A 44-year-old man with chronic heart failure due to ischemic heart disease on continuous inotropic support was transferred to our institution for consideration of heart transplantation (HT). His past medical history was notable for a large anterior ST-segment–elevation myocardial infarction complicated by a left ventricular thrombus and recent implantable cardioverter-defibrillator shocks for polymorphic ventricular tachycardia. Right heart catheterization performed on milrinone 0.375 μg/kg per minute demonstrated cardiogenic shock with elevated biventricular filling pressures and pulmonary hypertension: right atrial pressure 17 mm Hg, pulmonary artery pressure 60/42 mm Hg with mean 48 mm Hg, pulmonary capillary wedge pressure 30 mm Hg, pulmonary artery saturation 33.0%, and Fick cardiac index 1.3 liters per minute per meter squared. Expedited HT evaluation was initiated, and he was listed as an acceptable candidate. Despite medical optimization, pharmacological support with dual inotropes, and temporary mechanical support with an intraaortic balloon pump at 1:1 augmentation, he remained in cardiogenic shock and was transitioned to full hemodynamic support with peripheral venoarterial extracorporeal membrane oxygenation. Two days later, he underwent successful HT but required temporary peripheral venoarterial extracorporeal membrane oxygenation support and underwent delayed chest closure for postoperative allograft dysfunction. Caspofungin was used for open chest antifungal prophylaxis. He experienced early asymptomatic acute cellular rejection (International Society for Heart and Lung Transplantation grade, 2R) and was treated with intravenous pulse methylprednisolone for 3 days. He was discharged home in good condition one month later on tacrolimus, mycophenolate mofetil, and prednisone.
