Abstract
Background
While all resources have been mobilized to fight COVID-19, this study aimed to analyze the consequences of lockdown and pandemic stress in participants with and without Irritable Bowel Syndrome (IBS).
Methodology
An online survey was proposed to people with or without IBS during the exponential phase of the pandemic in France. The questionnaire included questions about socio-demographic data, conditions of confinement, activities carried out, IBS characteristics, measurement of stress level, consequences on sleep, fatigue, anxiety and depression, and quality of life (both perceived non-specific and specific for IBS).
Results/Discussion
From March 31 to April 15, 2020, 304 participants, 232 with IBS and 72 without were included in the survey (mean age: 46.8 ± 16.8 years, female gender: 75.3%). Age, level of education, financial resources, living space per person and activities performed during confinement were identical in both groups. Stress linked to fear of COVID-19, lockdown and financial worries was at the same level in both groups, but the psychological consequences and deterioration of quality of life (QOL) were both higher in IBS participants. In a univariate analysis, teleworking, solitary confinement, and low household resources had a variable impact on the scores of depression, anxiety, fatigue and non-specific perceived QOL, but in a multivariate analysis, the only factor explaining a deterioration of non-specific QOL was the fact of suffering from IBS.
Conclusion/Perspectives
Stress linked to the COVID-19 pandemic and confinement is high and equivalent in both IBS and non-IBS participants, with higher psychological and QOL consequences in IBS patients who have altered coping capacities.
Keywords: COVID-19, Irritable bowel syndrome, Pandemic, Quality of life, Stress
Introduction
On January 1, 2020, the World Health Organisation (WHO) declared an alert for a new infection with SARS-CoV-2 coronavirus. This virus originated in the city of Wuhan in China, and had caused numerous deaths from pneumonia and acute respiratory distress syndrome [1]. When the disease arrived in France, hospitals and health facilities cancelled all non-emergency programmed activities, in order to mobilize all resources against the COVID-19 pandemic; outpatient visits were also cancelled and people were urged to use online consultation services where possible. On March 14th, schools were closed in France and on March 16th, the French authorities announced a generalized lockdown because of an uncontrollable situation in the Grand Est and Île-de-France regions. This lockdown aimed at prohibiting outings except for healthcare professionals and essential professions such as road transport, food stores, and police. Working from home was strongly recommended for all other professions. For the general population, a limited number of reasons for going outside was authorized (work, if working from home was not possible, food shopping, the solitary practice of limited physical activity or exercising pets), with an obligation to present a certificate in the event of a police check.
The COVID-19 pandemic and the associated confinement represents a multidimensional stress [2]. The pandemic itself is a major source of stress due to fear of illness or death for oneself and for loved ones [2]. This stress is linked to messages conveyed by the media and can be enhanced by contradictory messages given by the health authorities [3], [4], in particular concerning the need for and availability of personal protective equipment, both for healthcare professionals and for the general population. The second dimension of this stress is linked to the deprivation of liberties caused by the lockdown and could be influenced by conditions of confinement. The last factor is due to financial fears with immediate consequences such as loss of income, but also by the announcement of an unprecedented economic crisis due to the organized paralysis of the country.
Due to a very significant mobilization of resources for COVID-19, other diseases have been left behind with risks of worsening [5]. Recently, alerts have been given on the psychological risks of confinement during the pandemic in patients with chronic disease and in healthy subjects [6], [7], with the possibility of developing post-traumatic stress [2], [8], [9]. IBS is the most frequent chronic digestive disorder, affecting 5 to 10% of the general population, associating abdominal pain and transit disorders [10]. Although not life-threatening, it can be associated, depending on its severity, with an impairment in quality of life of the same magnitude as diabetes mellitus, depression, and dialysis-dependent end-stage renal disease [11]. The link between stress and IBS has already been described, both for the onset of the disease or for the worsening of symptoms [10], [12].
Therefore, we designed an online survey to study the psychological consequences and effects on quality of life of multidimensional stress related to the COVID-19 pandemic and lockdown in participants with and without IBS.
Methods
On March 31, after 15 days of lockdown, in the exponential phase of the pandemic in France with around 40,000 infected people, 500 daily deaths and a total of 3500 deaths, an online survey was proposed by the French association of patients suffering from IBS (Association des patients souffrant du syndrome de l’intestin irritable, APSSII) to his members. Participants without IBS were also recruited among relatives and friends of some authors of this paper (J.-M. Sabate, A. Entremont, P. Jouet) and among friends of IBS participants. The patient's questionnaire was validated by members of the APSSII, members of the scientific committee and the non-IBS questionnaire by members of scientific committee and subjects without IBS. An invitation to fill an online questionnaire was sent by mail in accordance with GDPR (general data protection regulations) and with the French Data Protection Authority (Commission nationale de l’informatique et des libertés). Privacy of subject information was ensured by password-protected access to the data collection forms, the online response database did not contain any information that could reveal the identity of individual subjects, and was stored on a secured Internet server. No compensation was given for participation in the study.
