1.
The burden of morbidity and mortality in COVID‐19 falls disproportionately on older people and those with comorbid medical conditions. 1 We described a death rate for people with dementia three times what would normally be expected for the 5‐year average for April 2020, together with an increase in prescription of antipsychotic medication. 2 We now extend this observation over the subsequent course of the pandemic to highlight that a large proportion of increased COVID‐19 mortality has involved people with dementia, which continues to be the commonest cause of death in England and Wales. 3
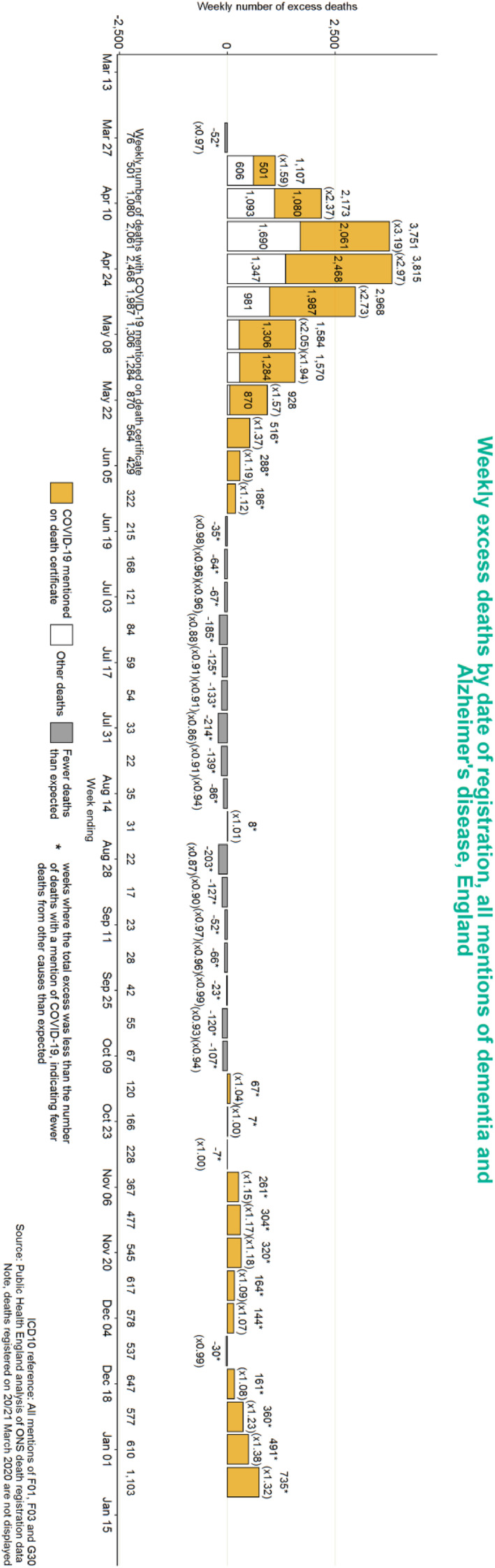
The Office of National Statistics produce weekly bulletins of death rates from which excess mortality rates are derived, that is, numbers of additional deaths compared to the average in previous years. We analysed these data 4 which record three different dementia diagnoses on death certificates: Alzheimer's disease, vascular dementia and unspecified dementia, which, taken together, will include most cases of dementia. Deaths within 28 days of a positive COVID‐19 test are also coded as is whether dementia is the underlying cause of death or a contributory cause mentioned on the death certificate.
The number of excess deaths in England in people with dementia, between 27 March 2020 and 8 January 2021, was 20,100 (figure, showing where dementia was specifically mentioned). This number represents the difference between the expected number of deaths (71,100, calculated from the previous 5‐year average) and the number of deaths in this period in 2020 which included dementia (91,200). During these months, assuming that most or all deaths of people with dementia were in those over the age of 65, this accounted for 31% of the excess deaths of everyone over the age of 65, a proportion that peaked at nearly 40% at the end of June 2020. This, combined with the fact that only 4% of people over the age of 65 have a formal dementia diagnosis, the suggests that COVID‐19 has already disproportionally impacted on the population with dementia, with a eightfold larger share of deaths.
It is likely that more excess deaths in people with dementia during the early stages of the pandemic were COVID‐19 related, but these were missed because fewer tests were carried out. In the second pandemic wave, COVID‐19 reported deaths of people with dementia have been reported more reliably because of increased provision of testing. Much of the increased mortality would have been in care home residents where the excess number of deaths was estimated to be 30,000, two thirds of whose residents have dementia.
During the summer of 2020, the number of deaths of people with dementia and COVID‐19 had reduced sharply to 17 in the week of 4 September 2020. By 27 November 2020, this had increased to 617 per week, a figure that doubled every fortnight from early October to mid‐November 2020. This increased rate of deaths stabilised at this level for the duration of December, before increasing again to 1100 deaths per week in early January 2021.
People with dementia will remain vulnerable to the direct effects of COVID‐19 and its indirect effects on health due to disruption of care services leading to greater isolation. It will be important to ensure that as many people with dementia as possible have rapid access to vaccination with only about a third of people with dementia being covered by the current care home vaccination programme. International vaccination programmes may wish to bear the UK experience in mind when planning strategies.
Robert Howard, Professor of Old Age Psychiatry, UCL Division of Psychiatry.
Alistair Burns, Professor of Old Age Psychiatry, University of Manchester.
Declarations of interest: RH reports grants from the English National Institute of Health Research, outside the submitted work; and is Trustee of the charity Alzheimer's Research UK. A. B. reports being National Clinical Director for Dementia at the National Health Service England (this report is in a professional academic capacity and does not represent the views of NHS England/Improvement) and receiving personal fees from National Health Service England, personal fees from International Journal of Geriatric Psychiatry, personal fees from various lectures and talks, personal fees from occasional court reports, other from Driver and Vehicle Licensing Authority, outside the submitted work.
REFERENCES
- 1. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID‐19‐related death using OpenSAFELY. Nature. 2020;584, 430–436. 10.1038/s41586-020-2521-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Howard R, Burns A, Schneider L. Antipsychotic prescribing to people with dementia during COVID‐19. Lancet Neurol. 2020;19(11):892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. https://www.gov.uk/government/publications/health‐profile‐for‐england/chapter‐2‐major‐causes‐of‐death‐and‐how‐they‐have‐changed (accessed: 29 April 2021).
- 4. https://fingertips.phe.org.uk/static‐reports/mortality‐surveillance/excess‐mortality‐in‐england‐week‐ending‐04‐Dec‐2020.html#deaths‐with‐a‐mention‐of‐specific‐causes (accessed: 29 April 2021).


