Abstract
Introduction
The COVID‐19 pandemic demanded a rapid response within Radiation Oncology services to minimise the risk of infection to patients and workforce. This study aimed to assess whether the operational changes put in place to reduce infection risks were effective in engaging and supporting staff.
Methods
Our service’s response saw staff and patients split into morning or afternoon shifts without overlap. Changes included extended clinic hours, modified treatment regimens, expanded online/electronic communication and remote working. Staff were invited to respond to an electronic questionnaire in September 2020, just after the peak of the second COVID‐19 wave in Victoria. Responses captured demographic data, parental status, profession, happiness levels, fear of COVID‐19 and e‐communication efficacy.
Results
A 57% response rate was achieved. 69% of respondents were female; 40% were aged 45+ and 35% had school‐aged children. Staff aged 45+ showed a significantly greater fear of COVID‐19 than younger staff. 36% of respondents reported feeling nervous or anxious watching news reports about COVID‐19. 92% of staff were happy with their work arrangements; staff with children were happier than staff without children with their shifts. Online chat/channels were reported as the preferred e‐communication method between colleagues.
Conclusion
Staff provided predominantly positive feedback to the changes made in response to the pandemic, reporting high levels of happiness and willingness to continue with the changes implemented during COVID‐19. The strategies adopted worked well and the overall high levels of staff satisfaction will allow our service to quickly pivot should further surges, or another pandemic, arise.
Keywords: COVID‐19, operational, Radiation Oncology, response, workforce
Introduction
Australia experienced the first surge of COVID‐19 1 , 2 , 3 in March and April 2020, with a maximum of 464 daily cases reported on March 28th. After a period of very low numbers, there was a further upswing in infections; a larger second wave commenced in June, with the maximum number of daily reported cases of 698 on August 5th. 4 The majority of the second wave infections occurred in the state of Victoria, within the city of Melbourne. At the height of the first wave, there were 541 active COVID‐19 cases in Victoria; at the height of the second wave on August 7th, there were 6769 active cases in Victoria. 5 Greater Melbourne introduced a strict Stage 4 lockdown (including a curfew between 8 pm and 5 am, travel limited to 5 km from home, and leaving home for four reasons only: shopping for food or essential items; permitted work; one hour of outdoor exercise per day; or medical care) to control the spread of the virus throughout much of the second wave (Fig. 1).
Fig. 1.
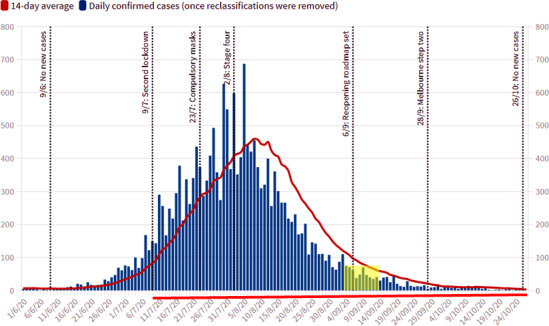
Daily active cases in Victoria. 5
The COVID‐19 pandemic necessitated a rapid response to scheduling and capacity within hospitals worldwide. 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 Different hospital services required the development of specific innovative changes to operations. Radiation Oncology was among the services that had to adapt, and these adaptions were undertaken in many countries including Canada, Singapore, China and Australia. By and large, these changes focussed on protecting both staff and patients from possible exposure to the virus and therefore included changes to workflow and physical location, with a particular focus on the delivery of telemedicine. 11 , 12 , 13 , 14 , 15 , 16 , 17 Although research has examined the impact of operational changes on patients and workflow, 8 , 10 , 18 , 19 the impact on staff remains unreported.
Radiotherapy requires daily patient visits and close contact with staff. It is also a multi‐disciplinary specialty with close collaboration between radiation therapists, physicists, medical staff, nursing, allied health and administrative staff groups. The risk for cross infection between staff groups and patients, and across the entire workforce is likely to be high without radical changes to work practices.