Common questionnaire for participants with and without IBS
The questionnaire described:
-
•
subjects’ characteristics (age, gender, level of education, monthly household income, profession);
-
•
conditions of lockdown (in a town or in the countryside, type and size of housing, room to isolate oneself, number of other people confined and relation to the subject, presence of children and method of education if continued, conditions of work (outings, working from home or cessation of professional activity) and activities carried out including physical activity classified in 4 categories (none, weak = sport activity (≥ 30 minutes) once a week, less than 30 minutes of walking per day; intermediate: sport activity 2 to 3 times per week, walking ≥ 30 min per day; high: sports activity ≥ 4 times per week;
-
•
personal experiences with the pandemic, overall level of stress, perceived stress dimensions (fear of COVID-19, stress related to lockdown, fear in relation to financial uncertainty, 0–100, 100 being the higher level of stress) and consequences of lockdown with the measurement of fatigue score (9 questions) [13], a validated depression and anxiety score (HAD scale, 14 questions) [14], sleep disturbance and perceived non-specific QOL assessed in one single question (“please indicate to what extent your quality of life is currently disrupted”; 0–100, 100 being the worst QOL).
Specific questions for participants with IBS
Disease duration, transit subtypes, IBS care pathway, IBS severity (IBS-SSS, from 0 to 500; in remission if < 75, minimal from 75 to 175, moderate from 175 to 300 and severe if > 300) [15], and specific IBS quality of life (IBS-QOL, varying from 0 to 100, 100 being the best QOL) [16] were recorded. Patients were also asked if symptoms or care were modified.
Statistical analysis
The number of patients to be included in this study was not calculated, it was decided to include as much participants with and without IBS as we could during a short period (15 days) of the study to avoid having a change in stress and lockdown conditions. Baseline demographics and relevant clinical information were calculated and compared between participants with and without IBS. Means and standard deviations were calculated for continuous variables and comparisons were performed using t-tests and ANOVA. Frequencies were calculated for categorical variables, and comparisons were performed using χ2 tests. Correlations between variables were made using the Pearson correlation test. A multivariate analysis using multiple regression analysis for non-specific perceived QOL was performed including baseline variables that reached a univariate P-value < 0.10. In all cases, P < 0.05 was considered significant. All statistical analyses were carried out with SPSS software, version 25.0 (IBM, New-York, US).
Results
Characteristics and lockdown conditions of participants with and without IBS
Between March 31 and April 15, 304 participants responded anonymously to the online survey: among the 794 members of the association, 232 (36.8% of the whole group) of the 629 people with IBS who had given their prior agreement to be contacted for online studies participated; of the 95 people without IBS contacted among friends of members of the association and of the main authors of the article (JMS, AE, PJ), 72 (84%) agreed to participate. The characteristics of the participants are given in Table 1 . Mean age of the whole group was 46.8 ± 16.8 years, and 75.3% were of female gender. The percentage of participants with a monthly household income < 2000 euros did not differ between the two groups (39.8% of IBS vs. 28.8 of non-IBS participants, P = 0.145). The percentage of participants living alone during lockdown was 30.9% in the IBS group and 19.4% in the non-IBS group (P = 0.067).
Table 1.
Socio-demographic characteristics of the participants and lockdown conditions.
| Characteristic | IBS group (n = 232) | Non-IBS (n = 72) |
|---|---|---|
| Median age (IQR) – yr | 45.4 (31.6–63.4) | 40.0 (31.2–54.7) |
| Female sex–no. (%) | 181 (78) | 48 (66.6) |
| Healthcare professional – % | 11 (4.74) | 15 (20.8) |
| Other disease than IBS at risk for COVID-19 - % | 5.6/0.8/2.6/1.3 | 2.7/1.3/0.5/0.5 |
| Hypertension/diabetes/obesity/othersa | ||
| Educational level – % | ||
| Middle school | 5.2 | 6.9 |
| High school | 10.3 | 5.6 |
| Graduate and postgraduate education | 84.5 | 87.5 |
| Student/active employment/retired – % | 3.9/56/26.7 | 8.3/75/12.5 |
| Household monthly income – % | ||
| < 1000 euros | 6 | 5.6 |
| Between 1000–2000 euros | 29.3 | 15.5 |
| Between 2000–3000 euros | 32.8 | 23.9 |
| Between 3000–5000 euros | 20.7 | 28.2 |
| > 5000 euros | 11.2 | 26.8 |
| Lockdown characteristic – % | ||
|---|---|---|
| In a town/the countryside – % | 65.2/34.8 | 79.1/20.9 |
| House %/apartment % | 50.7/49.3 | 62.7/37.3 |
| Presence of garden – % | 50.9 | 38.8 |
| Possibility of a room to isolate oneself – % | 95.4 | 86.5 |
| Number of people confined (mean ± sem) | 2.14 ± 21.3 | 2.5 ± 1.1 |
| % with children (under 18 years old) | 23.2 | 36.1 |
| Median whole size of the house (m2, IQR) | 85 (55.5–110) | 77 (60–130) |
| mean living space/person (m2) | 48.9 ± 27.5 | 44.8 ± 33.9 |
| % with pet | 15.8 | 17.9 |
Mean values are given with the SEM or median with interquartile range.There were no significant differences (P < 0.05) between the study groups except for Female Sex (P = 0.007), for health care professional (P < 0.001), for employment categories (P < 0.0001), for people confined to a town or the countryside (P = 0.031), for the presence of a garden (P = 0.038), for the possibility of a room to isolate (P = 0.022) and for people with children under 18 (P = 0.03).
