Abstract
Background
During the 2020 SARS-CoV-2 outbreak in New York City, hospitals canceled elective surgeries to increase capacity for critically ill patients. We present case volume data from our community hospital to demonstrate how this shutdown affected surgical care.
Methods
Between March 16 and June 14, 2020, all elective surgeries were canceled at our institution. All procedures performed during this operating room shutdown (ORS) were logged, as well as those 4 weeks before (PRE) and 4 weeks after (POST) for comparison.
Results
A total of 2,475 cases were included in our analysis, with 754 occurring during shutdown. Overall case numbers dropped significantly during ORS and increased during recovery (mean 245.0 ± 28.4 PRE versus 58.0 ± 30.9 ORS versus 186.0±19.4 POST cases/wk, P< 0.001). Emergency cases predominated during ORS (26.4% PRE versus 59.3% ORS versus 31.5% POST, P< 0.001) despite decreasing in frequency (mean 64.5 ± 7.9 PRE versus 34.4 ± 12.1 ORS versus 58.5 ± 4.0 POST cases/wk, P< 0.001). Open surgeries remained constant in all three phases (52.2-54.1%), whereas laparoscopic and robotic surgeries decreased (-3.4% and -3.0%, P< 0.001). General and/or vascular surgery, urology, and neurosurgery comprised a greater proportion of caseload (+9.5%, +3.0%, +2.8%), whereas orthopedics, gynecology, and otolaryngology/plastic surgery all decreased proportionally (-5.0%, -4.4%, -5.9%, P< 0.001).
Conclusion
Operative volume significantly decreased during the SARS-CoV-2 outbreak. Emergency cases predominated during this time, although there were fewer emergency cases overall. General/vascular surgery became the most active service and open surgeries became more common. This reallocation of resources may be useful for future crisis planning among community hospitals.
Keywords: SARS-CoV-2, COVID-19, Operating room, Resource allocation, General surgery, Quality improvement
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the pathogen that causes coronavirus disease 2019 (COVID-19), has presented unique challenges to surgical practice worldwide. COVID-19 has been linked to increased perioperative morbidity and mortality, and diagnosis of preexisting infection is often missed preoperatively.1 , 2 In addition, both patients and providers are at risk of transmitting or acquiring COVID-19 in the hospital environment, which discourages elective surgeries and creates technical obstacles for urgent or emergency surgeries.3 Lastly, COVID-19 surges have necessitated rapid reallocation of resources and personnel away from the operating room (OR) to accommodate influxes of critically ill COVID-19-positive patients, which can cause disruptions to surgical service. Because of these issues, current consensus guidelines have recommended proactive limitation or suspension of elective surgical services during COVID-19 surges, which can impact overall quality of surgical care.3, 4, 5, 6
When the COVID-19 outbreak first occurred in New York City in early spring 2020, it was marked by a rapid spike in cases, resulting in a devastating peak hospitalization rate of over 1,800 cases/day and a peak mortality rate of over 500 cases/day just four weeks after the first local diagnosis was made.7 This “first wave” of the pandemic in the United States, spanning roughly from March-May 2020, resulted in the diagnosis of over 203,000 confirmed COVID-19 cases throughout the city, which put significant strain on local healthcare systems.7, 8, 9 Accordingly, by gubernatorial mandate, New York-based hospital systems limited surgical services and shut down operating rooms to accommodate the new, overwhelming need for COVID-related hospitalizations during this time.1 , 10 These changes had a significant impact on caseloads and outcomes, although the full extent of this impact is not yet well-realized.
In this study, we present data from our New York-based community hospital during the spring of 2020 to demonstrate how the implementation of operating room restrictions affected operative case volumes between different surgical specialties. We further present data regarding changes in emergency caseloads, perioperative decision-making, and our subsequent recovery from this shutdown.
Methods
Restructuring the hospital
From March 16 to June 14, 2020, our 591-bed community hospital (NewYork-Presbyterian Brooklyn Methodist Hospital, NYPBMH) canceled all elective surgical procedures, expanding intensive care capacity by re-designating post-anesthesia care units, coronary care units, endoscopy suites, pediatric wards, and even psychiatric wards as COVID-19 overflow intensive care units (ICUs). To facilitate this expansion, the hospital purchased additional ventilators, hired traveling nursing staff and respiratory therapists, divided the emergency department into dedicated COVID and non-COVID sections with temporary respiratory isolation barriers, and formed anesthesiology-led dedicated emergency airway intubation teams. In the weeks following these preparations, the hospital saw an increase in average daily emergency department admission rates from 26.4% to 40.5%, with a peak COVID-related admission rate of 60 new cases per day in late March 2020.