In the Radiation Oncology service of a large public hospital in Victoria, Australia, management made the decision to segregate the workforce in line with recommendations of Mukherjee et al., 16 guided by the experience of the SARS outbreak in 2003. The goal was to protect vulnerable oncology patients from iatrogenic and lateral community COVID‐19 transmission, while preserving operational capacity. COVID‐19 infection amongst staff necessitates a 14‐day isolation period. The importance of avoiding patient infections has been highlighted; patients with cancer have worse outcomes in terms of hospital admission, ventilation or death due to COVID‐19. 15 , 17 , 20 Without a viable workforce, all patients would have treatments missed and interrupted. This would result in a significant impact to patient access to care and thus patient outcomes.
In a matter of days, the majority of staff were segregated into morning or afternoon shifts. Changes took place across both the metropolitan (4 Linac, brachytherapy, superficial) and regional (2 Linac, superficial) services. The duration of the split workforce approach was unknown at the outbreak of COVID‐19; it eventuated that staff worked split shifts for 8 months, from April to November 2020, with a staggered return to more blended workforce and patient mix commencing in Dec 2020.
The study described in this manuscript outlines the operational changes implemented in the Radiation Oncology service, across multiple disciplines, in response to COVID‐19.
A staff survey was performed, coincident with Victoria’s second COVID‐19 wave and Melbourne’s Stage 4 lockdown, inviting responses from all staff within the service to examine staff perceptions of the strategies, tolerance, health and wellness.
This exploratory review of the process and the staff reactions, taken in context with complimentary work on training, education and approaches taken in other services, 8 , 28 may inform future service responses to COVID‐19 or similar health events. The impact on patients is not captured within this work.
Methods
This was a Human Ethics‐approved single institution cross‐sectional survey study (Austin HREC/65378/Austin‐2020) that invited all staff who were employed within Austin Health Radiation Oncology service to participate. The study protocol and questionnaire were submitted for Ethics review in June 2020 with approval received in August 2020.
A REDCap 29 Electronic Data Capture portal was developed to facilitate data anonymisation and secure data storage. The first survey link was distributed to staff via email on Wednesday 9th September 2020, with reminder emails sent to staff over a two‐week completion window.
At the time of the surveys, the Radiation Oncology service consisted of 129 staff, working across various disciplines. Distribution of the survey coincided with one of the world’s longest and strictest lockdowns. As shown in Figure 1, the survey period occurred 2 months into a Stage 4 lockdown and 3 months following the start of lockdowns imposed in response to the second wave of COVID‐19 cases (red bars in Fig. 1 which indicate duration of lockdowns in response to the first and second COVID‐19 waves while the survey timeframe is illustrated by yellow shade). As this project was conceived of in April 2020, it was not intended that this survey would capture information pertaining to the second wave in Melbourne as this arose several months later.
Operational changes and model of care
In response to COVID‐19, the clinical treatment day was extended, with patient treatments taking place between 7 am and 8 pm. Patient activity was maintained to that of pre‐COVID‐19 operations. Patients and treatment staff were divided into two cohorts with no movement between linacs. Changes to staff working hours were put in place for Radiation Oncologists, Radiation Therapists, Medical Physicists, Nurses and administrative staff. Therapists and Physicists were segregated into morning and afternoon shifts, with minimal overlap of shifts. A half‐hour break at the linacs occurred between shifts for deep cleaning of the Linac area. Working from home was adopted where viable for Therapists and Physicists to further separate morning and afternoon workforce. Nursing staff were a small group, and while split shifts were deployed to enable clinical coverage, some crossover between morning and afternoon shifts was still required. A separate tea room was established to enable nursing staff to remain apart from other staff. Administrative staff worked in teams across the extended hours with no rotation between shifts. Medical Typists worked from home; other administrative staff worked on‐site to support off‐site medical staff, and to support patients coming on‐site.
Prior to COVID‐19, a significant part of the Radiation Oncologist workflow occurred remotely; in particular, the workload related to planning and image review also occurred off‐site. Remote working strategies were expanded and additional telehealth supports were quickly adopted; however, it was recognised that some patients would need to be examined and others would require procedures for which medical staff would need to be present (e.g. brachytherapy, naso‐endoscopy examinations). Approximately 90% of new and returning patient clinic reviews were converted to internet video or telephone modalities. Where possible, on‐treatment reviews were also delivered remotely. A weekly roster was established with 1–2 oncologists on‐site each day for emergencies. Fellows and Registrars were split into two teams, spanning 7 am to 8 pm.
