ABSTRACT
BACKGROUND
Top public health experts and organizations strongly recommend universal masking for children older than 2 years old during the COVID‐19 pandemic, but speculate it may be difficult for young children. This study sought to assess the usage of cloth face masks in grades pre‐K‐2 and identify associated characteristics and adverse events. It is the first data to assess mask wearing by young children in school.
METHODS
This online, prospective, observational, survey in multiple schools within a single school district in a major metropolitan area measured adherence to face covering mandates by students in grades pre‐K‐2 as measured by percentage of day with appropriate face mask wearing per report via daily teacher surveys for the first 4 weeks of school.
RESULTS
The primary outcome was percent of the day that the entire class was wearing their masks appropriately. Of the estimated almost 1000 students and 1048 classroom days reported, the mean percentage of the school day with appropriate mask usage was 76.9%.
CONCLUSIONS
For a majority of the day while conducting in‐person instruction, children in grades pre‐K‐2 are able to adhere to mask wearing as a key mitigation strategy for limiting SARS‐CoV2 infection spread and possible future use.
Keywords: COVID‐19, coronavirus, communicables disease, infection prevention, medical compliance, nonpharmaceutical interventions
SARS‐CoV‐2 is the virus that causes the novel coronavirus disease of 2019 (COVID‐19). Since its appearance in late 2019, it has caused significant morbidity and mortality worldwide. Many studies have demonstrated that children infected with SARS‐CoV‐2 are more likely to have mild or asymptomatic illness and much lower rates of hospitalization, critical illness, and death than adults. 1 , 2 , 3 In addition, a body of evidence suggests that children under the age of 10 may not spread the virus to the same degree as adults, either to peers, or their adult caregivers including parents and teachers. 4 , 5 , 6 , 7 , 8 , 9 , 10 However, older children may readily transmit the virus when mitigation strategies are not implemented. 11 There is sufficient evidence that social distancing and masking have proven effective at reducing the spread of SARS‐CoV‐2. 12 , 13 , 14
A task force overseeing 15 parochial primary schools within North Georgia around the Atlanta metropolitan area convened prior to the school year to create guidelines for these schools' return to in‐person instruction. After review of the scientific literature and discussions with stakeholders including staff and parents, the task force recommended universal masking with cloth face masks for all students pre‐Kindergarten (pre‐K) through 12th grade in addition to measures, such as physical distancing, enhanced disinfection, cohorting of students, and other strategies. The policy allowed students in grades pre‐K through 2nd, at the discretion of the teacher, to remove their masks when the masks had the potential to interfere with educational instruction. Subsequent to the school district adopting this policy, the US Centers for Disease Control and Prevention (CDC) published guidance on school reopening, reiterating their position for universal masking for individuals of all ages over 2, which was also supported by the American Academy of Pediatrics (AAP). 15 , 16 The school reopening guidance from these agencies noted that appropriate and consistent use of face coverings may be challenging for students in early elementary school. 16 , 17
At present, there are no known studies evaluating children of any age wearing cloth face masks for extended periods of time. Thus, the reopening of schools to in‐person instruction represented an opportunity to observe children in early elementary school and their adherence to masking guidelines.
With this observational study, the investigators sought to quantify the proportion of the school day that each class cohort wore their masks successfully. Additional aims included identifying patterns to mask usage, time periods during the school day when adherence is challenging, and effects of age and class size on mask usage. Furthermore, with no relevant safety data related to mask usage in this age group available, the information collected included adverse events related to wearing a mask, such as syncopal episodes, difficulty breathing, or anxiety attacks.
METHODS
This study was designed as an online, prospective, longitudinal, observational survey of children within 4‐grade levels as reported by their teachers over the course of 4 weeks at the start of the 2020 to 2021 school year.
Participants
Included participants were all teachers who taught either pre‐K, kindergarten, first, or second grades within schools in the Office of Catholic Schools in the Archdiocese of Atlanta. Principals at the primary schools were able to opt out their entire school from participation in the survey.
Procedure
Results and methods are presented adhering to the Checklist for Reporting Results of Internet E‐Surveys (CHERRIES). 18
The primary outcome was the percentage of the school day that the entire class wore their facemasks appropriately, excluding scheduled breaks (ie, lunch or recess) or breaks at the teachers' discretion.
