Abstract
Race‐based and other demographic information on COVID‐19 patients is not being collected consistently across provinces in Canada. Therefore, whether the burden of COVID‐19 is falling disproportionately on the shoulders of particular demographic groups is relatively unknown. In this article, we first provide an overview of the available geographic and demographic data related to COVID‐19. We then make creative use of these existing data to fill the vacuum and identify key demographic risk factors for COVID‐19 across Canada's health regions. Drawing on COVID‐19 counts and tabular census data, we examine the association between communities’ demographic composition and the number of COVID‐19 infections. COVID‐19 infections are higher in communities with larger shares of Black and low‐income residents. Our approach offers a way for researchers and policymakers to use existing data to identify communities nationwide that are vulnerable to the pandemic in the absence of more detailed demographic and more granular geographic data.
RÉSUMÉ
Les renseignements fondés sur la race et d'autres données démographiques sur les patients atteints du COVID‐19 ne sont pas recueillis de manière uniforme dans toutes les provinces du Canada. Par conséquent, si le fardeau du COVID‐19 tombe de manière disproportionnée sur les épaules de groupes démographiques particuliers est relativement inconnu. Dans cet article, nous fournissons d'abord un aperçu des données géographiques et démographiques disponibles liées au COVID‐19. Nous utilisons ensuite de manière créative ces données existantes pour combler le vide et identifier les principaux facteurs de risque démographiques du COVID‐19 dans les régions sociosanitaires du Canada. En nous basant sur les dénombrements de COVID‐19 et les données tabulaires du recensement, nous examinons l'association entre la composition démographique des communautés et le nombre d'infections au COVID‐19. Les infections au COVID‐19 sont plus élevées dans les communautés avec une plus grande proportion de résidents Noirs et à faible revenu. Notre approche offre aux chercheurs et aux décideurs un moyen d'utiliser les données existantes pour identifier les communautés à l'échelle nationale qui sont vulnérables à la pandémie en l'absence de données démographiques plus détaillées et géographiques plus granulaires.
INTRODUCTION
The global novel coronavirus disease 2019 (COVID‐19) pandemic has been raging for more than one year. In Canada, an initial wave emerged in mid‐March, and by mid‐April, there were roughly 1,500 new cases each day. This surge was followed by a period in the summer when Canada “flattened the curve” and was registering less than 500 new cases most days. At the time of writing, we are in the midst of a second wave that is worse than the first. Between October 1, 2020, and February 1, 2021, there have been just seven days when the count of new cases was less than 2,000. 1 The pandemic has broadly affected the physical (Chanchlani et al., 2020), mental (Zajacova et al., 2020a, 2020b), and economic (Lemieux et al., 2020) wellbeing of the nation's population.
But which groups and communities of Canadians are most at risk of contracting and dying from the COVID‐19 virus? In countries such as the United States (U.S.), the COVID‐19 pandemic has highlighted and exacerbated pre‐existing social and health disparities among traditionally disadvantaged groups. Racial/ethnic minorities and those from low‐income backgrounds are more likely to become infected and die from COVID‐19 (Bhala et al., 2020; Chin et al., 2019; Macias et al., 2020; Mahajan & Larkins‐Pettigrew, 2020). Whether this is also true in Canada is harder to assess.
Although data on COVID‐19 cases and deaths are available in Canada, detailed information on the race/ethnicity, socioeconomic status, and other demographic traits of patients is extremely limited (Blair et al., 2020; Ramos, 2020; Siddiqi et al., 2020). Early in the pandemic, detailed demographic data including information about patients’ race was deemed unnecessary because high‐risk groups were thought to include primarily the elderly and those with weakened immune systems (Boyd, 2020). We know now that other demographic groups are at risk as well (Denice et al., 2020; Kwak, 2020). Canada's data landscape stands in stark contrast to the U.K. and U.S., where the collection and publication of COVID‐19 data by race/ethnicity and sex are mandatory (Bhala et al., 2020). Although some provinces and municipalities in Canada have begun to collect and distribute this information, the overall lack of such data makes it difficult to assess whether there are racial/ethnic, demographic, or socioeconomic disparities in the vulnerability to COVID‐19 on a national level.
Our study fills this data and knowledge vacuum by examining whether communities in Canada with a greater proportion of Black, immigrant, and low‐income residents are also experiencing higher COVID‐19 infection counts. We link aggregated COVID‐19 data at the level of health regions with tabular census data to describe the association between regions’ demographic composition and the number of COVID‐19 cases during the peak of the first and second wave of the pandemic. We then combine the results from this analysis with information about the demographic composition of smaller geographic areas (census subdivisions and census divisions) to provide a more granular understanding of the spatial distribution of COVID‐19 infections across Canada. Finally, we replicate these analyses in Toronto—a city that has been especially hard hit by the pandemic and for which we have more detailed COVID‐19 and demographic information at the level of neighbourhoods. While we are unable to assess whether individuals who belong to particular demographic groups are more or less likely to be affected by the pandemic, we can describe the spatial and demographic variation in the severity of COVID‐19.
Our analyses focus on Black communities based on studies from other countries and Canadian government reports that consistently show that this group has been hit especially hard by the COVID‐19 pandemic (Bhala et al., 2020; City of Toronto, 2020; Statistics Canada, 2020; Sze et al., 2020; Thebaud et al., 2020). For example, by early November 2020, Black Torontonians were, respectively, 1.4, 4.6, and 7.2. times as likely as their South Asian, White, and East Asian counterparts to have contracted COVID‐19. 2 Black Canadians were also more likely than other groups to have experienced a job loss during the COVID‐19 pandemic. According to a report released by Statistics Canada in August, the unemployment rate for Black Canadians was 17.6 percent, compared to 16.6 percent for South Asians, 9.4 percent for Whites, and 13.2 percent for Chinese Canadians (Statistics Canada, 2020). The staggering levels of unemployment may have increased Black Canadians’ willingness and need to take jobs that increase their risk of exposure to COVID‐19. Black Canadians are also more likely than other groups to have multiple medical risk factors that render them particularly vulnerable to more severe forms of COVID‐19 (Chung, Adhopia, & Glanz, 2020; Lin, 2020).
BACKGROUND
The lack of race‐based and other demographic information about COVID‐19 patients in Canada reflects a longer history of resistance to or ambivalence about race. Until recently, the collection of race‐based data or the inclusion of race in governmental tabulations was relatively scant (Nath, 2011; Thompson, 2008). Indeed, although the Canadian censuses between 1901 and 1941 asked about race, explicit references to “race” were dropped in 1951. Until Statistics Canada reintroduced the question about “visible minority status” in the 1996 Canadian census, researchers had to rely on questions about ancestry, ethnic or cultural origins, and language proficiency to indirectly capture “race” (Christensen & Weinfeld, 1993; Li, 1992; Ramos, 2013). Even after 1996, unlike the U.S. census, the Canadian census does not explicitly ask respondents to report their “race” (Ruggles et al., 2020; Statistics Canada, 2017). Instead, the Canadian census asks respondents to choose their identity from a list of categories that conflates race, ethnicity, and national origin (e.g., White, South Asian, Black, Latin American).
Such resistance to the fuller collection of race‐based data has numerous explanations. Some have expressed concerns about adequate privacy protections for individuals and groups. It is worth noting, however, that many countries (such as the U.S.) regularly make de‐identified demographic data available safely and securely. Others—including those belonging to racialized minority groups—argue that the collection of race‐based data could exacerbate discrimination (Owusu‐Bempah & Millar, 2010). Information that certain groups experience more disadvantages or are more acutely affected by diseases like COVID‐19 can inadvertently reinforce biological understandings of race, heighten the surveillance of particular groups (especially if groups are viewed as spreaders of the disease), and increase the prejudice and stigma with which groups are viewed and treated (James, 2020). Simultaneously, some visible minority groups have underscored the importance of collecting racial data to address racism and racial inequality (Mignacca, 2020; Stacey, 2020).
