (81.69) |
| Control group | 121 | 18 (14.88) | 36 (29.75) | 67 (55.37) |
| χ2 | - | 10.551 | 8.617 | 21.381 |
| P | - | 0.001 | 0.003 | < 0.001 |
Comparison of psychological well-being
We found no differences in SAS and SDS scores between the two groups before intervention. The scores in observation group were lower than those in control group after intervention (P < 0.05) (Figure 1).
Figure 1.
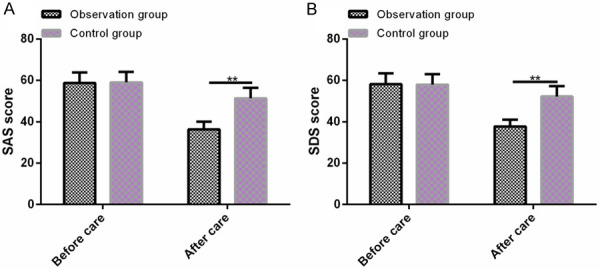
Comparison of psychological well-being. A: There is no significant difference in SAS scores between the two groups before intervention, and the scores in observation group are significantly lower than those in control group after intervention. B: There is no significant difference in SDS scores between the two groups before intervention, and the scores in observation group are significantly lower than those in control group after intervention. Note: *P < 0.05 vs. before intervention, **P < 0.01 vs. after intervention.
Comparison of PSQI scores
No significant differences in PSQI scores between the two groups were observed before intervention, but the scores in observation group were lower than those in control group after intervention (P < 0.05) (Figure 2).
Figure 2.
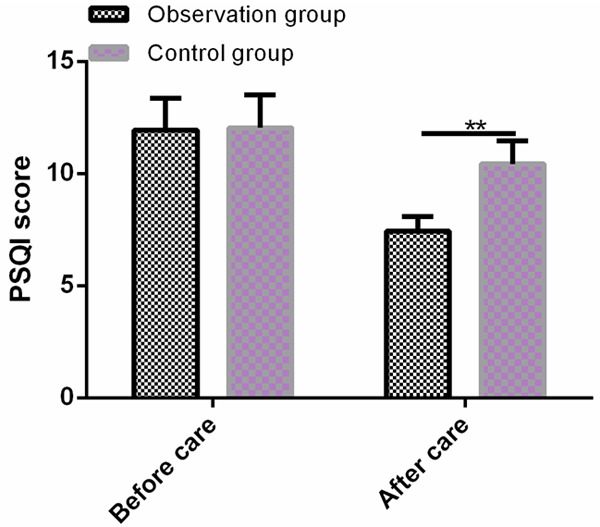
Comparison of PSQI scores. There is no significant difference in PSQI scores between the two groups before intervention, and the scores in observation group are significantly lower than those in control group after intervention. Note: *P < 0.05 vs. before intervention, **P < 0.01 vs. after intervention.
Comparison of NRS scores
After intervention, NRS scores in observation group and control group were 15.49% and 42.98%, respectively. Therefore, the incidence of postoperative pain in observation group was remarkably lower than that in control group (P < 0.05) (Table 5).
Table 5.
Comparison of NRS scores [n (%)]
| Group | Cases (n) | Pain perception (%) | Incidence of postoperative pain (%) | ||
|---|---|---|---|---|---|
|
| |||||
| Mild | Moderate | Severe | |||
| Observation group | 142 | 15 (10.56) | 7 (4.93) | 0 (0.00) | 22 (15.49) |
| Control group | 121 | 22 (18.18) | 26 (21.49) | 4 (3.31) | 52 (42.98) |
| t | - | 21.700 | 16.321 | 4.767 | 24.401 |
| P | - | < 0.001 | < 0.001 | 0.029 | < 0.001 |
Comparison of the incidence of complications
After intervention, the incidence of complications in observation group was remarkably lower than that in control group (4.23% vs. 13.22%) (P < 0.05) (Table 6).
Table 6.
Comparison of the incidence of complications [n (%)]
| Classification | Observation group (n=142) | Control group (n=121) | χ2 | P |
|---|---|---|---|---|
| Postoperative swelling | 2 (1.41) | 3 (2.48) | 0.401 | 0.526 |
| Wound disruption and bleeding | 1 (0.70) | 3 (2.48) | 1.374 | 0.241 |
| Subcutaneous hydrops | 1 (0.70) | 4 (3.31) | 2.371 | 0.123 |
| Flap necrosis | 0 (0.00) | 2 (1.65) | 2.365 | 0.124 |
| Appetite loss | 2 (1.41) | 4 (3.31) | 1.055 | 0.304 |
| Incidence of complications | 6 (4.23) | 16 (13.22) | 6.900 | 0.008 |
Comparison of FACT-B scores
Evaluating the QOL of patients in the two groups after intervention showed that the patients in the observation group presented higher FACT-B scores than those in the control group (P < 0.05) (Table 7).