Five months later, he presented with fevers and chest, back, and right shoulder pain. Urgent chest computed tomography angiography demonstrated a new saccular pseudoaneurysm (8.4 × 7.8 cm) of the aortic suture line with evidence of mass effect and rupture (Figure 1). He underwent emergent redo median sternotomy with aortic root replacement and ascending aorta and hemiarch graft. Pathological tissue examination revealed abscesses and numerous fungal hyphae, and fungal culture from the aortic suture line site grew Aspergillus fumigatus (Figure 2). He was treated with voriconazole. On postoperative day 4, he underwent successful transdiaphragmatic pedicled omental flap to achieve vascularized soft tissue reconstruction surrounding his aortic graft. He was discharged on postoperative day 14 on tacrolimus, prednisone, and voriconazole, and off mycophenolate mofetil.
FIGURE 1. Selected images from initial chest computed tomography with arterial phase contrast enhancement.
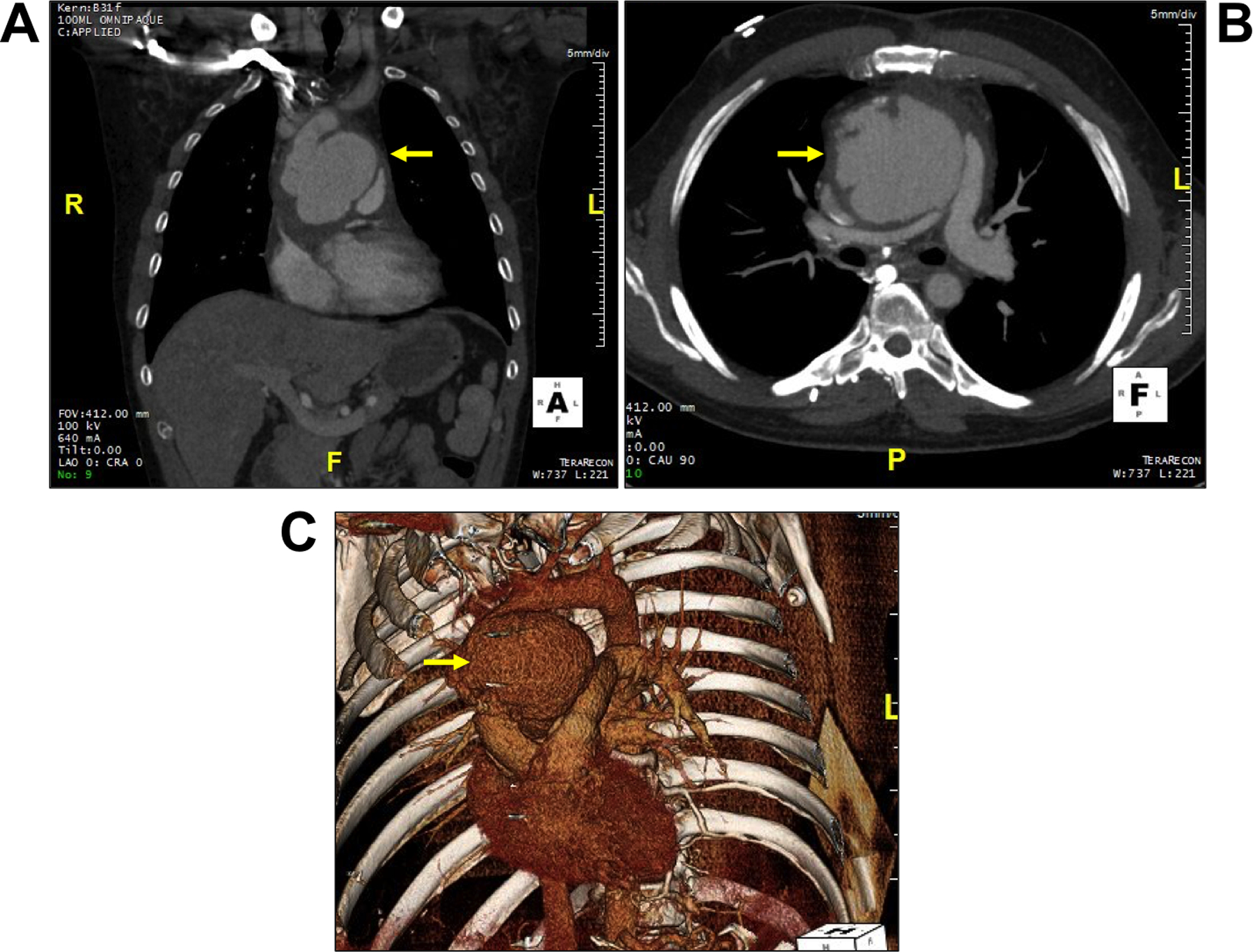
Coronal (A) and axial slices (B) reveal a large pseudoaneurysm of the ascending aorta (8.4 × 7.8 cm) with multilobulated contour and mural irregularity of the mid-ascending aorta. 3D volume rendered image (C) shows the pseudoaneurysm (arrow) involving the ascending aorta.
FIGURE 2. Pathology from aortic tissue excision demonstrating Aspergillus fumigatus.