The collection of racial data also runs counter to Canada's policy and national identity of multiculturalism (Boyd et al., 2000; Nath, 2011; Thompson, 2008). There is a reluctance among many to point out the ways in which we fall short of this lofty ideal or to highlight differences among Canadians. The dominant narrative in Canadian society and politics is that there are no major problems of race or racism (Thompson, 2008). Many Canadians, including policymakers, assert that racism is marginal, and something that the Canadian government need not necessarily address with further determination (Reitz & Banerjee, 2007). Indeed, a recent Global News poll found that nearly half of Canadian respondents believed that racism is “not really a problem” or only a “minor problem” (Simpson, 2019). 3 This view runs counter to the experiences of visible minority Canadians, among whom one‐in‐three believes their race/ethnicity has negatively affected their careers, and one‐in‐five reports that prejudice or lack of diversity and inclusion has influenced their decision to leave an employer (ADP, 2020).
Refusing to acknowledge the existence of racial discrimination may be exacerbating racial disparities and hindering our ability to address them. Prior work has shown that governments and institutions that “avoid race according to the principles of color blindness serve to solidify existing social hierarchies” (Thompson, 2008: 538). Social, economic, and political environments in Canada are highly racialized, and many racial minorities experience discrimination and unequal outcomes in the labour market, the criminal justice system, immigration policies, education, and other areas (Reitz & Banerjee, 2007; Soroka, Johnston, & Banting, 2007). Race‐based disparities also extend to health and access to care (Adelson, 2005; Lasser et al., 2006; Veenstra, 2009). Veenstra and Patterson (2016), for example, found that Black people had higher rates of diabetes and hypertension than Whites.
These issues are especially urgent during this pandemic. According to a report from Statistics Canada released in July 2020—the first to feature disaggregated racial data—Black and South Asian workers were twice as likely as white Canadians to lose their jobs during the pandemic (Hou, Frank, & Schimmele, 2020). COVID‐19 mortality rates were significantly higher in Canadian dissemination areas with higher shares of Black residents (Subedi et al., 2020). Black immigrants in Canada were also more likely than Whites and other groups to have three or more medical conditions known to increase the risk for more severe forms of COVID‐19 and COVID‐19‐induced mortality (Lin, 2020). Collecting demographic data related to COVID‐19 would tell us not just whether certain communities and groups are more vulnerable to the pandemic, but also why and help design precise and targeted policies to curb the spread of COVID‐19.
Assessing inequalities in the COVID‐19 pandemic
While data on COVID‐19 cases and deaths are available across Canada for provinces and health regions, the lack of widely and consistently available data at smaller geographic units or broken down by demographic traits such as race/ethnicity makes it difficult to know who is most affected by the pandemic. Some cities, including Toronto and Montreal, and provinces like Alberta have released official COVID‐19 counts for geographic units smaller than health regions. Since mid‐March, Alberta has released daily active (but not new or cumulative) counts of COVID‐19 infections for public health authorities, which are subdivisions of health regions. Beginning in May, the City of Toronto has reported cumulative infection counts. And daily “new” (but not cumulative) counts have been available in Montreal boroughs since mid‐March. If the goal is to understand the spatial distribution of COVID‐19 cases across Canada, then inconsistencies in data collection and reporting preclude us from observing COVID‐19 data for regions smaller than public health regions.
During the pandemic, we have seen some improvements in efforts to collect individual data about race and other demographic traits. In June 2020, federal, provincial, and territorial human rights commissions urged the federal government to establish a national strategy for the collection of data that could better identify Canadians who were being disproportionately affected by the pandemic. For example, Ontario's Human Rights Commission said that breaking down COVID‐19 infections and mortality by race as well as by socioeconomic status, disability, sex, and age is “the foundation of evidence‐informed decision‐making.”
Nonetheless, the collection and availability of race‐based and other demographic data related to COVID‐19 still vary across provinces. Manitoba, for instance, was one of the first provinces to announce that it would collect race‐based information about COVID‐19 patients in May 2020, but it had not released the data by the end of 2020 (Thorpe, 2020). Other provinces, such as British Columbia and Quebec, have signaled their willingness to collect race‐based and other demographic data. To our knowledge, such collection has not yet been implemented (Gilmour & Ross, 2020; Mariam, 2020). Indeed, community groups in Montreal frustrated with the absence of action by the province have launched their own platform to collect racial data through a voluntary and anonymous web survey (Mignacca, 2020). 4 By contrast, Ontario, and especially the City of Toronto, stand out as having made the most progress toward collecting and making available demographic information related to COVID‐19 cases. Ontario has a mandate to collect race‐based data, and the Ministry of Public Health indicates a plan to make these data available to select researchers. This commitment extends to other areas: for instance, Ontario is also the only province to require that racial data is collected when police force is used on an individual (Singh et al., 2020). The City of Toronto provides monthly reports of cases broken down by racial groups (as well as by sex and age) on their website.
Generally, researchers interested in assessing the unequal burden of the pandemic across places and groups in Canada must rely on associations at higher levels of geography. Two data sources, in particular, have been used to examine the spatial and demographic patterns in the spread of COVID‐19. First, data from the Public Health Agency of Canada (PHAC) report the daily infection and death counts for health regions. However, these data are not tallied by race or socioeconomic status. Furthermore, each health region encompasses approximately 415,000 residents; thus, they are too large geographically and too heterogeneous socio‐demographically to capture the impact of COVID‐19 on local communities and specific sub‐populations. Second, crowdsourced data, which relies on self‐reports of COVID‐19 cases, does collect finer‐grained measures of where individual patients live, like their postal code (Jones, 2020). While postal code areas are small enough to represent more local communities, these data likely miss a significant portion of COVID‐19 cases by relying on individuals’ access to and willingness to report their symptoms on internet sites. These data have been used to identify certain vulnerable communities—specifically, those who live in densely populated areas or places with higher shares of older (70+) residents—but they ignore the community's racial and socioeconomic composition. Even recent Statistics Canada reports on COVID‐19 infection and mortality rates among visible minorities in Canada rely on neighbourhood‐level analyses since the vital statistics data on which the report relies do not collect racial/ethnic information about individuals (Subedi et al., 2020).
Other researchers have thought creatively about how representation in certain sectors of the labour force or other social contexts heightens or lowers groups’ exposure to the virus. For example, one study found that the uneven distribution of occupational characteristics associated with a higher risk of exposure to the COVID‐19 virus (e.g., physical proximity with other workers) made women, visible minorities, and workers in low‐income occupations more vulnerable to contracting the disease (St‐Denis, 2020).
There is still much we do not know, however. Whether or not Black, immigrant, and low‐income communities throughout Canada have been disproportionately affected by COVID‐19 is a priori unclear. Similar to the U.S., Black people and immigrants in Canada are more socially and economically disadvantaged than whites (Attewell et al., 2010), potentially making them more at risk. Furthermore, Black Canadians have worse health statuses and outcomes than White Canadians (Veenstra, 2009). 5 There are, however, reasons to believe that the patterns in the spread of COVID‐19 will differ across the two countries. Unlike the U.S., Canada has universal health insurance. Relative to their U.S. counterparts, a larger share of the Black Canadian population are high‐skilled immigrants (Statistics Canada, 2019).
