Abstract
We use data from the UK Household Longitudinal Study (UKHLS) to compare measures of socioeconomic inequality in psychological distress, measured by the General Health Questionnaire (GHQ), before (Waves 9 and the Interim 2019 Wave) and during the first wave of the COVID‐19 pandemic (April to July 2020). Based on a caseness measure, the prevalence of psychological distress increased from 18.5% to 27.7% between the 2019 Wave and April 2020 with some reversion to earlier levels in subsequent months. Also, there was a systematic increase in total inequality in the Likert GHQ‐12 score. However, measures of relative socioeconomic inequality have not increased. A Shapley‐Shorrocks decomposition analysis shows that during the peak of the first wave of the pandemic (April 2020) other socioeconomic factors declined in their share of socioeconomic inequality, while age and gender account for a larger share. The most notable increase is evident for younger women. The contribution of working in an industry related to the COVID‐19 response played a small role at Wave 9 and the Interim 2019 Wave, but more than tripled its share in April 2020. As the first wave of COVID‐19 progressed, the contribution of demographics declined from their peak level in April and chronic health conditions, housing conditions, and neighbourhood characteristics increased their contributions to socioeconomic inequality.
Keywords: COVID‐19, GHQ, health equity, mental health, psychological distress, socioeconomic inequality
1. INTRODUCTION
Has the experience of the COVID‐19 pandemic in the UK had a greater impact on psychological distress among those in more disadvantaged pre‐existing circumstances and hence widened socioeconomic inequalities? The UK Household Longitudinal Study (UKHLS), Understanding Society, launched a COVID‐19 survey to examine the impact of the coronavirus pandemic on UKHLS participants. The release of these data provides an opportunity to address this question. The survey has been sent to adult UKHLS participants once a month with the first release collected in April 2020 (Institute for Social and Economic Research, 2020). We use data from UKHLS Wave 9 and the Interim 2019 Wave, along with the April 2020 and three subsequent releases of the COVID‐19 web survey to compare measures of socioeconomic inequality in mental health. Mental health is measured by the General Health Questionnaire (GHQ), which captures 12 indicators of psychological distress. This allows us to compare the distribution of GHQ before and during the first wave of the pandemic in the UK.
COVID‐19 originated in the city of Wuhan, China, in December 2019 and spread rapidly to become a global pandemic. Wednesday 29th January saw the first two patients test positive for COVID‐19 in the UK. On 11th March the UK Government announced its first package of financial support for those affected and on the same day the World Health Organisation (WHO) declared a global pandemic. The following week saw the announcement of a much larger financial package in the UK. The closure of pubs, restaurants, gyms and other social venues was announced on Friday 20th March and then on 23rd March a national lockdown was announced. This lockdown included the shielding on 1.5 million vulnerable people and the public as a whole were instructed to begin socially isolating and expected to stay at home. The exceptions to this were for essential workers and for non‐essential workers who were not able to work from home, shopping for essentials such as food and medical supplies, medical reasons, providing help to the vulnerable, and taking exercise once a day. It was not until 13th May that the first easing of lockdown was announced; two subsequent easings of lockdown were made on the 1st and 15th of June with a further easing on the 4th of July 1 .
By April 2020, when our new data were first collected, the UK appeared to be at the peak of the first phase of the pandemic. The direct impact of COVID‐19 on health and wellbeing had caused 20,283 COVID‐19 registered deaths in England and Wales up to 17th April. The pandemic highlighted existing socioeconomic inequalities in health and appears to have amplified the gradients in health by age, sex, ethnicity, income and wealth, education and housing. For example, the end of April coincided with the publication of evidence from the Office for National Statistics (2020a) that revealed a stark social gradient in the mortality rates associated with COVID‐19. Comparisons of data up to 17th April 2020 showed substantial socio‐geographic variation in death rates across local authorities in England and Wales 2 .
The nature of the economic and policy response to COVID‐19 has created specific gradients in both exposure to the disease itself and in exposure to the economic impact of the lockdown. These new or amplified facets of existing socioeconomic inequalities include, for example, those working in essential occupations (e.g., in health and social care and other public services), financial and employment hardship, the presence of children in households and living in multigenerational households or as lone parents. Moreover, other facets include the influence of housing and neighbourhood environment on people's ability to self‐isolate.
Beyond the direct impact of COVID‐19, the population as a whole has been exposed to the policy response to the pandemic. Lockdown, social distancing, self‐isolation, the economic impact of shut‐down of parts of the economy and the focusing of resources within the health and social care systems on coping with the pandemic may all have had an indirect impact on psychological distress and the mental health of the population (e.g., Haiyang et al., 2020). Given the characteristics of the policy and institutional responses outlined above, the burden of this psychological distress may have been unequally distributed within the population according to their pre‐existing circumstances. This is what we seek to explore in this paper.
To measure the impact of the UK response to the pandemic in terms of socioeconomic inequalities in health we build on methodological approaches that use the notion of equality of opportunity (e.g., Ramos & Van de Gaer, 2016; Roemer & Trannoy, 2016). The equality of opportunity perspective tends to focus on early life circumstances as the source of unfair or illegitimate inequalities in the outcome of interest. In this paper, we broaden that perspective and, to provide additional insights into the impact of the pandemic on socioeconomic inequity, we include factors that are specific to the policy debate concerning the adverse consequences of COVID‐19 for social inequality. In doing this we follow the spirit of Fleurbaey and Schokkaert (2009) and regard these factors, which were pre‐existing prior to the onset of the pandemic, as a source of unfair, or inequitable, variation in health outcomes. To put this approach into practice we use well‐established techniques that have been applied to the measurement of inequality of opportunity; we follow Davillas and Jones (2020), adapting and broadening their approach.
We compare the GHQ measure of psychological distress before (at UKHLS Wave 9 and at the 2019 Wave), at the peak of the initial phase of coronavirus (April 2020), and then in May, June and July 2020. The results show a substantial and systematic worsening of the levels of GHQ post‐COVID. This applies to nearly all of the individual elements of GHQ and to overall GHQ scores. For example, the prevalence of psychological distress based on the GHQ‐12 caseness scoring, increased from 18.5% at the 2019 Wave to 27.7% at the peak in April 2020. In addition, there is a statistically significant increase in total inequality in the Likert GHQ‐12 score between the data collected before and during the pandemic. However, we find no increase in relative socioeconomic inequality in April 2020 and subsequent months, suggesting that the proportion of total inequality attributed to observed circumstances has not increased with COVID‐19. A Shapley‐Shorrocks decomposition analysis allows us to explore the contribution of specific circumstances. During the peak of the UK response to the first wave of the pandemic (April 2020) key socioeconomic factors declined in their share of socioeconomic inequality and age and gender accounted for a larger share. As the pandemic progressed towards July 2020, the contribution of demographics declined from their peak levels and chronic health conditions, housing conditions, household composition and neighbourhood characteristics increased their contributions to socioeconomic inequality.
2. METHODS
2.1. Measuring socioeconomic inequality in psychological distress
We assume that the observed realisations of an individual's mental health can be expressed as:
| (1) |
where h is the specific mental health outcome of interest. In the language of inequality of opportunity, C are observed circumstances and E is a vector of efforts of inequality (which need not be observed) 3 . In the inequality of opportunity (IOp) literature these circumstances have typically been associated with early life circumstances. A broader interpretation is provided by Fleurbaey and Schokkaert's (2009) model of unfair health inequalities in which the C are defined generally as illegitimate, or unfair, sources of inequality and E as legitimate, or fair, sources of inequality. As described above, we take a broader view of the sources of socioeconomic inequalities that are regarded as a concern in the context of COVID‐19 and we define the list of observed circumstances accordingly; these circumstances are predetermined with respect to the COVID‐19 pandemic.
The specification of Equation (1) includes unobserved error terms to reflect that observed realisations of mental health outcomes are random; specifically, captures random variation in effort that is, independent of C, while captures random variation in outcomes, including any measurement error, that is, independent of C and E. Mental health outcomes are the realisations of a random process and we make no judgement about whether the unexplained component of these outcomes reflects unobserved circumstances, unobserved effort, measurement error or pure chance and, hence, whether the unexplained variation is legitimate or not 4 . Our focus is on measuring the component that can be attributed to the observed circumstance factors C.
