Abstract
Background:
Compared to general anesthesia, regional anesthesia confers several benefits including improved pain control and decreased postoperative opioid consumption. While the benefits of peripheral nerve blocks (PNB) have been well studied, there is little epidemiological data on PNB usage in mastectomy and lumpectomy procedures. The primary objective of our study was to assess national trends of the annual proportion of PNB use in breast surgery from 2010 to 2018. We also identified factors associated with PNB use for breast surgery.
Methods:
We identified lumpectomy and mastectomy surgical cases with and without PNB between 2010 and 2018 using the Anesthesia Quality Institute National Anesthesia Clinical Outcomes Registry (AQI NACOR). We modeled the nonlinear association between year of procedure and PNB use with segmented mixed-effects logistic regression clustered on facility identifier. The association between PNB use and year of procedure, age, sex, American Society of Anesthesiologists Physical Status (ASA PS), facility type, facility region, weekday, and tissue expander use was also modeled using mixed-effects logistic regression.
Results:
Of the 189,854 surgical cases from 2010 to 2018 that met criteria, 86.2% were lumpectomy cases and 13.8% were mastectomy cases. The proportion of lumpectomy cases with PNB was <0.1% in 2010 and increased each subsequent year to 1.9% in 2018 (trend P < 0.0001). The proportion of mastectomy cases with PNB was 0.5% in 2010 and 13% in 2018 (trend P < 0.0001). The year 2014 was the breakpoint selected for segmented regression. Before 2014, the odds of PNB among the mastectomy cases was not significantly different from year to year. After 2014, the odds of PNB increased by 2.24-fold each year (95% confidence interval [CI], 2.00–2.49; P < 0.001); interaction test for pre-2014 vs post-2014 was P < 0.001. Similar trends were seen in the lumpectomy cases, where after 2014, the odds of PNB increased by 2.03-fold (95% CI 1.81–2.27; P < 0.001); interaction test for pre-2014 vs post-2014 was P < 0.001. In the mastectomy cohort, year of procedure ≥ 2014, female sex, facility region, and tissue expander use were associated with higher odds of PNB. For lumpectomy cases, year of procedure ≥ 2014 and facility region were associated with higher odds of PNB use.
Conclusions:
We found increased annual utilization of PNB for mastectomy and lumpectomy since 2010, although absolute prevalence is low. PNB use was associated with year of procedure for both lumpectomy and mastectomy, particularly post-2014.
Keywords: Breast cancer, anesthesia, nerve block, paravertebral nerve block, plane block, mastectomy, lumpectomy, retrospective observational study, missingness, NACOR, AQI
Introduction
In 2019, there was an estimate of 268,600 new invasive breast cancer cases in women, 2,670 new invasive breast cancer cases in men, and 62,930 cases of in situ cases in women.1 Almost all mastectomy and lumpectomy procedures are performed due to a cancer diagnosis.2 Compared to general anesthesia, regional anesthesia confers several benefits including improved pain control, decreased postoperative opioid consumption, earlier ambulation,3 and decreased incidence of postoperative ileus.4 Regional anesthesia has been a component of many enhanced recovery programs (ERP) to enable early functional recovery and narcotic sparing.5
A prior study of peripheral nerve block (PNB) use in outpatient orthopedic procedures found a significant increase since 2010. Reasons for this increase were attributed to superior perioperative outcomes and initiatives to enhance training in ultrasound-guided regional anesthesia.6 Additional studies have reflected a similar increase in popularity of nerve blocks in orthopedic surgery, one of which found disparities in anesthetic care based on demographic and insurance status.7
This study uses the Anesthesia Quality Institute National Anesthesia Clinical Outcomes Registry (AQI NACOR). The source of this registry’s data is billing records from anesthesia groups. The primary objective of this study is to assess trends in the prevalence of PNB use in mastectomy and lumpectomy from 2010 to 2018 using AQI NACOR. We hypothesize that the use of PNB in breast cancer surgery has increased annually since 2010. We believe that the usage of PNB for mastectomy across the analyzed time period will be far more than for lumpectomy because the latter is a less aggressive procedure.
Methods
Data Source and Study Criteria
We obtained data from NACOR, the largest anesthesia registry in the United States.8 Multiple data sources were considered for this study. NACOR was selected because this database captures information on all procedure codes, including the type of PNB. The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) data dictionary does not specify PNB type,9 while the Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project Nationwide Ambulatory Surgery Sample does not describe anesthetic technique.10 U.S. Medicare data excludes patients under 65 years old. NACOR is built from anesthesiology case data collected from anesthesia practices and hospitals across the U.S. Contributions are voluntary and made on a monthly basis by most registrants. The NACOR data dictionary includes elements regarding the facility, patient demographics, Common Procedural Terminology (CPT) codes for anesthesia and surgery, International Classification of Diseases, Tenth Edition (ICD-10) diagnosis codes, quality metrics, and outcomes.11 In 2015, NACOR acquired data from roughly 25% of all anesthesia procedures performed in the U.S.12 As the NACOR data is deidentified, this study was deemed exempt from the consent requirement by our institution’s Institutional Review Board (Memorial Sloan Kettering Cancer Center, New York, NY). The study protocol including statistical analysis was prespecified a priori. Our study adheres to the applicable STROBE guidelines.
