Abstract
Purpose:
To report a case of a culture-negative deep fungal corneal infection that was diagnosed after histopathology of an anterior segment OCT-guided endothelial biopsy.
Methods:
A 22-year-old woman with history of contact lens wear and concomitant topical steroid use presented with a mid-stromal corneal infiltrate that failed to respond to oral acyclovir and topical fortified antibiotics. Although cornea stains, cultures and confocal microscopy were negative, there was high clinical suspicion for fungal keratitis. After 2 months on topical natamycin, oral voriconazole, and serial intrastromal and intracameral voriconazole injections, the infiltrate enlarged and deepened. Imaging with anterior segment OCT revealed that the infection had progressed to an endothelial plaque.
Results:
Diagnostic endothelial biopsy was performed in the operating room. Cultures were again negative, while histopathology of the removed specimen revealed fungal elements. The postoperative edema at the site of the biopsy resolved over the course of four weeks and a posterior stromal scar formed. Serial intrastromal and intracameral voriconazole injections were continued for the first post-operative month. At the 1-year and the 3-year follow up examinations the patient’s vision was 20/20 without recurrence.
Conclusions:
Intraoperative scraping of the endothelial plaque and histopathologic evaluation of the specimen proved to be of utmost importance for definitive diagnosis and resolution of the culture-negative deep fungal infection in this case. This young patient’s cornea was retained and vision remains excellent.
Keywords: Fungal corneal ulcer, contact lens keratitis, intracameral voriconazole, anterior segment OCT, intrastromal voriconazole, endothelial plaque
Introduction
Fungal keratitis accounts for up to 40% of all cases of microbial keratitis, depending upon the geographic location.1 The most common risk factor for fungal keratitis is trauma with vegetable or organic matter. While this has not changed significantly in developing countries, contact lens use, chronic corticosteroid use, ocular surface disease and history of prior ocular surgery have emerged as important risk factors for the occurrence of fungal keratitis in developed countries.2,3 The most common fungal pathogens are Candida, Fusarium, Aspergillus and Curvularia species.4
Fungal infections of the cornea pose a diagnostic and treatment challenge. Fungi are notorious for not growing readily in vitro and, thus, cultures of fungal keratitis are often negative.5 In addition, fungal cultures may require more than seven days of incubation, which is usually the time point when cultures are discarded in most laboratories unless specified otherwise by the treating physician. Finally, fungi tend to penetrate fast and deep in the cornea and form endothelial plaques.6 Thus, access to a fungal infiltrate for culture may be difficult, which furthers limits our ability to correctly and promptly diagnose and treat fungal keratitis.
A clinical characteristic that can help differentiate some forms of fungal keratitis from other causes of infectious keratitis is the presence of a deep stromal infiltrate with a limited inflammatory response and an intact corneal epithelium.7 In contrast, bacterial pathogens tend to present with an epithelial defect over the underlying infiltrate. An intact epithelium forms a natural barrier to the penetration of topical antifungal agents which tend to be hydrophilic in nature and, thus, do not penetrate readily through the hydrophobic corneal epithelial cell membranes.7 The limited armamentarium of antifungal agents along with the usual delay in diagnosis and the propensity of fungi to invade deep in the cornea result in poor outcomes of medical management for fungal keratitis. Thus, it is not surprising that in cases of fungal keratitis a therapeutic penetrating keratoplasty is often needed for eradication.8
Herein, we report a case with a culture-negative deep stromal infiltrate that failed to respond to topical, oral, intrastromal and intracameral antifungals. OCT-guided endothelial biopsy provided the definitive diagnosis of fungal infection and serial intrastromal and intracameral voriconazole injections post-operatively spared this young patient a therapeutic penetrating keratoplasty.
Case Report
A 22-year-old woman was referred to the Bascom Palmer Eye Institute for evaluation of a mid-stromal corneal infiltrate in her left eye. The patient had been on oral acyclovir, topical trifluridine and moxifloxacin for two weeks with worsening irritation, light sensitivity and blurred vision. She was a soft contact lens wearer and had been using prednisolone acetate 1% as needed for redness over the past year. Her best-corrected visual acuity was 20/20 in the right eye and 20/30 in the involved left eye. Slit lamp examination revealed moderate conjunctival injection and two fluffy-appearing mid-stromal infiltrates without overlying epithelial defects (Figure 1A). A mild anterior chamber reaction was also observed.
Figure 1.