Given the broad spread of staff across the day, numerous existing communication methods were employed more heavily during the COVID‐19 response than in the past and the hospital also rapidly implemented Microsoft Teams (Microsoft, Redmond). The change to service delivery was developed in consultation with staff and the Austin Hospital Infection Control department. It was designed to minimise physical interaction between employees. The arrangements were further supported by the allocation of separate office spaces, installation of sneeze guards at reception and nursing stations and meal areas for shift workers. Measurement of staff response to the efficiency and effectiveness of these communications methods was undertaken. In addition, the hospital‐guided response necessitated cessation of face‐to‐face meetings, daily staff checks of COVID‐19 symptoms and the use of personal protective equipment including face shields and face masks.
Measures
The questionnaire consisted of items drawn from the following validated measures, as well as items developed specifically for the study, and took approximately 15 min to complete.
Personal, work and patient‐related burnout
Demographic and role‐related items in the survey included: age, gender, profession, whether they had school‐aged children (yes/no), years employed at institution, shift allocation following COVID‐19 (morning, afternoon, no change), and hours per week worked on average in January 2020 and April 2020.
To assess burnout in staff, the Copenhagen Burnout Inventory’s (CBI) 30 personal burnout, work‐related and patient‐related sub‐scales were used. The sub‐scales assess physical and psychological fatigue associated with burnout across general populations. Although the CBI was designed with a 5‐point Likert scale, the response categories were revised to a 4‐point scale with the removal of the ’Seldom’ category for the personal and work‐related burnout questions, as it was considered to be similar to the ‘Almost Never’ category. As such, the overall subscale was not considered, with data analysed descriptively over the ‘Always’, ‘Often’, ‘Sometimes’ and ‘Never/Almost Never’ categories. The patient‐related burnout items included a 5‐point scale and N/A as some members of the workforce do not work with patients. For the current study, higher scores indicated higher levels of burnout.
Fear of COVID‐19
Specific anxiety about COVID‐19 was measured using a modified version of the Fear of COVID‐19 Scale. 31 This is a recently developed and validated scale with good evidence of reliability and validity. Respondents provide answers on a 5‐point Likert response scale. One question was omitted from the Fear of COVID‐19 Scale questions (Item 6 ‘I cannot sleep because I’m worrying about getting coronavirus‐19’), with one additional item about reductions in fear of COVID‐19 included in the survey (‘My fear of COVID‐19 decreased in the past 4–8 weeks’), which also considered a 5‐point Likert response scale. This modification aimed to capture staff reaction to the operational changes made in response to COVID‐19 in context of the prevalence of COVID‐19 in the community.
Staff perspectives on shift changes as part of the new operating system
Items were designed (Table 1) to capture staff responses to operational changes. These included items on satisfaction with their shift allocation, with work‐from‐home and satisfaction to continue with shifts into the foreseeable future.
Table 1.
Staff satisfaction with work arrangement changes
| Question | n (%) |
|---|---|
| With your allocation into your shift (e.g. morning/afternoon) | |
| Not at all happy | 1 (1%) |
| Somewhat unhappy | 5 (7%) |
| Somewhat happy | 26 (35%) |
| Very happy | 28 (38%) |
| N/A; No change or cannot WFH | 14 (19%) |
| With your work arrangements (e.g. Work‐from‐home or Work‐at‐work) | |
| Not at all happy | 0 (0%) |
| Somewhat unhappy | 5 (7%) |
| Somewhat happy | 25 (34%) |
| Very happy | 33 (45%) |
| N/A; No change or cannot WFH | 11 (15%) |
| To continue with your work arrangements for another month? | |
| Not at all happy | 0 (0%) |
| Somewhat unhappy | 8 (11%) |
| Somewhat happy | 28 (38%) |
| Very happy | 37 (50%) |
| N/A; No change or cannot WFH | 1 (1%) |
| To continue with your work arrangements for another six months? | |
| Not at all happy | 11 (15%) |
| Somewhat unhappy | 17 (23%) |
| Somewhat happy | 21 (28%) |
| Very happy | 23 (31%) |
| N/A; No change or cannot WFH | 2 (3%) |
| To continue with your work arrangements for another twelve months? | |
| Not at all happy | 23 (31%) |
| Somewhat unhappy | 14 (19%) |
| Somewhat happy | 15 (20%) |
| Very happy | 20 (27%) |
| N/A; No change or cannot WFH | 2 (3%) |
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Effectiveness of, and confidence in, methods offered to staff to communicate with colleagues as part of the new system
Perceptions of the effectiveness of, and confidence in, communication modalities offered to staff for working with colleagues were assessed using items specifically developed for the study. Respondents were asked about their capacity to use a range of modalities to communicate with colleagues and patients including: face‐to‐face; email; telephone; text messaging; chat channel; video conferences (e.g. MS Teams), and; notation with electronic medical record systems (Mosaiq and ARIA). Items sought to understand respondent’s capacity to use the various modalities to: communicate thoughts clearly, communicate thoughts efficiently, send messages to other staff, receive messages in real life, and communicate with patients. Confidence in communicating with colleagues using the communication modalities was also assessed.
