Abstract
Purpose:
The spread of COVID-19 and the associated stay-at-home orders and shutdowns of gyms and fitness centers has drastically influenced health behaviors leading to widespread reductions in physical activity (PA). The recent Call to Action from the American College of Sports Medicine has promoted “innovative strategies to promote PA during the COVID-19 pandemic”. We aimed to identify individual-level factors that protected against declines in PA levels amid the COVID-19 restrictions.
Methods:
We utilized the Pennington Biomedical COVID-19 Health Behaviors Survey for our analyses and used mixed-effect linear and generalized linear models to estimate the effects of individual-level factors on changes in PA levels during the COVID-19 restrictions.
Results:
Participants (n=4,376) provided information on PA behaviors before and during the COVID-19 shutdown. Overall, PA levels declined by a mean (SD) of 112 (1,460) MET minutes/week during the COVID-19 shutdown; however, changes in PA were heterogeneous, with 55% of the participants reporting increases in or maintenance of PA during that time. Several social and demographic factors were significantly related to declines in PA, including high pre-pandemic PA levels, living alone (difference=118 MET minutes/week), low household income (difference between the highest and lowest income group=363 MET minutes/week), COVID-19-related changes in income (difference=110 MET minutes/week), and loss of employment (difference=168 MET minutes/week). Substitution of pre-pandemic gym attendance with the purchase and use of home exercise equipment or exercise through virtual fitness platforms promoted increases in PA during the COVID-19 shutdown.
Conclusions:
While promoting PA through the COVID-19 pandemic, it is important to consider demographic factors, which greatly influence health behaviors and implementation of, and access to, replacement behaviors. Promotion of such strategies could help maintain PA levels during potential future stay-at-home orders.
Keywords: gym, exergaming, fitness, self-monitoring, income, social support
INTRODUCTION
Coronavirus disease (COVID-19) is an infectious disease that is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The highly transmissible virus is spread primarily through close contact with infected people, when saliva or respiratory secretions and/or (airborne) droplets from infected individuals are expelled during coughs, sneezes or while talking (1). To date, COVID-19 has affected over 74 million people in nearly 200 countries worldwide (2). Due to the rapid global increase in COVID-19 cases in early 2020, the World Health Organization (3) and Centers for Disease Control and Prevention (CDC) (4) released statements advising the public to reduce both international and domestic travel and to practice social distancing as basic means of limiting exposure to the highly transmittable virus. To enforce these precautions and effectively slow the spread of the virus, many countries subsequently issued stay-at-home orders and shutdowns of non-essential businesses and public places.
In the U.S., the duration of these mandated restrictions varied by state, though in general, they were in effect between late March/early April to mid-to-late May 2020 (5, 6). In most states and many countries around the world, the mandated shutdowns included gyms and fitness centers. Together with the directives against public gatherings and joint participation in outdoor activities, including physical activity (PA) and exercise, stay-at-home orders substantially affected the daily PA routine of millions of people. Several reports indicate overall declines in PA and subsequent increases in sedentary time as a result of the COVID-19-related restrictions (7-10). These detrimental changes contribute to deconditioning and reductions in cardiorespiratory fitness and have been shown to be associated with an increased risk for chronic health conditions such as obesity and cardiometabolic disease as well as with all-cause mortality (11-13). Importantly, maintaining PA and exercise amid the COVID-19 pandemic is a crucial preventative measure to reduce adverse outcomes and improve survival (14).
The recent Call to Action statement from the American College of Sports Medicine (ACSM) aims to address the shutdown-related declines in PA and encourages the use of “innovative strategies to promote PA during the COVID-19 pandemic” that follow mitigation guidelines (15). Previous analyses show that there is substantial heterogeneity in the behavioral response to the pandemic (8, 16-18), wherein not all individuals experience the aforementioned restriction-related decline in PA and some individuals may have adopted specific strategies to maintain PA levels despite restrictions, demonstrating a resilient phenotype. However, it is important to acknowledge that it will be difficult for many to safely engage in regular exercise, depending on individual circumstances.
There are several known barriers to engagement in regular PA. These include a perceived lack of time, energy, or motivation, high costs for memberships or equipment, and a lack of facilities, among others (19). Many of these factors are likely to be exacerbated during shutdowns associated with the COVID-19 pandemic. As mentioned in the Call to Action, we need creative strategies to combat declines in PA in the face of significant barriers to PA (15). However, we cannot ignore that many PA barriers and facilitators are also likely to be influenced by sociodemographic factors and financial resources (20), and that those with low income or loss of income may be at a disproportionate disadvantage in regards to maintaining PA levels in the face of the pandemic. Unfortunately, this may in turn widen existing health disparities.
The purpose of this secondary analysis of the Pennington Biomedical COVID Health Behaviors Survey was to identify individual-level factors that helped people maintain PA levels amid the initial COVID-19 shutdown. Findings from this analysis may inform additional recommendations for the general public and the development of targeted interventions as the pandemic continues. We hypothesized that mitigation measures in response to the COVID-19 pandemic would result in lifestyle changes (e.g., change in income, working from home) that significantly influence PA levels, and that those with the highest levels of PA prior to COVID-19 would be most affected. We also hypothesized that those who self-monitor PA with wearable fitness trackers would be more protected against a decline due to regular feedback on behavior and an increased ability to detect change. We expected that individuals who replaced previous active behaviors (i.e., going to the gym) with alternative behaviors would have attenuated declines in PA during the shutdown.
METHODS
Design and Participants
This study was approved by the Institutional Review Board at Pennington Biomedical Research Center (PBRC), and adults 18 years of age or older with access to the internet were eligible to participate (16). A link to the anonymous survey was distributed by paid advertisements on social media platforms, PBRC’s webpage, email listservs, and word of mouth between April 3, 2020 and May 3, 2020. Upon opening the survey link, interested individuals received instructions that detailed the purpose of the study. Participants verified that they were adults and provided consent to participate before proceeding with the survey. Deidentified data were collected using REDCap (Research Electronic Data Capture) (21). Participation in the survey was voluntary and no compensation was provided.
