Abstract
Individuals with the highest risk for adverse outcomes of COVID-19 should be prioritized by the vaccine allocation policies. We have conducted a literature review of published studies, which comprehend congenital heart disease (CHD) and COVID-19, in order to present the overall evidences of both exposure and clinical risk of patients with adult congenital heart disease (ACHD) and to propose a risk profile schema for those patients to be incorporated into vaccine distribution decisions.
Keywords: ACHD, COVID-19, Vaccine, Risk factors
Background
The coronavirus disease 2019 (COVID-19) has provoked an overwhelming impact on healthcare systems worldwide, with million of victims to date [1,2]. As things stand, the urgent availability of numerous vaccines is of utmost importance in combating the COVID-19 pandemic.
Individuals with the highest risk for adverse outcomes of COVID-19 should be prioritized by the vaccine allocation policies around the world [[2], [3], [4], [5]].
Diverse factors may influence the risk for adverse outcomes COVID-19-related, not to mention the chances of contagion and the risk for adverse clinical outcomes due to the acute infection.
On that account, we have conducted a literature review of published studies which comprehend congenital heart disease (CHD) and COVID-19, in order to present the overall evidences of both exposure and clinical risk of patients with adult congenital heart disease (ACHD) needed for vaccine allocation efforts, and to propose a risk profile schema for ACHD patients to be incorporated into vaccine distribution decisions.
Adult congenital heart disease
Congenital heart disease (CHD) is the most common global inborn disorder. With an increasing life expectancy, adults with CHD are exposed to acquired diseases, cardiovascular disease and to environmental threats, along with infectious diseases [6].
Different studies have recognized adult-onset cardiovascular disease as a risk factor for mortality in COVID-19 infections [3]. Hence, by the beginning of the COVID-19 pandemic, it was feared this risk might have been further multiplied in patients with CHD, especially when associated with diverse comorbidities such as pulmonary hypertension, heart failure, or in the presence of complex congenital heart disease [[6], [7], [8], [9]].
There are limited data with several knowledge gaps remaining about adult congenital heart disease (ACHD) and potentially adverse outcomes in patients contracting COVID-19 [10].
Moreover, the anatomy, physiology and functional status amongst ACHD patients are varied. For this reason, the risk for poor outcomes from COVID-19 in the very heterogeneous ACHD population remains, albeit poorly specified.
In this context, Cleary et al. [11] reported a comprehensive review of literature of a total of 94 suspected or confirmed cases from 7 papers [[12], [13], [14], [15], [16], [17], [18]]; of those, the largest published series comes from Italy [12], with 76 patients included. Amongst the 94 reported CHD cases with COVID-19 infection, 79 (84%) were adults whereas 15 (16%) children. Only one death reported from these combined series (mortality just over 1%).
Furthermore, Lewis et al. [19] reported a single-center cohort study from New York City evaluating COVID-19-related outcomes in patients with CHD. From a population of >7000 adults and children under follow-up at their tertiary center, only 53 CHD patients presented with COVID-19-related symptoms over a 4-month period, 43 (81%) of them adults; seven patients (5.7%) died from COVID-19 in this cohort [18].
Broberg et al. [20] reported a study from 58 ACHD centers, including 1044 infected patients: 118 (11%) with single ventricle physiology, 87 (8%) with cyanosis, and 73 (7%) with pulmonary hypertension. Twenty-four COVID-related deaths were reported, and factors associated with mortality consisted of male sex, diabetes, cyanosis, pulmonary hypertension, heart failure.
Finally, Schwerzmann [21] et al. showed that among 105 ACHD patients 13 had a severe disease course and 5 died with general risk factors (age, obesity and multiple comorbidities) resulting associated with an increased risk of mortality.
Accordingly, all the reported studies showed type of ACHD, including single ventricle physiology, was not associated with worse clinical outcomes related to COVID-19. ACHD patients at advanced physiological stage were at highest risk of a moderate/severe course of COVID-19 disease.
However, ACHD patients at advanced physiological stage, in turn were considered, if had one of the following criteria:
-
-
New York Heart Association (NYHA) functional class III or greater;
-
-
hypoxemia (pulse oximetry at rest <90%);
-
-
arrhythmias;
-
-
haemodynamically significant shunt (Qp:Qs ≥ 1.5:1 and/or chamber dilatation in correspondence to shunt);
-
-
moderate/severe aortic dilatation;
-
-
moderate or severe valvular stenosis or regurgitation;
-
-
clinical or laboratory evidence of end-organ failure;
-
-
pulmonary hypertension (mean pulmonary artery pressure ≥25 mmHg);
-
-
Eisenmenger syndrome.
Worldwide literature at present suggests that estimated prevalence of COVID-19 disease amongst ACHD patients and related mortality of ACHD to be low [[11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21]]. The former may be the result, at least in part, of precautionary shielding. Moreover, the disease does not seem to impact a specific form of CHD.