Informed consent from the teachers was obtained through disclosure in the front matter of the survey, which included a description of the aims, the expected length of time to complete the survey, a description of potential harms and benefits, and methods of data collection. Completion of the survey was considered indicative of informed consent. Identifying data collected in the survey consisted only of IP address, school affiliation, and grade level taught. The school affiliation was coded immediately through random number generation and the coding key was stored under standard password protection on computers only available to the study team. Participants were invited to participate through direct email communication. Teachers' email addresses were provided by the principal of their respective schools.
Surveys consisted of 2 pages with a total of 8 questions, with responses collected on SurveyMonkey.com. Questions were not randomized and adaptive questioning was not utilized. Seven of 8 questions required answers. Participants were able to review their answers before submission. IP addresses were collected as a default through SurveyMonkey. Responses were collected daily from teachers on school days beginning on August 17th, 2020 through September 11th, 2020. If classes were required to quarantine due to COVID‐19 exposure, responses from teachers were not obtained.
It is not possible to identify page views through Survey Monkey tools, however with a fixed number of teachers (92 total) and 19 school days in the survey period there was potential for 1748 responses, with 1052 collected, the response rate was 60.18%. It was decided a priori to exclude incomplete surveys from the final analysis. This removed 4 responses.
Data Analysis
A linear mixed model was used to estimate least squares (LS) means of percent mask adherence by grade level and class size while adjusting for clustering by school. Pairwise comparisons between grade levels were conducted using Tukey‐adjusted least square mean differences. Tukey adjustment was performed to control for an increase in Type I error from doing multiple pairwise comparisons. Class size categories were determined as small (less than or equal to the 25th percentile of continuous class size or 7‐14 students), medium (greater than the 25th percentile or less than the 75th percentile or 15‐21 students), and large (greater than or equal to the 75th percentile or 22‐27 students).
Trends in percent mask adherence over the course of the 4‐week survey period were assessed by aggregating reported mask adherence into weekly intervals.
RESULTS
Teachers from all 15 schools participated in the survey, of which 8 schools had pre‐K classes. Mean class size for pre‐K was 12.46 students (range 8‐26),17.34 students for Kindergarten (K) (range 7‐27), 18.17 students in Grade 1 (range 12‐27), and 17.56 for Grade 2 (9‐27). There were 10 pre‐K classes, 28 K classes, 27 Grade 1, and 27 Grade 2 in the sample. Only 2 classes were required to quarantine during the survey period resulting in no data for those days. Total classroom days was 1048.
The primary outcome was percent of the day, exclusive of planned and teacher‐determined breaks, that the entire class was wearing their masks appropriately. For all responses, the mean percentage was 76.9%. The least‐square means are as follows: pre‐K 56.25%, kindergarten 73.52%, first grade 76.92%, and second grade 87.62%. Percent mask adherence differed significantly across grade levels (overall p < .001) (Table 1). Differences in percent mask adherence between grades kindergarten versus pre‐K, first grade versus pre‐K, second grade versus pre‐K, second grade versus kindergarten, and first grade versus second grade were all statistically significant (p < .001) (Table 2).
Table 1.
Percent Adherence by Grade Level, Adjusting for Clustering by School
| Grade | LS‐Means | Standard Error | Overall p‐value for Fixed Effect |
|---|---|---|---|
| Pre‐K | 56.25 | 3.89 | < .0001 |
| K | 73.52 | 3.47 | |
| 1st | 76.92 | 3.53 | |
| 2nd | 87.62 | 3.49 |
Table 2.
Pairwise Comparisons of Percent Adherence by Grade Level, Adjusting for Clustering by School
| Grade | LS‐Mean Differences | Standard Error | Difference p‐value |
|---|---|---|---|
| K vs pre‐K | 17.27 | 2.31 | <.0001 |
| 1st vs pre‐K | 20.66 | 2.36 | <.0001 |
| 2nd vs pre‐K | 31.37 | 2.29 | <.0001 |
| 1st vs K | 3.39 | 1.64 | .1627 |
| 2nd vs K | 14.10 | 1.52 | <.0001 |
| 1st vs 2nd | −10.71 | 1.59 | <.0001 |
The least‐square means for each class size are as follows: small 75.18%, medium 75.22%, and large 67.68%. Percent mask adherence differed significantly across class sizes (p < .001) (Table 3). Pairwise comparisons between the different class sizes were conducted using Tukey‐adjusted least square mean differences. Tukey adjustment was done to control for an increase in Type I error from doing multiple pairwise comparisons. Differences between large versus small and large versus medium class sizes were statistically significant (p = .008, p < .001, respectively) (Table 4). Teachers were given considerable leeway by the district policy to create breaks during the school day in addition to scheduled breaks such as lunch and recess. The number of breaks varied between grades and were inversely related to grade level. The mean number of breaks per day for pre‐K were 4. 19 (range 1‐8), K 3.31 (1‐8), Grade 1 3.72 (0‐6), Grade 2 3.63 (0‐8).