Online Survey
The survey captured information across five domains: (1) demographics and household information, (2) PA and sedentary behavior, (3) diet, (4) sleep, and (5) mental health. Survey items included modifications from validated questionnaires together with investigator-created questions unique to this survey’s aims and the COVID-19 pandemic. PA, diet, and mental health domains included short-form and long-form instruments, in which participants could provide more detailed responses if desired. The protocol for the survey is registered with the PhenX Toolkit as a COVID-19 related measurement protocol (22).
For the purpose of the analyses reported herein, we utilized data from the long-form PA questionnaire with 12 items assessing PA behavior both pre- and during-shutdown. This instrument was modified from the Nurses’ Health Study Physical Activity Questionnaire (23), and activities included walking, jogging, running, bicycling, lap swimming, aerobic exercise, low-intensity exercise, household activities, resistance training, sports, using online exercise videos, and exergaming. We calculated total minutes of PA and metabolic equivalent (MET) minutes pre- and during-shutdown to examine change over time. METs for the different forms of PA, as reported by participants, were selected from the Compendium of Physical Activities (24). Survey items used the phrase “before” or “since the COVID-19 outbreak in your country or region”. From the survey, we also extracted information on the use of personal fitness trackers, gym memberships, the purchase of home exercise equipment during stay-at-home orders, and accessing virtual fitness classes as potential influences on change in PA. Virtual fitness included either online exercise videos or exergaming.
Statistical Analyses
Descriptive statistics were used for demographic data and are presented as mean (± SD) or frequency (percent). Differences between groups were examined with t-tests for continuous variables and chi-squared statistics for categorical variables. Main effects of individual-level characteristics on the change in PA levels (MET minutes or absolute minutes per week) were assessed with mixed-effect linear models/generalized linear models, and differences between groups were assessed using post-hoc pairwise comparisons applied to least squared means. All models had no covariates, unless otherwise specified. All analyses were conducted by a Center biostatistician (RAB) in SAS version 9.4 with alpha ≤ 0.05 as the predetermined level of significance. Model outcomes are presented as mean ± standard error (SE). Figures were produced in GraphPad Prism version 8.
RESULTS
Participant characteristics
A total of 7,753 adults participated in the online survey (16) and 4,376 participants completed the long-form PA questionnaire required for inclusion in the present analysis. Participant characteristics are provided in Table 1; the number of responses differed among some of the individual survey items, as all responses were voluntary, and participants could choose not to answer certain questions. On average, participants (80% female) were 52 (± 15) years old and had a BMI of 28.7 (± 7.0) kg/m2, with equal distribution across the BMI categories of healthy weight (33%), overweight (32%), and obesity (34%). Most participants (81%) reported a household size >1, and 38% had one or more dependents living in their household. Household income was relatively equally distributed across all income categories, with 52% of participants reporting an annual household income between $10,000 and $100,000. One third of participants faced income changes due to COVID-19 and 15% reported being laid off from their job. On average, participants reported being physically active during 348 (± 403) minutes/week prior to COVID-19 and reaching a mean of 1,453 (± 1,982) MET minutes/week. Forty-three percent of participants reported using wearable fitness trackers and 35% had memberships to a gym prior to COVID-19.
Table 1.
Participant characteristics.
| All participants (N=4,376) |
No change or Increase in PA (n=2,409) |
Decrease in PA (n=1,967) |
P-value | |
|---|---|---|---|---|
| DEMOGRAPHICS | ||||
| Sex, n (%) † | ||||
| Male | 849 (19.5) | 448 (18.7) | 401 (20.4) | 0.14 |
| Female | 3,515 (80.5) | 1,953 (81.3) | 1,562 (79.6) | |
| Age (years), mean (SD) ‡ | 52.0 (15.2) | 52.2 (14.9) | 51.8 (15.5) | 0.39 |
| Race * | ||||
| White | 3,920 (89.6) | 2,179 (90.5) | 1,741 (88.5) | 0.05 |
| Black | 195 (4.5) | 105 (4.4) | 90 (4.6) | |
| Other | 261 (6.0) | 125 (5.2) | 136 (6.9) | |
| BMI category, n (%) ¶ | ||||