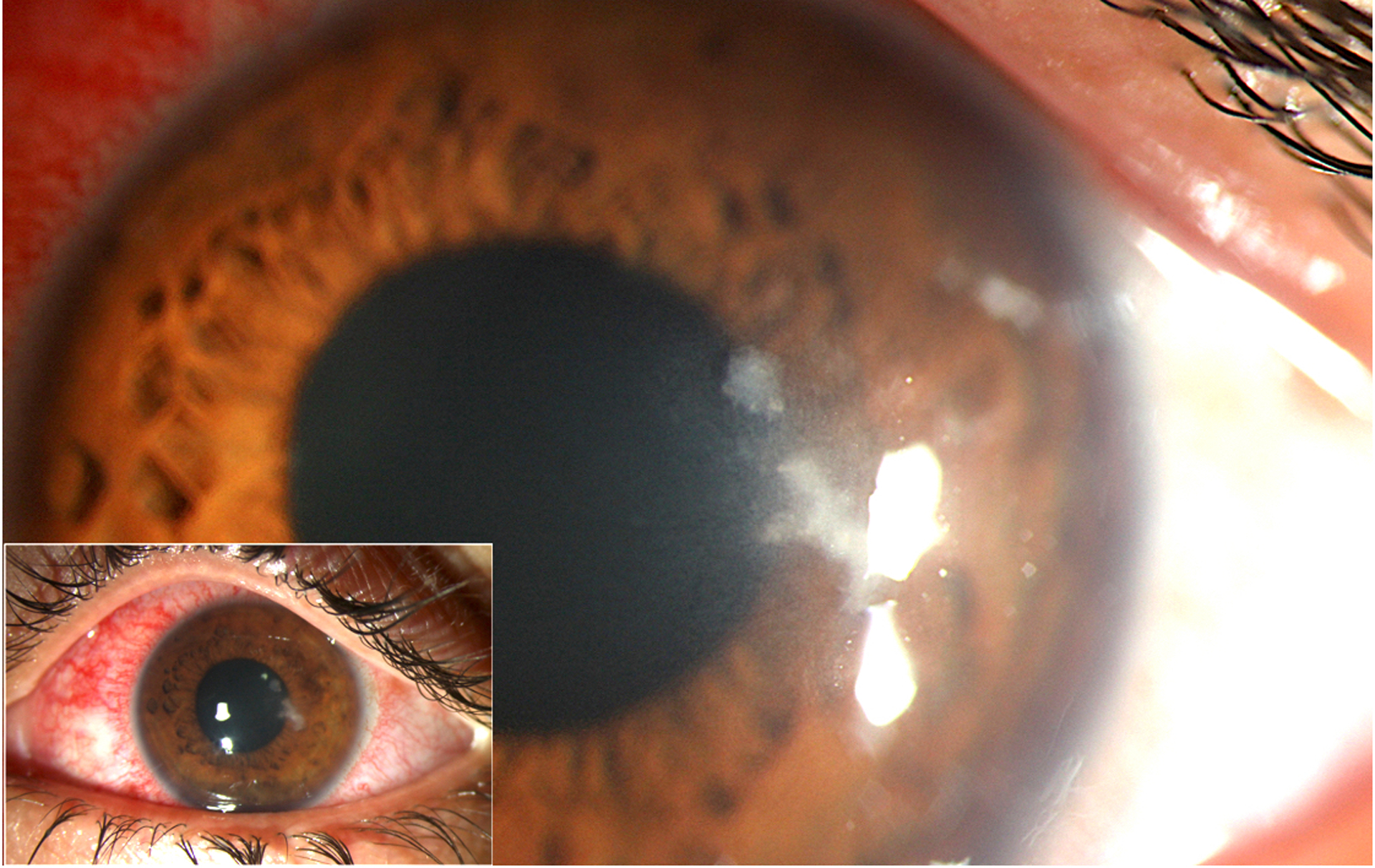
Slit lamp photographs of the patient’s left eye at presentation and after initial management. (A) At presentation, moderate conjunctival injection as well as two fluffy-appearing mid-stromal infiltrates without overlying epithelial defects were present. The patient’s vision was 20/30. (B) Four weeks after treatment with topical natamycin 1% every 1 to 2 hours (accompanied by epithelial debridement every 2 days) and oral voriconazole 200 mg twice a day, the infiltrate appeared larger and deeper, while the patient’s vision remained 20/30.
Corneal stains and cultures performed after a 24-hour antibiotic holiday were negative for bacteria, fungi, parasites and viruses. Confocal microscopy imaging at several time points during the treatment course did not show fungal hyphae. Following lack of response to a 10-day course of topical fortified antibiotics and a high clinical suspicion for fungal keratitis, the patient was started on topical natamycin 1% every hour and oral voriconazole 200 mg twice a day. Corneal epithelial debridement was performed every two days so as to improve penetration of the topical antifungal.
Despite patient compliance with the intensive administration of the antifungal agents and with the frequent follow up examinations, four weeks later the infiltrate appeared larger and deeper, while vision remained 20/30 (Figure 1B). Serial intrastromal voriconazole (100 μg) injections for 10 days failed to prevent the infiltrate from further enlarging in size and penetrating deeper in the cornea stroma. An anterior chamber culture was negative and the intrastromal injections were complemented with serial intracameral voriconazole (100 μg) injections as well for an additional week and a half. Three weeks later and following six intrastromal and four intracameral voriconazole injections, the patient presented with hypopyon and an even deeper infiltrate (Figure 2A). Vision had declined to 20/40. In order to properly identify the location of the infiltrate, anterior segment OCT (Visante, Zeiss, Dublin, CA; axial resolution 18 μm, range of image acquisition 10 mm × 3 mm, 512 A scans per line sampling) was performed and showed the presence of an endothelial plaque (Figure 2B).