Furthermore, reduced exposure because of shielding, rather than resistance to infection, and/or incomplete recognition due to the generally mild or asymptomatic COVID-19 disease in ACHD, may in part explain this. ACHD patients are generally a relative young population, which may have an effect on COVID-19 outcome.
Studies published so far [[11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21]] did not show similar critical respiratory outcomes and/or the higher mortality rates reported in other cardiovascular diseases [2,3]. This would suggest that advanced physiological state and adult-onset cardiovascular risk factors, like older age, obesity, hypertension and diabetes play a pivotal role in COVID-19 mortality, rather than congenital cardiac disease per se [22].
Thus, it is imperative to recognize the clinical characteristics of advanced physiological state of patients with ACHD that may lead to adverse outcomes, including mortality, at this time of ongoing COVID-19 pandemic.
Pulmonary hypertension
Data regarding patients with pulmonary hypertension (PH) are, likewise, limited; it seems, however, that PH carries an increased mortality risk related to COVID-19.
A survey amongst 77 American PH centers showed, even a similar incidence of COVID-19 infection in patients with PH to the general U.S. population (2.9 per 1000 patients), albeit rates of hospitalization and mortality were much higher, at 30% and 12% respectively amongst the former [23].
Although no studies are available at present examining the interaction between PH severity and COVID-19 infection and outcomes, we speculate COVID-19 may augment pulmonary vascular disease through multiple mechanisms including pneumonia - with worsening V/Q mismatch - and hypoxia, hypercapnic vasoconstriction, and/or thrombosis [24]. On the other hand, COVID-19 may also impact, directly, on endothelial cells leading to or accelerating endothelial dysfunction.25 The latter is particularly relevant in patients with haemodinamically significant PH, whereas the pre-existing endothelial dysfunction superimposed by COVID-19 act as a trigger for progressive vasoconstriction and end-organ damage.
Last but not least, it is possible that patients with PH had undergone fewer clinic visits and diagnostic testing because of shielding for COVID-19, potential compromising treatment and care, albeit this is speculative.
Proposed vaccination allocation and prioritization by ACHD clinical risk for COVID-19 adverse outcomes.
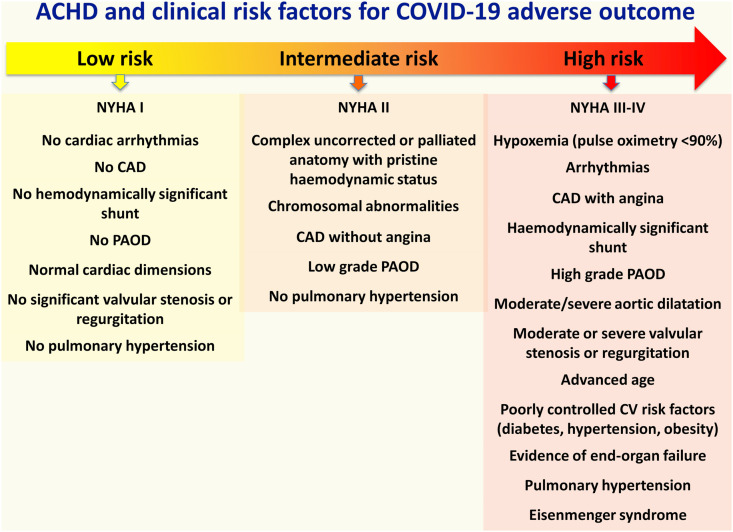
Based on literature review, available data and our experience, we propose a vaccine allocation schema (Fig. 1 ) that describes the major CV clinical risk considerations in the broader and complex context of ACHD.
Fig. 1.
Risk stratification schema of ACHD patients according to anatomical and physiological patterns. CAD = coronary artery disease; PAOD = peripheral arterial occlusive disease; CV = cardiovascular.
The schema prioritizes the high risk ACHD subsets, who should receive COVID-19 vaccination without delay.
