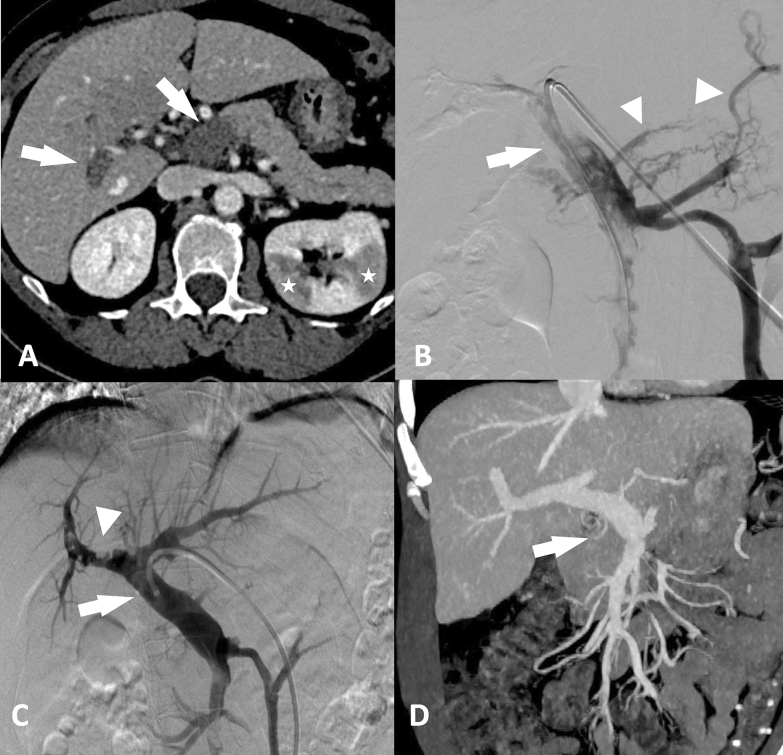
A 57-year-old woman developed portomesenteric vaccine-associated immune thrombosis and thrombocytopenia (VITT) 12 days after a second administration of AstraZeneca (AZ) (ChAdOx1 nCov-19, UK) COVID-19 vaccine. Abdominal computed tomography (CT) demonstrated the absence of contrast filling of the portal trunk and portal branches and bilateral kidney corticomedullary triangular hypodensity corresponding to a complete thrombosis of the portal trunk and branches with bilateral segmental kidney infarcts (Fig. 1A).
Fig. 1.
A 57-year-old woman developed portomesenteric vaccine-associate immune thrombosis and thrombocytopenia after a second administration of AstraZeneca COVID-19 vaccine. A Abdominal CT shows complete thrombosis of the portal trunk and the right portal branch (arrow), and left kidney infarcts (white stars). B Digital subtraction portography shows occlusion of the portal vein and branches, and the occlusion of the superior mesenteric vein (arrow). Obstruction of the portomesenteric veins result in the development of gastric and splenic collaterals (arrowheads). C Digital subtraction portography after mechanical thromboaspiration and 12 h fibrinolysis shows complete desobstruction of the portal trunk, the left portal branch and mesenteric vein (arrows) and marginated residual thrombus in the right portal branch (arrowhead). This desobstruction results in the disappearance of the venous collaterals. D Coronal reformatted abdominal CT in maximum intensity projection shows complete recanalization of the portomesenteric veins 7 days after treatment
Anticoagulation and corticosteroids were introduced. Transhepatic portography showed complete portal thrombosis and superior mesenteric vein with development of peri-gastric venous collaterals (Fig. 1B). Thromboaspiration followed by 12 h-intra-portal fibrinolysis resulted in a desobstruction of the portomesenteric veins with a right portal branch-marginated residual thrombus, and disappearance of the venous collaterals (Fig. 1C). A week after, abdominal CT found a complete portomesenteric veins recanalization (Fig. 1D).
Very rare cases of VITT have been reported shortly after the administration of the AZ vaccine with sometimes fatal outcome rising concerns about the administration of such vaccine. Extensive portomesenteric vein thrombosis may require aggressive and escalating interventions. Early thromboaspiration with fibrinolysis appears safe and efficient and may be considered as an option to treat portomesenteric VITT.
Declarations
Conflicts of interest
Authors do not report any conflict of interest nor any financial interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.