During this inpatient surge, only 3 of 18 inpatient operating rooms remained open to accommodate urgent and emergency surgery. In accordance with guidelines from the American College of Surgeons,5 emergency cases were defined as cases that required operative intervention within the first 24 hours of hospitalization (e.g., perforated viscus) and were treated immediately depending on operating room availability. Urgent surgery requests were reviewed by a multidisciplinary leadership group, which included representation from the general surgery, orthopedic surgery, urology, and neurosurgery departments; this body determined the timing of urgent surgeries on a case-by-case basis and reported directly to the greater NewYork-Presbyterian Health System. Non-urgent procedures with only mild symptoms were delayed indefinitely, and nonoperative management of emergency procedures (e.g., antibiotics or interventional radiology for appendicitis) was pursued when possible. While minimally invasive surgery was encouraged if considered standard-of-care (e.g., laparoscopic cholecystectomy), it was otherwise discouraged to preserve resources and reduce potential COVID-19 spread via pneumoperitoneum. Moreover, for all laparoscoipc surgeries, specialized smoke evacuators with filters were made mandatory, regardless of urgency. All attendings were aligned with this plan.
Data collection and study variables
For this analysis, surgical volumes and data were obtained directly from weekly case logs from the operating room. These logs documented all surgical cases performed within the hospital and tracked basic statistics, such as procedure time and/or date, patient medical record number, Current Procedural Terminology code (CPT), operating surgeon and/or service, and reason for admission. Additional data regarding patient demographics, length of hospital stay, and final disposition were obtained retrospectively from the electronic medical record. Surgical services were divided into six primary groups based on preexisting departmental structure within the hospital: general and vascular surgery; orthopedics and podiatry; obstetrics and gynecology; otolaryngology, plastic, and hand surgery; urology; and neurosurgery.
All procedures performed in the OR during the shutdown (ORS, 13 wk) were recorded, as well as those 4 weeks before (PRE) and 4 weeks after (POST) for comparison. This bookend time of 4 weeks was chosen since operating rooms were fully active for both time intervals; waiting 13 weeks for an identical time frame for comparison was not practical for this study. Total operative volume, volume by specialty, surgical approach (open versus laparoscopic versus robotic versus intravascular), and emergency status were analyzed and compared between PRE, ORS, and POST case cohorts.
All pediatric cases (<18 y old) requiring an overnight inpatient stay were transferred to a dedicated in-system pediatric hospital. Advanced pulmonary and gastroenterology endoscopic procedures such as bronchoscopies and endoscopies, while performed in the operating room during this time period, were excluded from analysis due to their small number and different resource requirements. Obstetrical caesarian sections and other related procedures were also excluded from this study since they were performed in a separate unit that was not impacted by the change in hospital policy.
An additional subgroup analysis of appendectomy cases was conducted to analyze the effect of an OR shutdown on a common emergency procedure. Within this analysis, further consideration was given for case severity on presentation, operative versus conservative management, surgical approach, and readmission after surgery.
Statistical analysis and ethics
Data from the registry were deidentified and entered into LibreOffice Calc (v7.0.3.1, The Document Foundation, Berlin, Germany) on a password-protected computer with an encrypted hard drive. R statistical programming language (v4.0.3, R Foundation for Statistical Computing, Vienna, Austria, 10 October 2020) was used for statistical analysis. Approval of the study was obtained via in-hospital institutional review board (IRB), which approved wavier of consent.
Surgical caseloads were categorized and normalized to average cases per week. Major categories and subgroups were also expressed as proportions (percentages) of overall caseload per time period. Associations between continuous variables were determined using student t-test or analysis of variance (ANOVA) where appropriate. Comparisons between categorical variables were made via Pearson chi-square test. A P-value ≤ 0.05 was considered significant.
Results
Timeline and overall caseloads
The operating room shutdown at NYPBMH lasted 13 weeks (March 16 to June 14, 2020). Accounting for an additional 4 weeks before (PRE) and after (POST) the shutdown (ORS), the total time period for data collection and analysis was 21 weeks (February 17 to July 12, 2020).