In sum, the provincial and federal governments in Canada, by and large, are not making racial and socioeconomic data on individual COVID‐19 patients available to researchers. As a result, there has not yet been a systematic study that examines whether racial minorities, immigrants, and low‐income individuals are particularly vulnerable to COVID‐19. We make creative use of existing data and identify the socio‐demographic risk factors for COVID‐19 in health regions. In Canada, the smallest geographic unit for which COVID‐19 data is consistently available the health region, which is too large and too heterogeneous to capture the spread of COVID‐19 in local communities. Using the results from our analyses of health regions and information about the socio‐demographic traits of smaller geographic areas (i.e., census subdivisions and divisions), we illustrate the spatial and demographic distribution of the pandemic across Canada. We also take advantage of more detailed data in Toronto to present a similar analysis on a smaller scale.
DATA AND METHODS
We rely primarily on two data sources. We obtain daily counts of COVID‐19 infections between January 21, 2020, and January 24, 2021, for most of Canada's health regions from the University of Toronto's COVID‐19 Canada Open Data Working Group (Berry et al., 2020). We focus on COVID‐19 infections in 89 health regions, excluding those in Yukon, the Northwest Territories, and Nunavut, which are sparsely populated and report very few cases.
We combine these COVID‐19 data with information from the 2016 Canadian census. These data, downloaded from the Statistics Canada website, report the demographic composition of health regions (HRs), census subdivisions (CSDs), and census divisions (CDs). Due to privacy concerns, Statistics Canada suppresses information when the tallied counts of CSD residents belonging to a particular demographic group are small. For example, if the number of Black residents in a CSD is less than 10, the value is suppressed. To minimize biases that come from suppressed data, we define communities as either (a) CSDs with more than 2,000 residents or (b) the residual areas within the CD outside of these populous CSDs. With a median population of 6,929 residents, these communities represent smaller and more localized geographic areas than health regions. There are 1,202 communities: 943 CSDs and 259 CDs.
Measures
We measure our outcome—the cumulative count of COVID‐19 infections—at two time points: (1) the peak of the first wave (April 20, 2020) and (2) the peak of the second wave of the pandemic (January 10, 2021). Our results are not sensitive to the specific choice of peak dates. Our focus on COVID‐19 counts instead of rates is consistent with reporting by the Public Health Agency of Canada. That said, we also report supplementary results using rates (per 100,000) in the appendix.
We include several covariates measuring the demographic composition from the 2016 census: the percentage of residents in a health region or pseudo‐CSD who are Black; 65 years and older; foreign‐born; low‐income; have a university degree, certificate, or degree at the bachelor level or above; and work in health care occupations. We also control for population density, measured by dividing the number of people in a geographic unit by its land area. Research in other national contexts has identified these as potential risk (or protective) factors for COVID‐19 (Thebault, Tran, & Williams, 2020; Yancy, 2020). Low‐income residents are defined as those whose income falls below Statistics Canada's low‐income cut‐off (LICO). Because the COVID‐19 epicenters in Canada are located predominantly in urban centers, we also controlled for urbanicity, measured as the share of a health region's or pseudo‐CSD's land area comprised by population centers. A population centre refers to an area with a population of at least 1000 and a population density of at least 400 persons per square kilometer; all other areas outside of population centres are classified as rural areas by the Canadian census (Statistics Canada, 2017). We used this measure to classify all the geographic areas into terciles (low, middle, high) of urbanicity. Table 1 presents descriptive statistics at the levels of health regions and pseudo‐CSDs.
Table 1.
Descriptive statistics of health regions
| Mean | SD | Min | Max | |
|---|---|---|---|---|
| Health Regions | ||||
| Percent Black | 1.7 | 2.1 | 0.2 | 9.5 |
| Percent foreign‐born | 12.3 | 12.0 | 0.8 | 53.5 |
| Percent low‐income | 6.7 | 2.7 | 2.5 | 17.9 |
| Percent working in health | 7.1 | 1.3 | 3.8 | 13.0 |
| Percent 65+ years | 18.2 | 4.5 | 3.8 | 26.4 |
| Percent w/bachelor's degree or more | 20.3 | 8.9 | 8.9 | 45.0 |
| Population density | 191.3 | 653.3 | 0.0 | 4334.5 |
| Urban residence (Column %) | ||||
| Rural | 32.6 | |||
| Semi‐urban | 34.8 | |||
| Urban | 32.6 | |||
| Total | 100.0 | |||
| N | 89 | |||
| Pseudo‐CSDs | ||||
| Percent Black | 0.4 | 0.8 | 0.0 | 9.5 |
| Percent foreign‐born | 8.7 | 8.5 | 0.0 | 67.5 |
| Percent low‐income | 5.2 | 2.7 | 0.3 | 36.4 |
| Percent working in health | 7.1 | 2.0 | 0.0 | 18.2 |
| Percent 65+ years | 20.0 | 6.7 | 2.6 | 62.0 |
| Percent w/bachelor's degree or more | 19.4 | 8.8 | 1.3 | 46.3 |
| Population density | 233.6 | 503.0 | 0.0 | 5492.6 |
| Urban residence (Column %) | ||||
| Rural | 33.3 | |||
| Semi‐urban | 33.5 | |||
| Urban | 33.2 | |||
| Total | 100.0 | |||
| N | 1,202 |
Notes: Data come from Statistics Canada's 2016 census tabular estimates. Pseudo‐CSDs refer to CSDs with more than 2,000 residents or to CDs outside of these populous CSDs.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
We exclude other measures capturing an area's demographic composition (e.g., percent Asian 6 ) due to multicollinearity (VIF > 10). We do not include the percentage of residents who are Indigeneous in our analyses for two reasons. First, according to media reports, COVID‐19 infections and deaths of Indigenous people have been vastly undercounted (Patel 2020). Second, preliminary analyses indicated that our conclusions were sensitive to the definition used for Indigenous people (i.e., official registration, sole ancestry, the primary language used at home).
Analytical strategy
Our primary analysis proceeds in two stages. First, we assess the relationship between the cumulative count of COVID‐19 infections and the demographic composition of health regions in Canada with Poisson regression models. We standardize all covariates, and we estimate separate models of the cumulative COVID‐19 infection counts at the peaks of the first and second waves of the pandemic.
In a series of sensitivity analyses, we re‐estimate our models in several ways: (a) using non‐standardized covariates, (b) removing health regions in Toronto and Montreal from our sample (to check whether these two especially hard‐hit urban centers are driving our results), (c) modeling cumulative infection rates (per 100,000) instead of counts, (d) using negative binomial regression instead of Poisson models, and (e) substituting the percent Black with the percent Asian and the percent visible minority. The results, which are available in Tables A1‐A3 of the appendix, are generally similar to those we present in the main text and illustrate considerable heterogeneity among Asian subgroups and visible minority groups.
Second, we identify COVID‐19 hotspots across Canada by predicting the relative number of infections at a more granular geographic level than health regions. To generate the predicted number of infections at the community level, we use (a) the coefficients describing the relationship between the measures of the demographic composition of health regions and COVID‐19 infections from Table 2, and (b) information about the demographic composition of the pseudo‐CSDs. We then use the predicted counts to partition the actual number of COVID‐19 infections in a health region across its constituent communities.
Table 2.