Then, assuming additive separability and linearity of and , a linear reduced form can be derived (see e.g., Carrieri et al. (2020) for a derivation):
| (2) |
where the coefficients reflect the total contribution of circumstances and include both the direct contribution of circumstances and their indirect contribution through their influence on efforts 5 . Linearity may be regarded as a restrictive assumption but it is needed to derive the linear reduced form and hence to provide us with a tractable decomposition analysis and empirical results that are open to an intuitive interpretation. We follow Davillas and Jones (2020) and adopt an approach based on ex ante compensation and utilitarian reward that focuses on inequality in the distribution of mean outcomes conditional on observed circumstances 6 . In practice, the mean‐based direct parametric approach is based on using predictions of from the reduced form regression (2) as the counterfactual outcome:
| (3) |
These predicted outcomes are the same for all individuals with identical circumstances and all of the variation in is attributable to differences in their observed circumstances (Ferreira & Gignoux, 2011; Wendelspeiss Chávez Juárez & Soloaga, 2014) 7 . The level of observed socioeconomic inequality can be estimated using a suitable inequality measure, I (.), applied to the vector of counterfactual outcomes :
| (4) |
The fraction of the overall inequality in mental health functioning that is, attributed to observed socioeconomic inequality can be expressed as a percentage share of total inequality:
| (5) |
We present results for three sets of mental health outcomes, all derived from the GHQ. These measures are compared between UKHLS Wave 9 and the 2019 Wave, the COVID‐19 data for April 2020 and subsequent waves of the web survey.
The GHQ is a widely used instrument to measure non‐psychotic psychological distress and we use it to define three sets of outcomes. The first are binary indicators for each of the 12 questions that comprise the GHQ questionnaire (see Supplementary Appendix A for full details). These collapse the responses to the 12 dimensions of GHQ into, so‐called, caseness binary indicators. To measure , we apply the dissimilarity index to each of these 8 . These indicators allow us to explore inequalities in each of the GHQ dimensions and, thus, identify which of the dimensions of physiological distress were most affected by the response to the pandemic.
The second outcome is the level of GHQ‐12 measured on a continuous Likert scale that sums the 12 components of the GHQ. Previous studies have argued that the mean logarithmic deviation (MLD) or the variance are relevant inequality indexes to be used for continuous outcomes, depending on the nature of the outcome variable (e.g., Davillas & Jones, 2020; Carrieri et al., 2020; Ferreira & Gignoux, 2011, 2013; Wendelspeiss Chávez Juárez & Soloaga, 2014). As the Likert GHQ‐12 score is not a ratio‐scaled variable, the variance of is used as our main inequality measure (Carrieri et al., 2020; Wendelspeiss Chávez Juárez & Soloaga, 2014) 9 . Then the share of the socioeconomic inequality, , is measured by the share of the total variance in our continuous mental health measure that is attributed to observed circumstances. For comparison, we also provide results using the MLD inequality measure.
The third outcome is an indicator based on dichotomising the overall GHQ‐12 index, which is constructed by the caseness scoring method, using appropriate thresholds. To measure socioeconomic inequality the dissimilarity index is applied to this indicator.
As discussed above, for the level of GHQ‐12 Likert score, which is a continuous non‐ratio scale measure, we use the variance as our main inequality measure with:
| (6) |
where the predicted conditional means are estimated using linear regression models. For our binary outcomes, we use the dissimilarity index (Paes de Barros et al., 2007; Wendelspeiss Chávez Juárez & Soloaga, 2014):
| (7) |
where the predicted sample proportions are estimated using probit models.
2.2. Decomposing the socioeconomic inequality in health
We use a Shapley‐Shorrocks decomposition to measure the contribution of the measured circumstance variables (C) to overall socioeconomic inequality (Davillas & Jones, 2020; Deutsch, et al., 2018; Shorrocks, 2013; Wendelspeiss Chávez Juárez & Soloaga, 2014). This is implemented by computing the inequality index for all permutations of the circumstances and then averaging the marginal contribution of each circumstance. This Shapley‐Shorrocks decomposition is path independent and exactly additive (Wendelspeiss Chávez Juárez & Soloaga, 2014). The decomposition is applied to the variance share for the overall Likert GHQ‐12 score and to dissimilarity indices for the binary indicator of experiencing distress (based on the overall caseness GHQ‐12 index) both before and during the pandemic.
3. DATA
The individual level data on outcomes and circumstances come from Understanding Society (UKHLS), a longitudinal, nationally representative study of the UK. The UKHLS is a large, national representative panel survey, based on a two‐stage stratified random sample of the household population. For this study we use the General Population Sample (GPS) of the UKHLS, a representative sample for the residential population living in private households in the UK at the first wave in 2009‐10 10 . As far as possible, individuals from the first wave are retained as part of the sample so long as they live in the UK. Other individuals joining their households are included while they live with the original sample member. Circumstances are assumed to be predetermined and, thus, are all measured before the outcomes using variables drawn from Waves 1‐8 of UKHLS.
Our baseline outcomes are taken from the GHQ questionnaires at two UKHLS waves: first the UKHLS Wave 9, which collected data between January 2017 and May 2019 prior to the onset of the pandemic, and second the 2019 UKHLS Wave release (Institute for Social and Economic Research, 2020). The latter is an interim data release that contains responses from the UKHLS Waves 10 (year 2 sample) and 11 (year 1 sample), that is, responses from households issued for interviews in 2019 (given the UKHLS design involves overlapping 2‐years waves). The Interim Wave has been released along with the COVID‐19 UKHLS surveys and is designed to enable comparisons with the more recently collected COVID‐19 survey data. Given that the Interim Wave release contains those households assigned for an interview in 2019, the majority of the actual fieldwork took place in 2019, with a small number of interviews completed in February 2020 11 . Establishing that there are limited differences in mental health and the relevant socioeconomic inequalities across the two baseline waves (Wave 9 and the Interim Wave), for a period of about 3 years (2017–2019) before the COVID‐19 outbreak, makes comparisons to the period of the outbreak more striking.
Our potential sample contains UKHLS respondents with valid GHQ measures at Wave 9 and the 2019 Wave that provided information on all our circumstances from previous waves (mainly Wave 8 for the time‐varying circumstances and waves 1–8 for the time‐invariant measures). We also restrict our analysis to adults aged 20 and above, as there are concerns for the validity of GHQ‐12 for adolescents (e.g., Tait et al., 2002). This results in a potential maximum sample of 13,611 adults.
Since April 2020, selected participants from the UKHLS survey have been approached each month to complete short web‐surveys that focuses on the impact of the COVID‐19 pandemic (Institute for Social and Economic Research, 2020). Responses to the 12 questions that make up the GHQ are used as our outcomes from the COVID‐19 web surveys. The questionnaire's wording is identical to that at UKHLS Wave 9 and the 2019 Wave (see Supplementary Appendix A).
For the needs of this study, we focus on the general population sample respondents of UKHLS Wave 9 who are followed at the 2019 Wave, gave valid responses to the web‐based GHQ questionnaires at least once during the April, May, June or July COVID‐19 Waves and have valid data on all the circumstance variables used in our analysis (based on UKHLS Waves 1–8) 12 these COVID‐19 waves cover the first wave of the COVID‐19 outbreak in the UK, which is the focus of our study. This results in a maximum final working sample of 8,222 respondents that varies between Wave 9 and the subsequent waves. Unlike following a balanced sample of individuals over time, this design ensures that most of the available sample (subject to our selection criteria as described above) will be used at each wave.
To ensure that the results are nationally representative we use the Wave 9 cross sectional survey weights supplied with the UKHLS for the analysis of the baseline data (Wave 9 and 2019 Wave). To allow for unit non‐response at the April, May, June and July waves of the Covid‐19 survey, the selection of respondents who responded to Wave 9, Interim Wave and each of the subsequent waves of interest, and item non‐response for the GHQ questions, we use our own set of longitudinal weights. Specifically, we use a stepwise probit model for the probability of responding in each of the four COVID‐19 Waves among those in the Wave 9 and Interim 2019 Wave sample, using their observed circumstances as predictors. The predicted probabilities from these models are used to compute inverse probability weights that are then used to adjust the UKHLS base weights. This gives a set of four longitudinal weights used for the analysis of each of the COVID‐19 waves 13 . To assess the potential role of unequal selection and non‐response we estimate our inequality results without sample weights. The results are available in Supplementary Appendix C (Tables C4–C.6.) and comparisons to our base case results are briefly described in the Results section of the paper below.