Table 3.
Percent Adherence by Class Size, Adjusting for Clustering by School
| Class Size | LS‐Means | Standard Error | Overall p‐value for Fixed Effect |
|---|---|---|---|
| Small | 75.18 | 3.73 | .0007 |
| Medium | 75.22 | 3.63 | |
| Large | 67.68 | 3.88 |
Table 4.
Pairwise Comparisons of Percent Adherence by Class Size, Adjusting for Clustering by School
| Class Size | LS‐Mean Differences | Standard Error | Difference p‐value |
|---|---|---|---|
| Medium vs small | 0.04 | 1.83 | .9997 |
| Large vs small | −7.50 | 2.50 | .0079 |
| Large vs medium | −7.54 | 1.98 | .0004 |
The survey took place over the first 4 weeks of the school year. To evaluate the temporal patterns of mask usage as children spent more time in school, the 5‐day periods in each ordinal school week were aggregated by grade level and then compared. The mean percent mask adherence is as follows: week 1, 76.84%; week 2, 76.36%; week 3, 76.40%; and week 4, 77.65%. Mean percent mask adherence appeared to increase slightly over the course of the survey. However, mean percent mask adherence did not differ significantly by week over the course of the survey (p = .6953). There was high variability in percent mask adherence reported by classrooms each week (Figure 1).
Figure 1.
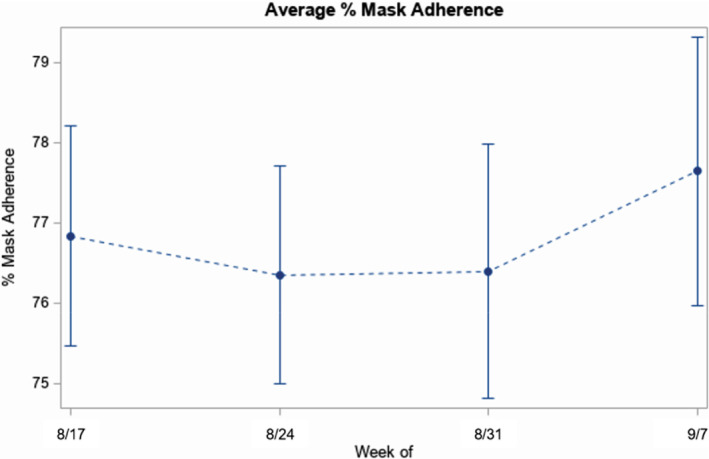
Mask Adherence over Time—August to September 2020
Weekly trends in percent mask adherence by grade level were assessed as well (Figure 2). The mean percent mask adherence for pre‐K is week 1, 50.00%; week 2, 58.70%; week 3, 58.60%; and week 4, 62.89%; kindergarten is week 1, 74.17%; week 2, 72.74%; week 3, 72.30%; and week 4, 70.47%; the first grade is week 1, 77.88%; week 2, 75.60%; week 3, 76.00%; and week 4 78.66%; and second grade is week 1, 87.21%; week 2, 86.25%; week 3, 87.21%; and week 4, 89.32%. Mean percent mask adherence increased most for pre‐K over the course of the survey. While mean percent mask adherence increased slightly for first and second grades over the course of the survey, it decreased slightly for kindergarten. However, mean percent mask adherence did not differ significantly by week for grade levels over the course of the survey (p = .2670) (Figure 2).
Figure 2.