Poisson regression models predicting cumulative COVID‐19 infections among health regions
| Peak of first wave | Peak of second wave | |||
|---|---|---|---|---|
| (April 20th) | (January 10th) | |||
| Standardized Covariates | β | β/se | β | β/se |
| Percent Black | 0.33*** | 46.70 | 0.10*** | 62.15 |
| Percent foreign‐born | −0.37*** | −37.73 | 0.21*** | 97.68 |
| Percent low‐income | 0.25*** | 22.72 | 0.16*** | 71.37 |
| Percent working in health industry | −0.31*** | −25.43 | 0.08*** | 31.87 |
| Percent w/bachelor's degree or more | 0.15*** | 14.78 | −0.01*** | −5.66 |
| Percent 65+ years | −0.06*** | −4.58 | −0.51*** | −195.23 |
| Population density | 0.13*** | 18.91 | 0.08*** | 55.42 |
| Urban center (Rural) | ||||
| Semi‐urban | 1.27*** | 35.49 | 0.54*** | 75.98 |
| Urban | 2.17*** | 63.02 | 1.45*** | 223.82 |
| Intercept | 3.98*** | 129.96 | 7.50*** | 1365.77 |
| N | 89 | |||
Notes: Data come from the University of Toronto's COVID‐19 Canada Open Data Working Group Dashboard and Statistics Canada's 2016 census tabular estimates. Covariates are standardized. Separate models are run for two time points: the cumulative count of COVID‐19 infections at the peak of the pandemic's first wave (April 22, 2020) and at the peak of the second wave (November 3, 2020). Statistical significance is indicated by: * p < .05, ** p < .01, *** p < .001. .
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Toronto analyses
Rather than relying simply on analyses at a high level of geographic aggregation (i.e., health regions), we replicate our analyses in a single, uniquely hard‐hit city. Specifically, we examine the association between cumulative COVID‐19 infections and demographic composition across 140 neighbourhoods in Toronto. We would not necessarily expect that results about health regions across Canada would also obtain for neighbourhoods in one specific city. At the same time, by focusing on smaller, less heterogeneous, and more meaningful geographic areas (i.e., neighbourhoods) in Toronto, we can more directly test how the social composition is associated with communities’ vulnerability to the present pandemic. This Toronto‐specific analysis also helps provide some face validity to our use of relationships at the health region level to predict cases at lower geographic units (i.e., pseudo‐CSDs). In these ways, we balance the trade‐offs between the national scope afforded by our main analyses of health regions, and the ability to examine more local dynamics in a city.
Three features of the City of Toronto make it an appealing test case. First, Toronto has been especially hard hit by the pandemic, trailing only Montreal in terms of infection and death rates. Since early March 2020, there have been over 25,000 infections and nearly 1,400 COVID‐19‐related deaths in the city. In mid‐April, the number of new infections peaked at around 300 new cases per day. While the rate of new infections slowed by late July, a fresh wave emerged in early October. Second, Toronto is organized into 140 geographically and politically meaningful neighbourhoods. The neighbourhood boundaries are based on Statistics Canada's census tracts and they follow natural and built impediments such as rivers, train tracks, and major roads. Each neighbourhood is comprised of two to five tracts and has an average of approximately 20,000 residents (range: 7,000 to 70,000). Politically, the municipal government and community agencies utilize these neighbourhoods to assist with the planning and delivery of services (City of Toronto, 2014, 2015). Third, information about both demographic composition and COVID‐19 cases is available at the neighbourhood level.
We use the same measures as our analyses at the health region level. Neighbourhood‐level counts of COVID‐19 infections are obtained from Toronto Public Health, and information about neighbourhoods' demographic composition comes from the City of Toronto's open data catalogue. The City computes their population estimates using the 2016 census. Also, as with the health regions, we estimate separate Poisson regression models predicting the cumulative count of COVID‐19 infections at two time points: the peaks of the first and second waves (on April 20 and January 10, 2021, respectively). In Table A4 of the Appendix, we present results for Toronto using negative binomial regression models rather than Poisson regression.
FINDINGS
Assessing the social determinants of Covid‐19 among health regions
Table 2 presents the results from Poisson regression models predicting cumulative COVID‐19 infections among 89 of Canada's health regions at the peak of the first wave (April 20, 2020) and at the peak of the second wave (January 10, 2021). COVID‐19 infections are higher in health regions with higher shares of Black and low‐income residents. Population density and urban centers are also positively correlated with COVID‐19 infections. COVID‐19 infections were lower in health regions with lower shares of foreign‐born residents during the first wave, but higher during the second wave. The same pattern obtains for the share of residents working in the health care industry.
Somewhat surprisingly, the share of adults at least 65 years old is negatively associated with COVID‐19 infections. This pattern likely emerges because (a) health regions with higher shares of adults at least 65 years old tend to be rural areas, (b) most COVID‐19 cases in this age group occurred among those at least 80 years old who are a small segment of this population, and (c) the elderly went to greater lengths to adhere to public health mitigation strategies once they found out that their risk of developing more severe forms of COVID‐19 and dying from COVID‐19 is higher than that of younger individuals (Seglins et al., 2020). In earlier versions of our paper, we found that health regions with higher shares of adults at least 65 years old had significantly higher mortality rates (available upon request).
Similarly, the share of residents with at least a bachelor's degree is positively related to COVID‐19 infections during the first peak of the pandemic, and negatively associated during the second peak. The initial positive association likely reflects the fact that (a) health regions are large and heterogeneous geographic units and (b) those with postsecondary education are more likely to be living in urban centers within the health region where there have also been more COVID‐19 infections. These unexpected patterns highlight the importance of collecting COVID‐19 data for smaller geographic units so that we can fully control for important social and spatial risk factors, such as urban/rural status.
Are these patterns driven by either the high numbers of COVID‐19 infections or the relatively large shares of Black and low‐income residents in urban centers like Toronto and Montreal? When we re‐estimate our models from Table 2 excluding health regions in Toronto and Montreal from the sample (see Panel C of Table A1 in the Appendix), our core results generally hold. This suggests that these broad patterns in the spread of the pandemic—as well as COVID‐19′s particular impact on areas with greater shares of certain groups—have been national in scope.
Predicting COVID‐19 hotspots among communities
Next, we use the relationships between health regions’ COVID‐19 infections and demographic composition from the Poisson regression results (Table 2) as well as the demographic composition of pseudo‐CSDs to predict the prevalence of COVID‐19 at a more local level of geography. Figure 1 contrasts observed counts across health regions with our predicted counts at the more local level of communities in both the first and second peaks of the pandemic. We categorize health regions and pseudo‐CSDs by cumulative infection terciles in the maps.
Figure 1.
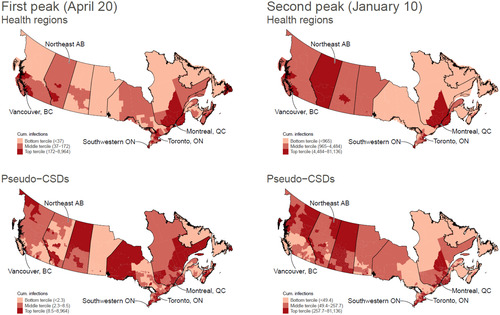
COVID‐19 infections in health regions and pseudo‐census subdivisions. Data: University of Toronto's COVID‐19 Canada Open Data Working Group Dashboard and Statistics Canada's 2016 census tabular estimates. Notes: Top panel shows the observed number of infections across health regions; bottom panel shows predicted infection counts across census subdivisions and divisions. Figures on the left plot infections during the first peak of the pandemic (April 20, 2020); figures on the right plot infections during the second peak (January 10, 2021). Provinces our outlined in black [Color figure can be viewed at wileyonlinelibrary.com]
Focusing first on the top panel of Figure 1, which illustrates the observed number of cumulative COVID‐19 infections across health regions, we can see that cases were high in both waves of the pandemic in Canada's largest cities, including Vancouver, Toronto, and Montreal. While only southern Alberta (which includes Calgary) was in the top tercile of cumulative COVID‐19 infections at the peak of the first wave, the entire province falls in this tercile in the second wave.