Physiological status, symptoms including history of heart failure and presence of pulmonary hypertension determine COVID-19 risks and not complexity of underplaying CHD conditions in the ACHD population. All ACHD patients, high or low risk should observe social distance measures and invest on optimizing modifiable risk factors such as obesity, smoking and lack of exercise, which will impact on quality of life and outcomes, the latter whether COVID-19 or not.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Cheng V.C., Lau S.K., Woo P.C., Yuen K.Y. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin Microbiol Rev. 2007;20:660–694. doi: 10.1128/CMR.00023-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehra M.R., Desai S.S., Kuy S., Henry T.D., Patel A.N. Cardiovascular disease, drug therapy, and mortality in Covid-19. N Engl J Med. 2020;382:e102. doi: 10.1056/NEJMoa2007621. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 3.Sabatino J., De Rosa S., Di Salvo G., Indolfi C. Impact of cardiovascular risk profile on COVID-19 outcome. A meta-analysis. PloS One. 2020 Aug 14;15(8) doi: 10.1371/journal.pone.0237131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Driggin E., Maddox T.M., Ferdinand K.C., Kirkpatrick J.N., Ky B., Morris A.A., Mullen J.B., Parikh S.A., Philbin D.M., Jr., Vaduganathan M. ACC health policy statement on cardiovascular disease considerations for COVID-19 vaccine prioritization: a report of the American college of cardiology solution set oversight committee. J Am Coll Cardiol. 2021 Apr 20;77(15):1938–1948. doi: 10.1016/j.jacc.2021.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Egidy Assenza G., Castaldi B., Flocco S., Luciani G.B., Meliota G., Rinelli G., Vairo U., Favilli S. Board of the Italian society of pediatric cardiology. COVID-19 vaccine priority access for adults and children with congenital heart disease: a statement of the Italian society of pediatric cardiology. Congenit Heart Dis. 2021 doi: 10.32604/CHD.2021.016713. [DOI] [Google Scholar]
- 6.Brida M., Chessa M., Gu H., Gatzoulis M.A. The globe on the spotlight: coronavirus disease 2019 (Covid-19) Int J Cardiol. 2020 Jul 1;310:170–172. doi: 10.1016/j.ijcard.2020.04.006. Epub 2020 Apr 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan W., Aboulhosn J. The cardiovascular burden of coronavirus disease 2019 (COVID-19) with a focus on congenital heart disease. Int J Cardiol. 2020 Jun 15;309:70–77. doi: 10.1016/j.ijcard.2020.03.063. Epub 2020 Mar 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morray B.H., Gordon B.M., Crystal M.A., Goldstein B.H., Qureshi A.M., Torres A.J., Epstein S.M., Crittendon I., Ing F.F., Sathanandam S.K. Resource allocation and decision making for pediatric and congenital cardiac catheterization during the novel coronavirus SARS-CoV-2 (COVID-19) pandemic: a U.S. Multi-institutional perspective. J Invasive Cardiol. 2020;32:E103–E109. doi: 10.25270/jic/20.00189. [DOI] [PubMed] [Google Scholar]
- 9.Lu X., Zhang L., Du H., Zhang J., Li Y.Y., Qu J., Zhang W., Wang Y., Bao S., Li Y., Wu C., Liu H., Liu D., Shao J., Peng X., Yang Y., Liu Z., Xiang Y., Zhang F., Silva R.M., Pinkerton K.E., Shen K., Xiao H., Xu S., Wong G.W.K. Chinese pediatric novel coronavirus study team. SARS-CoV-2 infection in children. N Engl J Med. 2020 Apr 23;382(17):1663–1665. doi: 10.1056/NEJMc2005073. Epub 2020 Mar 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diller G.P., Gatzoulis M.A., Broberg C.S., Aboulhosn J., Brida M., Schwerzmann M., Chessa M., Kovacs A.H., Roos-Hesselink J. Coronavirus disease 2019 in adults with congenital heart disease: a position paper from the ESC working group of adult congenital heart disease, and the International Society for Adult Congenital Heart Disease. Eur Heart J. 2021 May 14;42(19):1858–1865. doi: 10.1093/eurheartj/ehaa960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cleary A., Chivers S., Daubeney P.E., Simpson J.M. Impact of COVID-19 on patients with congenital heart disease. Cardiol Young. 2021 Jan;31(1):163–165. doi: 10.1017/S1047951120004345. [DOI] [PubMed] [Google Scholar]