3.1. Psychological distress outcomes (h)
Our analysis compares the level of socioeconomic inequality in the distribution of GHQ before and during the response to the pandemic. The GHQ instrument has been used to measure socioeconomic inequalities in mental health and, for example, the impact of the global financial crisis of 2008 on psychological distress (e.g., Maheswaran et al., 2015; Thomson et al., 2018). The Likert‐scaled GHQ‐12 is a widely used measure of non‐psychotic psychological distress with excellent psychometric properties (Bowling, 1991; Goldberg et al., 1997). Following the literature, we have also used a combined GHQ‐12 index that is based on the caseness scoring as an additional outcome (e.g., Maheswaran, et al., 2015). In addition, the questions on all 12 dimensions of the GHQ are used as separate outcomes in our analysis.
Specifically, the 12 dimensions of GHQ span concentration, loss of sleep, playing a useful role, ability to make decisions, coping under strain, overcoming difficulties, enjoying activities, facing problems, feeling depressed or unhappy, confidence, feeling worthless, and general happiness. Responses to the 12 dimensions are answered on a four‐category scale (‘not at all’, ‘no more than usual’, ‘rather more than usual’ and ‘much more than usual’). For each of the GHQ dimensions, the two categories indicating the most depressed states are coded as one and the remaining two categories, that reflect better mental health, are coded as zero (the caseness scoring).
We also use a single continuous index that combines all 12 dimensions (GHQ‐12). To create this index, we use a Likert scoring method that sums all 12 dimensions, which are scored from zero to three to reflect the four categories of each of the dimensions. This results in a single continuous GHQ‐12 index, ranging from 0 (least distressed) to 36 (most distressed). This allows us to treat GHQ‐12 as a pseudo‐continuous measure in our analysis (e.g., Davillas et al., 2016).
Following the literature, we have also used a combined GHQ‐12 index that is, based on the caseness scoring as an additional outcome (e.g., Maheswaran, et al., 2015). As the resulting GHQ index is characterised by spikes, the caseness scoring GHQ‐12 index is typically dichotomised to create an indicator for distress; in line with the literature (Maheswaran, et al., 2015), caseness GHQ‐12 is used as the threshold to define our dichotomous variable. We present analysis of socioeconomic inequality in all GHQ‐related outcomes at UKHLS Wave 9, the 2019 Wave and in all four COVID‐19 surveys.
3.2. Circumstances (C)
All of the circumstances are measured using data from before the measurement of the mental health outcomes at Wave 9 and 2019 Wave and, hence, also before the onset of the pandemic. Specially, we use data from the UKHLS Wave 8 (mainly) for the time‐varying circumstances and Waves 1‐8 for the time‐invariant variables. The choice of our circumstance variables embodies ethical judgments, defining sources of mental health inequality that are regarded as a cause for concern in the context of the response to the pandemic.
For the choice of circumstance variables, we follow the recent literature on health equity, along with the UK policy and legal context (e.g., Carrieri & Jones, 2018; Carrieri et al., 2020; Davillas & Jones, 2020; Jusot et al., 2013; Rosa Dias, 2009, 2010). To provide additional insights into the possible impact of the pandemic, we broaden the list of our pre‐existing circumstances beyond those that have typically been used in this literature to capture pre‐existing factors that are specific to the policy debate concerning the adverse consequences of COVID‐19 for socioeconomic inequality. These include pre‐existing chronic health problems, working in industries that are more relevant for or affected by the pandemic, individuals' employment status and their pre‐existing level of household income, the presence of children in households and living in multigenerational households or as lone parents, and housing tenure. Moreover, the influence of housing conditions on people's ability to self‐isolate and the neighbourhood environment are also factors to be considered.
Sex and age are included in our list of circumstances as they are protected characteristics under the UK Equality Act of 2010 (NHS England, 2017). Beyond this, for example, Alon et al. (2020) argue the impact of COVID‐19 may have a specific impact on gender: social distancing may have differential effects on the sectors and occupations where women are more likely to work; school closures and limited access to child care may affect working mothers. The latter may be offset by a shift to more flexible working and changes in social norms with respect to childcare. We create four age group indicators based on UKHLS wave 9 data (20–34 age group; 35–49 age group; 50–64 age group and those 65 and above) for males and females (giving eight age‐sex dummies).
Race is also protected under the Equality Act and the impact of COVID‐19 on those of black, Asian and minority ethnic (BAME) groups has been a particular focus of concern in public policy and debate in the UK and elsewhere (e.g., Office for National Statistics, 2020b). We have included indicators for white (reference group), black, Asian and mixed (including the other ethnic groups), following the ethnic breakdown from the Office for National Statistics (2020b).
Socioeconomic status (SES) in childhood is regarded as an important source of inequality of opportunity in health in the literature (e.g., Davillas & Jones, 2020; Jusot et al., 2013; Rosa Dias, 2009, 2010). We measure parental occupational status to proxy childhood SES. Two categorical variables (one for each parent) are used to capture the occupational status of the respondent's mother and father when the respondent was aged 14: not working (reference category), four occupation skill levels and a category for missing data. To construct these variables the occupational skill levels are based on the skill level structure of the Standard Occupational Classification 2010. Given that parental occupation is a time‐invariant variable, information from all UKHLS waves is used for those included in our sample (as it is collected when respondents first enroll in the survey). As in Davillas and Jones (2020), individuals' own education is included as a circumstance. Educational attainment is measured using indicators for five levels of qualification: no qualification (reference), basic qualification, O‐Level or equivalent qualification, A‐Level/post‐secondary, and degree.
Additional factors that have been identified as a source of socioeconomic inequality in context of impact of COVID‐19 are included as described below. These are considered as predetermined circumstances in our analysis and are based on information collected from UKHLS Wave 8 (unless otherwise stated); this is before the collection of our GHQ outcomes at Wave 9, the 2019 Wave and the COVID‐19 questionnaire. We measure housing tenure in a four‐category variable: own outright (reference category), own with mortgage, rent socially and private renters. Rental and mortgage costs have been considered as an important financial concern, with the UK Government undertaking initiatives to support those experiencing financial difficulties meeting mortgage and rental costs. Housing space is capturing by the ratio of the number of bedrooms to household size and by the number of other rooms in the home (apart from bedrooms, bathrooms, and kitchen); inequalities in housing space are an important factor affecting people's ability to self‐isolate.
Household composition is captured by a four‐category variable: single person household, lone parent household, multi‐occupancy households, while all other household types are treated as the reference category. Single adult households as well as multigenerational and multi‐occupancy household are particularly vulnerable to the COVID‐19 pandemic and lockdown. The presence of children in the household, imposing home‐schooling and additional childcare responsibilities during the lockdown, is captured by a dummy indicator taking the value of one in the presence of one or more children in household and zero otherwise.
Job status is included as a categorical variable: self‐employed, employee (reference), unemployed, retired and other. We have also included five dummy variables indicating whether respondent's occupation is in broad industrial sectors that are most relevant to the response to COVID‐19: health services, the food industry, retail, transportation, education and sports. We account for pre‐existing economic circumstances using long‐run average household income (up to a maximum of 8 waves) collected between UKHLS waves 1 (2009‐2011) and 8 (2016 and 2018). Household income is deflated using the RPI and equalised using the modified OECD scale to allow for different household compositions.
Given that people with health conditions are more vulnerable to COVID‐19, we include dichotomous variables covering ever‐diagnosed chronic conditions based on self‐reports: respiratory conditions, cardiovascular conditions, endocrine diseases, arthritis and other conditions 14 . Finally, two dummy variables are used to capture neighbourhood‐level characteristics that may be relevant for the response to COVID‐19. 15 Specifically, we include an indicator for respondents considering their neighbourhood as having poor/fair medical facilities and zero if very good/excellent. An indicator for poor/fair leisure facilities is also included. Summary statistics for our baseline circumstances are available in Supplementary Table B1 (Appendix B).
TABLE 1.