Others: chronic obstructive pulmonary disease, cardiovascular problems.
The initial diagnosis of IBS was made by a physician in 90% of cases, and 82% had undergone a normal colonoscopy; 63.4% of IBS participants were followed up (by a general practitioner in 23.1% of cases, a gastroenterologist in 69.4%, or another specialist in 7.5%); among them, 72% had consulted in the previous 12 months. Mean disease duration was 9.7 ± 0.8 years and the proportion of the different IBS subtypes (IBS-C 28%; IBS-D: 30.2%; IBS-M: 41.2%) was no different between women and men (P = 0.321). Mean IBS-SSS score was 274.8 ± 103.0, not influenced by gender or transit pattern and was not correlated with disease duration (r = 0.06; P = 0.359). IBS was severe according to IBS-SSS in 46.2%, moderate in 32.8%, minimal in 17.2% and in remission in 3.4%.
Activities carried out during lockdown
Activities during the lockdown period are presented in Table 2 . They were globally similar in both groups. Education was continued for at least one child in two, carried out in about 2/3 of the cases by the participants, and was provided in school within the authorized framework for children of healthcare professionals.
Table 2.
Activities carried out during lockdown.
| IBS group (n = 232) | Non-IBS (n = 72) | P-value | |
|---|---|---|---|
| Working from home | 39.4 | 45.4 | 0.385 |
| Education during lockdowna – % | 49.4 | 70.0 | 0.053 |
| by family/online/at school | 65/85/0 | 61.9/66.6/4.7 | |
| Level of physical activity – % | 16.5/39.2/26.6/17.7 | 14.9/29.8/34.0/21.3 | 0.596 |
| None/Weak/Intermediate/High |
| % of global activities (0–100) | |||
|---|---|---|---|
| Outside for buying food | 54.1 ± 34.3 | 55.4 ± 30.9 | 0.282 |
| Outside for physical exercise | 36.4 ± 34.5 | 41.1 ± 34.9 | 0.307 |
| Taking out pets | 8.3 ± 23.1 | 8.56 ± 22.3 | 0.929 |
| Reading books | 52.5 ± 26.5 | 44.3 ± 29.6 | 0.044 |
| Watching tv series or movies | 58.31 ± 26.3 | 59.8 ± 24.9 | 0.680 |
| Social networking | 54.9 ± 29.4 | 56.86 ± 28.3 | 0.282 |
If children < 18 years old.
Before lockdown, physical activity was identical between participants with and without IBS (P = 0.18), 54.6% and 54.5% respectively having intermediate physical activity. The percentage of participants with a change in physical activity during lockdown was the same in the two groups (68.1% with IBS vs.65.3% in without IBS; P = 0.774). In less than 10% of participants, this change corresponded to a shift towards the group of high physical activity; for the majority of cases, there was a shift from a group with intermediate activity towards a group with weak activity or none.
Experiences with COVID-19, perceived stress during lockdown and pandemic and consequences
Personal experiences with COVID-19 are presented in Table 3 , and were similar in the two groups. There was a trend for a higher overall level of stress in the group of participants with IBS, but the increase in stress related to lockdown was of the same order. The three dimensions of stress linked to the pandemic (fear of COVID-19 infection, lockdown, financial difficulties) were similar in the two groups. Participants with IBS thought they were more at risk for SARS-CoV-2 infection in 26.8% of cases and for a more severe form of the disease in 20.4%.
Table 3.
Experiences with COVID-19, perceived stress during lockdown and consequences.
| IBS group (n = 232) | Non-IBS (n = 72) | P-value | |
|---|---|---|---|
| Experiences with SARS-CoV-2 -% | |||
| Cases of COVID-19 infection in the immediate environment | 24.5 | 30.3 | 0.349 |
| Existence of symptoms possibly related to COVID-19 | 20.37 | 28.8 | 0.151 |
| Desire to be tested for COVID-19a | 62.3 | 50.8 | 0.103 |
| Perceived stress (0–100) | |||
| Global perceived stress | 49.0 ± 25.6 | 41.8 ± 27.6 | 0.053 |
| % with increase since lockdown | 52.7 | 43.9 | 0.42 |
| Stress linked to IBS | 46.5 ± 33.5 | – | |
| Fear of being infected by COVID-19 or of infecting loved ones and family | 46.0 ± 34.5 | 40.3 ± 33.2 | 0.231 |
| Lockdown stress | 38.2 ± 33.0 | 35.2 ± 33.4 | 0.530 |
| Fear of financial difficulties | 22.6 ± 29.6 | 22.6 ± 29.7 | 0.994 |
| Consequences | |||
| Anxiety component (HAD score) | 10.6 ± 3.9 | 6.9 ± 3.6 | < 0.001 |
| Depression component (HAD score) | 7.13 ± 3.85 | 4.8 ± 3.7 | < 0.001 |
| Global HAD score | 17.8 ± 6.5 | 11.8 ± 6.5 | < 0.001 |
| Fatigue Score (0–7) | 4.90 ± 1.5 | 3.59 ± 1.6 | < 0.001 |
| Sleep disturbances – % | 61.5 | 53 | 0.216 |
| New sleep disturbance | 12.0 | 9.1 | 0.206 |
| Increase in sleep disturbance | 27.7 | 13.6 | 0.038 |
| Mean IBS-QOL (0–100) | 47.6 ± 19.9 | – | |
| Mean non-specific perceived QOL (0–100) | 77.8 ± 16.8 | 52.2 ± 27.2 | < 0.001 |
Mean values are given with the standard deviation or median with interquartile range.