Table 7.
Comparison of FACT-B scores (mean ± SD)
| FACT-B score | Observation group (n=142) | Control group (n=121) | t | P |
|---|---|---|---|---|
| Physical well-being | 21.32±2.35 | 18.34±1.65 | 11.700 | 0.001 |
| Social/family well-being | 19.87±1.95 | 16.23±1.37 | 17.230 | < 0.001 |
| Functional well-being | 16.65±1.75 | 13.53±1.18 | 16.650 | < 0.001 |
| Emotional well-being | 15.76±1.58 | 13.31±1.22 | 13.890 | 0.001 |
| Additional concerns | 24.86±2.61 | 20.43±1.43 | 16.660 | < 0.001 |
| Total score | 98.46±9.47 | 81.84±8.05 | 15.190 | < 0.001 |
Comparison of patient satisfaction
The scores of timeliness of service delivery, management standardization, service attitude, hospital environment and comprehensive quality of nursing staff in observation group were higher than those in control group (P < 0.05) (Table 8).
Table 8.
Comparison of patient satisfaction (mean ± SD)
| Group | n | Timeliness of service delivery | Management standardization | Service attitude | Hospital environment | Comprehensive quality of nursing staff |
|---|---|---|---|---|---|---|
| Observation group | 142 | 25.43±2.22 | 24.46±2.43 | 13.42±2.23 | 14.76±2.26 | 10.97±1.06 |
| Control group | 121 | 20.16±2.14 | 19.24±2.18 | 10.32±1.94 | 11.56±2.09 | 7.41±0.54 |
| t | - | 19.510 | 18.200 | 11.920 | 11.850 | 33.430 |
| P | - | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Discussion
Despite improvements in lifestyle and living standards, the incidence of BC has been rising [20]. BC is the most common malignancy that mainly threatens women [21]. Clinically, surgery is usually the major treatment option, but it may damage the lymph nodes to a certain extent, resulting in edema of the affected limbs and severe psychological pressure of patients, thus affecting the subsequent QOL [22,23]. Therefore, the implement of nursing measures is of great significance, as it may improvethe prognosis and QOL of patients.
In the present study, EBN was used to intervene the psychological well-being, exercise compliance, postoperative complications and QOL of patients undergone BC surgery. It turned out that the postoperative recovery of patients was significantly accelerated after EBN intervention. Hu et al reported that postoperative complications frequently occur in patients with BC, and nursing cares can reduce the incidence, effectively shorten the hospital stay, and increase the survival rate [24], similar to our findings. In the present study, the observation group showed earlier time to first ambulation, swelling regression, extubation by vacuum sealing drainage than the control group, as well as shorter hospital stay. These results together suggest that effective nursing interventions accelerate patient recovery and EBN guides the postoperative rehabilitation positively and contributes to relieving clinical symptoms, shortening hospital stay, as well as improving prognosis. After BC surgery, most patients will develop edema in the affected limb which is due to radiotherapy- or surgery-induced local damage of lymph vessels, thereby leading to obstruction of lymphatic return and swelling of the upper limb [25]. There is evidence that an effective movement guidance can significantly restore the function of the upper limb [26]. We have shown that higher exercise compliance and BI scores in observation group indicate that functional exercise and enhancement of self-care performance implemented in EBN optimize the prognosis of patients, thus improving the exercise compliance, reducing the dependence, as well as speeding up the recovery. Depression and anxiety are more common in cancer patients than in the other population. And patients with BC usually suffer from anxiety and other negative emotions after diagnosis and during treatment and disease monitoring, resulting in reduced therapeutic effects [27,28]. After nursing intervention, SAS and SDS scores of patients decreased evidently in observation group, which is similar to previous report that an effective nursing intervention increases the psychological adaptability after BC surgery and alleviates depression and anxiety [29]. Therefore, EBN is effective in improving patients’ negative emotions and relieving their stress, so as to maintain a good attitude towards the follow-up treatment.