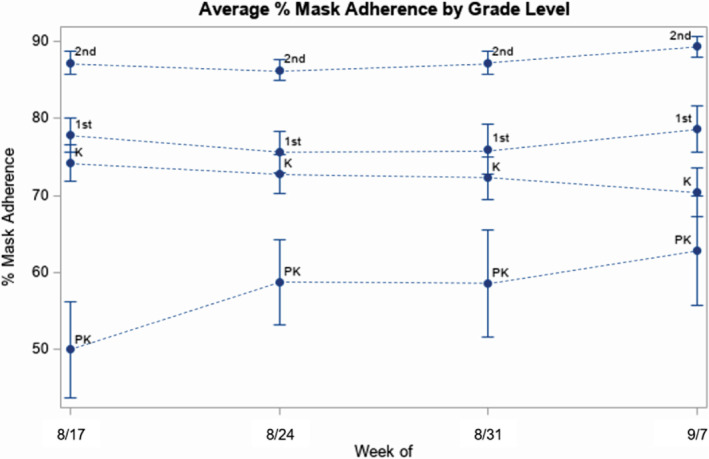
Mask Adherence by Grade Level—August to September 2020
As initial data collection for a potential quality improvement process, teachers were also asked what periods of the school day were challenging to reach full mask usage. Teachers reported that the most challenging time of day was “after recess” (567 reports), followed by “after lunch” (490 reports), and then “during independent work time” (324 reports). In the open comments section, a few teachers mentioned that full mask usage declined at the end of the day and week.
With no data regarding the safety profile of cloth masks used in these age groups, data were collected on adverse events in the classroom that in the teacher's opinion was directly related to mask use. Overall, adverse events were low with a total of 59 reported. Of note, teachers had a separate opportunity to mention any other issues and concerns. At times, the issues and concerns overlapped in theme with the adverse event reporting as well as some teachers summarized adverse events generally rather than listing them as a specific individual incident. The most common adverse event described was related to stress, anxiety, and “meltdown” over wearing the mask or being asked to continually fix/wear the masks which was mentioned 13 times by teachers. There were 12 reports of students' ears hurting and/or headaches. Six nosebleeds were documented, but in the teachers' opinions, it was unclear if these events were related to masks. Teachers noted 8 times total (in both issues and adverse events sections) that students were frustrated by difficulty hearing and communicating with both the teachers and their classmates. An increase in bathroom accidents was mentioned twice and attributed by the teachers to missing facial cues or not hearing the student's request to go to the bathroom. Students complained about difficulty breathing 6 times which were all easily managed (eg, a small break from the mask in appropriate settings). Teachers mentioned 7 times that the students were hot from the masks. There were no serious medical events requiring intervention. Notably, a theme of issues was mentioned 31 times regarding baseline poor fit of the masks as well as masks becoming wet and stretched which led to worsening fit over time.
DISCUSSION
This survey is the first to explore cloth face mask usage in early elementary school‐age children which is a critical strength. Given the urgency of the pandemic and the importance of in‐person instruction to avoid untoward consequences, 20 , 21 , 22 , 23 , 24 this project provides important information regarding expectations for students and mask usage as school districts across the United States consider moving back to in‐person instruction. The large number of students observed, estimated at 983 students, is also a strength of this project.
Our study demonstrates that the guidance from the CDC regarding difficulty with mask usage in this age group is warranted. While teachers reported a meaningful level of adherence during the school day for all ages, it required significant effort to achieve. Factors that increased usage were smaller class size, and higher grade level. Mask usage did not change in a significant manner over the course of the data collection period which is potentially concerning as one considers the length of time the pandemic is expected to last, particularly as young children are highly unlikely to receive doses of vaccines during the 2020 to 2021 school year.
Masks were well tolerated in the 4‐week survey period. Headaches/ears hurting was the top bodily symptom documented by teachers. This correlates with a survey amongst health care workers in which about 80% of respondents developed de‐novo headaches particularly those wearing personal protective equipment for more than 4 hours. 25 The authors speculate however that the most significant negative finding in this survey was student frustration over impaired communication with peers and teachers. This likely under‐represents the total number of students who had difficulty hearing/being heard considering teachers only documented when students were outwardly affected. At a minimum, masks reduce decibels, attenuate frequencies, and remove visual cues which is a risk for young children who are developing speech, language, and pre‐reading/reading skills. 26 , 27 No serious adverse events were reported. Given the significant hesitation for mask wearing in certain areas of the United States, this safety profile is an important finding.
There are significant limitations to our project, some of which may limit the general application of our findings to other circumstances and districts. First, as a parochial school system, there are fewer students of color, students with special needs, and students of lower socio‐economic status. These are all factors associated with lower likelihood of choosing in‐person instruction 28 , 29 , 30 and may also be associated with unrecognized confounders related to mask usage. Of particular importance is the relative lack of children with special needs that the CDC notes, appropriately in the opinion of the authors, may have medical reasons for not wearing masks or particular challenges with mask wearing.