Summary statistics for the GHQ
| Wave 9 | Interim 2019 | April 2020 | May 2020 | June 2020 | July 2020 | |
|---|---|---|---|---|---|---|
| Panel A: Sample proportions and means | ||||||
| GHQ‐12 elements a | ||||||
| Concentration | 0.154 | 0.162 | 0.274 d | 0.246 d | 0.239 d | 0.177 d |
| Sleep | 0.142 | 0.148 | 0.236 d | 0.198 d | 0.202 d | 0.157 |
| Role | 0.126 | 0.129 | 0.272 d | 0.236 d | 0.211 d | 0.161 d |
| Decisions | 0.086 | 0.090 | 0.131 d | 0.128 d | 0.139 d | 0.108 d |
| Strain | 0.220 | 0.219 | 0.282 d | 0.260 d | 0.260 d | 0.211 d |
| Overcoming difficulties | 0.124 | 0.130 | 0.140 | 0.142 d | 0.155 d | 0.127 |
| Enjoy activities | 0.160 | 0.168 | 0.462 d | 0.417 d | 0.373 d | 0.278 d |
| Face up problems | 0.094 | 0.098 | 0.124 d | 0.120 d | 0.131 d | 0.105 |
| Depressed | 0.184 | 0.196 | 0.270 d | 0.255 d | 0.237 d | 0.201 |
| Confidence | 0.147 | 0.156 | 0.158 | 0.175 d | 0.174 d | 0.154 |
| Worthlessness | 0.078 | 0.082 | 0.090 | 0.096 d | 0.101 d | 0.085 |
| Happiness | 0.142 | 0.148 | 0.231 d | 0.205 d | 0.200 d | 0.171 d |
| GHQ‐12 Likert b | 11.07 | 11.22 | 12.30 d | 12.25 d | 12.36 d | 11.65 d |
| GHQ‐12 Caseness ≥4 c | 0.171 | 0.185 | 0.277 d | 0.257 d | 0.245 d | 0.201 d |
| Panel B: Overall inequality measure (GHQ‐12 Likert b ) | ||||||
| Variance | 29.23 | 29.61 | 35.50 d | 35.19 d | 37.32 d | 31.68 |
| MLD index | 0.101 | 0.100 | 0.112 d | 0.108 d | 0.109 d | 0.101 |
| Sample size | 8,222 | 8,185 | 7,512 | 7,025 | 6,786 | 6,642 |
Notes: Results in the first two columns (wave 9 and interim 2019 wave) use the UK Household Longitudinal Study Wave 9 sample weights while those in the third‐sixth columns are weighted by using our own longitudinal weights.
For each of the GHQ dimensions, the two categories indicating the most depressed states are coded as one and the remaining two categories, that reflect better mental health, are coded as zero (dichotomous variables).
Continuous GHQ‐12 measure based on the overall score across all 12 dimensions using the Likert scoring (ranging between zero and 36).
Dichotomous variable taking the value of one if the overall GHQ‐12 Caseness score ≥4 and zero otherwise.
Comparison between the Interim 2019 Wave and the COVID‐19 waves: differences in the mean values (or variance) compared to the corresponding results at Interim 2019 Wave are statistically significant at least at the 5% level.
4. RESULTS
4.1. The distribution of GHQ before and during the pandemic
Summary statistics for the GHQ outcomes are presented in Table 1. We find limited differences in the GHQ outcomes between the two baseline waves (Wave 9 and 2019 Wave), with all the observed differences being non‐statistically significant at the 5% level (p‐values>0.05); the fact that similar mean values are observed for all individual elements of the GHQ implies the absence of substantial differences in all components of the GHQ‐12 score over and above the composite GHQ‐12 scores. These results suggest that there are limited differences in GHQ outcomes across waves prior to the COVID‐19 outbreak in the UK.
Compared to the 2019 Wave, Table 1 (Panel A) shows substantial and statistically significant worsening of levels of psychological distress (given that all measures are coded to reflect worse psychological distress) during the pandemic. This applies to nearly all of the individual elements of GHQ and to the aggregated Likert and caseness scores. For example, the aggregate caseness score, for the proportion of respondents above the threshold value for psychological distress, increases from 0.185 at the 2019 Wave to 0.277 in April 2020. In other words, on this measure, just under 20% of the sample were experiencing psychological distress in 2019, but by April 2020, almost 30% of the same sample of individuals were experiencing distress. Over and above the composite GHQ‐12 score, detailed results for the 12 individual elements allows us to explore which aspects of mental health worsened the most (as all measures are coded to reflect worse psychological distress) during the peak of the first wave of the pandemic (April 2020); not surprisingly, given the lockdown restrictions, the dimension that is mostly affected during the peak of the first wave of the pandemic (April 2020) is relevant to day‐to‐day activities, 16.8% of the sample reported not being able to enjoy normal day‐to‐day activities in the pre‐COVID 2019 wave as opposed to 46.2% at April 2020. During the same period, those dimensions that relate to playing a useful role, problems with concentration and being unhappy, are the second, third and fourth most affected dimensions and more respondents reported facing problems with these as compared to the interim 2019 wave.
In general, the levels of psychological distress move back towards pre‐pandemic levels by the July 2020 COVID‐19 Wave (collected after the almost complete easing of the first lockdown) but the worsening in GHQ scores, relative to 2019, remains statistically significant for many of the individual elements (concentration problems, not playing a useful role, inability to make decisions, feeling under strain, not being able to enjoy day‐to‐day activities and feeling unhappy); this is reflected in the aggregate scores that remain systematically higher than baseline, indicating a persistent worsening of psychological distress.
Panel B of Table 1 compares total inequality for the Likert GHQ‐12 score, measured by the variance and the MLD index, before and during the pandemic. Differences in inequality measures between Wave 9 and the 2019 Wave are not statistically significant, suggesting the absence of systematic differences in the level of inequality in psychological distress during the immediate period before the onset of the pandemic. However, there is a systematic and statistically significant increase in total inequality from baseline to the COVID‐19 waves; for example, the variance of the GHQ‐12 Likert score increases from 29.61 at the 2019 Wave to 35.51 in April and up to 37.32 in June 2020. Figure 1 shows the change in the shape of the, kernel smoothed, density function for GHQ‐12 between Wave 9, the 2019 Wave, and the COVID waves, with a flattening of the density and greater mass in the right‐hand tail of the distribution.
FIGURE 1.
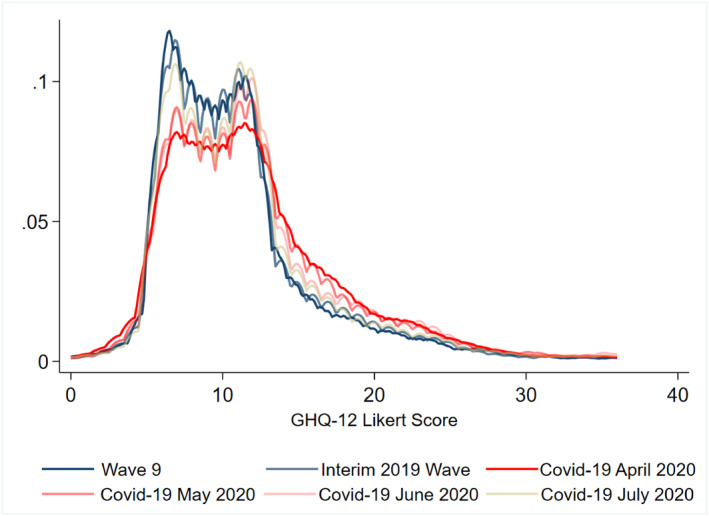
Distribution of General Health Questionnaire (GHQ)‐12 Likert score at UK Household Longitudinal Study Wave 9, Interim 2019 Wave and COVID‐19 Waves
Our analysis so far shows an increase in the total inequality in GHQ during the first wave of the pandemic, but does the same hold for observed socioeconomic inequality? To assess this, Table 2 presents the dissimilarity indices for socioeconomic inequality in each of the 12 elements of the GHQ. The baseline results for the restricted Wave 9 sample (conditional on responding to the COVID‐19 GHQ questionnaire) range between 0.223 and 0.346; the corresponding results for the 2019 Wave are similar and no systematic differences are observed in the dissimilarity indexes between Wave 9 and the 2019 Wave (p‐values>0.10, Table 2); this shows that socioeconomic inequality in components of the composite GHQ‐12 scores remained mostly unchanged between the pre‐pandemic UKHLS waves. Regarding the COVID‐19 waves, the estimated dissimilarity indices are smaller in magnitude for all but one of the 12 elements of the GHQ in April 2020 (the exception is confidence) 16 . The highest reduction in socioeconomic inequality is observed for not being able to enjoy day‐to‐day activities, the component with the most notable worsening of levels during the peak of the pandemic (Table 1). Dissimilarity indexes revert towards the pre‐pandemic levels in July (following the easing of the first lockdown) but in some cases there is still systematically lower observed socioeconomic inequality compared to the baseline. Overall, these results indicate that the proportion of total inequality attributed to our observed circumstances factors did not increase during the first wave of the pandemic (April‐July 2020).