| Underweight (<18.5 kg/m2) | 60 (1.6) | 32 (1.5) | 28 (1.6) | 0.76 |
| Healthy weight (18.5 – 24.9 kg/m2) | 1,257 (32.6) | 686 (32.0) | 571 (33.4) | |
| Overweight (25.0 – 29.9 kg/m2) | 1,215 (31.5) | 687 (32.0) | 528 (30.9) | |
| Obese (≥30.0 kg/m2) | 1,321 (34.3) | 739 (34.5) | 582 (34.1) | |
| BMI (kg/m2), mean (SD) ¶ | 28.7 (7.0) | 28.7 (7.0) | 28.7 (7.1) | 0.94 |
| Size of household, n (%) * | ||||
| 1 Person | 830 (19.0) | 435 (18.1) | 395 (20.1) | 0.09 |
| >1 Person | 3,546 (81.0) | 1,974 (81.9) | 1,572 (79.9) | |
| Dependents in household, n (%) § | ||||
| None | 2,184 (61.6) | 1,192 (60.4) | 992 (63.1) | 0.10 |
| ≥1 | 1,362 (38.4) | 782 (39.6) | 580 (36.9) | |
| Household income, n (%) * | ||||
| < US$ 10,000/year | 213 (4.9) | 112 (4.6) | 101 (5.1) | 0.06 |
| US$ 10,000 – 49,999/year | 1,099 (25.1) | 602 (25.0) | 497 (25.3) | |
| US$ 50,000 – 99,999/year | 1,195 (27.3) | 630 (26.2) | 565 (28.7) | |
| US$ 100,000 – 149,999/year | 639 (14.6) | 378 (15.7) | 261 (13.3) | |
| ≥ US$ 150,000/year | 531 (12.1) | 311 (12.9) | 220 (11.2) | |
| Prefer not to answer | 699 (16.0) | 376 (15.6) | 323 (16.4) | |
| Change in income due to COVID-19, n (%) * | ||||
| No | 2,817 (64.4) | 1,607 (66.7) | 1,210 (61.5) | <0.01 |
| Yes | 1,559 (35.6) | 802 (33.3) | 757 (38.5) | |
| Laid off or furloughed from job due to COVID-19, n (%) * | ||||
| No | 2,517 (57.5) | 1,412 (58.6) | 1,105 (56.2) | 0.06 |
| Yes | 649 (14.8) | 330 (13.7) | 319 (16.2) | |
| N/A, not working prior to COVID-19 | 1,210 (27.7) | 667 (27.7) | 543 (27.6) | |
| Working from home due to COVID-19, n (%) * | ||||
| No | 1,635 (37.4) | 859 (35.7) | 776 (39.5) | 0.02 |
| Yes | 1,411 (32.2) | 818 (34.0) | 593 (30.1) | |
| Already working from home prior to COVID-19 | 146 (3.3) | 85 (3.5) | 61 (3.1) | |
| N/A, not working prior to COVID-19 | 1,184 (27.1) | 647 (26.9) | 537 (27.3) | |
| PHYSICAL ACTIVITY & HEALTH | ||||
| Use of wearable fitness tracker, n (%) * | ||||
| No | 2,486 (56.8) | 1,410 (58.5) | 1,076 (54.7) | 0.01 |
| Yes | 1,890 (43.2) | 999 (41.5) | 891 (45.3) | |
| Gym membership prior to COVID-19, n (%) * | ||||
| No | 2,837 (64.8) | 1,701 (70.6) | 1,136 (57.8) | <0.01 |
| Yes | 1,539 (35.2) | 708 (29.4) | 831 (42.3) | |
| Purchase of fitness equipment during COVID-19, n (%) * | ||||
| No | 3,702 (84.6) | 2,047 (85.0) | 1,655 (84.1) | 0.45 |
| Yes | 674 (15.4) | 362 (15.0) | 312 (15.9) | |
| Total minutes/week prior to COVID-19, mean (SD) * | 348.1 (403.1) | 268.5 (358.2) | 445.5 (432.6) | <0.01 |
| Total MET minutes/week prior to COVID-19, mean (SD) * | 1,453.4 (1,981.9) | 1,101.2 (1,751.2) | 1,884.7 (2,155.6) | <0.01 |
We used t-tests for continuous variables and chi-square statistics for categorical variables to test for differences between participants who did not change or increased PA and those who decreased PA. Bold font denotes a significant difference (P<0.05).
Data available for 4,364 of 4,376 participants.
Data available for 4,373 of 4,376 participants.
Data available for 4,376 of 4,376 participants.
Data available for 3,853 of 4,376 participants.
Data available for 3,546 of 4,376 participants.
Abbreviations: BMI, body mass index; COVID-19, coronavirus disease; MET, metabolic equivalent; PA, physical activity; SD, standard deviation.
Demographics/employment factors
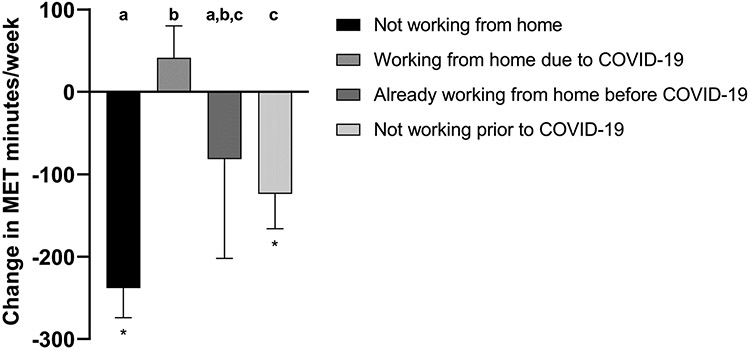
Overall, PA levels declined across the study sample (−112 ± 1,460 MET minutes/week, or −18 ± 306 absolute minutes/week), though PA changes were heterogeneous (Figure 1). While 1,967 participants (45%) reported a decline of more than 5 minutes/week, 2,409 (55%) reported that PA levels remained relatively unchanged (within ± 5 minutes/week) or even increased since the outbreak of the pandemic in their region. The characteristics of these subgroups are presented in Table 1. There were no effects of age (p = 0.67), sex (p = 0.14), or BMI (p = 0.97) on the change in PA levels. Those who lived alone experienced sharper declines in PA relative to those with other people in the home (−207 vs. −90, respectively; diff = 118 MET min/wk, p < 0.01). This was equivalent to a difference of 27 absolute minutes/week (p < 0.01). However, there was no effect of dependents in the home (p = 0.26).
Figure 1.
Variability in the change in PA levels from prior to COVID-19. The mean change in PA is represented by the dotted line for A) MET minutes/week = −112 ± 1460 and B) minutes/week = −18 ± 306. While 1,967 participants reporting a decline in PA levels, 2,409 reported no change or an increase in PA levels. Data are presented for those within ± 3 SD from the mean. Abbreviations: MET, metabolic equivalent of task.