We obtained the NACOR Public User File from 2018. Cases from 2010 through 2018 with no primary surgical CPT code, cases with obstetric anesthesia codes, and cases of patients aged 0 to 18 were excluded from the initial NACOR dataset (Figure 1). Then, we used the AHRQ Clinical Classifications Software for Services and Procedures13 to select cases with a CPT code in category 166 for “Lumpectomy, quadrantectomy of breast” or category 167 for “Mastectomy”. We excluded CPT 19300 “Mastectomy for gynecomastia”.
Figure 1.
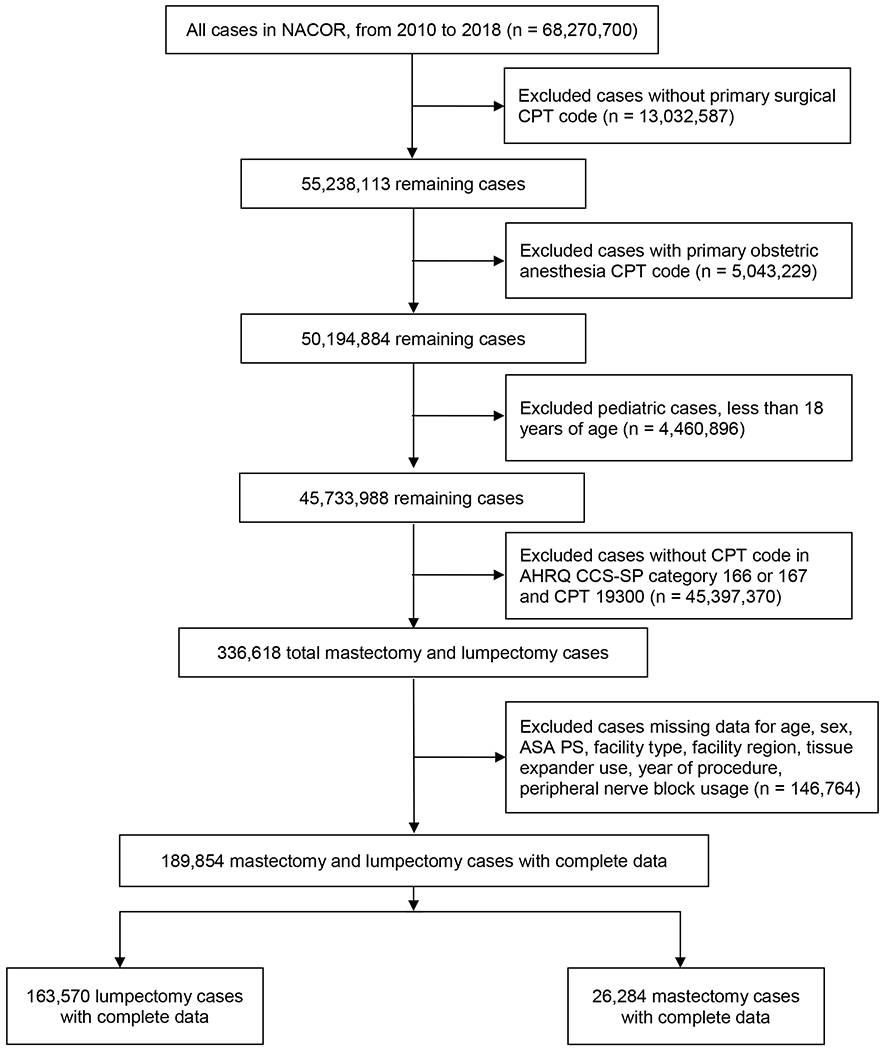
Study inclusion and exclusion criteria.
NACOR = National Anesthesia Clinical Outcomes Registry; CPT = Common Procedural Terminology; AHRQ CCS-SP = Agency for Healthcare Research and Quality Clinical Classifications Software for Services and Procedures; ASA PS = American Society of Anesthesiologists Physical Status.
We extracted information for the following variables: PNB type, age, sex, American Society of Anesthesiologists Physical Status (ASA PS), facility type, facility geographical region, procedure performed on workday versus holiday or weekend, tissue expander use, and year of procedure. PNB types were identified by secondary surgical CPT codes (Supplemental Digital Content 1, Table 1) and categorized as intercostal block, paravertebral block, and other blocks. When more than one CPT was present, the case was preferentially categorized in the order paravertebral, intercostal, transversus abdominis plane (TAP), brachial plexus. Diagnosis codes were not used. Other blocks included axillary, brachial, cervical, supraspinatus, and TAP blocks. The CPT code 64450 (“other peripheral nerve”) indicated a nerve block location that did not have a specific code. ASA PS was grouped into ASA PS ≤ 2 versus ASA PS >2. Categories for facility type included university hospitals, large community hospitals (>500 inpatient beds), medium community hospitals (100 to 500 inpatient beds), small community hospitals (<100 inpatient beds), and other facilities, which consisted of specialty hospitals, attached surgery centers, freestanding surgery centers, pain clinics, and surgeon offices. U.S. geographical regions based on facility included Northeast, Midwest, South, and West. Information regarding the day of the week on which the procedure was performed and whether the procedure was performed on a holiday allowed us to compare cases from regular workdays to cases performed during the weekend or on holidays. A case was determined to include a tissue expander if the CPT code 19357 was present.
The “primary anesthesia technique” field was not used to determine PNB status due to its missingness and non-specificity. In some practices “Regional” refers to a primary anesthetic using any neuraxial or peripheral block, while other practices only use “Regional” to refer to non-neuraxial nerve blocks. To improve the strength of the study, only CPT procedure codes were used to determine the presence of a PNB. The presence of an epidural nerve block procedure code (CPT codes 62310 through 62329) was used to identify cases that had an epidural catheter placed for post-operative analgesia.