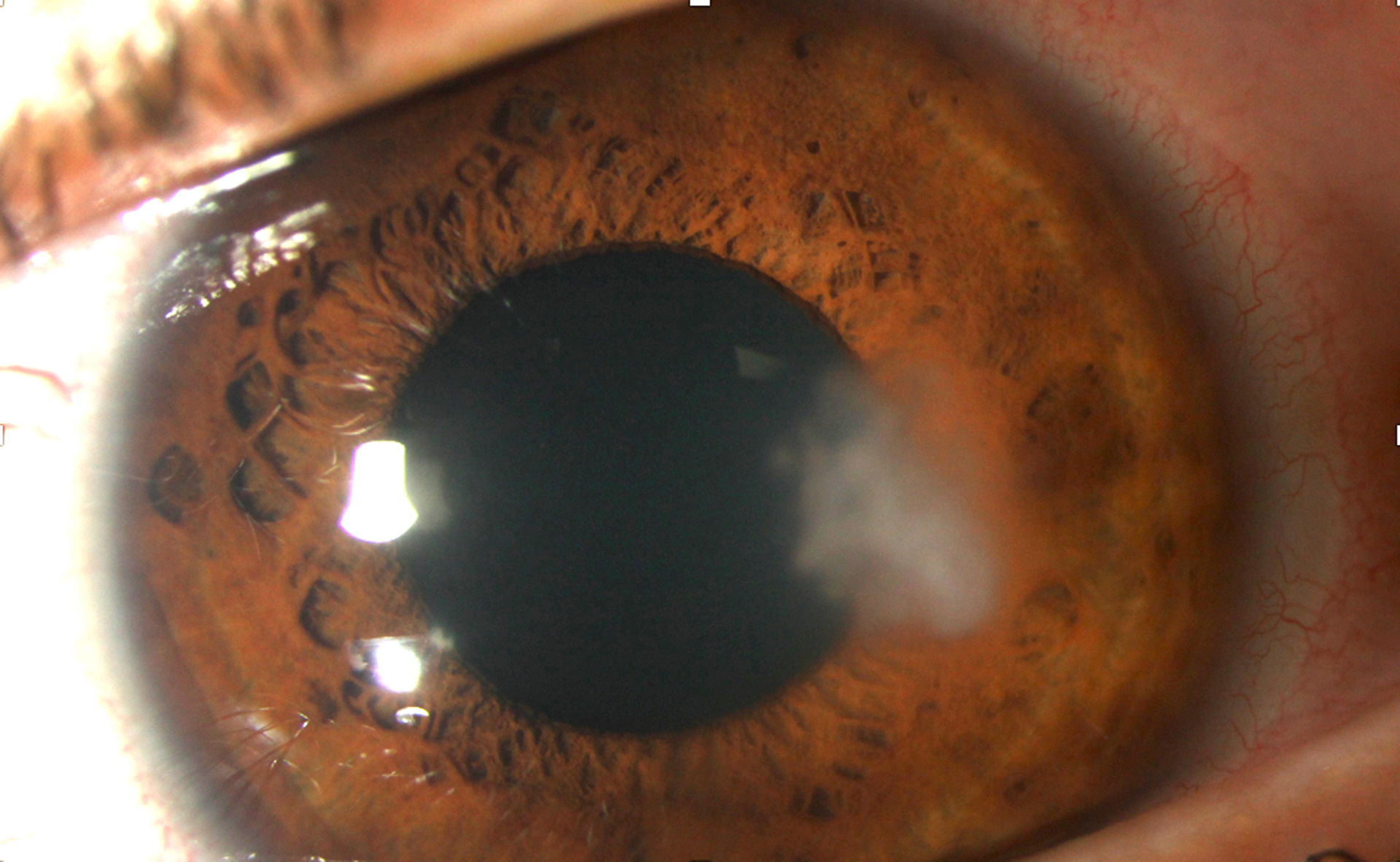
Figure 2.