Second, while surveying the teachers was a convenient sample, there are limitations to self‐reporting of such data including recall bias, unknown inter‐ and intra‐rater reliability issues, potential Hawthorne effects, and social desirability bias. With repeated daily surveys, recall bias may be mitigated. While this project was without an intervention, the act of asking teachers to report on their class may in turn have created motivation to improve mask adherence by their students beyond what would have been observed otherwise. This is a significant concern when combined with the potential impacts of social desirability bias both in terms of positive and negative survey results. While much of the public service messaging around masks has focused on how masks protect those around the wearer, it is also possible that since mask use has become a political issue in the United States some teachers may have negative feelings towards masks leading to decreased motivation to make students wear masks or result in subconsciously misrepresenting their answers.
Perhaps the most important limitation, our project design asked teachers to report the period of time that the entire class was wearing their masks appropriately. This was chosen as it is the optimal outcome of the mask mandate but opens the possibility of high adherence by most children being negated by minor disruptions or by only a few children having difficulty with mask wearing. While designing the survey it was felt that it would be easiest for the teachers to track the entire class adhering to the mandate, rather than asking to approximate usage of individual students during the day while also trying to teach effectively. Using a different methodology such as an external observer to monitor mask wearing of individual students has the potential to provide more granular results, but was not feasible due to visitor restrictions at the schools and time constraints.
Use of face masks is a critical nonpharmaceutical intervention for limiting the spread of SARS CoV‐2. Guidance from the CDC and the AAP suggested that mask use in younger age children may prove difficult. Our project is the first to evaluate the mask usage of younger children and demonstrates that children in early elementary school can reliably wear masks for significant portions of the day. Mask usage improves with age and with smaller class sizes. We also found a reassuring safety profile with no serious adverse events reported. These results should encourage other school districts to adapt universal masking policies during the COVID‐19 pandemic and in the future.
IMPLICATIONS FOR SCHOOL HEALTH AND EQUITY
Beyond the COVID‐19 pandemic, nonpharmaceutical interventions for many infectious diseases may remain valuable tools to keep children, teachers, and staff safe. Scientists are concerned that a surge in infections from viruses other than SARS‐CoV2 may occur as communities relax precautions. Evidence of this is occurring in the Southern Hemisphere. Australia saw historically low levels of flu‐like illness in children and adults in May 2020, when levels are usually high. Subsequently, when the country successfully reduced COVID‐19 and relaxed mitigation protocols, a 6‐fold surge in flu cases occurred in children aged 5 and younger by December 2020 when cases are usually lowest. 31 The surge may be due to the lack of a natural biological factors which in other years help maintain a level of infection rates. 32 , 33 The United States may experience this as the CDC tracking system and BioFire a company that provides diagnostic tests for viruses and bacteria in the United States are also showing stark declines in multiple contagious infections during COVID‐19 pandemic mitigation efforts. 34 , 35 The future of school health will be transformed by infectious disease and epidemiologic evidence learned during the COVID‐19 pandemic. Schools may consider utilizing proven strategies such as masking to reduce spread of contagious illness for years to come. With the findings in our study in mind, schools should:
Anticipate significant effort during the school day to maintain mask adherence. Teachers in younger grades will need remind to students frequently to readjust their masks. They should also anticipate that the majority of the class will likely do well with mask wearing but certain students may have greater challenges, necessitating an individualized approach.
Plan on mask breaks throughout the day to allow students respite from their masks, but recognize such breaks also run the risk of decreasing adherence as well. Return from recess and physical education class when students may be hot, for example, can be challenging to get masks placed back on correctly.
Poor fit was a common complaint from teachers, and many parents have realized over the course of the COVID‐19 pandemic that commercially available masks lack sizing consistency from brand to brand and style to style. It may prove fruitful, in situations where school budgets allow, for the school to provide multiple masks to children for the duration of any future masking need. This would provide consistency of sizing and assure uniformity for the student from day to day.
Plan for nonvocal communication cues for routine classroom interruptions such as asking for bathroom breaks.
Consider continual surveillance and reporting of mask adherence by teachers or outside observers to assess mask usage as part of an ongoing quality improvement process.
These recommendations will need to be implemented in a manner specific to each school and classroom as there unique needs and considerations for each.