Missingness in the NACOR dataset is described in Supplemental Digital Content 2. Checking of the missing completely at random (MCAR) assumption was conducted using Little’s MCAR test. We examined missingness patterns by procedure type (lumpectomy versus mastectomy), PNB use, age, sex, ASA PS, facility type, and facility geographical region. Since there were still a large number of observations complete for the main variables of interest, we chose a complete case analysis approach for this study. We included in the cohort all patients with complete data for age, sex, ASA PS, facility type, facility region, tissue expander status, year of procedure, and PNB use.
We calculated the proportion of cases using a PNB, separated by lumpectomy and mastectomy, for each year from 2010 to 2018. The denominator was determined by the total number of cases that met our study criteria. The numerator was determined by the number of cases that received PNB. Similarly, we calculated the proportion of PNB use according to PNB type, age, sex, ASA PS, facility type, facility region, procedure on weekday versus weekend or holiday, and use of tissue expander.
Statistical Analysis
Statistical analysis was performed separately for lumpectomy and mastectomy cases due to fundamental differences in procedure invasiveness. We treated case identifiers as independent. To assess potential nonlinearity of the relationship between year of procedure and PNB use and identify any breakpoints in longitudinal trends of PNB usage, we constructed a logistic regression for the odds of PNB against a restricted cubic spline for year of procedure. To confirm these findings, we performed a Cochran-Armitage trend test to assess the annual proportions of PNB use from 2010 to 2018. We accounted for nonlinearity by applying segmented logistic regression with mixed-effects clustered on facility identifier to assess PNB use before and after the identified breakpoint of 2014.14 The difference between the two slopes corresponding to the two time periods (prior to 2014 vs 2014 and beyond) are quantified using an interaction term between the dummy variable for post-2014 period (i.e., 0 if year of procedure < 2014 and 1 if year of procedure ≥ 2014) and the term (year of procedure - 2013). We assessed the association of patient and procedure characteristics with the year of procedure using a univariable logistic mixed effects model. Then, we built separate multivariable logistic regression models using the significant variables from the univariable models to obtain adjusted estimates for the relationship between year of procedure and PNB use. The variables age, gender, and ASA PS were forced into the multivariable models, as done in a previous study of regional anesthesia within the NACOR dataset.6 All analyses were conducted using R 3.6.2 (R Foundation, Vienna, Austria). Statistical tests were two-sided with P value for significance set at P < 0.001 due to the large sample size of this study.15
Results
Cohort
After exclusions, 189,854 cases in the original NACOR dataset of 68,270,700 cases had complete data for age, sex, ASA PS, facility type, facility region, tissue expander use, PNB use, and year of procedure. Of the cases with complete data, there were 26,284 (14%) mastectomies and 163,570 (86%) lumpectomies. There were 282 unique practice identifiers in the dataset and 1,166 unique facility identifiers. Of the 26,284 mastectomy cases, 728 (2.8%) received a PNB (Supplemental Digital Content 1, Table 2). This percentage was larger than the 518 of 163,570 (0.3%) lumpectomy cases with a PNB (Supplemental Digital Content 1, Table 3).
PNB types consisted of five categories: (1) axillary, brachial, cervical, or supraspinatus; (2) intercostal; (3) paravertebral; (4) TAP; and (5) other. Figure 2 shows the annual proportion of breast surgery cases with a PNB, grouped by mastectomy and lumpectomy. For both surgery types, intercostal block was the most frequently used PNB from 2011 to 2015. For mastectomy, paravertebral block was the most common in 2016 and 2017, while “Other” was the most common for lumpectomy. In 2018, “Other” is the leading category for both types of surgery. Of the five categories, the brachial plexus blocks and the TAP block comprised only 2.4% of all PNBs in the cohort (Supplementary Digital Content 1, Table 4).
Figure 2:
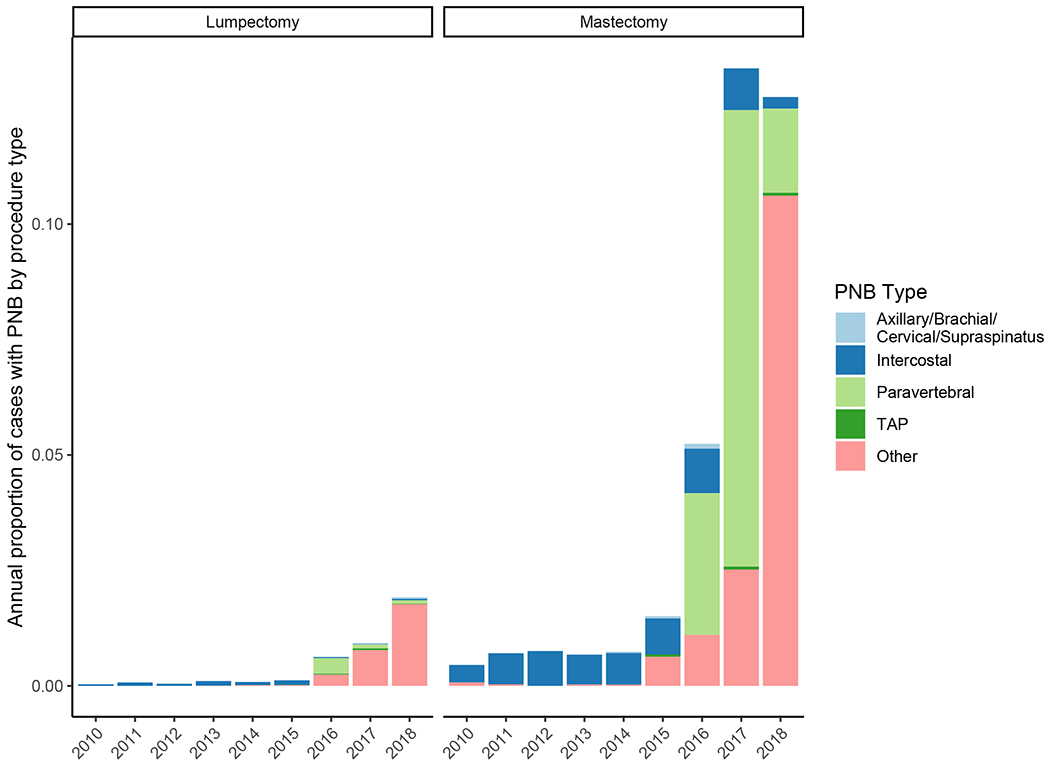
Annual proportion of peripheral nerve block type among complete cases by procedure type from 2010 to 2018.