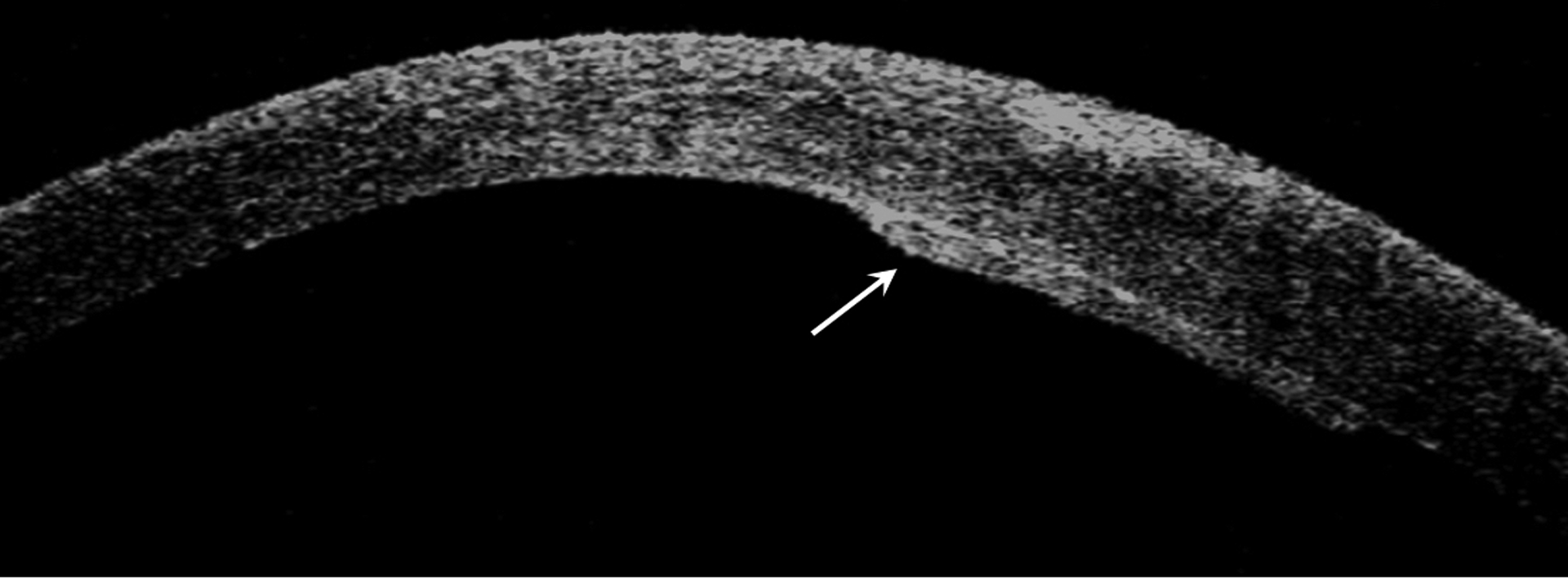
Slit lamp photograph and anterior segment OCT of the patient’s left eye after six intrastromal voriconazole (100 μg) injections, a negative anterior chamber culture and four intracameral voriconazole (100 μg) injections. (A) The infiltrate is larger in size and located even deeper in the cornea stroma, while the epithelium remains intact. The patient’s vision declined to 20/40. A small hypopyon is also evident. (B) Anterior segment OCT revealed the presence of an endothelial plaque (arrow).
Management options included a therapeutic penetrating keratoplasty or endothelial biopsy in order to identify the causative organism. After extensive discussion with the patient and her family about the risks and benefits of each approach, decision was made to proceed with an endothelial biopsy in the operating room. Following a 2-day antibiotic holiday, a 2.6 mm corneal incision was made superiorly and the Terry scraper was used to remove the entire plaque, which was approximately 3.0 × 3.0 mm in size and of rigid consistency. Cohesive viscoelastic was injected in the area of the plaque prior to its removal so as to limit the risk of seeding and to keep the anterior chamber stable. The plaque was removed in a single piece and the resultant endothelial defect in the area was approximately 3.0 × 3.5 mm in size. Following its removal, an anterior chamber wash was performed and intracameral voriconazole (100 μg) was injected. The plaque was submitted both for cultures and for histopathologic evaluation. Cultures were again negative, yet histopathology showed fungal elements (Figure 3A). In the immediate post-operative period focal corneal edema was present at the site of the biopsy, which slowly resolved over the next four weeks and yielded to a paracentral scar (Figure 3B). Intrastromal and intracameral voriconazole (100 μg) injections were continued 2 times a week for the first post-operative month. At the patient’s 3 year follow up a faint focal scar was present at the site of the prior infiltrate and her vision was 20/20.