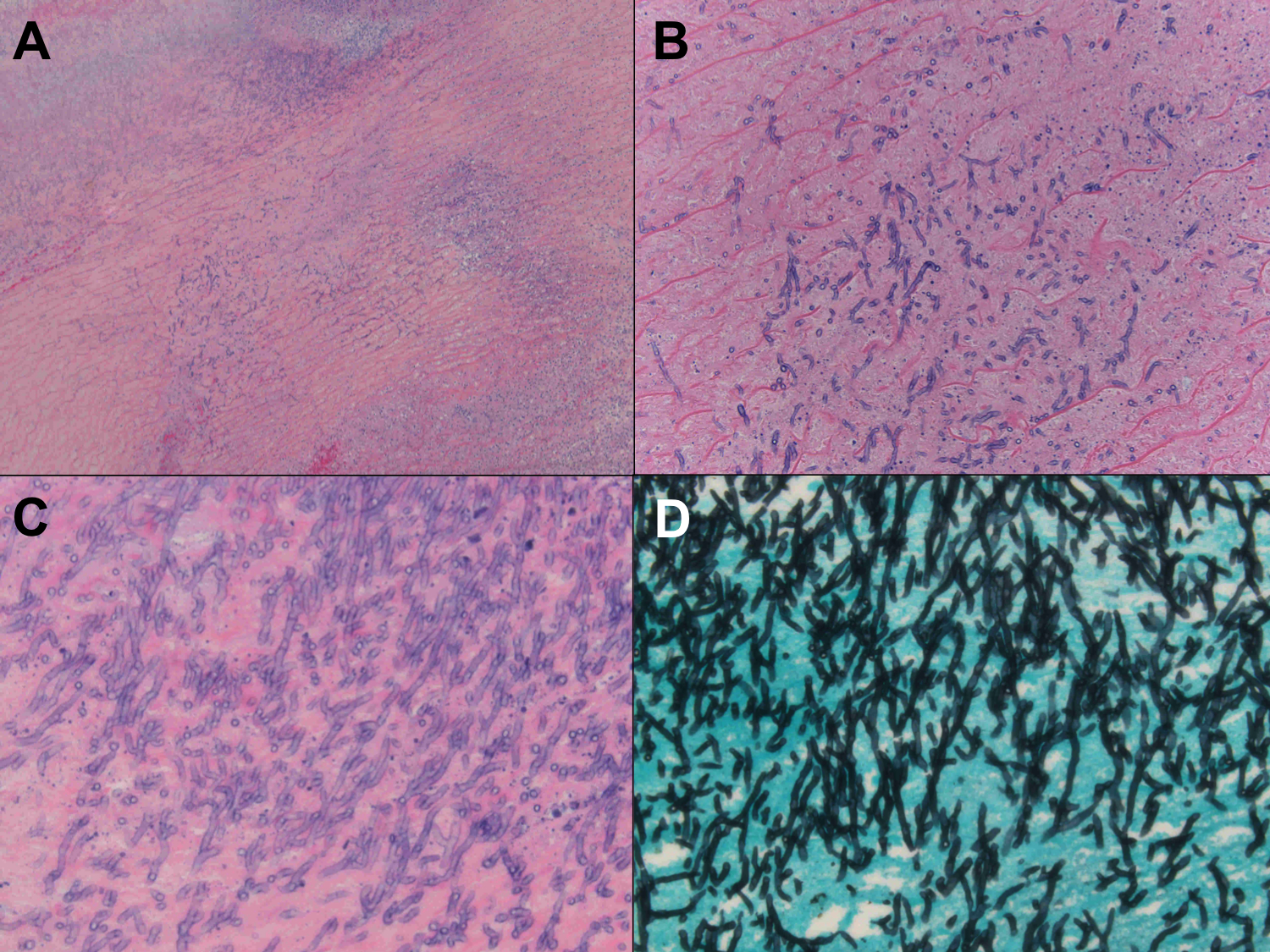
(A) Hematoxylin and eosin (H&E) image (5x) demonstrates mostly necrotic vessel wall. (B) H&E image (20x) reveals nonviable vessel wall with fungal hyphae. (C) Fungal hyphae with acute angle branching shown on H&E (40x) image. (D) Grocott special stain (40x) highlights numerous fungal hyphae with acute angle branching.
One month later, he underwent surveillance chest computed tomography angiography that revealed a new filling defect appearing to extend into the left atrium (Figure 3, Supplemental Video I). Expedited transesophageal echocardiography demonstrated a large echogenic mass, posterior to the ascending aorta graft, invading the anterior left atrial wall with a large, irregular mobile component (2.6 cm × 1.0 cm) protruding into the left atrial cavity (Figure 4, Supplemental Videos II and III), highly concerning for ongoing invasive Aspergillosis (IA). Amphotericin B and anticoagulation were initiated for additional fungal coverage and empirical management of potential left atrial thrombus, respectively. Surgical management was considered, however, he developed an acute intracranial hemorrhage resulting in prohibitive surgical risk.