TAP = transversus abdominis plane.
Of those mastectomy cases with a primary anesthesia type specified, almost all were General (98%). Among lumpectomy cases with a primary anesthesia type, 71% were General and 26% were MAC. Among all complete cases, only 73 had an epidural analgesia CPT code present. Of these cases, 66 had primary anesthesia type General, 1 was type MAC, and 6 had no type specified. In 5 of the mastectomy cases an epidural analgesia CPT code was present along with a PNB code.
Annual Peripheral Nerve Block Usage
The rates of PNB usage in lumpectomy and mastectomy saw an upward trend from 2010 to 2018 (Figure 2). The proportion of lumpectomy cases with PNB was less than 0.1% in 2010 and increased in each subsequent year to 1.9% in 2018. The proportion of mastectomy cases with PNB showed a larger increase from 0.5% in 2010 to 13% in 2018. There was a small exception to this trend in 2018 for the mastectomy cohort. Visual inspection of the relationship between year of procedure and proportion of PNB use from a restricted cubic spline model showed 2014 to be a breakpoint in both the mastectomy and lumpectomy cohorts (Figure 3). The Cochran-Armitage test showed an increase in PNB proportion over the years 2010 to 2018 (P < 0.0001 for mastectomy and lumpectomy). The univariable model showed significant violation of the linearity assumption, as can be seen in the relatively flat proportion of PNB prior to 2014, followed by a sharp increase after 2014 (ANOVA P = 0.0014 for mastectomy cohort, P = 0.0065 for lumpectomy cohort). For these reasons, a breakpoint at year 2014 was used for segmented regression for the year of procedure variable.
Figure 3.
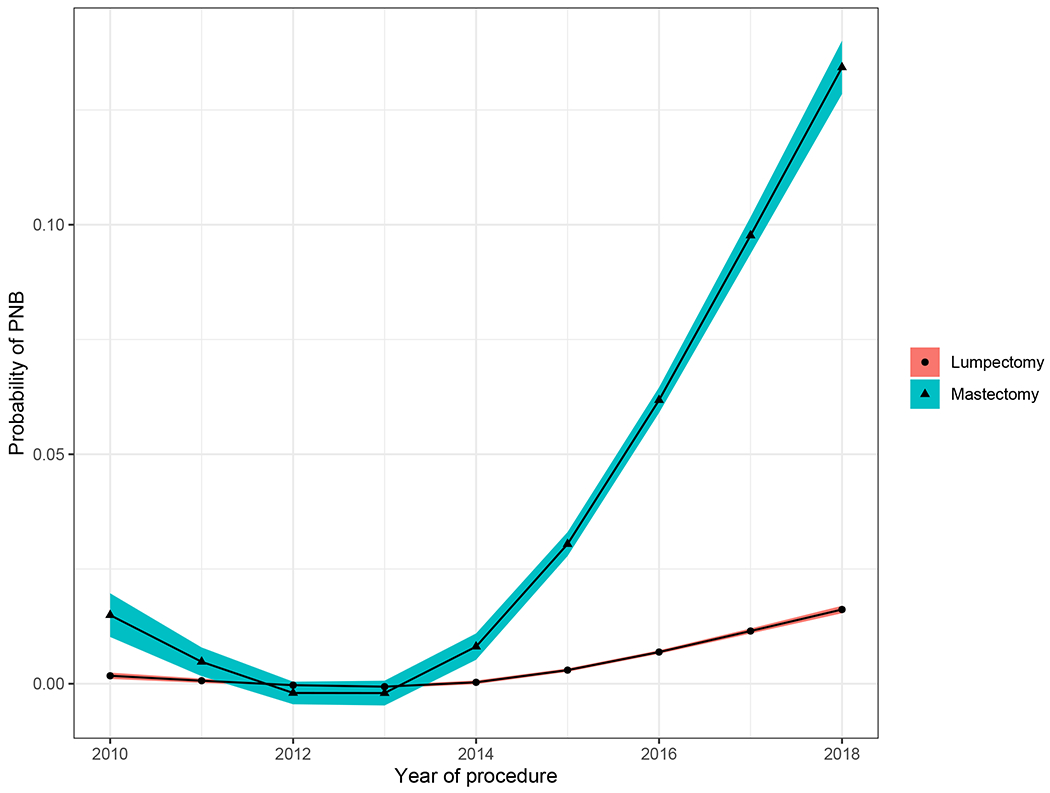
Probability of peripheral nerve block use in mastectomy and lumpectomy cohorts over time.