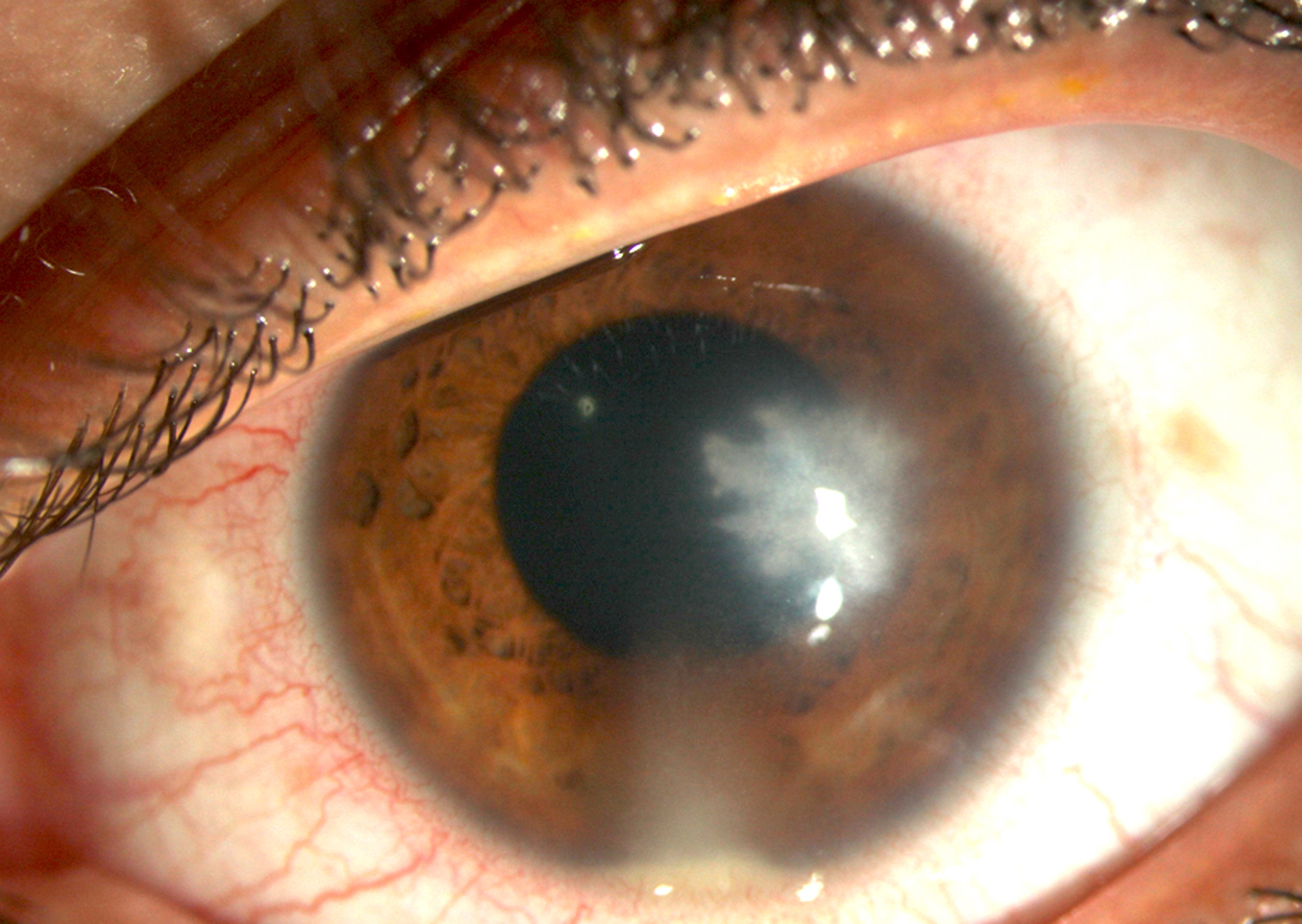
Figure 3.
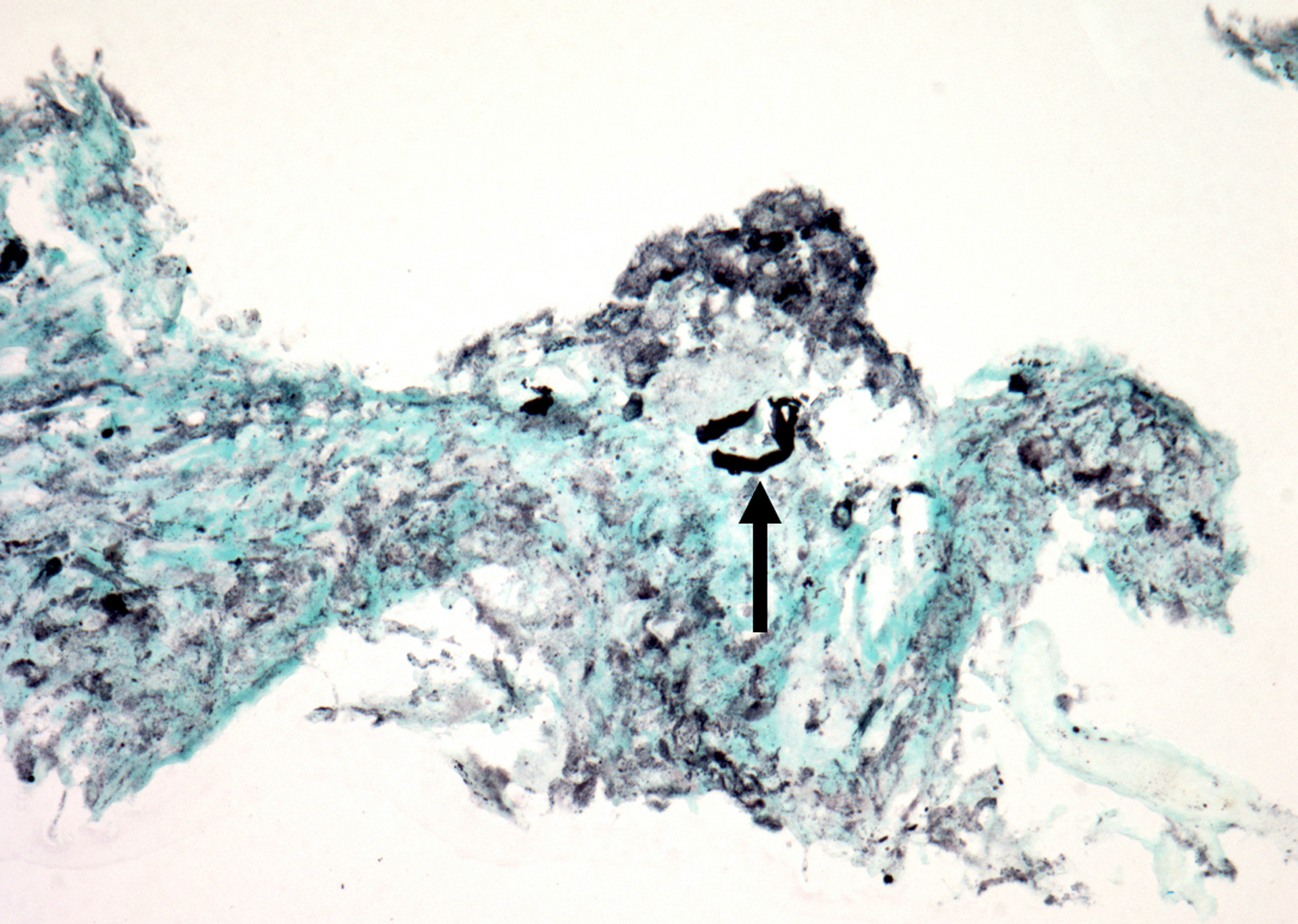
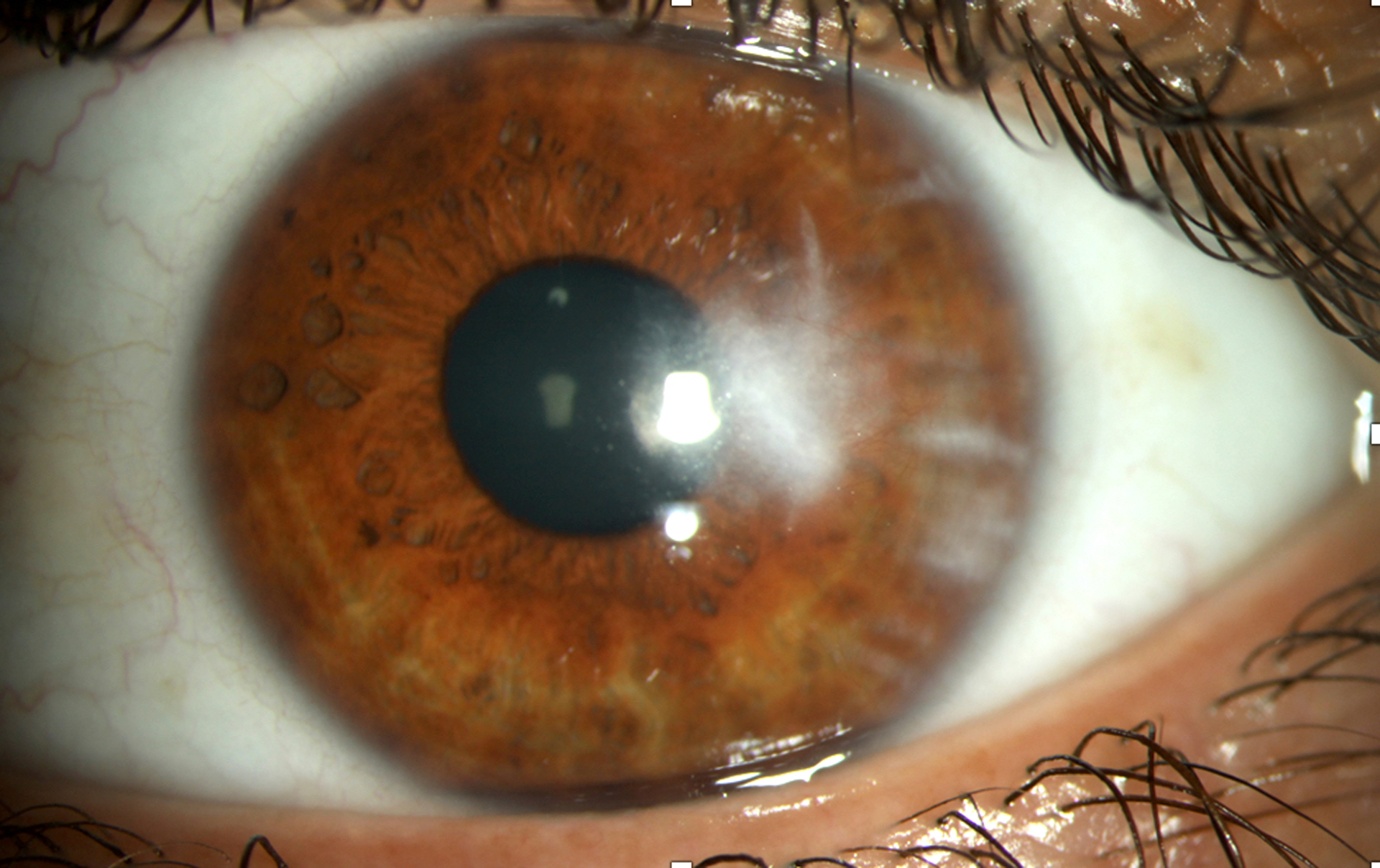
Histopathology photographs of the surgically removed endothelial plaque and slit lamp photograph of the patient’s left eye 4 weeks following the procedure. (A) Stains and cultures of the removed specimen were negative, but histopathology revealed fungal elements (arrow) within ulcerated corneal stroma (Gomori-methenamine silver; original magnification × 400). (B) The patient experienced transient focal edema at the site of the biopsy, which resolved entirely by the fourth postoperative week. A deep stromal scar remained in the area and the patient’s vision was restored to 20/20.