TABLE 2.
Measures of socioeconomic inequality (Dissimilarity Indices) for each element of the General Health Questionnaire (GHQ)
| Wave 9 | Interim 2019 | April 2020 | May 2020 | June 2020 | July 2020 | |
|---|---|---|---|---|---|---|
| GHQ‐12 elements (Dissimilarity indices) | ||||||
| Concentration | 0.245 a (0.009) | 0.242 a (0.010) | 0.218 a (0.012) | 0.211 a (0.011) | 0.216 a (0.013) | 0.242 a (0.011) |
| Difference to 2019 wave [p‐values] b | 0.753 | ─ | 0.155 | 0.043 | 0.074 | 0.925 |
| Sleep | 0.243 a (0.009) | 0.229 a (0.009) | 0.219 a (0.011) | 0.216 a (0.011) | 0.204 a (0.011) | 0.233 a (0.010) |
| Difference to 2019 wave [p‐values] b | 0.380 | ─ | 0.545 | 0.449 | 0.109 | 0.776 |
| Role | 0.271 a (0.010) | 0.268 a (0.009) | 0.174 a (0.010) | 0.204 a (0.011) | 0.221 a (0.010) | 0.220 a (0.010) |
| Difference to 2019 wave [p‐values] b | 0.889 | ─ | 0.000 | 0.000 | 0.000 | 0.008 |
| Decisions | 0.289 a (0.008) | 0.288 a (0.009) | 0.246 a (0.009) | 0.273 a (0.010) | 0.265 a (0.011) | 0.264 a (0.009) |
| Difference to 2019 wave [p‐values] b | 0.992 | ─ | 0.043 | 0.469 | 0.222 | 0.220 |
| Strain | 0.233 a (0.010) | 0.230 a (0.010) | 0.218 a (0.012) | 0.218 a (0.012) | 0.223 a (0.011) | 0.226 a (0.011) |
| Difference to 2019 wave [p‐values] b | 0.774 | ─ | 0.324 | 0.334 | 0.608 | 0.799 |
| Overcoming difficulties | 0.308 a (0.010) | 0.295 a (0.010) | 0.252 a (0.010) | 0.278 a (0.010) | 0.266 a (0.011) | 0.276 a (0.010) |
| Difference to 2019 wave [p‐values] b | 0.414 | ─ | 0.016 | 0.363 | 0.103 | 0.349 |
| Enjoy activities | 0.236 a (0.009) | 0.237 a (0.009) | 0.086 a (0.012) | 0.089 a (0.012) | 0.117 a (0.011) | 0.154 a (0.011) |
| Difference to 2019 wave [p‐values] b | 0.989 | ─ | 0.000 | 0.000 | 0.000 | 0.000 |
| Face up problems | 0.297 a (0.009) | 0.297 a (0.009) | 0.270 a (0.010) | 0.277 a (0.010) | 0.287 a (0.011) | 0.276 a (0.010) |
| Difference to 2019 wave [p‐values] b | 0.996 | ─ | 0.168 | 0.334 | 0.604 | 0.785 |
| Depressed | 0.223 a (0.010) | 0.207 a (0.010) | 0.177 a (0.011) | 0.195 a (0.012) | 0.208 a (0.013) | 0.211 a (0.012) |
| Difference to 2019 wave [p‐values] b | 0.224 | ─ | 0.024 | 0.383 | 0.916 | 0.785 |
| Confidence | 0.270 a (0.010) | 0.255 a (0.010) | 0.275 a (0.010) | 0.259 a (0.011) | 0.257 a (0.011) | 0.255 a (0.011) |
| Difference to 2019 wave [p‐values] b | 0.352 | ─ | 0.237 | 0.822 | 0.927 | 0.974 |
| Worthlessness | 0.346 a (0.009) | 0.368 a (0.009) | 0.309 a (0.010) | 0.339 a (0.010) | 0.305 a (0.010) | 0.312 a (0.009) |
| Difference to wave 9 [p‐values] b | 0.274 | ─ | 0.013 | 0.197 | 0.002 | 0.016 |
| Happiness | 0.257 a (0.009) | 0.245 a (0.009) | 0.165 a (0.011) | 0.197 a (0.011) | 0.229 a (0.011) | 0.231 a (0.011) |
| Difference to 2019 wave [p‐values] b | 0.466 | ─ | 0.000 | 0.000 | 0.283 | 0.375 |
Notes: Results in the first two columns (Wave 9 and the Interim 2019 Wave) use the UK Household Longitudinal Study sample weights while those in the third‐sixth columns are weighted by using our own longitudinal weights. Bootstrapped standard errors for the inequality measures in parenthesis (500 replications). The bold values are statistically significant at p < 0.05.
p < 0.01 (for the Ho hypothesis that the dissimilarity index is equal to zero)
Test for differences in the inequality measures compared to the corresponding results for the Interim 2019 Wave; bootstrapped p‐values using 500 replications.
Table 3, Panel A presents the measures for the variance share (and the MLD index share) for our composite GHQ‐12 Likert measure that show the fraction of the total inequality in the GHQ‐12 Likert measure that is attributed to the observed socioeconomic inequality. The baseline results for the 2019 Wave are statistically significant with observed circumstances accounting for 12.82% for the total variance in GHQ‐12 (14.53% for the MLD index). These values fall to 11.12% (11.52% for the MLD index) in April 2020, and this reduction is statistically significant, showing that circumstances account for a smaller share of total inequality and that relative socioeconomic inequality did not increase during the peak of the pandemic. Similar patterns are observed in the May‐July Waves. Figure 2 shows that despite the increase in the absolute total variance (total inequality) in the Likert GHQ‐12 composite score (also shown in Table 1, Panel B), the absolute explained variance has remained stable, hence the fall in the variance share (i.e., to the proportion of the total inequality attributed to observed circumstances). Overall, these results show that relative socioeconomic inequality did not increase during the peak of the pandemic. It should be explicitly mentioned here that our socioeconomic inequality results for the composite Likert scores reflect the observed patterns for the 12 individual components of GHQ as described above; this highlights that the inequality patterns observed for the composite measures during the first wave of the pandemic as opposed to the pre‐pandemic period are not an artefact of using the composite measures but are confirmed by all individual elements. Results from the dissimilarity indexes for the caseness score are similar; there are no systematic differences in dissimilarity indexes between Wave 9 and the 2019 Wave, while dissimilarity indexes are lower during the first wave of the pandemic.
TABLE 3.
Measures of socioeconomic inequality for levels of General Health Questionnaire (GHQ)‐12 (Likert scoring) and for dichotomous distress indicators
| Wave 9 | Interim 2019 | April 2020 | May 2020 | June 2020 | July 2020 | |
|---|---|---|---|---|---|---|
| Panel A. GHQ‐12 Likert | ||||||
| Relative inequality: Variance share | 12.11 a (0.413) | 12.82 a (0.449) | 11.12 a (0.355) | 12.33 a (0.415) | 12.26 a (0.423) | 10.87 a (0.400) |
| Difference to 2019 wave b [p‐value] | 0.110 | ─ | 0.000 | 0.336 | 0.240 | 0.000 |
| Relative inequality: MLD index share | 13.99 a (0.360) | 14.53 a (0.364) | 11.52 a (0.269) | 13.26 a (0.340) | 13.47 a (0.362) | 12.49 a (0.339) |
| Difference to 2019 wave b [p‐value] | 0.371 | ─ | 0.000 | 0.001 | 0.007 | 0.000 |
| Panel B. GHQ‐12 Caseness≥4 | ||||||
| Dissimilarity index | 0.262 a (0.010) | 0.241 a (0.010) | 0.203 a (0.011) | 0.211 a (0.011) | 0.211 a (0.011) | 0.228 a (0.011) |
| Difference to 2019 wave b [p‐value] | 0.129 | ─ | 0.004 | 0.010 | 0.010 | 0.403 |
Notes: Results in the first two columns (Wave 9 and Interim 2019 Wave) use the UK Household Longitudinal Study sample weights while those in the third‐sixth columns are weighted by using our own longitudinal weights. Bootstrapped standard errors for the inequality measures in parenthesis (500 replications). The bold values are statistically significant at p < 0.05.
p < 0.01 (for the Ho hypothesis that the inequality measure is equal to zero).