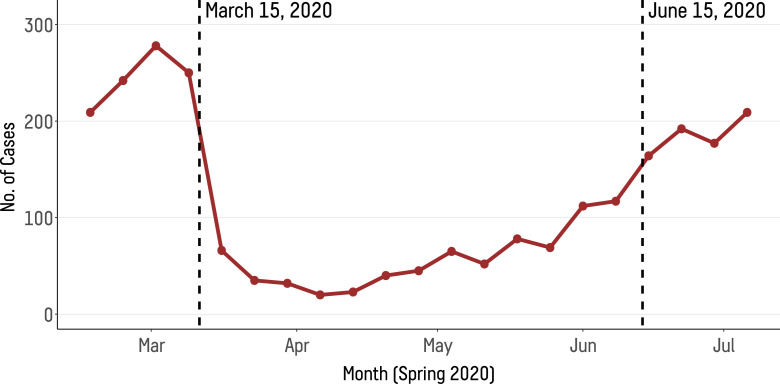
Over this 21-wk time frame, a total of 2,475 surgical cases were documented. Between the three phases of our analysis, case numbers dropped significantly during ORS and increased during recovery once restrictions were lifted (mean 245.0 ± 28.4 PRE versus 58.0 ± 30.9 ORS versus 186.0 ± 19.4 POST cases/wk, P < 0.001, see Fig. 1 ). Within ORS, the majority of cases occurred during the latter half of shutdown, with the highest weekly case tally occurring during the final week before reopening (117 cases, ORS wk #13) and the lowest weekly case tally occurring during early April (20 cases, ORS wk #4). By the end of the analysis, weekly case totals had returned to their pre-shutdown levels (209 cases during PRE wk #1 versus 209 cases during POST wk #4).
Fig. 1.
Operating room weekly case totals through the 21-wk study period. Case totals sharply decreased after cancellation of elective cases, followed by gradual increase during recovery as restrictions were lifted. Color version of figure is available online.
Total hospital admissions during the three time periods were 1,747, 3,974, and 1,233 during the PRE, ORS, and POST time periods, respectively. Corresponding total OR case counts for these time periods were 979, 754, and 742, demonstrating a decrease in case-admission ratio during ORS (56.0% versus 19.0% versus 60.0%).
Surgical cases by category
Table 1 shows that emergency cases comprised the majority of surgeries during ORS, while representing fewer than one-third of cases during the PRE and POST time periods (26.4% PRE versus 59.3% ORS versus 31.5% POST, P < 0.001, see Fig. 2 upper panel). Despite this, the overall frequency of emergency cases decreased during ORS (mean 64.5 ± 7.9 PRE versus 34.4 ± 12.1 ORS versus 58.5 ± 4.0 POST cases/wk, P < 0.001), with a nadir at ORS wk #4 (14 cases). By ORS wk #13, the weekly emergency case rate was similar to those of non-shutdown periods (60 cases/wk).
Table 1.
Average cases per wk and proportion of overall caseload categorized by emergency status, surgical approach, and service.
| Average cases per wk |
Proportion of overall caseload |
|||||||
|---|---|---|---|---|---|---|---|---|
| PRE (n = 979) |
ORS (n = 754) |
POST (n = 742) |
p-value (ANOVA) |
PRE (n = 979) |
ORS (n = 754) |
POST (n = 742) |
P-value (χ2) |
|
| Emergency | <0.001 | |||||||
| No | 180.0 ± 30.0 | 23.6 ± 20.0 | 127.0 ± 23.2 | <0.001 | 721 (73.6%) |