Discussion
This case highlights the value of anterior segment OCT in pinpointing the location of a deep corneal infiltrate, the importance of histopathology for diagnosis of culture-negative corneal infections and the potential value of surgical debulking of a fungal endothelial plaque. As an infection penetrates deeper in the cornea stroma, its exact location is difficult to discern on clinical slit lamp examination alone. In this case, anterior segment OCT imaging clearly showed that the infectious nidus had penetrated Descemet’s membrane and had formed an endothelial plaque. Retrocorneal plaques have been observed via anterior segment OCT in other forms of microbial keratitis, such as bacterial and herpetic infections.9, 10 In such cases the retrocorneal plaques are thought to be caused by collections of inflammatory cells rather than the causative pathogens.9, 10 On the other hand, both this report and two prior studies have shown that endothelial plaques in fungal keratitis contain fungi that have penetrated through Descemet’s membrane.10, 11
In our case, despite the deeper progression of the fungal infiltrate, the patient maintained good vision throughout the treatment course. Thus, our decision to proceed with endothelial biopsy had three objectives. The first goal was to obtain a definitive diagnosis of the pathogenic organism since all prior corneal and intracameral stains and cultures had been negative and the patient had responded poorly to topical, oral, intrastromal and intracameral antifungals. Histopathologic evaluation of the specimen in this case provided the final diagnosis of fungal infection; cultures and stains of the removed specimen were again negative. Fungi are notorious for poor growth in culture and in cases of progressive corneal infection, histopathology can provide the long-sought answer. For infections in the anterior corneal stroma, a corneal biopsy (typically using a 3 mm dermatologic trephine) can assist in diagnosis.12, 13 In fact, similar to our case, prior reports have indicated that histopathologic examination of biopsy specimens from previously culture-negative infectious keratitis patients is more likely to provide an answer as to the pathogenic organisms than culture of the same specimens.12, 14 For deeper cornea infections, the diagnosis often comes after therapeutic penetrating keratoplasty and histopathologic assessment of the removed corneal button.2, 5
The second goal in this case was to debulk the infectious nidus and potentially spare this young patient a therapeutic corneal graft. This was achieved, though, not without the risk of disseminating the infection in the anterior chamber and seeding the iris with fungal elements. For this reason, intracameral antifungals were injected at the end of the procedure. Moreover, serial deep intrastromal and intracameral injections of voriconazole were performed for the first four postoperative weeks. The alternative would have been a therapeutic penetrating keratoplasty with its overall poor long-term prognosis and the need for a subsequent optical graft.15, 16 The transient focal edema at the site of the biopsy resolved within 4 weeks presumably due to migration of peripheral endothelial cells which repopulated the involved area and the patient’s vision was restored to 20/20.
The third goal of the endothelial biopsy was to guide therapeutic management since the patient had failed to respond to combinations of topical, oral and intrastromal antifungals. Although stains and cultures of the removed specimen were negative, histopathologic evaluation eliminated the possibility that the infection was caused by a yeast. If Candida species were identified, our postoperative management strategy would have included intracameral amphotericin B injections.