Shaded ribbon displays 95% confidence interval. PNB = peripheral nerve block.
The mastectomy univariable model showed an odds ratio (OR) of 0.87 for year prior to 2014 (95% confidence interval [CI] 0.71 – 1.07; P = 0.2), indicating little change in likelihood of PNB during this time period. During and after 2014, the odds of receiving PNB in the mastectomy cohort rose by a factor of 2.24 for every subsequent year (95% CI 2.00 – 2.49; P < 0.001), a significant increase in odds over time. There were similar findings in the lumpectomy cohort, with OR 1.08 (95% CI 0.84–1.39; P = 0.60) prior to 2014 and OR 2.03 (95% CI 1.81–2.27; P < 0.001) after 2014 (Table 1). For both mastectomy and lumpectomy, the interaction test for pre-2014 vs post-2014 was P < 0.001. These findings confirmed our hypothesis of increasing PNB use in both lumpectomy and mastectomy, with a significant increase occurring after 2014.
Table 1:
Segmented mixed-effects logistic regression model for PNB use
| Characteristic | Lumpectomy | Mastectomy | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Per year increase (year of procedure < 2014) | 1.08 | 0.84 – 1.39 | 0.55 | 0.87 | 0.71 – 1.07 | 0.19 |
| Per year increase (year of procedure ≥ 2014) | 2.03 | 1.81 – 2.27 | <0.001 | 2.24 | 2.00 – 2.49 | <0.001 |
Footnote: Comparisons of post-2014 vs pre-2014 slopes (i.e., interaction term): For lumpectomy: p<0.001; for mastectomy: p<0.001.
Univariable mixed-effects logistic regression clustering on facility ID, with PNB status as outcome. ASA PS = American Society of Anesthesiologists Physical Status; CI = confidence interval; OR = odds ratio; PNB = peripheral nerve block.
In the univariable model for mastectomy, the following variables were associated with PNB: age, sex, ASA PS >2, facility region, and tissue expander use (Supplemental Digital Content 1, Table 5). In the multivariable model, year of procedure during or after 2014, sex, facility region, and tissue expander use were found to be significant. The adjusted odds of receiving PNB in mastectomy was 2.25 (95% CI 2.00 – 2.52, P < 0.001) each year during and after 2014 (Table 2).
Table 2.
Multivariable mixed-effects logistic regression analysis of PNB use among mastectomy cases.
| Characteristic | OR | 95% CI | P value |
|---|---|---|---|
| Per year increase (year of procedure < 2014) | 0.71 | 0.58 – 0.88 | 0.002 |
| Per year increase (year of procedure ≥ 2014) | 2.25 | 2.00 – 2.52 | <0.001 |
| Age at procedure, years | 0.99 | 0.98 – 1.00 | 0.004 |
| Male (vs Female) | 0.31 | 0.16 – 0.60 | <0.001 |
| ASA PS >2 | 0.87 | 0.69 – 1.10 | 0.25 |
| Facility Region | |||
| Region 1 Northeast | — | — | |
| Region 2 Midwest | 10.2 | 3.33 – 31.5 | <0.001 |
| Region 3 South | 2.98 | 0.87 – 10.3 | 0.084 |
| Region 4 West | 7.20 | 2.01 – 25.8 | 0.002 |
| Has tissue expander | 15.4 | 10.3 – 23.1 | <0.001 |
Footnote: Comparisons of post-2014 vs pre-2014 slopes (i.e., interaction term): p<0.001
Multivariable mixed-effects logistic regression clustering on facility ID, with PNB status as outcome in mastectomy cohort. ASA PS = American Society of Anesthesiologists Physical Status; CI = confidence interval; OR = odds ratio; PNB = peripheral nerve block.
In the univariable model for the lumpectomy cohort, age, sex, ASA PS >2, and facility region were associated with PNB (Supplemental Digital Content 1, Table 6). The multivariable model showed year of procedure during or after 2014 and facility region to be associated with PNB use. The adjusted odds of receiving PNB in lumpectomy was 1.81 (95% CI 1.61 – 2.03, P < 0.001) each year during or after 2014 (Table 3).
Table 3.
Multivariable mixed-effects logistic regression analysis of PNB use among lumpectomy cases.
| Characteristic | OR | 95% CI | P value |
|---|---|---|---|
| Per year increase (year of procedure < 2014) | 1.17 | 0.91 – 1.51 | 0.22 |
| Per year increase (year of procedure ≥ 2014) | 1.81 | 1.61 – 2.03 | <0.001 |
| Age at procedure, years | 1.01 | 1.00 – 1.01 | 0.14 |
| Male (vs Female) | 0.65 | 0.28 – 1.52 | 0.32 |
| ASA PS >2 | 1.09 | 0.86 – 1.37 | 0.47 |
| Facility Region | |||
| Region 1 Northeast | — | — | |
| Region 2 Midwest | 20.2 | 8.27 – 49.2 | <0.001 |
| Region 3 South | 6.60 | 1.96 – 22.2 | 0.002 |
| Region 4 West | 9.50 | 2.58 – 35.0 | <0.001 |
Footnote: Comparisons of post-2014 vs pre-2014 slopes (i.e., interaction term): p=0.006
Multivariable mixed-effects logistic regression clustering on facility ID, with PNB status as outcome in lumpectomy cohort. ASA PS = American Society of Anesthesiologists Physical Status; CI = confidence interval; OR = odds ratio; PNB = peripheral nerve block.