Sleep disorder and depression are the main complaints of cancer patients [30]. In the present study, the PSQI scores in observation group were lower than those in control group, indicating that EBN helps patients relieve negative emotions and psychological pressure, and improve their sleep quality. Moreover, the lower incidence of postoperative pain in the observation group reveals that the psychological well-being, postoperative pain and sleep quality have been improved simultaneously by EBN, thereby facilitating prognosis and treatment. Complications, such as breast edema, wound infection, delayed wound healing, are likely to occur in patients undergoing BC surgery or radiotherapy [31]. So it is necessary to perform nursing cares to enhance the nursing quality and reduce the incidence of accidental skin defects as previously repoprted [32]. This is similar to our results that the incidence of complications in observation group was lower than that in control group after intervention, which indicates that effective nursing interventions decrease the complications during surgery or rehabilitation, and that EBN reduces the incidence of postoperative complications and promotes patient recovery. As the survival of BC patients is getting better in the past decades, considerable attention has been devoted to the enhancement of QOL [33]. Our finding that FACT-B scores in observation group were higher than those in control group after intervention is consistent with a previous study, that patients receiving telehealth intervention present increased QOL and reduced pressures [34]. Therefore, EBN is associated with better psychological status, fewer postoperative complications, and higher self-care ability and QOL. We further compared the patient’s satisfaction in the two groups. It was found that patients in the observation group were more satisfied with the nursing service, indicating the high patient acceptance of EBN, which provides a powerful reference for its subsequent adoption.
The present study verified the benefits of EBN for patients undergoing BC surgery, but there are still several limitations. For example, analysisng the risk factors affecting postoperative recovery of BC is able to nurses to identify the factors that need additional attention. The limitations will be addressed to supplement our conclusions.
To sum up, EBN is effective in relieving symptoms, reducing negative emotions and postoperative complications, as well as enhancing the QOL of patients undergoing BC surgery.
Acknowledgements
This study is financially supported by Effect of acupoint application of traditional Chinese medicine on recovery of perceived function and quality of different chemotherapy processes in breast cancer (2021ZB029).
Disclosure of conflict of interest
None.
References
- 1.Amraoui J, Pouliquen C, Fraisse J, Dubourdieu J, Rey Dit Guzer S, Leclerc G, de Forges H, Jarlier M, Gutowski M, Bleuse JP, Janiszewski C, Diaz J, Cuvillon P. Effects of a hypnosis session before general anesthesia on postoperative outcomes in patients who underwent minor breast cancer surgery: the HYPNOSEIN randomized clinical trial. JAMA Netw Open. 2018;1:e181164. doi: 10.1001/jamanetworkopen.2018.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hung YT, Wu CF, Liang TH, Chou SS, Chen GL, Wu PN, Su GR, Jang TH, Liu CY, Wang CY, Tseng LM, Sheu SJ. Developing a decision-aid website for breast cancer surgery: an action research approach. J Med Internet Res. 2019;21:e10404. doi: 10.2196/10404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bojinovic-Rodic D, Popovic-Petrovic S, Tomic S, Markez S, Zivanic D. Upper extremity function and quality of life in patients with breast cancer related lymphedema. Vojnosanit Pregl. 2016;73:825–830. doi: 10.2298/VSP150208075B. [DOI] [PubMed] [Google Scholar]