PCR for SARS-CoV-2 was performed in 4 IBS participants (positive in 2) and in 3 non-IBS subject (positive in 1).
The consequences in terms of anxiety, depression, fatigue, increase in sleep disorders, and perceived QOL were significantly higher in participants with IBS compared to those without IBS. More participants with IBS than without IBS had significant anxiety (HAD-A > 10, 52.6% vs.16.4%; P < 0.001) and severe depression (global HAD > 19, 37.9% vs. 12%; P < 0.001); 20.6% of participants with IBS were treated with anxiolytics and 20.6% with antidepressants, whereas those without IBS took anxiolytics in only 5.8% and antidepressants in 7.3%.
In all participants, female gender was associated with a higher overall stress level (49.1 ± 26.0 vs.41.9 ± 26.2; P = 0.045), HAD anxiety score (10.3 ± 4.0 vs.8.3 ± 4.2; P < 0.001), similar HAD depression score (6.6 ± 3.8 vs.6.6 ± 4.3; P = 0.907), with a higher fatigue score (4.7 ± 1.5 vs.4.2 ± 1.7; P = 0.019), and with a trend for a more impaired non-specific QOL (74.9 ± 20.1 vs.69.2 ± 24.0; P = 0.09). In participants with IBS, women had a higher HAD anxiety score than men (10.9 ± 3.82 vs.9.56 ± 4.0; P = 0.027).
In all participants, overall level of stress was correlated with had anxiety score (r = 0.572, P < 0.001), HAD depression score (r = 0.357, P < 0.001), global HAD score (r = 0.539, P < 0.001), non-specific perceived QOL (r = 0.303, P < 0.001) and with IBS-QOL in participants with IBS (r = 0.317, P < 0.001).
Non-specific perceived QOL was correlated in participants without IBS with a HAD score (r = 0.586, P < 0.001) and fatigue score (r = 0.583, P < 0.001) and in participants with IBS with HAD scores (r = 0.330, P < 0.001), fatigue score (r = 0.366, P < 0.001) and IBS-QOL (r = 0.564, P = 0.001).
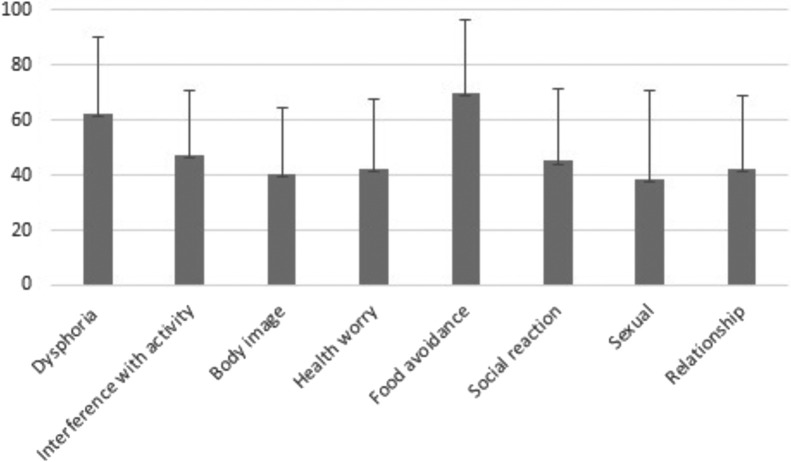
IBS-QOL was altered in each dimension (Fig. 1 ), no more in women than in men (48.3 ± 20.4 vs. 45.3 ± 18.0; respectively, P = 0.34), it was correlated with IBS-SSS (r = 0541; P < 0.001), global HAD score (r = 0.545; P < 0.001), HAD anxiety and depression sub-scores and with fatigue score (r = 0.484, P < 0.001). IBS-SSS score was correlated with a global HAD score (r = 0.337; P < 0.001), HAD sub-scores, and with fatigue score (r = 0.346; P < 0.001).
Figure 1.
IBS-QOL domains in participants with IBS (n = 232) during COVID-19 pandemic and lockdown (mean and standard deviations). (IBS-QOL varies from 0 to 100, 100 considered as the best quality of life).