Discussion
To our knowledge, this is the first national study to evaluate the frequency of PNB use for breast cancer surgery. Our retrospective analysis of the NACOR database showed a dramatic increase in PNB usage in mastectomy cases on a national level since 2014. PNB usage for lumpectomy has also increased although at a more modest rate. We believe that a greater understanding of the benefits of PNB has encouraged more anesthesiologists to use the technique in breast surgery anesthesia practice.
Many standardized pathways have incorporated regional anesthesia as part of their ERP for improvements in mobilization, pain, and surgical stress reduction.16 Other reasons for the rise in annual proportion of PNB use in breast cancer surgery may include adoption of ultrasound guidance, greater emphasis on learning PNB techniques, and increased expertise in regional anesthesia over time. In the years leading to 2014, there were studies suggesting the adoption of ERP for breast cancer surgery that encouraged PNB.17 FDA testing for the use of liposomal bupivacaine in nerve blocks occurred during this time as well.18
The NACOR database is ideal for this research question because it is the only generally available national registry that includes complete procedure codes for each anesthetic. An incentive for participating in NACOR is to gain compliance with the federal Quality Payment Program under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). Since MACRA requires accurate procedure code reporting, participating practices are likely to submit complete data on surgical and anesthesia procedure codes.
Mastectomy was underreported in NACOR compared to findings reported by the AHRQ, which reported 30,101 unilateral and bilateral mastectomy cases across 13 states in the year 2013 for women.2 Our final dataset included 3,399 mastectomy cases for both men and women in the year 2013. However, we believe our findings represent national trends in PNB usage because the NACOR cohort has been growing over time, becoming more representative of all practices with each year. The average age of mastectomy patients in our dataset was 61 years, which was comparable to the average age of bilateral and unilateral mastectomy cases (58 years) reported by AHRQ in 2013.2
The rate of PNB for mastectomy was much higher than that of lumpectomy. This was expected, as mastectomy is a more invasive procedure. There are prospective studies and case reports of PNB used for lumpectomy, with mention of reasons pertaining to patient candidacy for general anesthesia (e.g. elderly age and co-morbidities).19,20 PNB may not have been frequently used for lumpectomy because there is insufficient evidence that PNB for lumpectomy results in significantly better postoperative outcomes.
Paravertebral blocks appear as a separate category in 2016 due to the introduction of a specific CPT code for the procedure that same year.21 There is no specific CPT code for novel “plane blocks” including pectoral nerve (Pecs) blocks,22 which are increasingly described for breast surgery and may also reduce pain and opioid consumption.23 Therefore, we speculate that many of the cases encompassed by the “Other” category may well be fascial plane blocks. While surgical and anesthetic procedural coding is highly regulated in the United States, coding practices do differ between institutions. There can be subtle variations in how similar information is reported given the differences in coding software and local practice.
In addition to year of procedure, our mixed-effects logistic regression showed facility region to be associated with PNB utilization in both mastectomy and lumpectomy. Procedures performed in facilities located in the Midwest were more likely to receive PNB. The increase in proportion of PNB reported by university hospitals is likely accounted for by residency and fellowship training. Regional anesthesiology and acute pain medicine (RAAPM) fellowships began accreditation with the Accreditation Council for Graduate Medical Education (ACGME) in 2016. In 2017, twelve RAAPM fellowship programs received ACGME accreditation.24 The voluntary nature of NACOR reporting may have resulted in an over- or underrepresentation of practices in the Midwest compared to the actual national distribution.
Mastectomies with a tissue expander were more likely to receive PNB. Given the anticipated postoperative pain associated with tissue expander use,25 this finding was consistent with our expectations that anesthesiologists are more likely to offer a PNB to patients undergoing mastectomy with tissue expander placement.
An occasionally cited indication for PNB use is patients with advanced age and/or severe comorbidities who may poorly tolerate general anesthesia.26 However, the multivariable models in this study did not show a significant relationship between PNB use and age or ASA PS > 2. In the mastectomy cohort the age covariate OR of 0.99 (95% CI 0.98 – 1.00) shows a lack of any clinically significant effect of age.
No significant association was found between cases being performed on the weekend and use of PNB. Even though many anesthesia practices have fewer staff present on weekends,27 weekend cases do not reduce the likelihood of a PNB being administered for mastectomy or lumpectomy.
The presence of brachial plexus and transverse abdominal plane nerve block codes (2.4% of PNBs) is unexpected given that the nerves anesthetized in these blocks incompletely innervate the breast. These codes could be present due to the mastectomy or lumpectomy being performed at the same time as a separate procedure that would benefit from the block, a coding error by the proceduralist or biller, or a frank knowledge deficit on the part of the proceduralist.
The voluntary nature of NACOR submissions raises the potential for bias. Because the threshold to participate is easily attainable, the aggregation of data appears extremely heterogenous due to the wide variety of contributors. Therefore, NACOR is not a completely random sample of U.S. anesthesia care. This was reflected in our missingness analysis that showed that the data was not missing completely at random. Other studies have found missingness to be an issue in NACOR as well, leading the need to strike a difficult balance between generalizability and validity.28 Initiatives to improve reporting in a manner that allows more consistency between practices and geographical regions would improve NACOR analyses in the future so that studies may provide a more comprehensive, accurate picture of U.S. anesthesia practices.