307 (40.7%) |
508 (68.5%) |
|
| Yes | 64.5 ± 7.9 | 34.4 ± 12.1 | 58.5 ± 4.0 | <0.001 | 258 (26.4%) |
447 (59.3%) |
234 (31.5%) |
|
| Surgical Approach | <0.001 | |||||||
| Intravascular | 10.5 ± 1.9 | 6.9 ± 2.9 | 9.5 ± 1.7 | 0.045 | 42 (4.3%) |
90 (11.9%) |
38 (5.1%) |
|
| Minimally Invasive | 87.5 ± 20.3 | 18.8 ± 15.2 | 71.5 ± 10.4 | <0.001 | 350 (35.8%) |
244 (32.4%) |
286 (38.5%) |
|
| Open | 132.0 ± 12.7 | 30.7 ± 14.8 | 96.8 ± 16.5 | <0.001 | 530 (54.1%) |
399 (52.9%) |
387 (52.2%) |
|
| Robotic | 14.2 ± 1.26 | 3.5 ± 2.3 | 7.8 ± 4.4 | <0.001 | 57 (5.8%) |
21 (2.8%) |
31 (4.2%) |
|
| Service | <0.001 | |||||||
| General Surgery | 81.0 ± 11.2 | 24.7 ± 8.4 | 66.2 ± 6.9 | <0.001 | 324 (33.1%) |
321 (42.6%) |
265 (35.7%) |
|
| Orthopedics & Podiatry | 74.2 ± 14.5 | 14.7 ± 9.7 | 51.8 ± 7.3 | <0.001 | 297 (30.3%) |
191 (25.3%) |
207 (27.9%) |
|
| Urology | 23.8 ± 4.2 | 8.7 ± 7.2 | 24.8 ± 7.3 | <0.001 | 95 (9.7%) |
96 (12.7%) |
99 (13.3%) |
|
| Gynecology | 34.0 ± 8.3 | 6.0 ± 5.3 | 18.2 ± 3.9 | <0.001 | 136 (13.9%) |
72 (9.5%) |
73 (9.8%) |
|
| ENT, Plastics, Hand, & Dental Surgery |
27.5 ± 8.3 | 4.0 ± 2.7 | 18.2 ± 5.4 | <0.001 | 110 (11.2%) |
40 (5.3%) |
73 (9.8%) |
|
| Neurosurgery | 4.3 ± 1.7 | 2.8 ± 1.8 | 6.3 ± 1.9 | 0.014 | 17 (1.7%) |
34 (4.5%) |
25 (3.4%) |
|
PRE = pre-shutdown (February 17 - March 15, 2020); ORS = operating room shutdown (March 16 - June 14, 2020); POST = post-shutdown (June 15 - July 12)
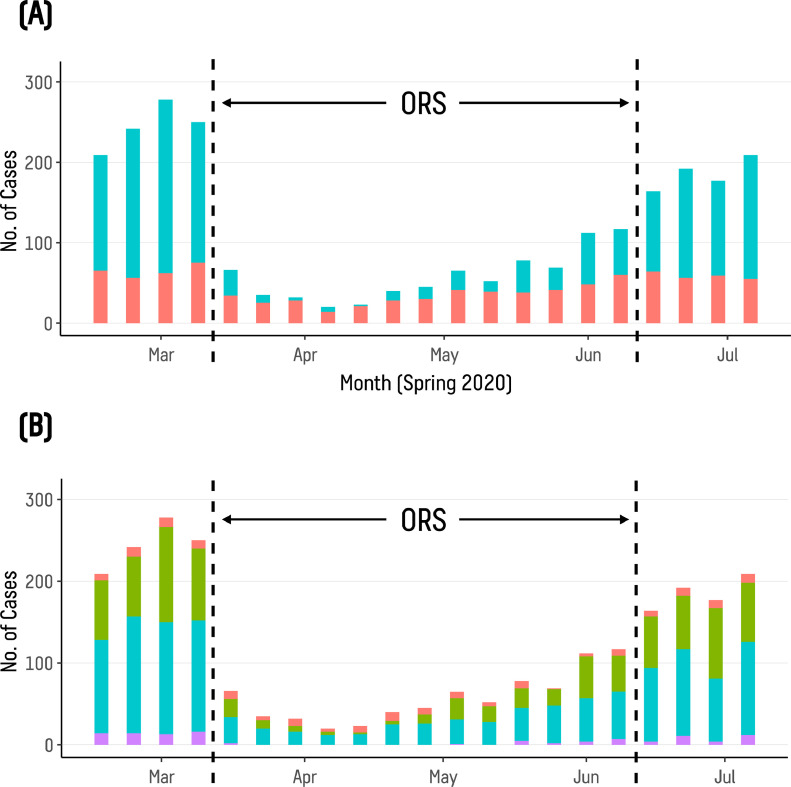
Fig. 2.
Operating room weekly case totals categorized by emergency status (top panel, A) and surgical approach (bottom panel, B). Top panel: non-emergency (blue) versus emergency (red). Bottom panel: intravascular (red) versus minimally invasive (green) versus open (blue) versus robotic (purple). Color version of figure is available online.
Figure 2 (upper panel) depicts the changes in emergency and elective surgeries during the three phases. The most common emergency surgery performed during ORS was insertion of permanent dialysis catheter (53 cases), followed by orthopedic open reductions and internal fixations (42 cases) and appendectomies (28 cases). Case totals for tracheostomies were low overall: 3, 8, and 2 during the PRE, ORS, and POST time periods, respectively. This represented a proportional increase in tracheostomies during ORS, although this result was not significant (0.3% PRE versus 1.1% ORS versus 0.3% POST, p = 0.051).