Impact of lockdown characteristics on pandemic consequences
In all participants, living in a town vs. the countryside, in an apartment vs. a house, with vs.without a garden, having a room to isolate oneself, the whole area of the house, living space per person, and having a pet, did not influence HAD score or sub-scores, fatigue score or non-specific QOL. In all participants, living alone was not associated with different global HAD scores, HAD sub-scores, and fatigue scores, but was associated with a trend for more impaired perceived non-specific QOL (77.1 ± 18.5 vs.71.6 ± 22.2; P = 0.057). Working from home was associated with a trend for lower global HAD score (15.6 ± 7.2 vs.17.0 ± 6.8; P = 0.110) with no effect on a HAD anxiety score (9.6 ± 4.2 vs.9.9 ± 4.0; P = 0.46) but with a lower HAD depression score (6.0 ± 3.8 vs.7.0 ± 4.0; P = 0.039), and a trend for a better non-specific perceived QOL (70.1 ± 24.2 vs.75.2 ± 19.2; P = 0.058). Monthly income per household < 2000 euros was associated with a higher HAD global score (18.5 ± 6.9 vs.15.9 ± 6.9; P = 0.003), a higher HAD anxiety score (10.9 ± 4.1 vs.9.6 ± 4.0; P = 0.019), HAD depression score (7.6 ± 4.2 vs.6.2 ± 3.8; P = 0.006), fatigue score (5.0 ± 1.5 vs.4.5 ± 1.6; P = 0.019), and impairment of non-specific QOL (78.1 ± 19.3 vs.72.1 ± 21.6; P = 0.028). In a multiple linear regression analysis of non-specific perceived QOL in the whole group, only the type of participant (with IBS or without IBS) was an explanatory factor (Beta = −0.424, P < 0.001; CI [−26.8; −15.4], whereas gender, working from home, living alone and household monthly income were not.
Impact of the pandemic and lockdown on IBS symptoms and care
Participants with IBS considered that their disease was modified in 41.2%, with worsening of symptoms in 19.9% and improvement in 21.3%. Among those in whom the disease was modified, worsening/improvement was noted for abdominal pain in 40.9%/35.9%, for bloating in 39.3%/27.0% and for transit disorders in 37.0%/34.8%. The medical follow-up was modified in 23.6%, with cancellation of a consultation by the doctor in 58.8% and by the patient himself in 37.2%, for fear of going to the doctor. Online consultations were performed in 29.4%. The therapeutic management of IBS was modified in 24.5% (data not shown). Anxiolytic treatment in participants with IBS remained stable in 71.6%, increased in 10.4%, decreased or stopped in 16.6%. Antidepressant treatment in participants with IBS remained stable in 79.2%, was increased or initiated in 4% and decreased or stopped in 5%. Diet was modified in 48.6% of participants with IBS and in 45.4% of those without IBS, due to supply difficulties in 31% and 20%, respectively. In participants with IBS, the change in diet consisted of a better adaptation to IBS in 47.1% with more time to cook in 78% of participants (especially for low FODMAPs diet).
Discussion
In this online survey carried out in France during lockdown and the COVID-19 pandemic, on participants with and without IBS, we have shown that these groups shared similarly high level of stress of a multidimensional nature, but had differential effects in terms of psychological consequences and deterioration of QOL.
There was a trend for a higher overall stress level in participants with IBS compared with those without IBS. This could be explained by the additional stress caused by their disease, patients also believing that IBS was a risk factor for infection and for a more severe form of COVID-19. However, the different dimensions of stress in the two groups since lockdown were at the same level, and as in China and in the USA the fear of being infected or infecting loved ones was the primary concern [17], [18]. Indeed, in both groups, the threat was present because participants often knew people who had been infected, thought they themselves had symptoms of COVID-19 (in more than 20%), and over 50% wanted to be tested for the virus. Lockdown was the second concern, far ahead of financial fears. It has already been described in similar circumstances that the loss of usual routine and of social contact can cause boredom, frustration and sense of isolation [2], [19]. The lesser impact of financial considerations could be explained by the generous financial aid from the French government, and because the global context of the economic crisis was less obvious due to a delay in pandemic consequences for the UK and for the USA. In a recent American study, fears of job loss and income, although less frequent than fears related to COVID-19 and confinement were among the most stressful [17].
Although this multidimensional stress was similarly high in both groups, its consequences in terms of anxiety, depression, increase in sleep disturbance, fatigue and non-specific QOL impairment were greater in participants with IBS. Several hypotheses can explain these differences. The pre-existence of anxiety and depression before lockdown in some participants with IBS, which is usual in IBS studies [10], [20], could explain higher HAD scores and greater impact of stress on QOL as it was shown recently during COVID-19 pandemic in psychiatric patients having anxiety and depressive disorders [21]. The negative effects of stress and anxiety on the sleep disorders during the COVID-19 pandemic has been recently reported in China in healthy subjects [22] and an increase in sleep disturbance as we found in patients with IBS is known to have an impact on pain, distress and QOL [23].
Coping capacities [2] and stress resilience [24] are important factors in resisting major pandemic stress, as already shown for the H1N1 pandemic threat [25], [26]. Coping capacities are important for managing illness in multiple chronic conditions such as diabetes, hypertension, depression [27]. They can be impaired in IBS, as we have previously shown with the French patients’ organization using a different QOL score which assessed coping capacities [20]. This could explain more severe consequences of pandemic and lockdown in these participants with IBS. Altered coping strategies are associated with higher severity of IBS, anxiety and depression and poorer QOL [28], [29]. However, it has been described during COVID-19 pandemic that coping strategies could be also altered even in healthy people [30].