While we presume that all mastectomy cases are due to primary or secondary breast cancer, a minority of lumpectomy surgeries are performed for benign lesions. We were unable to discern which lumpectomy surgeries were true cancer surgeries because postoperative pathology results are not available in this data set.
According to Centers for Medicare and Medicaid Services (CMS) guidelines, a separate PNB charge may only be submitted if the nerve block is not the primary anesthetic.29 Thus, our count of PNBs may be an underestimate because any case with a primary anesthesia type other than “general” would not have a PNB CPT included.
Most studies articulating general trends in regional anesthesia usage are primarily focused on orthopedic surgery. This study is one of the first to discuss patterns in the use of PNB in oncologic surgery within the U.S., and our findings reflect those of prior non-oncologic studies.6,7 Identifying factors that predict PNB usage is useful in probing deeper into eccentricities in anesthesia practice that need to be addressed. Future research is warranted in investigating the role of PNB in less invasive anterior chest wall procedures, similar to lumpectomy. Evaluating other national databases such as the ACS NSQIP for patterns in nerve block use would also be informative.
Supplementary Material
Key Points.
Question: How has the utilization of peripheral nerve blocks for mastectomy and lumpectomy procedures changed in recent years?
Findings: There has been an increase in annual proportion of peripheral nerve block usage in mastectomy and lumpectomy since 2010 in the United States, with a more accelerated increase in the years 2014 to 2018.
Meaning: Peripheral nerve blocks are infrequently used for breast surgery in the United States, but utilization is increasing.
Acknowledgments
Sources of support that require acknowledgement:
The research was supported by the National Cancer Institute of the National Institutes of Health under Award Numbers R25CA020449 and P30CA008748. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Glossary of Terms
- ERP
enhanced recovery program
- PNB
peripheral nerve block
- AQI
Anesthesia Quality Institute
- NACOR
National Anesthesia Clinical Outcomes Registry
- ACS NSQIP
American College of Surgeons National Surgical Quality Improvement Program
- AHRQ
Agency for Healthcare Research and Quality
- CPT
Common Procedural Terminology
- ICD
International Classification of Diseases
- ASA PS
American Society of Anesthesiologists Physical Status
- TAP
transversus abdominis plane
- MCAR
missing completely at random
- OR
odds ratio
- CI
confidence interval
- MACRA
Medicare Access and CHIP Reauthorization Act
- RAAPM
regional anesthesiology and acute pain medicine
- ACGME
Accreditation Council for Graduate Medical Education
- CMS
Centers for Medicare and Medicaid Services
Footnotes
Financial disclosures: Anoushka Afonso provided one-time consulting for Merck, unrelated to this study, in 2019. Dr McCormick’s spouse holds stock in Johnson & Johnson.
Conflicts of interest: The authors report no conflicts of interest.
Contributor Information
Stephanie Lam, Department of Anesthesiology and Critical Care Medicine, Memorial Sloan Kettering Cancer Center; Philadelphia College of Osteopathic Medicine.
Helena Qu, Department of Anesthesiology and Critical Care Medicine, Memorial Sloan Kettering Cancer Center; University of Mississippi Medical Center.
Margaret Hannum, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center.
Kay See Tan, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center.
Anoushka Afonso, Department of Anesthesiology and Critical Care Medicine, Memorial Sloan Kettering Cancer Center; Department of Anesthesiology, Weill Cornell Medicine.
Hanae K. Tokita, Department of Anesthesiology and Critical Care Medicine, Memorial Sloan Kettering Cancer Center.
Patrick J. McCormick, Department of Anesthesiology and Critical Care Medicine, Memorial Sloan Kettering Cancer Center; Department of Anesthesiology, Weill Cornell Medicine.
References
- 1.American Cancer Society. Cancer Facts & Figures 2019. Atlanta, GA, 2019. Available at: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf. [Google Scholar]
- 2.Steiner CA, Weiss AJ, Barrett ML, Fingar KR, Davis PH. Trends in Bilateral and Unilateral Mastectomies in Hospital Inpatient and Ambulatory Settings, 2005-2013. HCUP Statistical Brief #201. February 2016. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb201-Mastectomies-Inpatient-Outpatient.pdf. Accessed October 28, 2020. [PubMed] [Google Scholar]
- 3.Hopkins PM. Does regional anaesthesia improve outcome? Br J Anaesth 2015;115:26–33. [DOI] [PubMed] [Google Scholar]
- 4.Kessler J, Marhofer P, Hopkins PM, Hollmann MW. Peripheral regional anaesthesia and outcome: lessons learned from the last 10 years. Br J Anaesth 2015;114:728–45. [DOI] [PubMed] [Google Scholar]
- 5.Chiu C, Aleshi P, Esserman LJ, Inglis-Arkell C, Yap E, Whitlock EL, Harbell MW. Improved analgesia and reduced post-operative nausea and vomiting after implementation of an enhanced recovery after surgery (ERAS) pathway for total mastectomy. BMC Anesthesiol 2018;18:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gabriel RA, Ilfeld BM. Use of Regional Anesthesia for Outpatient Surgery Within the United States. Anesth Analg 2018;126:2078–84. [DOI] [PubMed] [Google Scholar]
- 7.Cozowicz C, Poeran J, Memtsoudis SG. Epidemiology, trends, and disparities in regional anaesthesia for orthopaedic surgery. Br J Anaesth 2015;115:57–67. [DOI] [PubMed] [Google Scholar]
- 8.Anesthesia Quality Institute. 2019 NACOR User Guide. 2019. Available at: https://www.aqihq.org/files/MIPS/2019/2019_NACOR_User_Guide_FINAL_OCT_2019.pdf. Accessed October 28, 2020.