Open surgeries represented half of all surgeries throughout all three phases and remained relatively constant proportional to caseload (52.2-54.1%, see Table 1; Fig. 2 lower panel). By comparison, intravascular surgeries were proportionally increased during ORS, whereas minimally invasive and robotic surgeries were proportionally decreased (+7.6%, -3.4%, -3.0%, respectively, P < 0.001). As shown in Fig. 2 (lower panel), robotic cases ceased entirely between ORS wk #2-8, resuming at low numbers by ORS wk #9; in spite of this, it was the second-most decreased case-type in terms of average cases per week (14.2 ± 1.26 PRE versus 3.5 ± 2.3 ORS average cases/wk, net decrease 75.4%, P< 0.001).
The surgical approach that saw the steepest decline in utilization was minimally invasive surgery, which decreased from 87.5 ± 20.3 PRE to 18.8 ± 15.2 ORS average cases/wk (net decrease -78.5%, P < 0.001, see Fig. 2 lower panel). When considering emergency cases in isolation, minimally invasive surgeries decreased during the shutdown (30.6% PRE versus 24.4% ORS versus 36.8% POST), with proportional increases in open and intravascular surgeries between the PRE and ORS periods (+2.8% and +5.1%, respectively, P = 0.002).
As shown in Fig. 3 , all services had a significant decrease in average weekly case rates during the shutdown. The services most impacted during this time were the otolaryngology, plastics, and hand surgery services, which combined saw a decrease from 27.5 ± 8.3 PRE to 4.0 ± 2.7 ORS average cases/wk (net decrease -85.5%, P < 0.001). Neurosurgery had the lowest average weekly case rate between all three periods and was also the least affected by the shutdown (4.3 ± 1.7 PRE versus 2.8 ± 1.8 ORS average cases/wk, net decrease -34.9%, P < 0.001).
Fig. 3.
Operating room average case rates per wk (top panel) and percentage of total caseload (bottom panel). Specialties are denoted by color: general/vascular surgery (blue), orthopedics/podiatry (orange), obstetrics/gynecology (purple), otolaryngology/plastics/hand/dental surgery (red), urology (green), and neurosurgery (brown). Color version of figure is available online.
Importantly, general/vascular surgery saw the largest proportional increase of any service during ORS, followed by urology and neurosurgery (+9.5%, +3.0%, +2.8%, respectively, see Fig. 3). In contrast, orthopedics, gynecology, and otolaryngology/plastics/hand surgeries all decreased (-5.0%, -4.4%, -5.9%, respectively, P < 0.001). Nearly all specialties recovered to pre-shutdown levels after the OR was reopened. Changes in emergency status, surgical approach, and surgical service are further detailed in Table 1.
Appendectomies during operative shutdown
As the acute care surgery service was the busiest in all three time periods, we looked at the appendectomy rate both during the operating room shutdown (29/754 cases, 3.8%) and during the observed time frame as a whole (76/2475 cases, 3.1%). Patients more frequently presented with perforated appendicitis during ORS, although this result was not significant (3.7% PRE versus 12.5% ORS versus 0.0% POST, P = 0.132). Occasionally, patients presenting with acute appendicitis were treated nonoperatively with antibiotics, drainage by interventional radiology, or both; however, we noted no significant difference in decision-making for nonoperative management of appendicitis between time periods (7.4% PRE versus 9.4% ORS versus 4.3% POST, P = 0.779). The majority of appendectomies were performed via laparoscopic approach during all three periods (92.6% PRE versus 90.6% ORS versus 95.6% POST, P = 0.957), and complication rates were low overall (all minor surgical site infections, 3.7% PRE versus 6.3% ORS versus 0.0% POST, P = 0.476).
Discussion
The cancellation of elective procedures during the spring 2020 SARS-CoV-2 outbreak in New York City resulted in the expected decrease in operative caseloads across all types of surgery at our institution, allowing for temporary redeployment of resources to critical areas. We show that the operating room services were able to recover quickly after closure, with weekly case volumes reaching pre-COVID levels by 4 weeks after reopening. We observe that not all types of surgery decreased equally during shutdown, and certain case types, operative methodologies, and surgical specialties were more likely to be seen and utilized than others. These results suggest potential strategies for reallocation of operating room resources in crisis scenarios, especially when rapid deployment is a priority.