Activities carried out at home (reading, cooking, listening to music, watching television or films, using social networks…) and teleworking which can be considered as coping strategies [31] were not different between the two groups with the exception of teaching for children or reading activities but may not have produce the same effects in patients with IBS and in subjects without IBS. The increase in sleep disturbances that is necessary for a good adaptation to stress [32] was more common in patients. Other factors may be important, such as a decrease in the social support and relationships that are crucial to patients with IBS and that were altered due to confinement [33], [34].
Although lower than in participants with IBS, the consequences of the COVID-19 pandemic and lockdown in participants without IBS were significant and comparable to those described in China, where more than 50% of cases suffered a psychological impact, 16% a moderate to severe depression and 28% of moderate to severe anxiety [18]. A recent study has shown that the level of stress and depression was different depending on the country during lockdown and COVID-19 pandemic [31]. This could be linked to the conditions of lockdown or to the severity of the pandemic which differed depending on the country but also to prevention messages disseminated by the media for the public to put in place coping strategies. Thus, while the United States was the most affected country, it is remarkable that in this study the level of stress and depression was lower than that of India [31]. In France, during the first wave and during the period of this study, no prevention message for coping strategies was broadcasted and conversely the population was focused on the TV news channels who only spoked about the pandemic.
We studied the factors that could influence the consequences of pandemic stress and lockdown. The female gender was associated with greatest anxiety in the whole group and in participants with IBS, as reported in China in healthy subjects [18]. Female gender is also associated with an increased risk for post-traumatic stress [32]. The negative impact of female gender on IBS QOL has already been described, with variable effects on different domains of QOL [20], [35]. Living in a town vs. the countryside, in an apartment vs. a house, with or without a garden, size of the house and living space per person had no effect, but there was a trend for more impaired non-specific QOL in participants who lived alone, teleworking having the opposite effect decreasing depression scores. In the literature, contrasting effect have been reported with the practice of teleworking with greater job-isolation for some [36] and for others positive effect of lower blood pressure [37]. A monthly household income lower than 2000 euros, considered in France to be the poverty line for a couple with two children, was associated with higher global HAD scores, fatigue score, and impairment of non-specific QOL. This may be explained in these families by increased difficulties in gaining access to food and essential supplies after school closures. Indeed, in France as in the USA, meals from schools fulfil an important part of children's daily nutritional needs [38]. However, the only independent factor in a multivariate analysis to explain impairment in non-specific QOL was the (existence or absence of) fact of having or not IBS, confirming the major impact of having a chronic disease with pre-existing psychological factors.
While the effect of stress on IBS for the worsening of symptoms is usual [10], [12] lockdown and the COVID-19 pandemic had contrasting effects on IBS symptoms, 40% of patients having symptom changes, more frequently improved than worsened. Being at home could make it easier to access toilets, to manage abdominal pain, and to have an appropriate diet. Lockdown has also changed patient care, with fewer healthcare professional visits and more online consultations.
Limitations
This study had certain limitations. The duration of 15 days of confinement before the start of this survey could be considered insufficient to verify certain effects, in particular fears linked to a collapse of the economy, but a previously published report has shown that a duration of 10 days is sufficient to see psychological consequences [2]. As it is an online study, one could question the IBS diagnosis which is usually a diagnostic of exclusion in the absence of a diagnostic test; however, this diagnosis was made by a doctor in most cases, and a colonoscopy that decreases the risk of differential diagnosis was frequently performed. The predominance of female gender, the disease duration and transit sub-types were usual [20], [39]. A higher percentage of women was found among participants with IBS, but it had the same influence in both groups that were comparable in terms of age, level of education, income, and other comorbidities known to be able to worsen COVID-19 infection. Confinement conditions such as entire size of the house, number of people confined, living space per person, and activities performed were also similar. The two groups could not be matched but are similar in age and IBS patients have similar age than in a study using the French Health Data system with 30,000 IBS patients [40]. In the period of the COVID-19 pandemic where all consultations were cancelled and where the message of “stay at home” was given, research on non-hospitalized illness is particularly difficult. Only patients who were easily reachable and who had given their prior agreement to participate in online studies could therefore be included, which is the case for members of this French association. Others studies about healthy subjects in China during COVID-19 pandemic had the same bias of representability compared to general population and were performed among friends or people contacted by social network as we did [18]. In the absence of prior data in both groups of participants the causality of the impairment in quality of life and of psychological consequences in participants with and without IBS cannot be formally established despite an increase in perceived stress in both groups. Moreover, in participants with IBS two causes are possible, on one hand the disease itself and on the other hand the COVID-19 pandemic and the associated lockdown.
Conclusion
In a period when all available resources are mobilized for the treatment of patients with COVID-19, this survey is one of the few to study the collateral effects of pandemic and lockdown stress, both in people with and without chronic illness. This study showed a similar level of multidimensional stress in participants with or without IBS, but greater consequences in patients with IBS. It highlighted certain factors associated with confinement conditions, such as the existence of lower financial resources. Attention should be paid to immediate and long-term psychological consequences of pandemic and lockdown, such as the development of post-traumatic stress, both in the general population and in particular in patients with chronic illness. Spreading simple messages via the media with advice to better deal with sleep problems and coping strategies could help to limit the psychological consequences of the pandemic [31], [41] and a nationwide strategic planning for psychological aid during and after pandemic potentially delivered through telemedicine should be established as it is now recommended in China [9].