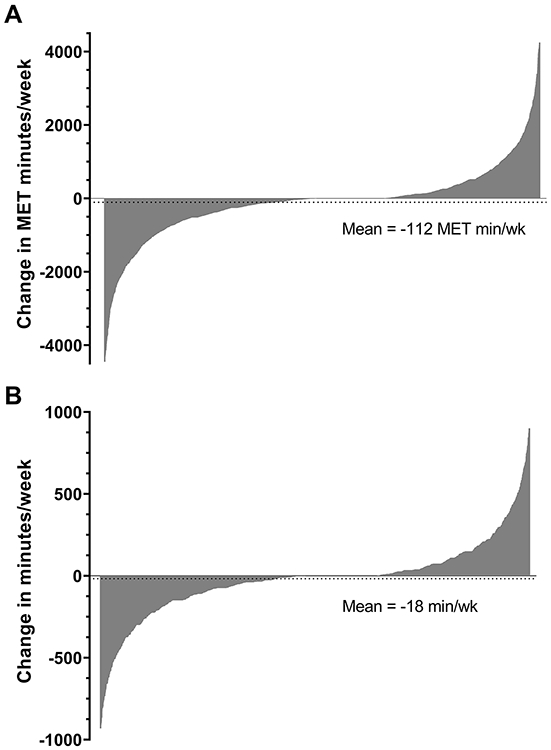
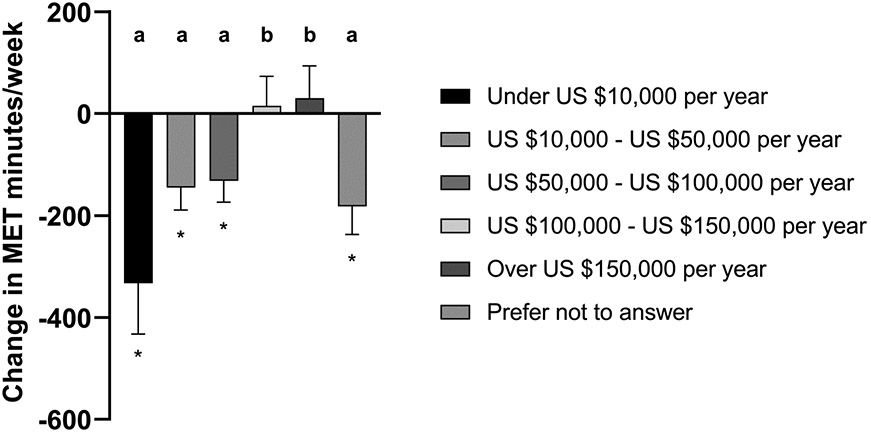
Analyses revealed a dose-response relationship between income and change in PA levels (Figure 2), such that those with the lowest income experienced the greatest declines, while those with the highest income had an increase in PA (−333 vs. 30, respectively; diff = 363 MET min/wk, p < 0.01). This was equivalent to a difference of 82 absolute minutes/week (p < 0.01). Those who experienced a change in income due to COVID-19 showed a greater decline in PA levels compared to those who did not (−182 vs. −73, respectively; diff = 110 MET min/wk, p < 0.01). This was equivalent to a difference of 24 absolute minutes/week (p < 0.01). Similarly, those who reported having been laid off or furloughed from their jobs experienced a greater decline in PA levels relative to those who had not (−232 vs. −64, respectively; diff = 168 MET min/wk, p < 0.01). This was equivalent to a difference of 36 absolute minutes/week (p < 0.01). Those who transitioned to working from home saw an increase in PA, while all others (not working from home, already working from home before COVID, not working before COVID) experienced a decline (Figure 3). Results were similar for MET minutes and absolute minutes per week.
Figure 2.
Effect of income on change in PA levels (MET minutes/week). * Denotes a significant within-group change from prior to COVID-19, while letters (a-d) denote significant between-group differences, p < 0.05 (letters that differ from each other indicate group differences). Abbreviations: MET, metabolic equivalent of task.
Figure 3.
Effect of the change or stability in work environment on change in PA levels (MET minutes/week). * Denotes a significant within-group change from prior to COVID-19, while letters (a-d) denote significant between-group differences, p < 0.05 (letters that differ from each other indicate group differences). Abbreviations: MET, metabolic equivalent of task.
Physical activity-specific factors
There was a negative association between baseline PA and change in PA levels, such that those with the highest levels of PA at baseline experienced the greatest declines (p < 0.01 for MET minutes and absolute minutes, Figure 4). Given that BMI was negatively associated with baseline PA levels (p < 0.01), we conducted this analysis with BMI as a covariate. Models remained significant with the inclusion of BMI (all p < 0.01). There was no effect of having a fitness tracker vs. not on changes in PA levels (p = 0.41).
Figure 4.
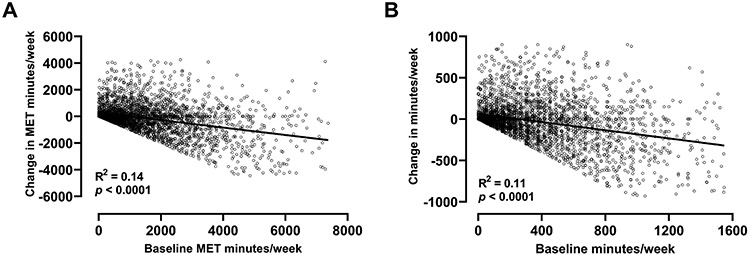
Associations between baseline PA levels and change in PA levels, as measured in A) MET minutes/week, and B) absolute minutes/week. Data are presented for those within ± 3 SD from the mean for each contributing variable. Abbreviations: MET, metabolic equivalent of task.
Those who previously had an active gym membership had a significantly greater decline in PA relative to those who did not (−330 vs. −12, respectively; diff = 317 MET min/wk, p < 0.01). This was equivalent to a difference of 61 absolute minutes/week (p < 0.01). Those who purchased home exercise equipment reported an increase in PA levels, while those who did not, had a decline in PA (32 vs. −138, respectively; diff = 170 MET min/wk, p < 0.01). This was equivalent to a difference of 39 absolute minutes/week (p < 0.01). Those who increased their use of virtual fitness platforms (exergaming, exercise videos) showed an increase in total PA levels compared to those who did not (430 vs. −193, respectively; diff = 663 MET min/wk, p < 0.01). This was equivalent to a difference of 156 absolute minutes/week (p < 0.01).