Since elective procedures were selectively discontinued at our institution, emergency surgeries comprised the majority of cases during the shutdown period. Remarkably, the weekly case rate of actual emergency surgeries was also decreased during this time, for reasons that are unclear. A major component of this decrease in surgeries may have been the citywide lockdown that was put into effect during March 2020 in New York City. By restricting population movement, this policy had the combined effect of discouraging patient presentation at hospitals while reducing the likelihood of traumatic injury requiring surgery. A number of studies from countries with similar lockdown policies during the early stages of the pandemic (e.g., Italy, Spain) report an analogous decrease in both emergency department visits and emergency and/or acute care surgeries during COVID-19 spikes.11, 12, 13 Likewise, in an observational retrospective study of more than 80,000 emergency room visits across a five-hospital system between March 2019 and March 2020, Baugh et al. report a 30.9% reduction in all emergency room visits across nearly all non-COVID-19 conditions.14
A potential consequence of decreased emergency room visitation is delayed diagnosis, which can result in increased complication rates and worse outcomes. In a prospective analysis of 606 patients presenting at a tertiary referral center in Israel during the outset of the COVID-19 pandemic (March-April 2020), Aviran et al. describe a 25% lower admission rate during the pandemic period, with patients taking approximately 1.5 days longer on average to report to the emergency department with symptoms. At the same time, patients reporting during the COVID-19 period were also found to have worse clinical status on presentation, including elevated heart rate, more leukocyte disturbances, higher creatinine levels, and higher CRP levels, with a greater proportion of patients ultimately requiring urgent surgery (39.0% versus 27.4%, P = 0.03).15 A similar retrospective analysis of multiple emergency surgeries at a single Italian referral center by D'Urbano et al. suggests that patients requiring emergency surgery during a pandemic lockdown are not only less likely to present at the emergency department (-41.3% between March 2019 and March 2020), but are also more likely to experience postoperative complications (55.6% versus 36.9%), regardless of SARS-CoV-2+ status.16 Put in context, our subgroup analysis of patients presenting with acute appendicitis during shutdown demonstrated a similar higher incidence of perforated appendicitis and post-appendectomy complications compared to those admitted during non-COVID periods, although these findings were not statistically significant. Moreover, despite the increased severity of appendicitis presentation at our institution during shutdown, the overall frequency of appendicitis decreased during this period, and there were no instances of readmission for cases treated with nonsurgical techniques. This trend may suggest a larger role for nonoperative management of appendicitis during crisis situations, which may further apply to other common surgical illnesses in these scenarios.
We observed a shift away from minimally invasive and robotic approaches in favor of open surgeries during operating room shutdown, particularly for emergency cases. This practice was in accordance with early literature regarding surgical best-practices during the COVID-19 pandemic, which cited several benefits of open procedures, including shorter operative durations, lower resourcerequirements, and decreased need for specialized personnel.5 , 17 , 18 Moreover, minimally invasive surgeries such as laparoscopy were avoided by staff for fear of elevated SARS-CoV-2 transmission risk via use of compressed gas and subsequent viral aerosolization.19 Further decreases in rates of laparoscopic surgery were attributable to logistical issues, in which cases were delayed or deferred while additional equipment was purchased to filter pneumoperitoneum.
In the time since these initial studies, there has been increasing evidence that minimally invasive approaches can be performed safely in a pandemic scenario and should be used if they conform to standard of care (e.g., laparoscopic cholecystectomy)20 , 21 Robotic surgeries are similarly safe in the COVID-19 environment, although they are still resource-intensive.22 In our subgroup analysis of appendectomies during the pandemic, the majority of patients underwent laparoscopic appendectomy during all three time periods without significant difference (P = 0.957), and differences in operative management were not associated with any change in clinical outcomes. Moreover, we did not observe any SARS-CoV-2 conversions from laparoscopic procedures.