Comparing the top and bottom panels in Figure 1, it is clear that focusing on geographically large and socio‐demographically heterogeneous areas (i.e., health regions) masks a lot of variation in the spread and distribution of COVID‐19. Results for smaller geographic units in the bottom panel (that is, our predicted infection counts among census subdivisions and divisions) reveal urban/rural differences in COVID‐19 infections between southwest Alberta near Calgary and southeast Alberta. Northeastern Alberta and Northern Saskatchewan have also experienced high numbers of COVID‐19 infections—a pattern hidden in both the first and second waves of the pandemic by averaging their high caseload across the large health region spanning all of the northern parts of the province. Northeastern Alberta is home to large numbers of temporary migrant workers living in tight quarters while they work in the oil sands, conditions ripe for the spread of an infectious disease like COVID‐19. There is considerable travel across these two regions due to their geographic proximity. The bottom panel of Figure 1 also highlights large numbers of COVID‐19 infections in southern and southwestern Ontario along the border with Michigan and Minnesota—communities with high shares of Black, immigrant, and low‐income populations.
Focusing on the social determinants of COVID‐19 in Toronto
We turn now to our analysis of Toronto. Table 3 presents descriptive statistics for variables measuring the demographic composition of Toronto's 140 neighbourhoods. Comparing Tables 1 and 3, we see that Toronto is much more ethno‐racially and socioeconomically diverse than Canada generally. On average, 8.8 percent of residents in Toronto's neighbourhoods are Black, 48.7 percent are foreign‐born, and 16.9 percent are low‐income, compared to less than 1.0 percent, 8.7 percent, and 5.2 percent, respectively, among Canada's pseudo‐CSDs. A higher share of Torontonians has attained some postsecondary education: 43.6 percent of residents of Toronto compared to roughly 20 percent of those living elsewhere.
Table 3.
Descriptive statistics of Toronto's neighbourhoods
| Mean | SD | Min | Max | |
|---|---|---|---|---|
| Percent Black | 8.8 | 7.7 | 0.9 | 35.4 |
| Percent foreign‐born | 48.7 | 14.1 | 22.1 | 76.3 |
| Percent low‐income | 16.9 | 6.7 | 4.1 | 36.4 |
| Percent working in health industry | 5.8 | 1.6 | 2.7 | 12.5 |
| Percent w/bachelor's degree or more | 43.6 | 17.0 | 11.3 | 79.0 |
| Percent 65+ years | 16.0 | 4.2 | 4.8 | 28.0 |
| Population density | 6261.1 | 4840.4 | 1040.0 | 44321.4 |
| N | 140 | |||
Notes: Data come from Toronto Public Health and Toronto's Open Data Catalogue.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
How are these demographic factors related to COVID‐19 infections across Toronto's neighbourhoods? In Figure 2, we divide Toronto's neighbourhoods into terciles based on their percentage of residents who are Black, and we illustrate the cumulative number of COVID‐19 infections among these groups between January 21, 2020, and January 24, 2021. Early in the pandemic, until about March 10, there were virtually no differences in the number or spread of COVID‐19 infections across Toronto's neighbourhoods. However, as the City approached the peak of the first wave in April, the virus spread considerably faster in neighbourhoods with the highest share of Black residents. During the second wave, which has proven worse than the first, the gap continued to grow between neighbourhoods with relatively higher versus lower shares of Black residents. Indeed, a wider gap emerged between neighbourhoods in the middle and lowest terciles as well. By the peak of the second wave in early January, there were 26,528 more infections in neighbourhoods with the highest share of Black residents relative to neighbourhoods with the lowest share.
Figure 2.
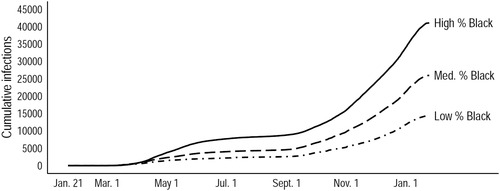
Cumulative count of COVID‐19 infections in the 140 neighbourhoods in the City of Toronto, by percent Black terciles, Data: Toronto Public Health and Toronto's Open Data Catalogue. Notes: The 140 neighbourhoods in the City of Toronto are divided into categories based on terciles of the percent of its residents who are Black
Table 4 presents a more systemic examination of the relationship between cumulative COVID‐19 infections at the peaks of the first and second waves of the pandemic and the demographic composition of Toronto's 140 neighbourhoods. We estimate Poisson regression models similar to those in Table 2. As in our health region analysis, the share of Black residents in a neighbourhood is positively and significantly related to the number of COVID‐19 infections. The higher number of COVID‐19 infections in neighbourhoods with higher shares of Black residents is not simply due to other demographic factors such as the share of foreign‐born or socioeconomically disadvantaged residents. This relationship exists independent of these other measures.
Table 4.
Poisson regression models predicting cumulative COVID‐19 infections among Toronto's neighbourhoods
| Peak of first wave | Peak of second wave | |||
|---|---|---|---|---|
| (Apr. 20, 2020) | (Jan 1th, 2021) | |||
| Standardized Covariates | β | β/se | β | β/se |
| Percent Black | 0.23*** | 10.87 | 0.11*** | 19.66 |
| Percent foreign‐born | 0.29*** | 12.82 | 0.47*** | 74.27 |
| Percent low‐income | −0.08*** | −3.50 | −0.17*** | −26.36 |
| Percent working in health | 0.08*** | 4.38 | 0.04*** | 7.96 |
| Percent w/bachelor's degree or more | 0.00 | 0.11 | −0.18*** | −23.18 |
| Percent 65+ years of age | −0.05** | −2.69 | −0.18*** | −35.72 |
| Population density | 0.08*** | 5.88 | −0.01** | −2.79 |
| Intercept | 3.59*** | 246.62 | 6.10*** | 1417.75 |
Notes: Data come from Toronto Public Health and Toronto's Open Data Catalogue. Covariates are standardized. Separate models are run for two time points: the cumulative count of COVID‐19 infections at the peak of the pandemic's first wave (April 10, 2020) and at the peak of the second wave (January 10th, 2021). Statistical significance is indicated by: * p < .05, ** p < .01, *** p < .001.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Furthermore, while some relationships between other demographic factors and COVID‐19 cases are generally consistent with the results from our health region models in Table 2, others are different. The negative relationship between percent of residents with at least a bachelors’ degree and COVID‐19 cases at the peak of the second wave highlights the protective nature of education and social class in Toronto's neighbourhoods, including the ability of individuals with postsecondary degrees to have the types of jobs that allows them to work from home (Messcar et al., 2020). Discrepancies between the results from our analyses of health regions and Toronto neighbourhoods also underscore the fact that health regions may be too large to adequately capture the true impact of the educational composition of one's neighbourhood of residence, stressing the need for the collection of COVID‐19 data at a more granular level. Finally, neighbourhoods with higher shares of foreign‐born residents also experience higher COVID‐19 infection counts. This could reflect the fact that Toronto is an immigrant gateway city; as such, a higher share of its foreign‐born population has limited English proficiency, lower health care utilization rates, and fewer socioeconomic resources at their disposal (Chadwick & Collins, 2015; Kirkman‐Liff & Mondragón, 1991; Yu et al., 2007).
Taken together, the results from Toronto show that several demographic factors operate similarly and highlight the unique vulnerability of areas with higher shares of Black residents. At the same time, the differences between neighbourhoods in Toronto and health regions in Canada overall underscore the limitations and biases of not having nationally consistent, available, and detailed demographic information about victims of the pandemic.