FIGURE 3. Selected images from follow-up contrast enhanced chest computed tomography.
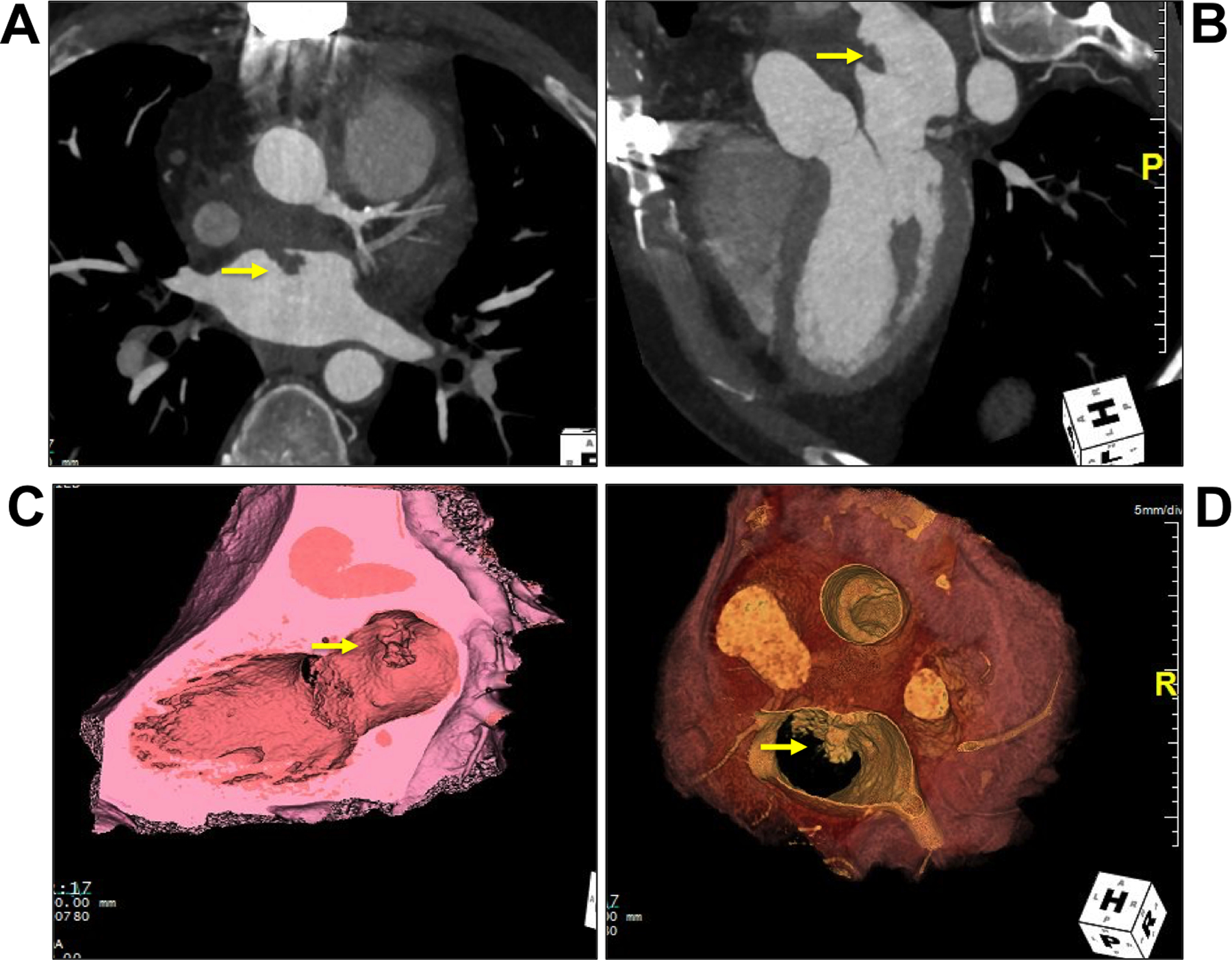
Axial image (A), coronal oblique image (B), and long axis (C) and short axis (D) 3D endoluminal reconstruction demonstrates a large mass posterior to the ascending aorta graft that protrudes into the left atrium (arrow).