Most importantly, we observed that general and vascular surgery were the most active surgical services during all three phases of the study, while orthopedic surgery was the second-most active surgical service. However, while general and vascular surgery subsumed a greater proportion of overall caseload during shutdown (+9.5%), orthopedic surgery comprised proportionally fewer cases during this period (-5.0%), even though open reduction internal fixation procedures remained the most common type of surgery during all three time periods. In practice, the reason for this dynamic was the loss of elective total knee replacements and arthroscopies during shutdown, which eliminated a significant portion of orthopedic caseloads; common general surgery procedures such as appendectomies and cholecystectomies remained relatively constant throughout all three time periods. In keeping with this trend, specialties such as ENT, plastics, and hand surgery experienced a significant decrease in activity during the shutdown, likely owing to a higher proportion of their patient volume requiring elective procedures. These findings align with what has been described in COVID-19 shutdown guidelines, and specialists from less busy services can be reassigned to roles befitting their expertise, depending on hospital needs.4 , 5
In addition to shifts in caseloads, financial factors also played a role in our hospital's resource management during the COVID-19 surge. Unsurprisingly, cancellation of elective surgeries and outpatient clinics led to significant revenue loss, especially within the orthopedics, neurosurgical, ENT, plastics, and hand surgery services. Concurrently, however, significant increases in complex intensive care patients resulted in unforeseen increases in income, particularly at the peak of the surge when the intubated patient count of our hospital more than quadrupled. The net result was an elevation of case mix index (CMI) at our institution during spring 2020, although financial losses were still substantial during this time. Accordingly, several studies addressing the economic burden of COVID-19 at the hospital level report similar decreases in hospital revenue on the U.S. East Coast during spring 2020, with rural and low-resource hospitals most severely affected.23 , 24
This study has several limitations. In an effort to showcase the dynamic of surgical management over the course of the COVID-19 operating room shutdown, time periods representing roughly equal caseloads before, during, and after the shutdown were selected and findings were normalized to average cases per week for fair comparison (see Methods). Since these time frames are inherently unequal with arbitrary cutoff dates, they are subject to some degree of selection bias. Moreover, multiple surgical subspecialties were categorized into six major groups for clarity of analysis, which may have caused some loss of resolution among certain findings. Finally, while subgroup analysis was performed for acute appendicitis at our institution, other common procedures were not analyzed; this was done for comparison with other institutions and because acute appendicitis is the most common general surgical emergency worldwide.25, 26, 27
Conclusion
In conclusion, this study highlights the changes in surgical caseloads after complete cessation of elective surgeries during the early days of the SARS-CoV-2 pandemic in New York City. During this shutdown, weekly case rates dropped among all types of surgery, including emergency surgery. General and vascular surgery became the predominant surgical services during this time, with orthopedic surgeries diminished but remaining second-most common. Furthermore, open surgeries were favored over minimally invasive surgeries throughout the shutdown period. As a result, while decreased overall caseloads may allow for some redistribution of surgical resources and personnel to critical care units, it is important to maintain active, rapid-response general surgery and orthopedic services to treat emergencies, which comprise the bulk of surgeries during operating room shutdown. This reallocation of resources may be useful for future lockdown or crisis planning among community hospitals.
Acknowledgments
Acknowledgment
PHM and MEZ developed the study concept and design. All authors participated in data acquisition. PHM and OC performed the analysis of the data. PHM, OC, and JH wrote the manuscript. RL and MEZ provided critical revision and review of the manuscript. All authors reviewed and gave final approval of the manuscript before submission.
Disclosure
PHM, OC, JH, JGH, ACW, RL, and MEZ have no related conflicts of interest to declare. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Financial Disclosure
None of the authors assume any financial interest. No external funding was obtained for this study.
Author Contributions
PHM and MEZ developed the study concept and design. All authors participated in data acquisition. PHM and OC performed the analysis of the data. PHM, OC, and JH wrote the manuscript. RL and MEZ provided critical revision and review of the manuscript. All authors reviewed and gave final approval of the manuscript before submission.
References
- 1.Knisely A. Perioperative Morbidity and Mortality of Patients With COVID-19 Who Undergo Urgent and Emergent Surgical Procedures. Ann. Surg. 2021;273(1):34–40. doi: 10.1097/SLA.0000000000004420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nahshon C., Bitterman A., Haddad R., Hazzan D., Lavie O. Hazardous postoperative outcomes of unexpected COVID-19 infected patients: a call for global consideration of sampling all asymptomatic patients before surgical treatment. World J. Surg. 2020;44:2477–2481. doi: 10.1007/s00268-020-05575-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coccolini F. Surgery in COVID-19 patients: operational directives. World J. Emerg. Surg. 2020;15:25. doi: 10.1186/s13017-020-00307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. CDC Interim Guidance for Healthcare Facilities: Preparing for Community Transmission of COVID-19 in the United States. (2020).
- 5.American College of Surgeons. Guidelines for Triage and Management of Elective Cancer Surgery Cases during the Acute and Recovery Phases of Coronavirus Disease 2019 (COVID-19) Pandemic. 1-45 (2020).
- 6.Moletta L. International guidelines and recommendations for surgery during Covid-19 pandemic: a Systematic Review. Int. J. Surg. 2020;79:180–188. doi: 10.1016/j.ijsu.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.New York City Department of Health and Mental Hygiene. NYC Coronavirus Disease 2019 (COVID-19) Data. https://github.com/nychealth/coronavirus-data (2020).