Public significance statement.
The multidimensional stress associated with COVID-19 pandemic and lockdown (with fear of being infected or to infect loved ones, stress related to lockdown conditions, and fear in relation to financial uncertainty) could affect differently people with or without a chronic condition influenced by stress such as Irritable Bowel Syndrome (IBS). In a study performed in France, although the conditions of a strict lockdown and the perceived level of stress were similar, the impact in terms of fatigue, anxiety, depression and deterioration in quality of life was greater in patients with IBS. This could be explained by the impairment in coping capacities, which are important to resist to pandemic stress, in patients with IBS.
In outbreaks of pandemic disease, attention must be paid to the general population and particularly to patients with chronic diseases related to stress, for the risk of immediate psychological consequences and post-traumatic stress. Giving advice on coping strategies and establishing national psychological aid plan could help to reduced psychological consequences.
Human and animal rights
The authors declare that the work described has been carried out in accordance with the Declaration of Helsinki of the World Medical Association revised in 2013 for experiments involving humans as well as in accordance with the EU Directive 2010/63/EU for animal experiments.
Informed consent and patient details
The authors declare that this report does not contain any personal information that could lead to the identification of the patient(s) and/or volunteers.
Disclosure of interest
The authors declare that they have no competing interest.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contibutions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship. Individual author contributions are as follows:
JM Sabate, MD, PhD and Pauline Jouët, MD, PhD designed the study, administrated the study, recruited the patients, collected, analyzed, and interpreted the data and drafted the manuscript. Suzelle Façon is the president of the French IBS patients’ organization (APSSII), she made a great contribution for the IBS participant questionnaire. AE designed the electronic form of the survey. DD, CM, contributed to analysis and interpretation of the data and critically revised of the manuscript for important intellectual content. FZ, FM, JJR, MB critically revised of the manuscript for important intellectual content.
Guarantor of the article: JM Sabate, MD, PhD had full responsibility for the conduct of the study. He has had access to the data and had control of the decision to publish.
Acknowledgments
The authors thank all participants with IBS (of the French patients’ organization) or without IBS for their implication in this survey. We also thank Mrs Juliet Tyson for her proofreading of English.
References
- 1.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerwin L.E. The challenge of providing the public with actionable information during a pandemic. J Law Med Ethics. 2012;40:630–654. doi: 10.1111/j.1748-720X.2012.00695.x. [DOI] [PubMed] [Google Scholar]
- 4.Taha S., Matheson K., Cronin T., Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: the case of the 2009 H1N1 pandemic. Br J Health Psychol. 2014;19:592–605. doi: 10.1111/bjhp.12058. [DOI] [PubMed] [Google Scholar]
- 5.Rosenbaum L. The untold toll – The pandemic’s effects on patients without COVID-19. N Engl J Med. 2020;328:2368–3271. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 6.Kang C., Yang S., Yuan J., Xu L., Zhao X., Yang J. Patients with chronic illness urgently need integrated physical and psychological care during the COVID-19 outbreak. Asian J Psychiatr. 2020;51:102081. doi: 10.1016/j.ajp.2020.102081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang S.X., Wang Y., Rauch A., Wei F. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288:112958. doi: 10.1016/j.psychres.2020.112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bisson J.I., Cosgrove S., Lewis C., Robert N.P. Post-traumatic stress disorder. BMJ. 2015;351 doi: 10.1136/bmj.h6161. [h6161] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ford A.C., Lacy B.E., Talley N.J. Irritable bowel syndrome. N Engl J Med. 2017;376:2566–2578. doi: 10.1056/NEJMra1607547. [DOI] [PubMed] [Google Scholar]
- 11.Gralnek I.M., Hays R.D., Kilbourne A., Naliboff B., Mayer E.A. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119:654–660. doi: 10.1053/gast.2000.16484. [DOI] [PubMed] [Google Scholar]
- 12.Bennett E.J., Tennant C.C., Piesse C., Badcock C.A., Kellow J.E. Level of chronic life stress predicts clinical outcome in irritable bowel syndrome. Gut. 1998;43:256–261. doi: 10.1136/gut.43.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krupp L.B., LaRocca N.G., Muir-Nash J., Steinberg A.D. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 14.Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 15.Francis C.Y., Morris J., Whorwell P.J. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11:395–402. doi: 10.1046/j.1365-2036.1997.142318000.x. [DOI] [PubMed] [Google Scholar]
- 16.Patrick D.L., Drossman D.A., Frederick I.O., DiCesare J., Puder K.L. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci. 1998;43:400–411. doi: 10.1023/a:1018831127942. [DOI] [PubMed] [Google Scholar]