Test for differences in the inequality measures compared to the corresponding results for the Interim 2019 Wave; bootstrapped p‐values using 500 replications.
FIGURE 2.
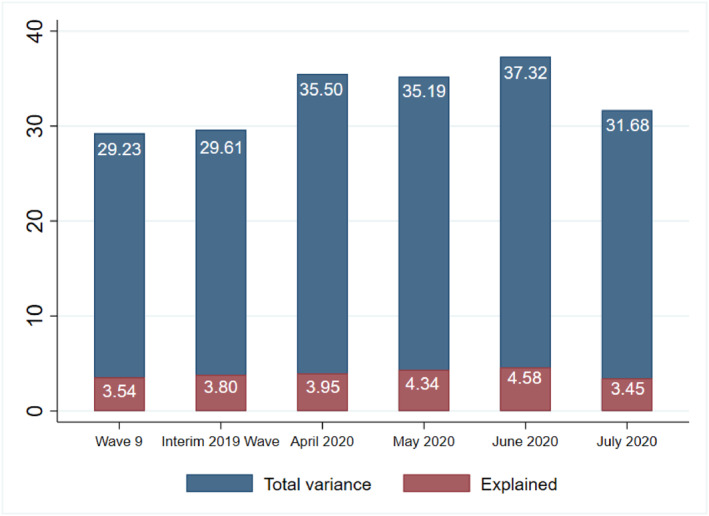
Total and explained variance of General Health Questionnaire (GHQ)‐12 Likert score
To explore the extent of the potential role of non‐response and sample selection bias in our inequality results we also estimated our inequality measures without accounting for sample weights (full results are available in Supplementary Tables C4–C6., Appendix C) 17 . Overall, we find that our inequality results are comparable with and without accounting for weights and, thus, the potential role of the non‐response and selection bias seems not to affect our main conclusions. Specifically, we find that without accounting for sample weights our inequality measures are reduced by around 10 percentage points compared to the base case results (Tables 2 and 3); this highlights the presence of a modest underestimation of inequality when we do not adjust for non‐response. One may argue however that restriction of our baseline sample (Wave 9 and Interim Wave) to those who ever completed a COVID‐19 survey may impose further biases to our analysis that are not adequately addressed using our sample weights. Estimation of our inequality and decomposition results based on the non‐restricted Wave 9 sample shows practically identical results to the corresponding results for the Wave 9 sample presented in the main text of the paper (results available upon request) 18 .
4.2. Decomposition analysis
Figure 3 presents the Shapley‐Shorrocks decomposition of the variance share results for our composite Likert GHQ‐12 measure (also available in Supplementary Table B2, Appendix B). Table B3 (Appendix B) presents the corresponding Shapley‐Shorrocks decomposition results for the dissimilarity indices for the GHQ‐12 caseness score; these results echo those in Figure 3. Our results show the detailed contribution of each of our age‐gender categories and are grouped by categories of the other circumstance variables: ethnicity, education, housing conditions, household composition, employment status, industry, income, neighbourhood, parental occupation, and chronic conditions. Before the pandemic, in Wave 9 and the 2019 Wave, the largest contributions to socioeconomic inequality are those attributed to chronic conditions (about 32%), housing conditions (18–20%) and employment status (15–16%). In contrast, during the peak of the first wave of the pandemic (April 2020) these three factors decline in their relative shares and demographic factors (age and gender) account for the largest share, increasing their share from 15% to 33%, with most notable increase for younger women. The contribution of working in an industry relevant to the response to the pandemic plays a small role at the 2019 Wave (1.05%), but nearly triples its share in April 2020 (2.68%).
FIGURE 3.
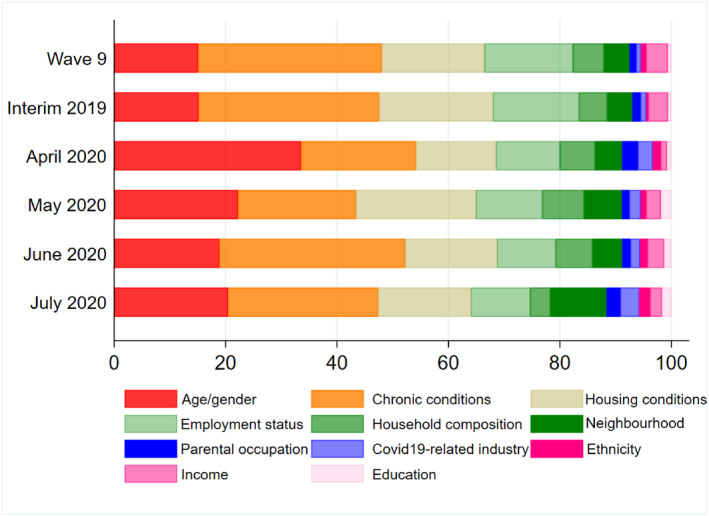
Decomposition analysis of General Health Questionnaire (GHQ)‐12 Likert scores. Note: Factor's contributions are ordered according to their contributions at April 2020 COVID Wave
As the first wave of the pandemic progressed, the contribution of demographics dropped from the peak levels of April and the contribution of other factors, such as chronic health conditions, housing conditions, household composition and neighbourhood characteristics have begun to explain a larger share. These results are in line with other evidence that has shown a strong demographic gradient on how the pandemic affects the mental health of the population, especially among younger women (Banks & Xu, 2020). They also reveal the increasing role of other socioeconomic circumstances as sources of stress during the COVID‐19 outbreak. For example, household composition shows an increasing contribution (May and June 2020) which may capture loneliness among single‐person households during the lockdown and the anxiety associated with the higher risks of COVID‐19 transmission for multi‐generational and multi‐occupied households (Haroon et al., 2020).
To provide further evidence on the role of our circumstances variables (and as a way explore the robustness of our results) we estimate regression models on the continuous Likert GHQ‐12 during the peak of the first wave of the COVID‐19 (April 2020) separately for the sub‐samples of those with and without psychological distress at the baseline (using the binary GHQ‐12 Caseness≥4 indicator). Table B4 (Supplementary Appendix) presents Shapley decomposition of the contribution of circumstance variables to explained variance of the continuous Likert GHQ‐12 score (i.e., the model R‐squared). Overall, these results confirm the dominant role of age and gender as they account for more than 45% of the explained variance in the GHQ‐12 scores for those who did not experience psychological distress at baseline; in particular this suggests that demographics play an important role in worsening mental health during the peak of the pandemic. The corresponding percentage contribution for demographics is much less evident for the case of those already experienced mental health issues at baseline. Moreover, of particular relevance for our inequality decomposition results, income itself seems not to exert notable contributions, while housing conditions and chronic conditions have the largest contributions in explaining GHQ Likert outcomes for those with and without cases of psychological distress at the baseline.
5. CONCLUSION
The UK population as a whole has been exposed to the policy responses to the COVID‐19 pandemic. Measures taken include a lockdown, social distancing and self‐isolation. Their economic impact has been substantial and resources within the health and social care systems have been diverted to the pandemic. Given evidence that the impact of the pandemic on physical health and mortality has been more severe for those in disadvantaged circumstances (e.g., Office for National Statistics, 2020a) it might reasonably be expected that the impact on psychological distress and the mental health of the population may also have been unequally distributed within the population.