- 9.Matel B ACS NSQIP Participant Use Data File. 2020. Available at: https://www.facs.org/quality-programs/acs-nsqip/participant-use. Accessed October 28, 2020.
- 10.Agency for Healthcare Research and Quality. Overview of the Nationwide Ambulatory Surgery Sample (NASS). 2020. Available at: https://www.hcup-us.ahrq.gov/nassoverview.jsp. Accessed October 28, 2020.
- 11.Liau A, Havidich JE, Onega T, Dutton RP. The National Anesthesia Clinical Outcomes Registry. Anesth Analg 2015;121:1604–10. [DOI] [PubMed] [Google Scholar]
- 12.Dutton RP. Making a difference: the Anesthesia Quality Institute. Anesth Analg 2015;120:507–9. [DOI] [PubMed] [Google Scholar]
- 13.Healthcare Cost and Utilization Project (HCUP). HCUP CCS-Services and Procedures. 2018. Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp. Accessed October 28, 2020.
- 14.Bates DM, Watts DG. Practical Considerations in Nonlinear Regression. In: Nonlinear regression analysis and its applications. New York, NY, USA: John Wiley & Sons, Ltd, 2008:67–133. Available at: http://doi.wiley.com/10.1002/9780470316757.ch3. [Google Scholar]
- 15.Ioannidis JPA. The proposal to lower P value thresholds to .005. JAMA 2018;319:1429–30. [DOI] [PubMed] [Google Scholar]
- 16.McIsaac DI, Cole ET, McCartney CJL. Impact of including regional anaesthesia in enhanced recovery protocols: a scoping review. Br J Anaesth 2015;115:ii46–56. [DOI] [PubMed] [Google Scholar]
- 17.Arsalani-Zadeh R, ELFadl D, Yassin N, MacFie J. Evidence-based review of enhancing postoperative recovery after breast surgery. Br J Surg 2011;98:181–96. [DOI] [PubMed] [Google Scholar]
- 18.Ilfeld BM, Malhotra N, Furnish TJ, Donohue MC, Madison SJ. Liposomal bupivacaine as a single-injection peripheral nerve block: A dose-response study. Anesth Analg 2013;117:1248–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim D- H, Kim S, Kim CS, Lee S, Lee I- G, Kim HJ, Lee J- H, Jeong S- M, Choi KT. Efficacy of Pectoral Nerve Block Type II for Breast-Conserving Surgery and Sentinel Lymph Node Biopsy: A Prospective Randomized Controlled Study. Pain Res Manag 2018;2018:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ueshima H, Otake H. A combination of an erector spinae plane block and a transversus thoracic muscle plane block for partial mastectomy. J Clin Anesth 2019;54:1. [DOI] [PubMed] [Google Scholar]
- 21.Vorenkamp K Performance and Documentation of Imaging Guidance. Timely Topics: Payment and Practice Management. 2016. Available at: https://www.asahq.org/-/media/sites/asahq/files/public/resources/practice-management/ttppm/2016-10-13-performance-and-documentation-for-imaging.pdf. Accessed October 28, 2020.
- 22.Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): A novel approach to breast surgery. Revi Esp Anestesiol Reanim 2012;59:470–5. [DOI] [PubMed] [Google Scholar]
- 23.Lovett-Carter D, Kendall MC, McCormick ZL, Suh EI, Cohen AD, De Oliveira GS. Pectoral nerve blocks and postoperative pain outcomes after mastectomy: a meta-analysis of randomized controlled trials. Reg Anesth Pain Med 2019;44:923–8. [DOI] [PubMed] [Google Scholar]
- 24.Mariano ER, Rosenquist RW. The road to accreditation for fellowship training in regional anesthesiology and acute pain medicine. Curr Opin Anaesthesiol 2018;31:643–8. [DOI] [PubMed] [Google Scholar]
- 25.Kulkarni AR, Pusic AL, Hamill JB, Kim HM, Qi J, Wilkins EG, Roth RS. Factors associated with acute postoperative pain following breast reconstruction. JPRAS Open 2017;11:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pawa A, Wight J, Onwochei DN, Vargulescu R, Reed I, Chrisman L, Pushpanathan E, Kothari A, El-Boghdadly K. Combined thoracic paravertebral and pectoral nerve blocks for breast surgery under sedation: a prospective observational case series. Anaesthesia 2018;73:438–43. [DOI] [PubMed] [Google Scholar]
- 27.Dexter F, Dutton RP, Kordylewski H, Epstein RH. Anesthesia Workload Nationally During Regular Workdays and Weekends. Anesth Analg 2015;121:1600–3. [DOI] [PubMed] [Google Scholar]
- 28.Andreae MH, Gabry JS, Goodrich B, White RS, Hall C. Antiemetic Prophylaxis as a Marker of Health Care Disparities in the National Anesthesia Clinical Outcomes Registry. Anesth Analg 2018;126:588–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Society of Anesthesiologists. Reporting postoperative pain procedures in conjunction with anesthesia. 2015. Available at: https://www.asahq.org/-/media/sites/asahq/files/public/resources/standards-guidelines/reporting-postoperative-pain-procedures-in-conjunction-with-anesthesia.pdf. Accessed October 28, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