FIGURE 4. Selected images from transesophageal echocardiography.
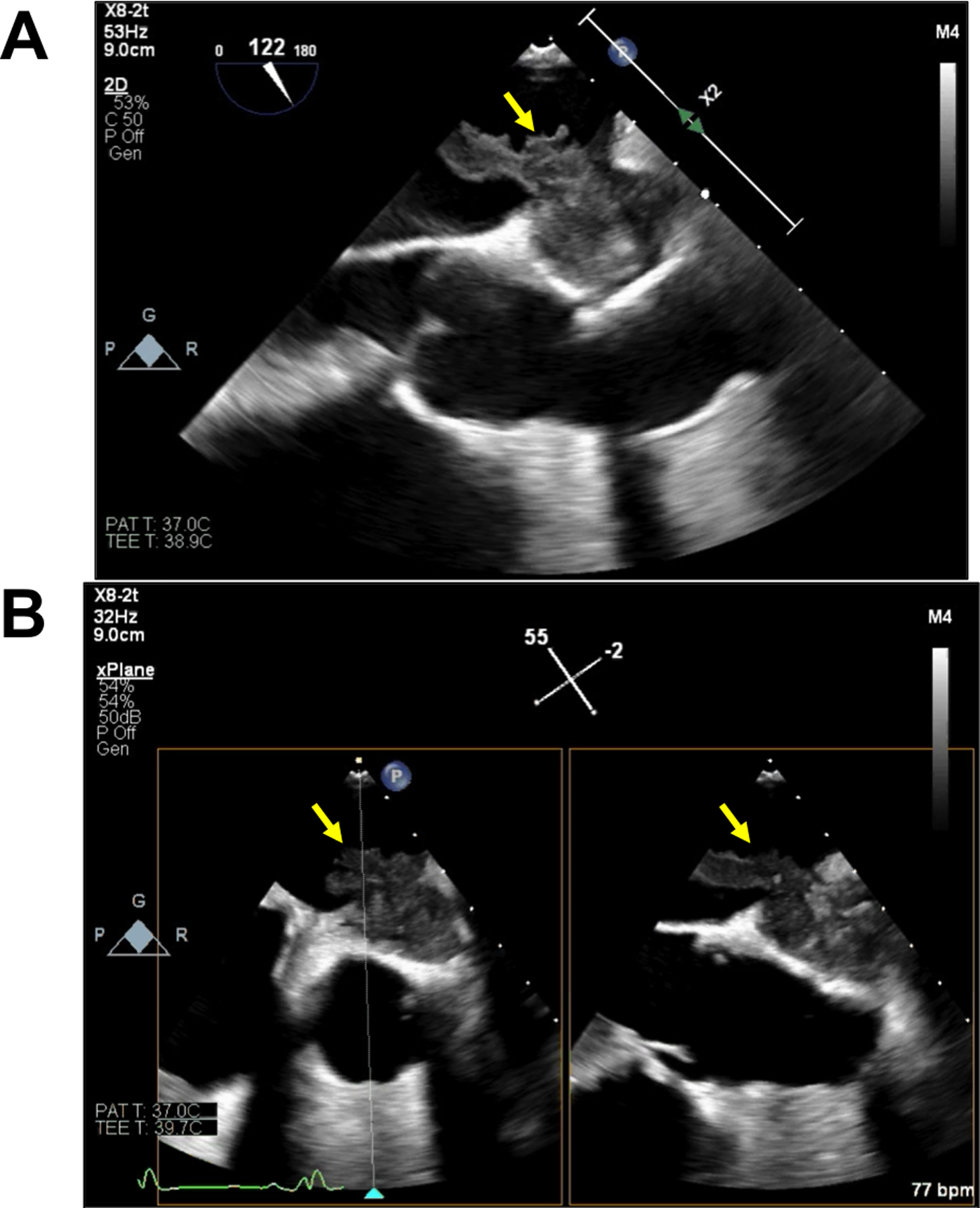
Mid-esophageal ascending aorta long axis view (A) and x-plane view (B) reveal a large echogenic mass posterior to the ascending aorta graft invading the anterior left atrial wall with a large, irregular mobile component (2.6 cm × 1.0 cm) extending into the left atrial cavity.