Replacement behaviors
There were significant differences between those who engaged in replacement behaviors (i.e., purchasing home equipment, using virtual fitness platforms in place of previous gym membership) and those who did not, regarding the changes in MET minutes/week and absolute minutes/week (Figure 5; main effects, all p < 0.01). These changes in physical activity were independent of BMI (all p > 0.17). However, the majority of survey respondents did not purchase equipment (n=3,702, 85%) and did not increase their use of virtual fitness platforms (n=3,808, 87%), regardless of whether they had a gym membership prior to the pandemic.
Figure 5.
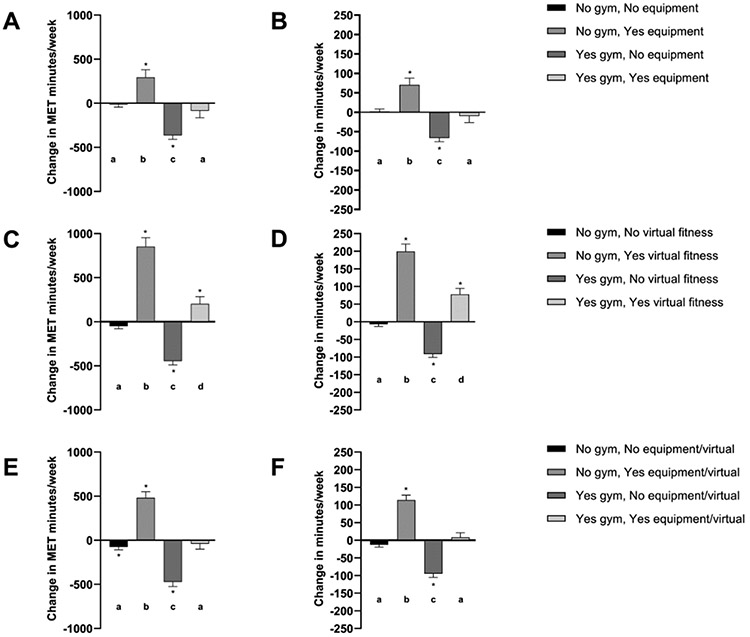
Effects of replacement behaviors on changes in PA levels. Each graph depicts whether participants had an active gym membership prior to COVID-19 (No gym vs. Yes gym) and whether or not they purchased home-based exercise equipment (No equipment vs. Yes equipment) and/or increased use of virtual fitness platforms (No virtual fitness vs. Yes virtual fitness). A) Change in MET minutes/week by gym and equipment; B) Change in absolute minutes/week by gym and equipment; C) Change in MET minutes/week by gym and virtual fitness; D) Change in absolute minutes/week by gym and virtual fitness; E) Change in MET minutes/week by gym and equipment and/or virtual fitness; F) Change in absolute minutes/week by gym and equipment and/or virtual fitness. * Denotes a significant within-group change from prior to COVID-19, while letters (a-d) denote significant between-group differences, p < 0.05 (letters that differ from each other indicate group differences). Abbreviations: MET, metabolic equivalent of task.
Only 347 participants (7.9%) reported purchasing home exercise equipment in place of an active gym membership during the shutdown, while an additional 327 (7.5%) purchased equipment despite no previous use of a gym membership (Figures 5A and B). Among those with a previous gym membership, those who purchased equipment had an attenuated decline in MET minutes/week relative to those who did not purchase equipment (−80 vs. −361, respectively; diff = 281 MET min/wk, p < 0.01). This was equivalent to a difference of 57 absolute minutes/week (−8 vs. −65 min/wk, respectively; p < 0.01). Those who did not have a gym membership but purchased home equipment reported an increase of 294 MET minutes/week from prior to COVID-19 (p < 0.01), or 70 absolute minutes/week (p < 0.01).
Regarding virtual fitness platforms, 337 participants (7.7%) reported an increase in their use of online exercise videos or exergaming in place of an active gym membership during the shutdown, while an additional 231 (5.3%) increased use of virtual fitness platforms despite no previous use of a gym membership (Figures 5C and D). Among those with a previous gym membership, those who increased use of virtual fitness platforms reported an increase in MET minutes/week, while those who did not, experienced a decline (206 vs. −445, respectively; diff = 650 MET min/wk, p < 0.01). This was equivalent to a difference of 170 absolute minutes/week (79 vs. −91 min/wk, respectively; p < 0.01). Those who did not have a gym membership, but increased use of virtual fitness platforms reported an increase of 853 MET minutes/week from prior to COVID-19 (p < 0.01), or 199 absolute minutes/week (p < 0.01).
In total, 589 participants (13.5%) who previously had an active gym membership reported either purchasing equipment and/or using virtual fitness platforms, suggesting some overlap of replacement approaches (Figures 5E and F). Participants who previously had a gym membership and did not purchase equipment nor increase use of virtual fitness platforms (n = 845, 19.3%) reported the sharpest declines in PA (−472 MET min/wk or −94 min/wk; both p < 0.01).
DISCUSSION
The purpose of this secondary analysis was to identify individual-level factors and strategies that helped adults maintain PA levels during the COVID-19 pandemic and associated shutdowns. This analysis was in response to the recent ACSM Call to Action Statement on COVID-19 and PA (15). We hypothesized that those with the highest levels of PA prior to COVID-19 would report the sharpest declines, and that self-monitoring of PA, purchasing home-based exercise equipment, and accessing virtual fitness platforms would protect against this decline. Our hypotheses were largely supported, with the exception of self-monitoring with wearable fitness trackers, which was not associated with the change in PA levels in our study. Despite significant declines in PA overall, purchasing home exercise equipment and increasing use of virtual fitness platforms, such as online exercise videos and exergaming, did mitigate the reduction in PA. However, we also saw significant effects of income, work, and home-related factors on PA levels that must be accounted for when developing strategies to keep people active.