CONCLUSION
While the pandemic has affected Canadians across all communities and backgrounds, some groups have been hit particularly hard by COVID‐19. Yet the absence of race‐based and other socio‐demographic data related to COVID‐19 infections and deaths prevents researchers from identifying who is the most vulnerable and why these vulnerabilities emerge. We fill this void by combining information about COVID‐19 cases with tabular census data to (a) identify population risk factors associated with the virus's spread and (b) pinpoint potential COVID‐19 hotspots among smaller geographic communities.
Similar to the U.S. and U.K., urban regions in Canada with higher shares of Black residents have been disproportionately impacted by COVID‐19. This may help explain why places like Toronto and Montreal, with relatively large numbers of Black Canadians and Black immigrants, have emerged as epicenters of the pandemic in Canada. At the same time, these results are not due simply driven by these two cities (as our analysis in Table A1 excluding Toronto and Montreal from the sample shows), nor does this relationship emerge solely due to socioeconomic disadvantage (as we also control for the share of low‐income residents in an area). These results may be surprising to those who believe that racial discrimination against Black communities is less severe, and as such, Blacks are not as disadvantaged in Canada as they are elsewhere like the U.S. (Reitz & Banerjee, 2007; Simpson, 2019). These findings further underscore the importance of systematically examining racial and ethnic inequalities in health in the Canadian context where many public health officials and politicians have not seen the need to collect racial data on grounds that documenting health inequality by race/ethnicity may lead to discrimination (Mulligan et al., 2020; Siddiqi et al., 2020).
In the health region analysis, the association between the percentage of foreign‐born and the number of COVID‐19 infections is negative in the first wave but positive in the second wave (see Table 2). By contrast, this association is positive in both waves of the Toronto‐specific neighbourhood analysis (see Table 4). These contrasting findings are in line with findings from Statistics Canada (Subedi et al., 2020) that regional variation in the concentration of particular immigrant groups with differential levels of vulnerability to COVID‐19 may have partially contributed to geographic differences in COVID‐19 rates (e.g., East Asians in British Columbia vs. Black immigrant groups in Toronto and Montreal). 7 These findings also highlight the limitations of examining associations among large, socially heterogeneous areas like health regions, within which the resources and experiences of immigrants are likely to vary.
Indeed, we find that collecting COVID‐19 data at larger units of geography (such as health regions) masks important heterogeneity within these areas, such as urban/rural differences in the severity of the spread in COVID‐19. The hotspots we identify in Figure 2—which use the relationships between demographic composition and COVID‐19 infections among health regions, as well as the demographic composition of pseudo‐CSDs—align with media reports of especially severe outbreaks and help suggest reasons for why outbreaks occur where they do. For instance, the high number of infections in northeastern Alberta may be attributable to the prevalence of industries that employ large numbers of immigrant workers and house them in close group quarters (Taylor, 2020).
We recognize that our study has some limitations. First, we rely on the aggregate data about the demographic composition of communities to infer traits about individual residents. This approach could lead to ecological fallacies. Just because one lives in a geographic region or neighbourhood with relatively high shares of racial minorities or lower‐income residents does not mean that they are a racial minority or low‐income. Given the high level of aggregation—whether we are talking about large health regions or even smaller neighbourhoods—the approach on which we and others rely does not allow researchers or policymakers to specifically get at which individuals are at a higher risk of infection and systematically assess why these individuals have a higher risk of infection. However, only a subset of Canadian provinces has collected and made available data on individual COVID‐19 patients or has broken‐down case counts by demographic groups (Allen, 2020; Blair et al., 2020). Second, the “health region” is the smallest geographic unit for which COVID‐19 data are consistently and publicly available across Canada. When we predicted infection counts at smaller levels of geography using our health‐region‐level results, we assumed that the risk factors associated with COVID‐19 infections do not vary across communities within health regions. Third, our reliance on public‐use tabular census data precludes us from considering several potentially vulnerable groups, such as temporary migrants and the age‐ and gender‐specific distributions of different populations. Finally, we rely on official counts of COVID‐19 cases. Borjas (2020) found that testing rates were lower among residents of minority and low‐income neighbourhoods in New York City. As a result, we may be underestimating the severity of COVID‐19 in such communities in Canada.
If we know more about which groups are especially susceptible to COVID‐19, and more importantly why certain groups have experienced higher rates of infection and mortality, policies and interventions designed to combat its spread and address the social, psychological, and material consequences of the pandemic can be better targeted and ensure that no one is left out of the national, provincial, and more local responses. Such information might also suggest policies that go beyond combatting the current pandemic, and help to address the long‐standing inequalities highlighted and made worse by the pandemic. This includes more diversity training, better policies to target racial discrimination, more equal access to health care, less crowded and better‐quality housing, investments in neighbourhood infrastructure (like better walkability and more open spaces), and rethinking the nature of and supports for work in Canada. We hope that our findings highlight the importance of systematically collecting and analyzing race‐based data, rather than relying on our perceptions of what Canada should be.
Supporting information
Supporting Information
ACKNOWLEDGEMENTS
An earlier version of this paper was presented in the Centre for Population Dynamics at McGill University in June 2020. We gratefully acknowledge funding from the Social Sciences and Humanities Research Council (Grant 430‐2017‐00920).
Denice P., Haan M., Zajacova A. & Choi K. H. Studying the social determinants of COVID‐19 in a data vacuum Canadian Review of Sociology/Revue canadienne de sociologie. 2021;58:146–164. 10.1111/cars.12336
Notes
Authors’ calculations of data from the Government of Canada's COVID‐19 Situational Awareness Dashboard (https://health‐infobase.canada.ca/covid‐19/dashboard/).
See https://www.toronto.ca/home/covid‐19/covid‐19‐latest‐city‐of‐toronto‐news/covid‐19‐status‐of‐cases‐in‐toronto (accessed on November 12, 2020). Note that there is much heterogeneity in COVID‐19 rates across visible minority groups.
There has been some positive change on this score more recently: The survey research firm Ipsos found that 60 percent of Canadians think that racism is a “serious problem” (Bricker, 2020). This represents an increase of nearly 13 percentage points since 2019 and a reversal of the declining trend over recent decades in the share of Canadians who believe racism is a serious problem (Simpson, 2019).
This community‐led data collection project can be found here: https://thecolorsofcovid.com/.
However, other research finds that native‐born Black Canadians report comparable or better health outcomes than native‐born White Canadians (Lebrun & LaVeist 2013).
Percent Asian is highly correlated with percent foreign‐born. Significant variation also exists in the COVID‐19 infection counts of Asian subgroups and the geographic distribution of Asian subgroups across Canada, precluding us from making use of percent Asian as the key independent variable.
Small sample sizes and multicollinearity precluded us from including multiple immigrant groups in our analysis without running into issues of multicollinearity. In supplementary analyses (available upon request), we examine the association between specific immigrant groups and COVID‐19 cases.