In line with the evidence on physical health, our results show a substantial worsening of the overall levels of GHQ during the peak (of the first wave) of the pandemic. This applies to nearly all of the individual elements of GHQ‐12 and to overall composite GHQ‐12 scores. The specific GHQ dimensions that are most affected during the peak of the first wave of the pandemic (April 2020), as opposed to pre‐COVID baseline period, are relevant to people's ability to enjoy day‐to‐day activities, playing a useful role, problems with concentration and being unhappy. In addition, there is a statistically significant increase in total inequality in the Likert GHQ‐12 score between the periods before (Wave 9 and the 2019 Wave) and during the pandemic (April–July 2020). Nevertheless, we find that the proportion of the total inequality that is, attributed to our observed set of pre‐existing socioeconomic circumstances did not increase during the first wave of the pandemic; these results reflect similar patterns observed for the 12 individual dimensions of GHQ. Our results suggest that, with respect to psychological distress, the greater total inequality that is, evident, is broadly diffused across the population. This is consistent with the notion that the first wave of the pandemic was, to some extent, a leveller as far as pre‐existing circumstances are considered. For example, recent evidence from the USA shows that individuals with higher socioeconomic status experienced a greater increase in depressive symptoms and a decrease in life satisfaction during COVID‐19 in comparison to those with lower socioeconomic status (Wanberg et al., 2020). However, it should be noted here that greater unexplained variation may prove challenging for policy makers and it will be interesting to see whether this finding persists in future waves of the pandemic. Finally, we undertook extensive sensitivity analyses to explore whether these results are contaminated by unequal selection and non‐response to the UKHLS COVID‐19 surveys. We find that our results are robust to these potential biases and these are unlikely to affect the conclusions of our study.
The Shapley‐Shorrocks decomposition analysis of the shares of inequality that are attributable to observed circumstances shows that during the peak of the pandemic (April 2020), key socioeconomic factors declined in their share of socioeconomic inequality and that age and gender accounts for a larger share. As the first wave of the pandemic progressed, the contribution of demographics declined from their peak levels of April and other factors such as chronic health conditions, housing conditions, household composition and neighbourhood characteristics made increasing contributions to socioeconomic inequality compared to April 2020.
Our results are broadly in line with the COVID‐19 Marmot Review (Marmot et al., 2020), which argues that pre‐existing circumstances have contributed to the unequal burden of the COVID‐19 outbreak for the UK population. However, we find that absolute socioeconomic inequalities remained stable, implying a decline in their relative contribution to total inequality. Our decomposition analysis highlights the role of different socioeconomic factors and their contribution to socioeconomic inequalities in mental health across different stages of the first wave of the COVID‐19 outbreak. These findings are in line with the call for a multifaceted policy response to reduce health inequality in the post‐COVID world.
CONFLICT OF INTEREST
Authors have no conflict of interest to declare.
Supporting information
Supplementary Material 1
ACKNOWLEDGMENTS
Understanding Society is an initiative funded by the Economic and Social Research Council and various Government Departments, with scientific leadership by the Institute for Social and Economic Research, University of Essex, and survey delivery by NatCen Social Research and Kantar Public. The research data are distributed by the UK Data Service. Andrew Jones acknowledges funding from the Leverhulme Trust Major Research Fellowship (MRF‐2016‐004). The funders, data creators and UK Data Service have no responsibility for the contents of this paper. We are grateful to Stephen Jenkins, Nicolas Pistolesi, Carol Propper and two anonymous reviewers for their comments on an earlier version.
ENDNOTES
COVID‐19 policy tracker. The Heath Foundation. https://www.health.org.uk/news‐andcomment/charts‐and‐infographics/covid‐19‐policy‐tracker.
Specifically, the most deprived London boroughs had the highest COVID‐19 age‐standardised death rates with Newham at 144.3 deaths per 100,000, Brent at 141.5 and Hackney at 127.4 compared to an average of 36.2 per 100,000 in England and Wales as a whole.
Roemer (1998) defines a ‘responsibility cut’ that partitions all factors influencing individual attainment between a category of effort factors, for which individuals should be held partly responsible, and a category of circumstance factors, which are judged to be a source of unfair differences in outcomes. The concept of equality of opportunity draws on two ethical principles: compensation and reward (e.g., Fleurbaey & Schokkaert, 2012). There are two broad perspectives on the definition and measurement of inequality of opportunity: the ex ante and the ex post approaches. The ex ante approach defines equality of opportunity if all individuals face the same opportunity set, prior to their efforts and outcomes being realised; then, individuals have equal opportunities if there are no differences in expected outcomes across types who have different circumstances. The expectation over outcomes within types can be based on a simple mean (utilitarian reward) or with some degree of inequality aversion within types.
One of the sources of potential measurement error in GHQ outcomes may be the mixed interview modes (web vs. face‐to‐face surveys) used in the baseline and subsequent COVID‐19 waves regarding the GHQ questionnaire. However, our conclusions are unlikely to be contaminated by any potential measurement error due to interview mode (see footnote 12 and Supplementary Appendix C).
A feature of this approach is that the distribution of effort within each type constitutes a circumstance in itself. The model therefore assumes that effort is a function of circumstances, with circumstances being pre‐determined. The reduced form (2) captures both direct and indirect contributions of circumstances.
Here we differ from the approach taken to health equity in Fleurbaey and Schokkaert (2009) who work within an ex post framework, based on a model like Equation (1) that conditions on both C and E, from which they derive two different standardised measures of the outcome: the fairness gap and the direct unfairness measures. Their approach requires E to be defined and observed.
Given that some of our mental health outcomes are binary variables, a probit model is used to estimate the conditional probability function, given our set of circumstances, and the relevant counterfactual predictions are obtained (analogously to, Equations (2) and (3)).
Dissimilarity indexes have been used by the World Bank to compute the Human Opportunity Index (e.g., Paes de Barros et al., 2007).
The variance has been proposed as an inequality measure in a number of recent contributions to the IOp literature (see, e.g., Carrieri & Jones, 2018; Fleurbaey & Schokkaert, 2009, 2012; Jusot et al., 2013).
As a survey of those living in private households UKHLS does not include those living in care homes, an important group in terms of the direct impact of COVID‐19.
A small number of the UKHLS Interim Wave interviews (37 cases in our final sample), took place in March‐May 2020 (after the onset of the pandemic in the UK), these are excluded from our Interim 2019 UKHLS sample.
The use of different modes during a survey may affect how respondents answer the same questions. Particular concern may arise regarding the web‐based COVID‐19 surveys, as responses to online questionnaires may affect the comparability of responses to the GHQ‐12 questionnaire as compared to conventional face‐to‐face interviews. However, UKHLS had already invited a proportion of the participants to complete online questionnaires (using a push‐to‐web mixed‐mode design as a way to mitigate fieldwork costs) during the pre‐COVID‐19 UKHLS Wave 9 and the 2019 Wave. Sensitivity analysis focusing solely on those who responded to web‐based GHQ questionnaires at Wave 9 and the 2019 Wave (Supplementary Appendix C, Tables 1, 2, 3) shows limited differences to our base case inequality and decomposition results in Tables 2–4 (Wave 9 and 2019 Wave). This suggests that focusing on the web‐based questionnaires does not result in notably different conclusions regarding the inequality results.
Similar procedures involving stepwise regression models are used by UKHLS to create the set of derived sample weights available in the dataset. Stepwise regressions fitting regression models in which the choice of predictive variables is carried out by an automatic procedure from a larger set of explanatory variables chosen by the researcher. Here, all (pre‐determined) circumstances variables used in our inequality analysis are also used as explanatory variables for the stepwise probit models; stepwise backward elimination procedure selects certain covariates from all candidate variables following repeated steps of eliminating and re‐entering variables based on their statistical significance following standard rules of thumb and the (re‐)estimation of the relevant probit models.
We include chronic health conditions, rather than disability, in order to capture a wider range of conditions, including less severe conditions that do not necessarily entail “substantial” limitations on people's daily activities. This is of particular relevance for the equity impact of the COVID‐19 pandemic as, for example, people with (mild) respiratory conditions (captured by our chronic conditions variables) may be more vulnerable to COVID‐19 than some of those with disabilities. Another example is chronic conditions that can be managed using medication but are still risk factors for COVID‐19. These are captured by the chronic conditions' questions in UKHLS but not necessarily by the disability questions. Moreover, the wording for the specific disability questions in UKHLS refers to substantial difficulties with areas of life (which may not be the case for those with well managed chronic conditions).
Unlike all other time‐varying circumstance variables (collected at UKHLS Wave 8), the neighbourhood‐level characteristics are measured at UKHLS Wave 6.
Formal tests for the differences in dissimilarity indexes between the 2019 Wave and the COVID‐19 waves show that the reduction in socioeconomic inequality is statistically significant for some elements of the GHQ‐12 questionnaire; for example, the dissimilarity index for limited enjoyment of day‐to‐day activities decreases from 0.236 at Wave 9 and in 2019 to values in the range 0.086–0.154 for the COVID‐19 waves.