Based on known barriers to and facilitators of physical activity, we anticipated unique challenges associated with the COVID-19 pandemic. Adults may have increased demands on their time, with competing work and family responsibilities during the pandemic. Increased stress and strain on mental health may contribute to reduced motivation or energy for PA (25). With the closures of gyms and community centers, access to safe facilities is at an all-time low, and the ability to purchase home-based exercise equipment is likely simultaneously limited by physical space to accommodate it and the financial strain experienced during the economic downturn. Factors that can help facilitate regular PA (in the absence of a pandemic) have been previously described, including access to PA opportunities that are affordable and convenient (19, 20). For this reason, access to home-based fitness options would be optimal during a shutdown (26, 27). With stay-at-home and shelter-in-place orders lifted, it is imperative to have the ability to safely walk or bike in one’s neighborhood (28). In addition, social support is an important facilitator of PA in many studies and is often included as a component of PA interventions (29, 30). Those with more individuals in the home during the shutdown may have an easier time maintaining PA levels, compared to those living in isolation. Online fitness platforms or virtual health coaching could help facilitate PA for those who lack social support in the home. Self-monitoring through wearable fitness trackers has been used as a strategy in previous PA interventions (30), and many devices come with access to a tracking app with social platforms. We explored as many of these factors as possible influences on the COVID-19 associated change in PA within the current analysis.
Despite relatively low uptake (13% of participants), access to virtual fitness platforms appeared to have a strong protective effect against declines in PA. Early adopters of virtual fitness approaches (i.e., exergaming or online exercise videos) reported an increase in overall PA levels relative to those who did not. As the pandemic continues, further promotion of virtual fitness opportunities could be an effective strategy to promote health. Our findings are in line with reports from Yang and colleagues that fitness apps were effective in helping people maintain physical activity levels, especially when using gamification (31). Importantly, this strategy requires access to specific technologies (gaming console, internet, smartphone, etc.), which should be taken into account when engaging adults in low-resource situations. Free or reduced-cost content that is still stimulating enough to promote engagement is encouraged, where possible. Similarly, we saw relatively low rates (15.4%) of purchasing home-based exercise equipment, likely due to the known financial burden and additional anecdotal evidence of low availability for consumers. Based on these combined results, low-cost, virtual exercise content that requires minimal to no equipment is likely to be an effective strategy (32).
This is particularly true for some of our highest risk participants – those with lower incomes or who experienced/are experiencing a loss of income due to changes in job status. The economic effects of the COVID-19 pandemic in the United States and elsewhere have been well documented (33, 34). Previous studies have shown that those with low incomes already face health disparities in regards to meeting guidelines for PA and healthy eating (35, 36). Many studies have now shown that the COVID-19 pandemic has had significant effects on both PA and eating behaviors (7, 16, 18, 37-39), and our results now suggest that the current situation is widening existing income-related disparities in health behavior. Simultaneously, these disparate individuals are also subject to more severe COVID-19 clinical outcomes (40, 41), highlighting the urgency with which health-promoting lifestyle behaviors need to be supported.
Based on the current analyses, another high-risk group in regards to PA declines are those living alone. Unfortunately, those living in isolation are also the most likely to suffer mental health declines during the pandemic-associated stay-at-home orders (42, 43). Given well-documented associations between PA and mental health (44-46), finding strategies to promote PA in this group is likely to have beneficial effects beyond physical health (47). We saw that self-monitoring alone (as determined by the use of wearable fitness trackers) was not effective in mitigating the reduction in PA levels seen overall. Therefore, we believe additional social support and accountability may be needed in this extreme situation.
The inherent limitations of self-reported surveys are well known. We used validated instruments wherever available, but needed to include additional investigator-created questions to capture the unique environment. The addition of a virtual fitness question to the Nurse’s Health Study Physical Activity Questionnaire is one such example. It is possible that certain vulnerable populations may be underrepresented in this survey, as participation was limited to those with access to the internet via WiFi or cellular service during the stay-at-home orders. Based on the timing of our survey, it was not possible to gather pre-pandemic responses in real time, and thus participants recalled and reported behaviors retrospectively. Based on our previous analysis, we saw that 96% of respondents were affected by government mandates to control the spread of the virus (16), and responses were captured not more than one month into the COVID-19 shutdown, in most cases. Importantly, many participants did report a significant change in their behaviors, suggesting that they did indeed recognize the effects of the pandemic on their lifestyle. There were likely regional differences due to weather which may have impacted physical activity as well as the ability to implement replacement behaviors to maintain physical activity. Based on the available data from the present survey, we were unable to assess the effects of weather or climate on changes in PA. With repeated surges in COVID-19 in various regions of the world, it will be important to evaluate seasonal influences on these behaviors and provide additional support, as needed. We had a broad distribution of income and weight status across the study sample. However, despite recruitment strategies to obtain a diverse set of respondents, the majority of survey respondents identified as white, female, older adults from similar geographic regions, which may limit the generalizability of some of our findings. Our primary source of advertisement was through Facebook, where the majority of users are women. Additionally, multiple reports have shown that women have been disproportionally burdened with care-related tasks (e.g., childcare, home schooling, caring for elderly) throughout the pandemic (48, 49) which would likely influence changes to physical activity. Future studies during this pandemic should examine the acceptability of virtual fitness options, for example, among men and individuals from other racial or ethnic backgrounds.
In sum, individuals are experiencing significant barriers to participating in regular PA, beyond the usual circumstances. Attenuating the reduction in PA should be a public health priority now and in response to future pandemic mitigation measures. Few adults (24%) meet the recommended guidelines for PA (50), and further declines will exacerbate the known health consequences of low PA and associated low cardiorespiratory fitness (11-14). Therefore, combating the decline in PA is likely to have an impact on physical health over the long term. Understanding individual-level factors that affect PA during the pandemic is the first step to addressing the problem. Now we, as health practitioners and researchers, must consider these contextual factors in our responsive action.