REFERENCES
- Adelson N. (2005) The embodiment of inequity: Health disparities in aboriginal Canada. Canadian Journal of Public Health, 96(2), S45‐S61. 10.1007/BF03403702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Always Designing for People (ADP) . (2020) New ADP survey shows Canadians believe workplaces have work to do on diversity and inclusion. ADP. Available at: https://adp‐ca‐origin.adp.com/‐/media/adpca/redesign2019/pdf/adp‐canada‐release‐survey‐on‐diversity‐and‐inclusion‐in‐the‐workplace.pdf?la=en&hash=2813C7F3FDAB60526FF9837C45483E8D78B60784 [Google Scholar]
- Allen, K. (2020) Ontario is starting to collect race‐based COVID‐19 data. some worry that it could do more harm than good. Toronto Star, July 2. Available at: https://www.thestar.com/news/gta/2020/07/02/ontario-is-starting-to-collect-race-based-covid-19-data-some-worry-it-could-domore-harm-than-good.html [Accessed 5th July 2020]. [Google Scholar]
- Attewell P., Kasinitz P. & Dunn K. (2010) Black Canadians and Black Americans: Racial income inequality in comparative perspective. Ethnic and Racial Studies, 33(3), 473‐495. 10.1080/01419870903085883 [DOI] [Google Scholar]
- Soroka, S.N. , Johnston, R. & Banting, K. (2007) Ties That Bind? Social Cohesion and Diversity in Canada. In: Banting, K. , Courchene, T. , & Seidle, F.L. (Eds). Belonging? Diversity, recognition, and shared citizenship in Canada. Montreal, QC: Institute for Research on Public Policy. [Google Scholar]
- Berry I., Soucy J.‐P.R., Tuite A. & Fisman D. (2020) Open access epidemiologic data and an interactive dashboard to monitor the COVID‐19 outbreak in Canada. Canadian Medical Association journal"> Canadian Medical Association journal, 192(15), E420–E420. 10.1503/cmaj.75262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhala N., Curry G., Martineau A.R., Agyemang C. & Bhopal R. (2020) Sharpening the Global Focus on Ethnicity and Race in the Time of COVID‐19. The Lancet, 395(10238),1673‐1676. 10.1016/S0140-6736(20)31102-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair, A. Warsame, K. Naik, H. Byrne, W. , Parnia, A. & Siddiqi, A. (2020) Identifying gaps in COVID‐19 health equity data reporting in Canada using a scorecard approach. Canadian Journal Public Health. Available at: 10.17269/s41997-021-00496-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd, A. (2020). Race‐based Coronavirus data not needed in Canada yet, health officials say. Toronto Star, April 10. Available at: https://www.thestar.com/news/canada/2020/04/10/race-based-coronavirus-data-not-needed-in-canada-yet-health-officials-say.html [Accessed 5th July 2020] [Google Scholar]
- Boyd, M. , Goldmann, G. & White, P. (2000) Race in the Canadian Census. In: Dreidger, L. & Hali, S. (Eds.) Visible minorities: Race and racism in Canada. Ottawa, ON: Carleton University Press, pp. 98–120. [Google Scholar]
- Bricker, D. (2020) Majority see racism as a serious problem in Canada Today, Up 13 points since last yea r. Factum. Toronto, ON: Ipsos. [Google Scholar]
- Chadwick K.A. & Collins P.A. (2015) Examining the relationship between social support availability, urban center size, and self‐perceived mental health of recent immigrants to Canada: A mixed‐methods analysis. Social Science & Medicine, 128, 220‐230. 10.1016/j.socscimed.2015.01.036 [DOI] [PubMed] [Google Scholar]
- Chanchlani N., Buchanan F. & Gill P.J. (2020) Addressing the indirect effects of COVID‐19 on the health of children and young people. Canadian Medical Association journal, 192(32), E921‐E927. 10.1503/cmaj.201008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin M., Kane T.J., Kozakowski W., Schueler B.E. & Staiger D.O. (2019) School district reform in Newark: Within‐ and between‐school changes in achievement growth. ILR Review, 72(2), 323–354. 10.1177/0019793918774318 [DOI] [Google Scholar]
- City of Toronto. TSNS 2020 neighbourhood equity index: methodological documentation. (2014) Available at: https://www.toronto.ca/wp‐content/uploads/2017/11/97eb‐TSNS‐2020‐NEI‐equity‐index‐methodology‐research‐report‐backgroundfile‐67350.pdf
- City of Toronto. (2015) Toronto strong neighbourhoods strategy 2020. Available at: https://www.toronto.ca/city‐government/accountability‐operations‐customer‐service/long‐term‐vision‐plans‐and‐strategies/toronto‐strong‐neighbourhoods‐strategy‐2020/
- Denice P., Choi K.H., Haan M. & Zajacova A. (2020) Visualizing the geographic and demographic distribution of COVID‐19. Socius, 6, 237802312094871. 10.1177/2378023120948715 [DOI] [Google Scholar]
- Gilmour, M. & Ross, S. (2020) After promising to release race‐based COVID‐19 data, Quebec has changed its mind. CTV News, August 19. [Google Scholar]
- Hou, F. , Frank, K. & Schimmele, C. (2020). Economic impact of COVID‐19 among visible minority groups. 45280001. Ottawa, ON: Statistics Canada. [Google Scholar]
- James, L. (2020) Race‐based COVID‐19 data may be used to discriminate against racialized communities. The Conversation, September 14. Available at: https://theconversation.com/race-based-covid-19-data-may-be-used-to-discriminateagainst-racialized-communities-138372 [Accessed 30th September 2020] [Google Scholar]
- Jones, A. (2020). Canadian university students create map of self‐reported potential COVID‐19 cases. CTV News, March 27. [Google Scholar]
- Kirkman‐Liff B. & Mondragón D. (1991) Language of interview: Relevance for research of Southwest Hispanics. American Journal of Public Health, 81(11), 1399–1404. 10.2105/ajph.81.11.1399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwak, J.A. (2020) Opinion: Why Canada's Decision to Exclude Race from COVID‐19 Statistics Is Fundamentally Flawed. McGill Journal of Political Studies. Available at: https://mjps.ssmu.ca/2020/06/17/opinion-why-canadas-decision-to-exclude-race-from-covid-19-statistics-is-fundamentallyflawed/?utm_source=rss&utm_medium=rss&utm_campaign=opinion-why-canadas-decision-to-exclude-race-from-covid-19-statistics-is-fundamentally-flawed [Google Scholar]
- Lasser K. E., Himmelstein D. U. & Woolhandler S. (2006). Access to care, health status, and health disparities in the United States and Canada: Results of a cross‐national population‐based survey. American Journal of Public Health, 96(7), 1300–1307. 10.2105/AJPH.2004.059402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebrun L.A. & Laveist T.A. (2013). Health Status among Black Canadians: Results from a National Survey. Canadian Ethnic Studies /Études Ethniques Au Canada, 45, 143‐155. [Google Scholar]
- Lin, S.L. (2020). Intersectionality and inequalities in medical risk for severe COVID‐19 in the Canadian longitudinal study on aging. The Gerontologist, gnaa143. Advance online publication. 10.1093/geront/gnaa143 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Lemieux T., Milligan K., Schirle T. & Skuterud M. (2020) Initial Impacts of the COVID‐19 Pandemic on the Canadian Labour Market. Canadian Public Policy, 46(S1), S55–S65. 10.3138/cpp.2020-049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macias Gil R., Marcelin J.R., Zuniga‐Blanco B., Marquez C., Mathew T. & Piggott D. A. (2020) COVID‐19 Pandemic: Disparate Health Impact on the Hispanic/Latinx Population in the United States. Journal of Infectious Diseases, 222(10), 1592‐1595. 10.1093/infdis/jiaa474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahajan U.V. & Larkins‐Pettigrew M. (2020) Racial demographics and COVID‐19 confirmed cases and deaths: A correlational analysis of 2886 US Counties. Journal of Public Health, 42(3), 445‐447. 10.1093/pubmed/fdaa070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariam, B. (2020). COVID‐19 Racial Data, Policy Needed for B.C. to Fight Inequality in Heath Care: Doctor. City News, November 8. [Google Scholar]