Summary statistics (Table B1.) show that the mean values of the pre‐existing circumstance (Waves 1‐8) are similar between the baseline Wave 9/Interim Wave sample and the subsequent COVID‐19 waves (columns b‐f). This suggests that our longitudinal sample weights are relevant in achieving a good balance in the mean value of the pre‐existing circumstances in COVID‐19 waves (compared to baseline) and, thus, they may provide good adjustments for non‐response biases.
As a further reassurance the comparison of the mean values for the pre‐existing circumstance variables between the full Wave 9 and the restricted Wave 9 sample show limited differences (Table B1 columns a and b).
DATA AVAILABILITY STATEMENT
Understanding Society is an initiative funded by the Economic and Social Research Council and various Government Departments, with scientific leadership by the Institute for Social and Economic Research, University of Essex, and survey delivery by NatCen Social Research and Kantar Public. The research data are distributed by the UK Data Service. Andrew Jones acknowledges funding from the Leverhulme Trust Major Research Fellowship (MRF‐2016‐004). The funders, data creators and UK Data Service have no responsibility for the contents of this paper.
REFERENCES
- Alon, T. M. , Doepke, M. , Olmstead‐Rumsey, J. , & Tertilt, M. (2020). The impact of COVID‐19 on gender equality, (p. 26947). NBER Working Paper. [Google Scholar]
- Banks, J. , & Xu, X. (2020). The mental health effects of the first two months of lockdown during the COVID‐19 pandemic in the UK. Fiscal Studies, 41(3), 685–708. [Google Scholar]
- Bowling, A. (1991). Measuring health: A review of quality of life measurement scales. Open University Press. [Google Scholar]
- Carrieri, V. , Davillas, A. , & Jones, A. M. (2020). A latent class approach to inequity in health using biomarker data. Health Economics, 29, 808–826. [DOI] [PubMed] [Google Scholar]
- Carrieri, V. , & Jones, A. M. (2018). Inequality of opportunity in health: A decomposition‐based approach. Health Economics, 27, 1981–1995. [DOI] [PubMed] [Google Scholar]
- Davillas, A. , Benzeval, M. , & Kumari, M. (2016). Association of adiposity and mental health functioning across the lifespan: findings from understanding society (the UK household longitudinal study). PloS One, 11(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davillas, A. , & Jones, A. M. (2020). Ex ante inequality of opportunity in health, decomposition and distributional analysis of biomarkers. Journal of Health Economics, 69, 2020. [DOI] [PubMed] [Google Scholar]
- Deutsch, J. , Pi Alperin, M. N. , & Silber, J. (2018). Using the shapley decomposition to disentangle the impact of circumstances and efforts on health inequality. Social Indicators Research, 138, 523–543. [Google Scholar]
- Ferreira, F. H. G. , & Gignoux, J. (2011). The measurement of inequality of opportunity: Theory and an application to Latin America. Review of Income and Wealth, 57, 622–657. [Google Scholar]
- Ferreira, F. H. G. , & Gignoux, J. (2013). The measurement of educational inequality: Achievement and Opportunity1. The World Bank Economic Review, 28, 210–246. [Google Scholar]
- Fleurbaey, M. , & Schokkaert, E. (2009). Unfair inequalities in health and health care. Journal of Health Economics, 28, 73–90. [DOI] [PubMed] [Google Scholar]
- Fleurbaey, M. , & Schokkaert, E. (2012). Equity in health and health care. In Barros P., McGuire T., & Pauly M. (Eds.), Handbook of health economics (Vol. 2, pp. 1003–1092). [Google Scholar]
- Goldberg, D. P. , Gater, R. , Sartorius, N. , Ustun, T. B. , Piccinelli, M. , Gureje, O. , et al. (1997). The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychological Medicine, 27, 191–197. [DOI] [PubMed] [Google Scholar]
- Haiyang, L. , Peng, N. , & Long, Q. (2020). Do quarantine experiences and attitudes towards COVD‐19 affect the distribution of psychological outcomes in China? A quantile regression analysis. GLO Discussion Paper. No.512. [Google Scholar]
- Haroon, S. , Chandan, J. S. , Middleton, J. , & Cheng, K. K. (2020). Covid‐19: Breaking the chain of household transmission. BMJ, 370, m3181. [DOI] [PubMed] [Google Scholar]
- Institute for Social and Economic Research . (2020). Understanding Society COVID‐19. Version 5.1, December 2020. Colchester: University of Essex. [Google Scholar]
- Juárez, F. W. C. , & Soloaga, I. (2014). iop: Estimating ex‐ante inequality of opportunity. STATA Journal, 14, 830–846. [Google Scholar]
- Jusot, F. , Tubeuf, S. , & Trannoy, A. (2013). Circumstances and efforts: How important is their correlation for the measurement of inequality of opportunity in health? Health Economics, 22, 1470–1495. [DOI] [PubMed] [Google Scholar]
- Maheswaran, H. , Kupek, E. , & Petrou, S. (2015). Self‐reported health and socio‐economic inequalities in England, 1996‐2009: Repeated national cross‐sectional study. Social Science & Medicine, 136–137, 135–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot, M. , Allen, J. , Goldblatt, P. , Herd, E. , & Morrison, J. (2020). Build back fairer: The COVID‐19 Marmot Review. The pandemic, socioeconomic and health inequalities in England. Institute of Health Equity. [Google Scholar]
- NHS England (2017). NHS England’s response to the specific equality duties of the Equality Act 2010. [Google Scholar]
- Office for National Statistics (2020a). Deaths involving COVID‐19 by local area and socioeconomic deprivation: deaths occurring between 1 March and 17 April 2020. Statistical Bulletin, Office for National Statistics. [Google Scholar]
- Office for National Statistics (2020b). Coronavirus (COVID‐19) related deaths by ethnic group, England and Wales: 2 March 2020 to 10 April 2020. Office for National Statistics. [Google Scholar]
- Paes de Barros, R. , Ferreira, F. , Molinas Vega, J. , & Saavedra Chanduvi, J. (2007). Measuring inequality of opportunity in Latin America and the Caribbean. The World Bank. [Google Scholar]
- Ramos, X. , & Van de Gaer, D. (2016). Approaches to inequality of opportunity: Principles, measures and evidence. Journal of Economic Surveys, 30, 855–883. [Google Scholar]
- Roemer, J. E. (1998). Equality of opportunity. Harvard University Press. [Google Scholar]
- Roemer, J. E. , & Trannoy, A. (2016). Equality of opportunity: Theory and measurement. Journal of Economic Literature, 54, 1288–1332. [Google Scholar]
- Rosa Dias, P. (2009). Inequality of opportunity in health: Evidence from a UK cohort study. Health Economics, 18, 1057–1074. [DOI] [PubMed] [Google Scholar]
- Rosa Dias, P. (2010). Modelling opportunity in health under partial observability of circumstances. Health Economics, 19, 252–264. [DOI] [PubMed] [Google Scholar]
- Shorrocks, A. F. (2013). Decomposition procedures for distributional analysis: A unified framework based on the shapley value. The Journal of Economic Inequality, 11, 99–126. [Google Scholar]
- Tait, R. J. , Hulse, G. K. , & Robertson, S. I. (2002). A review of the validity of the General Health Questionnaire in adolescent populations. Australian and New Zealand Journal of Psychiatry, 36, 550–557. [DOI] [PubMed] [Google Scholar]
- Thomson, R. M. , Niedzwiedz, C. L. , & Katikireddi, S. V. (2018). Trends in gender and socioeconomic inequalities in mental health following the great recession and subsequent austerity policies: A repeat cross‐sectional analysis of the health surveys for England. BMJ Open, 8, e022924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanberg, C. R. , Csillag, B. , Douglass, R. P. , Zhou, L. , & Pollard, M. S. (2020). Socioeconomic status and well‐being during COVID‐19: A resource‐based examination. Journal of Applied Psychology, 105(12), 1382–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1
Data Availability Statement
Understanding Society is an initiative funded by the Economic and Social Research Council and various Government Departments, with scientific leadership by the Institute for Social and Economic Research, University of Essex, and survey delivery by NatCen Social Research and Kantar Public. The research data are distributed by the UK Data Service. Andrew Jones acknowledges funding from the Leverhulme Trust Major Research Fellowship (MRF‐2016‐004). The funders, data creators and UK Data Service have no responsibility for the contents of this paper.