- 12.Sabatino J., Ferrero P., Chessa M., Bianco F., Ciliberti P., Secinaro A., Oreto L., Avesani M., Bucciarelli V., Calcaterra G., Calabrò M.P., Russo M.G., Bassareo P.P., Guccione P., Indolfi C., Di Salvo G. COVID-19 and congenital heart disease: results from a nationwide survey. J Clin Med. 2020 Jun 8;9(6):1774. doi: 10.3390/jcm9061774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simpson M., Collins C., Nash D.B., Panesar L.E., Oster M.E. COVID-19 infection in children with pre-existing heart disease. J Pediatr. 2020;S0022–3476(20):30968–30969. doi: 10.1016/j.jpeds.2020.07.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shekerdemian L.S., Mahmood N.R., Wolfe K.K., Riggs B.J., Ross C.E., McKiernan C.A., Heidemann S.M., Kleinman L.C., Sen A.I., Hall M.W., Priestley M.A., McGuire J.K., Boukas K., Sharron M.P., Burns J.P., International COVID-19 PICU Collaborative Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020 Sep 1;174(9):868–873. doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrero P., Piazza I., Ciuffreda M. COVID-19 in adult patients with CHD: a matter of anatomy or comorbidities? Cardiol Young. 2020;30:1196–1198. doi: 10.1017/S1047951120001638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bezerra R.F., Franchi S.M., Khader H., Castro R.M., Liguori G.R., da Fonseca da Silva L., Pedro da Silva J. COVID-19 as a confounding factor in a child submitted to staged surgical palliation of hypoplastic left heart syndrome: one of the first reports of SARS-CoV-2 infection in patients with congenital heart disease. J Thorac Cardiovasc Surg. 2021 Feb;161(2):e97–e101. doi: 10.1016/j.jtcvs.2020.05.081. Epub 2020 Jun 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salik I., Mehta B. Tetralogy of Fallot palliation in a COVID-19 positive neonate. J Clin Anesth. 2020;66:109914. doi: 10.1016/j.jclinane.2020.109914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krishnan U.S., Krishnan S.S., Jain S., et al. Severe acute respiratory syndrome associated with Coronavirus 2 infection in patients with down syndrome, congenital heart disease, and pulmonary hypertension: is down syndrome a risk factor? J Pediatr. 2020;S0022–3476(20):30830–30831. doi: 10.1016/j.jpeds.2020.06.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis M.J., Anderson B.R., Fremed M., et al. Impact of coronavirus disease 2019 (COVID-19) on patients with congenital heart disease across the lifespan: the experience of an academic congenital heart disease center in New York City. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.017580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Broberg C.S., Kovacs A.H., Sadeghi S., Rosenbaum M.S., Lewis M.J., Carazo M.R., Rodriguez F.H., 3rd, Halpern D.G., Feinberg J., Galilea F.A., Baraona F., Cedars A.M., Ko J.M., Porayette P., Maldonado J., Sarubbi B., Fusco F., Frogoudaki A.A., Nir A., Chaudhry A., John A.S., Karbassi A., Hoskoppal A.K., Frischhertz B.P., Hendrickson B., Bouma B.J., Rodriguez-Monserrate C.P., Broda C.R., Tobler D., Gregg D., Martinez-Quintana E., Yeung E., Krieger E.V., Ruperti-Repilado F.J., Giannakoulas G., Lui G.K., Ephrem G., Singh H.S., Almeneisi H.M., Bartlett H.L., Lindsay I., Grewal J., Nicolarsen J., Araujo J.J., Cramer J.W., Bouchardy J., Al Najashi K., Ryan K., Alshawabkeh L., Andrade L., Ladouceur M., Schwerzmann M., Greutmann M., Meras P., Ferrero P., Dehghani P., Tung P.P., Garcia-Orta R., Tompkins R.O., Gendi S.M., Cohen S., Klewer S., Hascoet S., Mohammadzadeh S., Upadhyay S., Fisher S.D., Cook S., Cotts T.B., Aboulhosn J.A. COVID-19 in adults with congenital heart disease. J Am Coll Cardiol. 2021 Apr 6;77(13):1644–1655. doi: 10.1016/j.jacc.2021.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwerzmann M., Ruperti-Repilado F.J., Baumgartner H., Bouma B., Bouchardy J., Budts W., Campens L., Chessa M., Del Cerro Marin M.J., Gabriel H., Gallego P., Garcia-Orta R., Gonzalez A.E., Jensen A.S., Ladouceur M., Miranda-Barrio B., Morissens M., Pasquet A., Rueda J., van den Bosch A.E., van der Zwaan H.B., Tobler D., Greutmann M., EPOCH Clinical outcome of COVID-19 in patients with adult congenital heart disease. Heart. 2021 Mar 8 doi: 10.1136/heartjnl-2020-318467. heartjnl-2020-318467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yuan S., Oechslin E. Anatomical complexity does not predict outcomes after COVID-19 in adults with congenital heart disease. Heart. 2021 Apr 16 doi: 10.1136/heartjnl-2021-319054. heartjnl-2021-319054. [DOI] [PubMed] [Google Scholar]
- 23.Lee J.D., Burger C.D., Delossantos G.B., et al. A survey based estimate of COVID-19 incidence and outcomes among patients with pulmonary arterial hypertension or chronic thromboembolic pulmonary hypertension and impact on the process of care. Ann Am Thorac Soc. 2020;17:1576–1582. doi: 10.1513/AnnalsATS.202005-521OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ssentongo P., Ssentongo A.E., Heilbrunn E.S., Ba D.M., Chinchilli V.M. Association of cardiovascular disease and other pre-existing comorbidities with COVID-19 mortality: a systematic review and meta-analysis. PloS One. 2020;15 doi: 10.1371/journal.pone.0238215. [DOI] [PMC free article] [PubMed] [Google Scholar]