- 17.Park C.L., Russell B.S., Fendrich M., Finkelstein-Fox L., Hutchison M., Becker J. Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med. 2020;35:2296–2303. doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) Epidemic among the general population in China. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infect Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sabaté J.M., Ducrotté P., Piche T., Zerbib F., Dapoigny M., Bruley des Varannes S., et al. Expectations of IBS patients concerning disease and healthcare providers: results of a prospective survey among members of a French patients’ association. Clin Res Hepatol Gastroenterol. 2020 doi: 10.1016/j.clinre.2020.02.014. [DOI] [PubMed] [Google Scholar]
- 21.Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiao H., Zhang Y., Kong D., Li S., Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921. doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel A., Hasak S., Cassell B., Ciorba M.A., Vivio E.E., Kumar M., et al. Effects of disturbed sleep on gastrointestinal and somatic pain symptoms in irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44:246–258. doi: 10.1111/apt.13677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vinkers C.H., van Amelsvoort T., Bisson J.I., Branchi I., Cryan J.F., Domschke K., et al. Stress resilience during the coronavirus pandemic. Eur Neuropsychopharmacol. 2020 doi: 10.1016/j.euroneuro.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCauley M., Minsky S., Viswanath K. The H1N1 pandemic: media frames, stigmatization and coping. BMC Public Health. 2013;13:1116. doi: 10.1186/1471-2458-13-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Teasdale E., Yardley L., Schlotz W., Michie S. The importance of coping appraisal in behavioural responses to pandemic flu. Br J Health Psychol. 2012;17:44–59. doi: 10.1111/j.2044-8287.2011.02017.x. [DOI] [PubMed] [Google Scholar]
- 27.Cheng C., Inder K., Chan S.W.-C. Patients’ experiences of coping with multiple chronic conditions: a meta-ethnography of qualitative work. Int J Ment Health Nurs. 2019;28:54–70. doi: 10.1111/inm.12544. [DOI] [PubMed] [Google Scholar]
- 28.Torkzadeh F., Danesh M., Mirbagher L., Daghaghzadeh H., Emami M.H. Relations between coping skills, symptom severity, psychological symptoms, and quality of life in patients with irritable bowel syndrome. Int J Prev Med. 2019;10:72. doi: 10.4103/ijpvm.IJPVM_464_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilpart K., Törnblom H., Svedlund J., Tack J.F., Simrén M., Van Oudenhove L. Coping skills are associated with gastrointestinal symptom severity and somatization in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2017;15:1565–1571.e3. doi: 10.1016/j.cgh.2017.02.032. [DOI] [PubMed] [Google Scholar]
- 30.Agha S. Mental well-being and association of the four factors coping structure model: a perspective of people living in lockdown during COVID-19. Ethics Med Public Health. 2021;16:100605. doi: 10.1016/j.jemep.2020.100605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sameer A.S., Khan M.A., Nissar S., Banday M.Z. Assessment of mental health and various coping strategies among general population living under imposed COVID-lockdown across world: a cross-sectional study. Ethics Med Public Health. 2020;15:100571. doi: 10.1016/j.jemep.2020.100571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gerson M.-J., Gerson C.D. The importance of relationships in patients with irritable bowel syndrome: a review. Gastroenterol Res Pract. 2012;2012:157340. doi: 10.1155/2012/157340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lackner J.M., Brasel A.M., Quigley B.M., Keefer L., Krasner S.S., Powell C., et al. The ties that bind: perceived social support, stress, and IBS in severely affected patients. Neurogastroenterol Motil. 2010;22:893–900. doi: 10.1111/j.1365-2982.2010.01516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Björkman I., Jakobsson Ung E., Ringström G., Törnblom H., Simrén M. More similarities than differences between men and women with irritable bowel syndrome. Neurogastroenterol Motil. 2015;27:796–804. doi: 10.1111/nmo.12551. [DOI] [PubMed] [Google Scholar]
- 36.Golden T.D., Veiga J.F., Dino R.N. The impact of professional isolation on teleworker job performance and turnover intentions: does time spent teleworking, interacting face-to-face, or having access to communication-enhancing technology matter? J Appl Psychol. 2008;93:1412–1421. doi: 10.1037/a0012722. [DOI] [PubMed] [Google Scholar]
- 37.Lundberg U., Lindfors P. Psychophysiological reactions to telework in female and male white-collar workers. J Occup Health Psychol. 2002;7:354–364. doi: 10.1037//1076-8998.7.4.354. [DOI] [PubMed] [Google Scholar]
- 38.Dunn C.G., Kenney E., Fleischhacker S.E., Bleich S.N. Feeding low-income children during the COVID-19 pandemic. N Engl J Med. 2020;382:e40. doi: 10.1056/NEJMp2005638. [DOI] [PubMed] [Google Scholar]
- 39.Canavan C., West J., Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80. doi: 10.2147/CLEP.S40245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sabaté J.-M., Rivière S., Jouet P., Gastaldi-Menager C., Fagot-Campagna A., Tuppin P. Healthcare use by 30,000 patients with irritable bowel syndrome (IBS) in France: a 5-year retrospective and one-year prospective national observational study. BMC Gastroenterol. 2019;19:111. doi: 10.1186/s12876-019-1031-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Altena E., Baglioni C., Espie C.A., Ellis J., Gavriloff D., Holzinger B., et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020:e13052. doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]