Human Subjects Approval Statement
This project received a Not Human Subject Research determination from the Institutional Review Board of Children's Healthcare of Atlanta, and therefore, was exempt from review.
Conflict of Interest
All authors of this article declare they have no conflicts of interest.
This study was funded in part by the Wilbur and Hilda Glenn Family Foundation and in part, by the Pediatric Biostatistics Core, which is subsidized by Emory University and Children's Healthcare of Atlanta. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the funding sources.
Contributor Information
Geoffrey E. Mickells, Email: Geoffrey.mickells@choa.org.
Janet Figueroa, Email: Janet.figueroa@emory.edu.
Kelly Withers West, Email: kwestmd@gmail.com.
Anna Wood, Email: Anna.wood@emory.edu.
Barbara O. McElhanon, Email: bmcelhanon@emory.edu.
REFERENCES
- 1. Souza T, Nadal J, Nogueira R, Pereira R, Brandão M. Clinical manifestations of children with COVID‐19: a systematic review. Pediatr Pulmonol. 2020;55(8):1892‐1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gudbjartsson D, Helgason A, Jonsson H, et al. Spread of SARS‐CoV‐2 in the Icelandic population. N Engl J Med. 2020;382(24):2302‐2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shekerdemian L, Mahmood N, Wolfe K, et al. Characteristics and outcomes of children with coronavirus disease 2019 (COVID‐19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020;174(9):868‐873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. van der Hoek W, Backer JA, Bodewes R, et al. De rol van kinderen in de transmissie van SARS‐CoV‐2 [The role of children in the transmission of SARS‐CoV‐2]. Ned Tijdschr Geneeskd. 2020;164:D5140. [PubMed] [Google Scholar]
- 5. Ludvigsson J. Children are unlikely to be the main drivers of the COVID‐19 pandemic—a systematic review. Acta Paediatr. 2020;109(8):1525‐1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Posfay‐Barbe K, Wagner N, Gauthey M, et al. COVID‐19 in children and the dynamics of infection in families. Pediatrics. 2020;146(2):e20201576. [DOI] [PubMed] [Google Scholar]
- 7. Lee B, Raszka W. COVID‐19 transmission and children: the child is not to blame. Pediatrics. 2020;146(2):e2020004879. [DOI] [PubMed] [Google Scholar]
- 8. Bailey L, Razzaghi H, Burrows E, et al. Assessment of 135,794 pediatric patients tested for severe acute respiratory syndrome coronavirus 2 across the United States. JAMA Pediatr. 2021;175(2):176‐184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Viner R, Mytton O, Bonell C, et al. Susceptibility to SARS‐CoV‐2 infection among children and adolescents compared with adults. JAMA Pediatr. 2021;175(2):143‐156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leeb R, Price S, Sliwa S, et al. COVID‐19 trends among school‐aged children—United States, march 1–September 19, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(39):1410‐1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Szablewski C, Chang K, Brown M, et al. SARS‐CoV‐2 transmission and infection among attendees of an overnight camp—Georgia, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(31):1023‐1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chu D, Akl E, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person‐to‐person transmission of SARS‐CoV‐2 and COVID‐19: a systematic review and meta‐analysis. Lancet. 2020;395(10242):1973‐1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hendrix M, Walde C, Findley K, Trotman R. Absence of apparent transmission of SARS‐CoV‐2 from two stylists after exposure at a hair salon with a universal face covering policy—Springfield, Missouri, May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(28):930‐932. [DOI] [PubMed] [Google Scholar]
- 14. Wang X, Ferro E, Zhou G, Hashimoto D, Bhatt D. Association between universal masking in a health care system and SARS‐CoV‐2 positivity among health care workers. JAMA. 2020;324(7):703‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. US Centers for Disease Control and Prevention . COVID‐19: Considerations for Wearing Masks. 2020. Available at: https://www.cdc.gov/coronavirus/2019‐ncov/prevent‐getting‐sick/cloth‐face‐cover‐guidance.html. Accessed August 08, 2020.
- 16. Korioth T. AAP urges universal cloth face coverings for those ages 2 and up, with 'rare exception'. August 17, 2020. Available at: https://www.aappublications.org/news/2020/08/13/covid19facecoverings081320 Accessed August 17, 2020.