Acknowledgments
This work was partially supported by a NORC Center Grant # P30DK072476 entitled “Nutrition and Metabolic Health Through the Lifespan” sponsored by NIDDK. In addition, this work was supported in part by U54 GM104940 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center. C.H. is supported by an NIH NIDDK National Research Service Award (T32DK064584). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest
None of the authors declare a conflict of interest. The results of the present study do not constitute endorsement by ACSM. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
REFERENCES
- 1.World Health Organization. Transmission of SARS-CoV-2: implications for infection prevention precautions 2020. [cited 2020 9 July]. Available from: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions.
- 2.Coronavirus Resource Center JHUaM. COVID-19 Dashboard by the CSSE at JHU 2020. [cited 2020 18 November]. Available from: https://coronavirus.jhu.edu/map.html.
- 3.World Health Organization. Coronavirus disease (COVID-19) advice for the public 2020. [cited 2020]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- 4.<w>Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19) - Social Distancing 2020. [cited 2020]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html.
- 5.Centers for Disease Control and Prevention. Timing of State and Territorial COVID-19 Stay-at-Home Orders and Changes in Population Movement — United States, March 1–May 31, 2020 2020. [cited 2020 4 September]. Available from: https://www.cdc.gov/mmwr/volumes/69/wr/mm6935a2.htm#F1_down. [DOI] [PMC free article] [PubMed]
- 6.Kaiser Family Foundation. When State Stay-at-Home Orders Due to Coronavirus Went into Effect 2020. [cited 2020]. Available from: https://www.kff.org/other/slide/when-state-stay-at-home-orders-due-to-coronavirus-went-into-effect/.
- 7.Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity. 2020;28(8):1382–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fitbit. The Impact of Coronavirus on Global Activity 2020. [cited 2020 23 March]. Available from: https://blog.fitbit.com/covid-19-global-activity/.
- 9.Di Sebastiano KM, Chulak-Bozzer T, Vanderloo LM, Faulkner G. Don't Walk So Close to Me: Physical Distancing and Adult Physical Activity in Canada. Frontiers in psychology. 2020;11:1895. Epub 2020/08/28. doi: 10.3389/fpsyg.2020.01895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Progress in cardiovascular diseases. 2020. Epub 2020/04/12. doi: 10.1016/j.pcad.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mok A, Khaw KT, Luben R, Wareham N, Brage S. Physical activity trajectories and mortality: population based cohort study. Bmj. 2019;365:l2323. Epub 2019/06/28. doi: 10.1136/bmj.l2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: emerging evidence for a new health risk. Mayo Clinic proceedings. 2010;85(12):1138–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. European heart journal. 2011;32(5):590–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lavie CJ, Carbone S, Kachur S, O'Keefe EL, Elagizi A. Effects of Physical Activity, Exercise, and Fitness on Obesity-Related Morbidity and Mortality. Current sports medicine reports. 2019;18(8):292–8. [DOI] [PubMed] [Google Scholar]
- 15.Denay KL, Breslow RG, Turner MN, Nieman DC, Roberts WO, Best TM. ACSM Call to Action Statement: COVID-19 Considerations for Sports and Physical Activity. Current sports medicine reports. 2020;19(8):326–8. Epub 2020/08/10. [DOI] [PubMed] [Google Scholar]
- 16.Flanagan EW, Beyl RA, Fearnbach SN, Altazan AD, Martin CK, Redman LM. The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity. 2020. Epub 2020/10/13. doi: 10.1002/oby.23066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castaneda-Babarro A, Arbillaga-Etxarri A, Gutierrez-Santamaria B, Coca A. Physical Activity Change during COVID-19 Confinement. International journal of environmental research and public health. 2020;17(18). Epub 2020/09/25. doi: 10.3390/ijerph17186878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knell G, Robertson MC, Dooley EE, Burford K, Mendez KS. Health Behavior Changes During COVID-19 Pandemic and Subsequent "Stay-at-Home" Orders. International journal of environmental research and public health. 2020;17(17). Epub 2020/09/03. doi: 10.3390/ijerph17176268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Overcoming Barriers to Physical Activity 2020. [cited 2020 17 September]. Available from: https://www.cdc.gov/physicalactivity/basics/adding-pa/barriers.html.
- 20.Bethancourt HJ, Rosenberg DE, Beatty T, Arterburn DE. Barriers to and facilitators of physical activity program use among older adults. Clinical medicine & research. 2014;12(1-2):10–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.International R. PhenX Toolkit - COVID-19 Protocols 2020. [cited 2020 17 September]. Available from: https://www.phenxtoolkit.org/covid19.