- 4.Chen R, You S, Yin Z, Zhu Q, Jiang C, Li S, Li Y, Zha X, Wang J. Non-doctoral factors influencing the surgical choice of Chinese patients with breast cancer who were eligible for breast-conserving surgery. World J Surg Oncol. 2019;17:189. doi: 10.1186/s12957-019-1723-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prieto-Callejero B, Rivera F, Fagundo-Rivera J, Romero A, Romero-Martin M, Gomez-Salgado J, Ruiz-Frutos C. Relationship between chemotherapy-induced adverse reactions and health-related quality of life in patients with breast cancer. Medicine (Baltimore) 2020;99:e21695. doi: 10.1097/MD.0000000000021695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan KS, Zeng D, Leung JHT, Ooi BSY, Kong KT, Yeo YH, Goo JTT, Chia CLK. Measuring upper limb function and patient reported outcomes after major breast cancer surgery: a pilot study in an Asian cohort. BMC Surg. 2020;20:108. doi: 10.1186/s12893-020-00773-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charalampopoulou M, Bacopoulou F, Syrigos KN, Filopoulos E, Chrousos GP, Darviri C. The effects of pythagorean self-awareness intervention on breast cancer patients undergoing adjuvant therapy: a pilot randomized controlled trial. Breast. 2020;49:210–218. doi: 10.1016/j.breast.2019.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Byun HS, Hwang H, Kim GD. Crying therapy intervention for breast cancer survivors: development and effects. Int J Environ Res Public Health. 2020;17:4911. doi: 10.3390/ijerph17134911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ding TT, Luo BR. Effect of individualized intervention on postpartum breast-feeding behavior after cesarean section. Sichuan Da Xue Xue Bao Yi Xue Ban. 2019;50:609–614. [PubMed] [Google Scholar]
- 10.Karlsson A, Lindeborg P, Gunningberg L, Jangland E. Evidence-based nursing-How is it understood by bedside nurses? A phenomenographic study in surgical settings. J Nurs Manag. 2019;27:1216–1223. doi: 10.1111/jonm.12802. [DOI] [PubMed] [Google Scholar]
- 11.Kilicli AB, Kelber ST, Akyar I, Litwack K. Attitude, source of knowledge, and supporting factors on evidence-based nursing among cardiovascular nurses: a cross-sectional descriptive study in Turkey. J Eval Clin Pract. 2019;25:498–506. doi: 10.1111/jep.13132. [DOI] [PubMed] [Google Scholar]
- 12.Park Y, Oh S, Chang H, Bang HL. Effects of the evidence-based nursing care algorithm of dysphagia for nursing home residents. J Gerontol Nurs. 2015;41:30–39. doi: 10.3928/00989134-20151015-04. [DOI] [PubMed] [Google Scholar]
- 13.Cal A, Bahar Z, Gorken I. Effects of Health Belief Model based nursing interventions offered at home visits on lymphedema prevention in women with breast cancer: a randomised controlled trial. J Clin Nurs. 2020;29:2521–2534. doi: 10.1111/jocn.15271. [DOI] [PubMed] [Google Scholar]
- 14.Yoon GY, Eom HJ, Choi WJ, Chae EY, Cha JH, Shin HJ, Ko BS, Kim HH. Feasibility of supine MRI (Magnetic Resonance Imaging)-navigated ultrasound in breast cancer patients. Asian J Surg. 2020;43:787–794. doi: 10.1016/j.asjsur.2019.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Huang SC, Kuo SF, Tsai PS, Tsai CY, Chen SS, Lin CY, Lin PC, Hou WH. Effectiveness of tailored rehabilitation education in improving the health literacy and health status of postoperative patients with breast cancer: a randomized controlled trial. Cancer Nurs. 2020;43:E38–E46. doi: 10.1097/NCC.0000000000000665. [DOI] [PubMed] [Google Scholar]
- 16.Li WT, Chen XZ, Tu WJ, Huang ZZ, Chang LH, Wang J, Zhang GH. Psychopathological characteristics in patients with deviation of nasal septum: a preliminary analysis. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2016;51:655–660. doi: 10.3760/cma.j.issn.1673-0860.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Fontes F, Goncalves M, Pereira S, Lunet N. Neuropathic pain after breast cancer treatment and its impact on sleep quality one year after cancer diagnosis. Breast. 2017;33:125–131. doi: 10.1016/j.breast.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 18.Cho Y, Do J, Jung S, Kwon O, Jeon JY. Effects of a physical therapy program combined with manual lymphatic drainage on shoulder function, quality of life, lymphedema incidence, and pain in breast cancer patients with axillary web syndrome following axillary dissection. Support Care Cancer. 2016;24:2047–2057. doi: 10.1007/s00520-015-3005-1. [DOI] [PubMed] [Google Scholar]
- 19.Matthies LM, Taran FA, Keilmann L, Schneeweiss A, Simoes E, Hartkopf AD, Sokolov AN, Walter CB, Sickenberger N, Wallwiener S, Feisst M, Gass P, Lux MP, Schuetz F, Fasching PA, Sohn C, Brucker SY, Graf J, Wallwiener M. An electronic patient-reported outcome tool for the FACT-B (functional assessment of cancer therapy-breast) questionnaire for measuring the health-related quality of life in patients with breast cancer: reliability study. J Med Internet Res. 2019;21:e10004. doi: 10.2196/10004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zahmatkesh B, Keramat A, Alavi N, Khosravi A, Kousha A, Motlagh AG, Darman M, Partovipour E, Chaman R. Breast cancer trend in Iran from 2000 to 2009 and prediction till 2020 using a trend analysis method. Asian Pac J Cancer Prev. 2016;17:1493–1498. doi: 10.7314/apjcp.2016.17.3.1493. [DOI] [PubMed] [Google Scholar]