- 17. US Centers for Disease Control and Prevention . Guidance for K‐12 School Administrators on the Use of Cloth Face Coverings in Schools. 2020. Available at: https://www.cdc.gov/coronavirus/2019‐ncov/community/schools‐childcare/cloth‐face‐cover.html. Accessed August 8, 2020.
- 18. Eysenbach G. Correction: improving the quality of web surveys: the checklist for reporting results of internet E‐surveys (CHERRIES). J Med Internet Res. 2012;14(1):e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Munro A, Faust S. Children are not COVID‐19 super spreaders: time to go back to school. Arch Dis Child. 2020;105(7):618‐619. [DOI] [PubMed] [Google Scholar]
- 20. US Centers for Disease Control and Prevention . The Importance of Reopening America's Schools This Fall. 2020. Available at: www.cdc.gov/coronavirus/2019‐ncov/community/schools‐childcare/reopening‐schools.html. Accessed August 8, 2020.
- 21. Christakis DA. School reopening ‐ the pandemic issue that is not fetting its due. JAMA Pediatr. 2020;174(10):928. [DOI] [PubMed] [Google Scholar]
- 22. Patel S, Epalza Ibarrondo C, Toubiana J, Van der Linden D. Urgent need to develop evidence‐based COVID‐19 recommendations for primary schools. Arch Dis Child. 2020;29:archdischild‐2020‐321017. 10.1136/archdischild-2020-321017 [Online ahead of print]. [DOI] [PubMed] [Google Scholar]
- 23. Christakis D, Van Cleve W, Zimmerman F. Estimation of US children's educational attainment and years of life lost associated with primary school closures during the coronavirus sisease 2019 pandemic. JAMA Netw Open. 2020;3(11):e2028786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sharfstein J, Morphew C. The urgency and challenge of opening K‐12 schools in the fall of 2020. JAMA. 2020;324(2):133‐134. [DOI] [PubMed] [Google Scholar]
- 25. Ong J, Bharatendu C, Goh Y, Tang J, Sooi K, Tan Y. Headaches associated with personal protective equipment – a cross‐sectional study among frontline healthcare workers during COVID‐19. Headache. 2020;60(5):864‐877. [DOI] [PubMed] [Google Scholar]
- 26. Nobrega M, Opice R, Lauletta M, Nobrega C. How face masks can affect school performance. Int J Pediatr Otorhinolaryngol. 2020;138:110328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Goldin A, Weinstein BE, Shiman N. How do medical masks degrade speech perception? Hearing Review. 2020;27(5):8‐9. [Google Scholar]
- 28. Kroshus E, Hawrilenko M, Tandon P, Christakis D. Plans of US parents regarding school attendance for their children in the fall of 2020. JAMA Pediatr. 2020;174(11):1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kaiser Family Foundation . KFF Health Tracking Poll—July 2020. Coronavirus: Reopening, Schools, and the Government Response 2020. Available at: https://www.kff.org/coronavirus‐covid‐19/report/kff‐health‐tracking‐poll‐july‐2020/. Accessed December 9, 2020.
- 30. Chua K, DeJonckheere M, Reeves S, Tribble A, Prosser L. Factors associated with school attendance plans and support for COVID‐19 risk mitigation measures among parents and guardians. Acad Pediatr. 2020:S1876‐S2859(20)30593‐3. 10.1016/j.acap.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hurley D. Coronavirus shutdowns have quashed nearly all other common viruses. But scientists say a rebound is coming. The Washington Post. 2021. Available at: https://www.washingtonpost.com/health/2021/01/12/covid‐shutdowns‐viruses/. Accessed February 3, 2021.
- 32. Baker R, Park S, Yang W, Vecchi G, Metcalf C, Grenfell B. The impact of COVID‐19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc Natl Acad Sci. 2020;117(48):30547‐30553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wu A, Mihaylova V, Landry M, Foxman E. Interference between rhinovirus and influenza a virus: a clinical data analysis and experimental infection study. Lancet Microbe. 2020;1(6):e254‐e262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Syndromic Trends . Biofire By Biomerieux. Available at: https://syndromictrends.com/metric/panel/rp/percent_positivity/organism/main. Accessed February 3, 2021.
- 35. US Centers for Disease Control and Prevention . RSV, HMPV, norovirus, parainfluenza, other types of coronavirus National Trends. February 3, 2021. Available at: https://www.cdc.gov/surveillance/nrevss/index.html. Accessed February 3, 2021.