- 23.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. International journal of epidemiology. 1994;23(5):991–9. [DOI] [PubMed] [Google Scholar]
- 24.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Medicine and science in sports and exercise. 2011;43(8):1575–81. [DOI] [PubMed] [Google Scholar]
- 25.Meyer J, McDowell C, Lansing J, et al. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 US Adults. International journal of environmental research and public health. 2020;17(18). Epub 2020/09/10. doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quinn L, Macpherson C, Long K, Shah H. Promoting Physical Activity via Telehealth in People With Parkinson Disease: The Path Forward After the COVID-19 Pandemic? Physical therapy. 2020;100(10):1730–6. Epub 2020/08/01. doi: 10.1093/ptj/pzaa128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lucini D, Gandolfi CE, Antonucci C, et al. #StayHomeStayFit: UNIMI's approach to online healthy lifestyle promotion during the COVID-19 pandemic. Acta Biomed. 2020;91(3):e2020037. Epub 2020/09/15. doi: 10.23750/abm.v91i3.10375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bentlage E, Ammar A, How D, et al. Practical Recommendations for Maintaining Active Lifestyle during the COVID-19 Pandemic: A Systematic Literature Review. International journal of environmental research and public health. 2020;17(17). Epub 2020/09/03. doi: 10.3390/ijerph17176265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stragier J, Mechant P, De Marez L, Cardon G. Computer-Mediated Social Support for Physical Activity: A Content Analysis. Health education & behavior : the official publication of the Society for Public Health Education. 2018;45(1):124–31. [DOI] [PubMed] [Google Scholar]
- 30.Heath GW, Parra DC, Sarmiento OL, et al. Evidence-based intervention in physical activity: lessons from around the world. Lancet. 2012;380(9838):272–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang Y, Koenigstorfer J. Determinants of physical activity maintenance during the Covid-19 pandemic: a focus on fitness apps. Translational behavioral medicine. 2020. Epub 2020/09/15. doi: 10.1093/tbm/ibaa086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schwendinger F, Pocecco E. Counteracting Physical Inactivity during the COVID-19 Pandemic: Evidence-Based Recommendations for Home-Based Exercise. International journal of environmental research and public health. 2020;17(11). Epub 2020/06/05. doi: 10.3390/ijerph17113909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Couch KA, Fairlie RW, Xu H. Early Evidence of the Impacts of COVID-19 on Minority Unemployment. J Public Econ. 2020:104287. Epub 2020/09/22. doi: 10.1016/j.jpubeco.2020.104287. PubMed PMID: 32952224; PubMed Central PMCID: PMCPMC7489888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raifman J, Bor J, Venkataramani A. Unemployment insurance and food insecurity among people who lost employment in the wake of COVID-19. medRxiv. 2020. Epub 2020/08/09. doi: 10.1101/2020.07.28.20163618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Siahpush M, Robbins RE, Ramos AK, Michaud TL, Clarke MA, King KM. Does Difference in Physical Activity Between Blacks and Whites Vary by Sex, Income, Education, and Region of Residence? Results from 2008 to 2017 National Health Interview Surveys. J Racial Ethn Health Disparities. 2019;6(5):883–91. [DOI] [PubMed] [Google Scholar]
- 36.Armstrong S, Wong CA, Perrin E, Page S, Sibley L, Skinner A. Association of Physical Activity With Income, Race/Ethnicity, and Sex Among Adolescents and Young Adults in the United States: Findings From the National Health and Nutrition Examination Survey, 2007-2016. JAMA pediatrics. 2018;172(8):732–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cancello R, Soranna D, Zambra G, Zambon A, Invitti C. Determinants of the Lifestyle Changes during COVID-19 Pandemic in the Residents of Northern Italy. International journal of environmental research and public health. 2020;17(17). Epub 2020/09/03. doi: 10.3390/ijerph17176287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mattioli AV, Sciomer S, Cocchi C, Maffei S, Gallina S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutrition, metabolism, and cardiovascular diseases : NMCD. 2020;30(9):1409–17. Epub 2020/06/24. doi: 10.1016/j.numecd.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martinez-Ferran M, de la Guia-Galipienso F, Sanchis-Gomar F, Pareja-Galeano H. Metabolic Impacts of Confinement during the COVID-19 Pandemic Due to Modified Diet and Physical Activity Habits. Nutrients. 2020;12(6). Epub 2020/05/30. doi: 10.3390/nu12061549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Muñoz-Price LS, Nattinger AB, Rivera F, et al. Racial Disparities in Incidence and Outcomes Among Patients With COVID-19. JAMA Netw Open. 2020;3(9):e2021892. Epub 2020/09/26. doi: 10.1001/jamanetworkopen.2020.21892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maroko AR, Nash D, Pavilonis BT. COVID-19 and Inequity: a Comparative Spatial Analysis of New York City and Chicago Hot Spots. Journal of urban health : bulletin of the New York Academy of Medicine. 2020;97(4):461–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sfendla A, Hadrya F. Factors Associated with Psychological Distress and Physical Activity During the COVID-19 Pandemic. Health Secur. 2020. Epub 2020/09/19. doi: 10.1089/hs.2020.0062. [DOI] [PubMed] [Google Scholar]
- 43.Matias T, Dominski FH, Marks DF. Human needs in COVID-19 isolation. Journal of health psychology. 2020;25(7):871–82. [DOI] [PubMed] [Google Scholar]
- 44.Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005;18(2):189–93. [DOI] [PubMed] [Google Scholar]
- 45.Mason OJ, Holt R. Mental health and physical activity interventions: a review of the qualitative literature. J Ment Health. 2012;21(3):274–84. [DOI] [PubMed] [Google Scholar]
- 46.Pascoe M, Bailey AP, Craike M, et al. Physical activity and exercise in youth mental health promotion: a scoping review. BMJ Open Sport Exerc Med. 2020;6(1):e000677. Epub 2020/02/26. doi: 10.1136/bmjsem-2019-000677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Callow DD, Arnold-Nedimala NA, Jordan LS, et al. The Mental Health Benefits of Physical Activity in Older Adults Survive the COVID-19 Pandemic. Am J Geriatr Psychiatry. 2020;28(10):1046–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.UN Women UN. Whose time to care: Unpaid care and domestic work during COVID-19 2020. [cited 2020 November 25]. Available from: https://data.unwomen.org/publications/whose-time-care-unpaid-care-and-domestic-work-during-covid-19.
- 49.Del Boca D, Oggero N, Profeta P, Rossi M. Women's and men's work, housework and childcare, before and during COVID-19. Rev Econ Househ. 2020:1–17. Epub 2020/09/15. doi: 10.1007/s11150-020-09502-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Centers for Disease Control and Prevention. Trends in meeting the 2008 Physical Activity Guidelines, 2008-2018 2018. [cited 2020]. Available from: https://www.cdc.gov/physicalactivity/downloads/trends-in-the-prevalence-of-physical-activity-508.pdf.