- Messacar, D. , Morissette, R. & Deng, Z. (2020) Inequality in the feasibility of working from home during and after COVID‐19. Available from: https://www150.statcan.gc.ca/n1/pub/45‐28‐0001/2020001/article/00029‐eng.htm
- Mignacca, F.G. (2020) Quebec is still not publishing race‐based data about COVID‐19. These Community Groups Aim to Fill the Void. CBC News, August 19, Available at: https://www.cbc.ca/news/canada/montreal/community-groups-launch-national-covid-19-race-database-1.5691937 [Accessed 20th August 2020]. [Google Scholar]
- Mulligan, K. , Rayner, J. & Nnorom, O. (2020) Race based data urgently needed during the pandemic. The Conversation, April 30. Available at: https://theconversation.com/race-based-health-data-urgently-needed-during-the-coronaviruspandemic-136822 [Accessed 5th July 2020]. [Google Scholar]
- Nath N. (2011) Defining narratives of identity in Canadian political science: Accounting for the absence of race. Canadian Journal of Political Science /Revue Canadienne de Science Politique, 44(1), 161‐193. [Google Scholar]
- Owusu‐Bempah A. & Millar P. (2010) Research note: Revisiting the collection of justice statistics by race in Canada. Canadian Journal of Law and Society, 25(1), 97‐104. [Google Scholar]
- Patel, R. (2020) Canada Must Improve COVID‐19 Data Collection for Indigenous Communities, Minister Says. CBC News, May 7. [Google Scholar]
- Ramos, H. (2020) Being counted in Canada's coronavirus data: stronger data collection is essential to understand how COVID‐19 impacts immigrants across Canada. New Canadian Media: The Pulse of Immigrant Canada, April 14. [Google Scholar]
- Reitz, J.G. & Banerjee, R. (2007) Racial Inequality, Social Cohesion, and Policy Issues in Canada. In: Banting, K. , Courchene, T. & Seidle, F . Belonging? Diversity, recognition, and shared citizenship in Canada. Montreal, QC: Institute for Research on Public Policy. [Google Scholar]
- Ruggles, S. , Flood, S. , Goeken, R. , Grover, J. , Meyer, E. , Pacas, J. et al. (2020) IPUMSUSA: Version 10.0 . Minneapolis, MN: IPUMS. Available at: 10.18128/D010.V10.0 </Dataset> [DOI] [Google Scholar]
- Seglins, D. , Wesley, A. & Rocha, R. (2020) We looked at every confirmed COVID‐19 case in Canada. Here's what we found. CBC News, September 22. Available at: https://www.cbc.ca/news/canada/public-health-agency-of-canada-covid-19-statistics-1.5733069 [Accessed 24th September 2020]. [Google Scholar]
- Siddiqi, A. , Blair, A. & Parnia, A. (2020) A lack of data hides the unequal burden of COVID‐19 . Toronto Star, April 16. Available at: https://www.thestar.com/opinion/contributors/2020/04/16/a-lack-of-data-hides-the-unequal-burden-of-covid-19.html [Accessed 5th July 2020]. [Google Scholar]
- Simpson, S. (2019) Global news racism. Ipsos Public Affairs. Available at: https://www.ipsos.com/sites/default/files/ct/news/documents/2019‐05/ipsos_global_news_‐_racism_‐_2019.pdf [Google Scholar]
- Singh, I. , Ivany, K. & Gilchrist, S. (2020) Why race‐based data collection by police could play a role in reform debate. CBC News, July 7. Available at: https://www.cbc.ca/news/canada/race-police-data-ontario-1.5636301 [Accessed 8th July 2020]. [Google Scholar]
- Stacey, M. (2020) Black lives matter seeks race‐related London data through survey. London Free Press, November 20. [Google Scholar]
- Statistics Canada . (2019). Diversity of the Black population in Canada: An overview. Available at: https://www150.statcan.gc.ca/n1/en/pub/89‐657‐x/89‐657‐x2019002‐eng.pdf?st=g1VVke6J
- Statistics Canada . (2020). Labor Force Survey, (August 2020). Available at: https://www150.statcan.gc.ca/n1/daily‐quotidien/200904/dq200904a‐eng.pdf
- Statistics Canada . (2017). Population Centre. Available at: https://www12.statcan.gc.ca/census‐recensement/2016/ref/dict/geo049a‐eng.cfm
- St‐Denis X. (2020) Sociodemographic determinants of occupational risks of exposure to COVID‐19 in Canada. Canadian Review of Sociology/Revue Canadienne de Sociologie, 57(3), 399–452. 10.1111/cars12336.12288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subedi, R. , Greenberg, L. & Turcotte, M. (2020) COVID‐19 mortality rates in Canada's ethno‐cultural neighbourhoods. Available at: http://publications.gc.ca/collections/collection_2020/statcan/45‐28/CS45‐28‐1‐2020‐79‐eng.pdf
- Sze S., Pan D., Nevill C.R., Gray L.J., Martin C.A., Nazareth J., Minhas J.S., Divall P., Khunti K., Abrams K.R., Nellums L.B. & Pareek M. (2020). Ethnicity and clinical outcomes in COVID‐19: A systematic review and meta‐analysis. EClinical Medicine, 29‐30, 100630. Available from: https://www.thelancet.com/action/showPdf?pii=S2589‐5370%2820%2930374‐6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, S. (2020). COVID 19 outbreak in Northern Saskatchewan ‘of Concern’ Says Canada's Chief Health Officer. Global TV News, May 6. Availability at: https://globalnews.ca/news/6912579/covid-19-outbreak-saskatchewan-dr-theresa-tam/ [Accessed 9 May 2020]. [Google Scholar]
- Thebault, R. , Tran, A. & Williams, V. (2020) The Coronavirus is infecting and killing Black Americans at an alarmingly high rate. The Washington Post, April 7. Available at: https://www.washingtonpost.com/nation/2020/04/07/coronavirus-is-infecting-killingblack-americans-an-alarmingly-high-rate-post-analysis-shows/ [Accessed 10 April 2020]. [Google Scholar]
- Thompson D. (2008) Is Race Political? Canadian Journal of Political Science /Revue Canadienne de Science Politique, 41(3), 525–547. [Google Scholar]
- Thorpe, R. (2020) Suffering in the dark. Winnipeg Free Press, November 13. [Google Scholar]
- Veenstra G. (2009) Racialized identity and health in Canada: Results from a nationally representative survey. Social Science & Medicine, 69(4), 538‐542. 10.1016/j.socscimed.2009.06.009 [DOI] [PubMed] [Google Scholar]
- Veenstra G. & Patterson A.C. (2016) Black‐White health inequalities in Canada. Journal of Immigration and Minority Health, 18(1), 51–57. [DOI] [PubMed] [Google Scholar]
- Yancy C. W. (2020) COVID‐19 and African Americans. Jama, 323(19), 1891. 10.1001/jama.2020.6548 [DOI] [PubMed] [Google Scholar]
- Yu S., Ouellet E. & Warmington A. (2007) Refugee integration in Canada: A survey of empirical evidence and existing services. Refuge: Canada's Journal on Refugees, 17–34. 10.25071/1920-7336.21381 [DOI] [Google Scholar]
- Zajacova A., Jehn A., Stackhouse M., Choi K. H., Denice P., Haan M. & Ramos H. (2020a) Mental health and economic concerns from March to May during the COVID‐19 pandemic in Canada: Insights from an analysis of repeated cross‐sectional surveys. SSM ‐ Population Health, 12, 100704. 10.1016/j.ssmph.2020.100704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova A., Jehn A., Stackhouse M., Denice P. & Ramos H. (2020b) Changes in health behaviours during early COVID‐19 and socio‐demographic disparities: A cross‐sectional analysis. Canadian Journal of Public Health, 111, 953‐962, 10.17269/s41997-020-00434-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