- 8.Thompson C.N. COVID-19 outbreak — New York City, February 29-June 1, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1725–1729. doi: 10.15585/mmwr.mm6946a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CDC COVID-19 Response Team Geographic differences in COVID-19 cases, deaths, and incidence — United States. MMWR Morb. Mortal. Wkly. Rep. 2020;69:465–471. doi: 10.15585/mmwr.mm6915e4. February 12-April 7, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Axiotakis, L.G., Risk of acquiring perioperative COVID-19 during the initial pandemic peak: a retrospective cohort study. Ann. Surg.Publish Ahead of Print, (2020). [DOI] [PMC free article] [PubMed]
- 11.Martellucci J. Emergency surgery in the time of Coronavirus: the pandemic effect. Minerva Chir. 2020 doi: 10.23736/S0026-4733.20.08545-4. [DOI] [PubMed] [Google Scholar]
- 12.Patriti A., Baiocchi G.L., Catena F., Marini P., Catarci M. Emergency general surgery in Italy during the COVID-19 outbreak: first survey from the real life. World J. Emerg. Surg. 2020;15:36. doi: 10.1186/s13017-020-00314-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cano-Valderrama O. Acute Care Surgery during the COVID-19 pandemic in Spain: changes in volume, causes and complications. A multicentre retrospective cohort study. Int. J. Surg. 2020;80:157–161. doi: 10.1016/j.ijsu.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baugh, J. J., The cases not seen: Patterns of emergency department visits and procedures in the era of COVID-19. Am. J. Emerg. Med. S0735675720309645 (2020) doi: 10.1016/j.ajem.2020.10.081. [DOI] [PMC free article] [PubMed]
- 15.Aviran E. The Impact of the COVID-19 pandemic on general surgery acute admissions and urgent operations: a comparative prospective study. Isr. Med. Assoc. J. IMAJ. 2020;11:673–679. [PubMed] [Google Scholar]
- 16.D'Urbano, F., Fabbri, N., Radica, M. K., Rossin, E., Carcoforo, P. Emergency surgery in COVID-19 outbreak: has anything changed? Single center experience. World J. Clin. Cases8, 3691-3696 (2020). [DOI] [PMC free article] [PubMed]
- 17.Zheng M.H., Boni L., Fingerhut A. minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann. Surg. 2020;272:5–6. doi: 10.1097/SLA.0000000000003924. Available at: https://journals.lww.com/annalsofsurgery/Fulltext/2020/07000/Minimally_Invasive_Surgery_and_the_Novel.4.aspx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pryor, A., SAGES and EAES Recommendations Regarding Surgical Response to COVID-19 Crisis. (2020).
- 19.De Simone B. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann. R. Coll. Surg. Engl. 2020;102:323–332. doi: 10.1308/rcsann.2020.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Leeuw R.A. COVID-19 and laparoscopic surgery: scoping review of current literature and local expertise. JMIR Public Health Surveill. 2020;6:e18928. doi: 10.2196/18928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El Boghdady, M., Ewalds-Kvist, B. M., Laparoscopic Surgery and the debate on its safety during COVID-19 pandemic: A systematic review of recommendations. The SurgeonS1479666×20301049 (2020) doi: 10.1016/j.surge.2020.07.005. [DOI] [PMC free article] [PubMed]
- 22.Porter J. Society of robotic surgery review: recommendations regarding the risk of COVID-19 transmission during minimally invasive surgery: COVID-19 transmission during minimally invasive surgery. BJU Int. 2020;126:225–234. doi: 10.1111/bju.15105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323:2127–2128. doi: 10.1001/jama.2020.6269. [DOI] [PubMed] [Google Scholar]
- 24.Levy JF, Ippolito BN, Jain A. Hospital revenue under maryland's total cost of care model during the COVID-19 pandemic. JAMA. 2021;325(4):398–400. doi: 10.1001/jama.2020.22149. March-July 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Javanmard-Emamghissi H. The management of adult appendicitis during the COVID-19 pandemic: an interim analysis of a UK cohort study. Tech. Coloproctology. 2020 doi: 10.1007/s10151-020-02297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kumaira Fonseca M., Trindade E.N., Costa Filho O.P., Nácul M.P., Seabra A.P. Impact of COVID-19 outbreak on the emergency presentation of acute appendicitis. Am. Surg. 2020;86:1508–1512. doi: 10.1177/0003134820972098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou Y., Cen L.-S. Managing acute appendicitis during the COVID-19 pandemic in Jiaxing. World J. Clin. Cases. 2020;8:4349–4359. doi: 10.12998/wjcc.v8.i19.4349. China. [DOI] [PMC free article] [PubMed] [Google Scholar]