In addition to our patient, aspiration of a retrocorneal plaque was recently reported to provide the diagnosis in two patients with progressive culture-negative deep stromal infections.11 In these two cases, diagnosis was made by Fungiflora Y® staining of the aspirates but histopathology was not performed.11 Both patients recovered without the need for a therapeutic penetrating keratoplasty, but with a final vision of hand motions and 20/80. In the other three patients in this study that already had positive fungal stains and cultures, retrocorneal plaque aspiration spared two of them from a therapeutic graft. On the other hand, in a prior study whereby fungal endothelial plaques were imaged with anterior segment OCT but no removal of the endothelial plaques was attempted, 5 out of the 6 patients ended up needing a therapeutic penetrating keratoplasty.10 Finally, endophthalmitis was reported as a severe complication of the retrocorneal plaque aspiration, though it is not clear how many patients developed it nor is it clear whether the intracameral injections of voriconazole that were performed in 3 of the 5 patients at the end of the procedure were protective.11
In conclusion, this case shows that anterior segment OCT can aid in defining the exact location of a deep corneal infection and it can reveal the presence of an endothelial plaque that may not be visible on slit lamp examination. Endothelial biopsy can be performed both for diagnostic purposes of culture-negative infections and in order to debulk the infectious nidus and guide subsequent management. The removed specimen should be submitted both for cultures and for histopathological examination, as cultures may be negative for fastidious organisms. In order to avoid seeding of the anterior segment and the development of endophthalmitis, we feel that intracameral antifungal and/or antibiotic injections should be performed at the end of the procedure and during the postoperative follow up period. In this case, debulking of the fungal endothelial plaque combined with postoperative intracameral and intrastromal voriconazole injections saved the patient from an unavoidable otherwise corneal graft. Further studies are needed to assess whether the benefits of such biopsies for retrocorneal fungal infections outweigh the risks.
Funding:
NIH Center Core Grant P30EY014801 (Bethesda, Maryland) and Research to Prevent Blindness Unrestricted Grant (New York, New York).
Footnotes
Proprietary/Financial Interests: None
References
- 1.Shah A, Sachdev A, Coggon D, et al. Geographic variations in microbial keratitis: an analysis of the peer-reviewed literature. Br J Ophthalmol. 2011;95(6):762–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Srinivasan M Fungal keratitis. Curr Opin Ophthalmol. 2004;15(4):321–327. [DOI] [PubMed] [Google Scholar]
- 3.Prajna NV, Krishnan T, Mascarenhas J, et al. Predictors of outcome in fungal keratitis. Eye (Lond). 2012;26(9):1226–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kredics L, Narendran V, Shobana CS, et al. Filamentous fungal infections of the cornea: a global overview of epidemiology and drug sensitivity. Mycoses. 2015;58(4):243–260. [DOI] [PubMed] [Google Scholar]
- 5.Garg P, Roy A, Roy S. Update on fungal keratitis. Curr Opin Ophthalmol. 2016;27(4):333–339. [DOI] [PubMed] [Google Scholar]
- 6.Thomas PA, Leck AK, Myatt M. Characteristic clinical features as an aid to the diagnosis of suppurative keratitis caused by filamentous fungi. Br J Ophthalmol. 2005;89(12):1554–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tuli SS. Fungal keratitis. Clin Ophthalmol. 2011;5:275–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prajna NV, Krishnan T, Mascarenhas J, et al. The mycotic ulcer treatment trial: a randomized trial comparing natamycin vs voriconazole. JAMA Ophthalmol. 2013;131(4):422–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Konstantopoulos A, Kuo J, Anderson D, et al. Assessment of the use of anterior segment optical coherence tomography in microbial keratitis. Am J Ophthalmol. 2008;146(4):534–542. [DOI] [PubMed] [Google Scholar]
- 10.Takezawa Y, Suzuki T, Shiraishi A. Observation of retrocorneal plaques in patients with infectious keratitis using anterior segment optical coherence tomography. Cornea. 2017;36(10):1237–1242. [DOI] [PubMed] [Google Scholar]
- 11.Kitazawa K, Fukuoka H, Inatomi T, et al. Safety of retrocorneal plaque aspiration for managing fungal keratitis. Jpn J Ophthalmol. 2020;64(2):228–233. [DOI] [PubMed] [Google Scholar]
- 12.Younger JR, Johnson RD, Holland GN, et al. Microbiologic and histopathologic assessment of corneal biopsies in the evaluation of microbial keratitis. Am J Ophthalmol. 2012;154(3):512–519 e512. [DOI] [PubMed] [Google Scholar]
- 13.Alexandrakis G, Haimovici R, Miller D, et al. Corneal biopsy in the management of progressive microbial keratitis. Am J Ophthalmol. 2000;129(5):571–576. [DOI] [PubMed] [Google Scholar]
- 14.Ishibashi Y, Hommura S, Matsumoto Y. Direct examination vs culture of biopsy specimens for the diagnosis of keratomycosis. Am J Ophthalmol. 1987;103(5):636–640. [DOI] [PubMed] [Google Scholar]
- 15.Xie L, Zhai H, Shi W. Penetrating keratoplasty for corneal perforations in fungal keratitis. Cornea. 2007;26(2):158–162. [DOI] [PubMed] [Google Scholar]
- 16.Yao YF, Zhang YM, Zhou P, et al. Therapeutic penetrating keratoplasty in severe fungal keratitis using cryopreserved donor corneas. Br J Ophthalmol. 2003;87(5):543–547. [DOI] [PMC free article] [PubMed] [Google Scholar]