- 21.Fahad Ullah M. Breast cancer: current perspectives on the disease status. Adv Exp Med Biol. 2019;1152:51–64. doi: 10.1007/978-3-030-20301-6_4. [DOI] [PubMed] [Google Scholar]
- 22.Lee CM, Zheng H, Tan VK, Tan TJ, Kanesvaran R, Wong FY, Sim YR, Yong WS, Madhukumar P, Ong KW, Tan BK. Surgery for early breast cancer in the extremely elderly leads to improved outcomes - An Asian population study. Breast. 2017;36:44–48. doi: 10.1016/j.breast.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 23.Zhang X, Wang X, Zhang B, Yang S, Liu D. Effects of acupuncture on breast cancer-related lymphoedema: a systematic review and meta-analysis of randomised controlled trials. Acupunct Med. 2019;37:16–24. doi: 10.1136/acupmed-2018-011668. [DOI] [PubMed] [Google Scholar]
- 24.Hu C, Song H, Wang L, Jin L, Zhou X, Sun L. Clinical efficacy of anesthesia with intensive care nursing in attenuating postoperative complications in patients with breast cancer. J Int Med Res. 2020;48:300060520930856. doi: 10.1177/0300060520930856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berlit S, Brade J, Tuschy B, Hornemann A, Leweling H, Eghardt V, Sutterlin M. Whole-body bioelectrical impedance analysis in assessing upper-limb lymphedema after breast cancer therapy. Anticancer Res. 2013;33:4553–4556. [PubMed] [Google Scholar]
- 26.Zhou K, Wang W, An J, Li M, Li J, Li X. Effects of progressive upper limb exercises and muscle relaxation training on upper limb Function and health-related quality of life following surgery in women with breast cancer: a clinical randomized controlled trial. Ann Surg Oncol. 2019;26:2156–2165. doi: 10.1245/s10434-019-07305-y. [DOI] [PubMed] [Google Scholar]
- 27.Gold M, Dunn LB, Phoenix B, Paul SM, Hamolsky D, Levine JD, Miaskowski C. Co-occurrence of anxiety and depressive symptoms following breast cancer surgery and its impact on quality of life. Eur J Oncol Nurs. 2016;20:97–105. doi: 10.1016/j.ejon.2015.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bredicean AC, Crainiceanu Z, Oprean C, Rivis IA, Papava I, Secosan I, Frandes M, Giurgi-Oncu C, Grujic D. The influence of cognitive schemas on the mixed anxiety-depressive symptoms of breast cancer patients. BMC Womens Health. 2020;20:32. doi: 10.1186/s12905-020-00898-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou K, Li J, Li X. Effects of cyclic adjustment training delivered via a mobile device on psychological resilience, depression, and anxiety in Chinese post-surgical breast cancer patients. Breast Cancer Res Treat. 2019;178:95–103. doi: 10.1007/s10549-019-05368-9. [DOI] [PubMed] [Google Scholar]
- 30.Mansano-Schlosser TC, Ceolim MF, Valerio TD. Poor sleep quality, depression and hope before breast cancer surgery. Appl Nurs Res. 2017;34:7–11. doi: 10.1016/j.apnr.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 31.Mi Y, Lv P, Wang F, Li L, Zhu M, Cao Q, Liu J, Dong M, Shi Y, Fan R. Efficacy, late complications, and cosmetic outcomes of targeted intraoperative radiotherapy in breast-conserving surgery for early-stage breast cancer: a single-centre study in China. Jpn J Clin Oncol. 2019;49:1120–1125. doi: 10.1093/jjco/hyz128. [DOI] [PubMed] [Google Scholar]
- 32.Chiang CY, Lee YC, Yang CY, Wang MW, Yang LH. Using time management and quality improvements to decrease the incidence of unexpected skin defects in post-mastectomy breast cancer patients. Hu Li Za Zhi. 2018;65:87–94. doi: 10.6224/JN.201812_65(6).11. [DOI] [PubMed] [Google Scholar]
- 33.Ng ET, Ang RZ, Tran BX, Ho CS, Zhang Z, Tan W, Bai Y, Zhang M, Tam WW, Ho RC. Comparing quality of life in breast cancer patients who underwent mastectomy versus breast-conserving surgery: a meta-analysis. Int J Environ Res Public Health. 2019;16:4970. doi: 10.3390/ijerph16244970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen YY, Guan BS, Li ZK, Li XY. Effect of telehealth intervention on breast cancer patients’ quality of life and psychological outcomes: a meta-analysis. J Telemed Telecare. 2018;24:157–167. doi: 10.1177/1357633X16686777. [DOI] [PubMed] [Google Scholar]