Data regarding the incidence and prevalence of invasive fungal infections (IFI) after heart transplantation are limited. A prospective multicenter United States study of IFI in solid organ transplant patients identified a 3.4% cumulative incidence of IFI during the first year after HT with Aspergillus species accounting for 23% of IFI.1 Among all solid organ transplant cases in this series, Aspergillus fumigatus was the most common species isolated, and 78% of aspergillosis cases led to pulmonary infection only. In a single-center Spanish series of 479 consecutive HT recipients, only 2 of 31 patients who developed IA had extrapulmonary involvement and only one of these involved the mediastinum2. In our case, chest computed tomography at the time of initial diagnosis did not demonstrate radiographic evidence of pulmonary aspergillosis.
Risk factors for IFI after HT have not been well studied. Limited multicenter data suggest that reoperation, cytomegalovirus disease, post-HT hemodialysis, and an episode of IA in the same HT unit in a 3-month pre-HT or post-HT period are risk factors for IA; our patient had none of these risk factors. Additional single-center studies have identified the use of post-HT ECMO as a risk factor for fungal infection and post-HT acute cellular rejection as a risk factor for IA, both of which our patient experienced. Individual centers have instituted fungal prophylaxis protocols for at-risk patients; however, this practice is not uniform across HT centers.
Only 4 cases of Aspergillus fumigatus mediastinitis after HT have been previously reported. Of these cases, one HT recipient3, like ours, was found to have a ruptured pseudoaneurysm of the ascending aorta with hyphae in the aortic wall, our patient did not report preceding signs or symptoms of mediastinitis.
To our knowledge, we herein describe the first case of IA causing aortic pseudoaneurysm with concomitant intracardiac fungal invasion in an HT recipient. Multimodality cardiovascular imaging proved to be critical for diagnosis and therapeutic surgical management.
Supplementary Material
ACKNOWLEDGMENTS
SOURCES OF FUNDING
Dr Reza is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number KL2TR001879. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Owens is supported by the Winkelman Family Fund for Innovation.
Footnotes
DISCLOSURES
All authors report no disclosures.
SUPPLEMENTAL MATERIALS
Supplemental Videos I-III
REFERENCES
- 1.Pappas PG, Alexander BD, Andes DR, Hadley S, Kauffman CA, Freifeld A, Anaissie EJ, Brumble LM, Herwaldt L, Ito J, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin Infect Dis. 2010;50(8):1101–1111. [DOI] [PubMed] [Google Scholar]
- 2.Muñoz P, Cerón I, Valerio M, Palomo J, Villa A, Eworo A, Fernández-Yáñez J, Guinea J, Bouza E. Invasive aspergillosis among heart transplant recipients: a 24-year perspective. J Heart Lung Transplant. 2014;33:278–288. [DOI] [PubMed] [Google Scholar]
- 3.Byl B, Jacobs F, Antoine M, Depierreux M, Serruys E, Primo G, Thys JP. Mediastinitis caused by Aspergillus fumigatus with ruptured aortic pseudoaneurysm in a heart transplant recipient: case study. Heart Lung. 1993;22(2):145–147. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