Statistical analysis
Descriptive analysis was conducted to summarise the responses to questions using Stata (StataCorp LLC, College Station, TX, USA). Data are presented as counts and percentages for the categorical variables. Staff responses were compared to the overall staff characteristics to indicate the potential extent of bias in responses. Comparisons and differences between groups were tested using Chi‐squared tests or Fishers Exact tests to support the presented data.
Results
Over the two‐week survey period, 74 respondents completed the survey across the two work sites, an overall response rate of 57%. Return rates for Oncologists, Therapists, Physicists and Nurses/Allied Health were 6/12 (50%), 35/59 (59%), 12/15 (80%) and 8/11 (73%) respectively, indicating a representative sample of the service. Of the responses, 51 (69%) were female, with nearly 60% of the sample being aged <45 years and with 35% having school age children. A mix of professions with a range of experience provided responses. Work hours remained similar at an average of 36 h per week at the time of the survey in September 2020 in comparison to 38 h per week in January 2020.
The responses to the modified fear of COVID‐19 questions are indicated in Figure 2. Overall, 13% of respondents indicated that they agreed or strongly agreed with the statement that they were most afraid of COVID‐19, with this proportion being higher for Medical Physicists and Nursing/Allied Health staff (42% and 38%, respectively), with none of the 6 Radiation Oncologists (0%) indicating agreement. Fear of COVID‐19 was greatest in staff members over the age of 45 with 15% strongly agreeing and 26% agreeing they were most afraid of COVID‐19, compared to 7% strongly agreeing and 5% agreeing they were most afraid for staff 45 years and younger. Of all respondents, 36% indicated they agreed that they were nervous or anxious when watching news reports regarding COVID‐19.
Fig. 2.
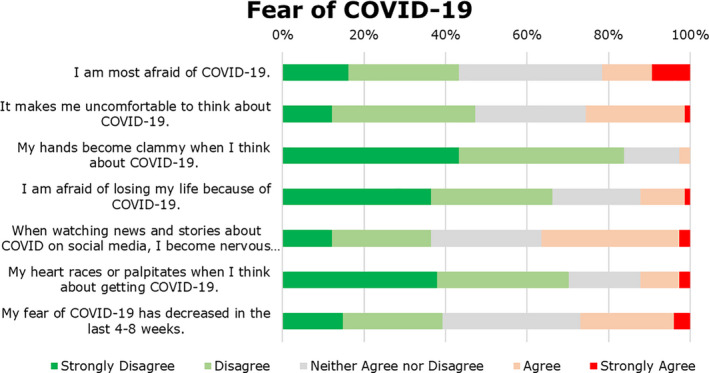
Responses to Modified Fear of COVID‐19 Scale questions.
A substantial proportion of the respondents indicated that they often or always felt tired (61%), physically (27%) or emotionally (35%) exhausted and/or worn‐out (39%) based on the responses to the CBI Personal Burnout questions (Fig. 3, Panel a). Over half of respondents indicated that they often or always felt worn‐out at the end of the working day, with nearly 60% indicating that they Never/Almost Never or Sometimes had enough energy for family and friends during leisure times (Fig. 3, Panel b). There was no indication of patient‐related burnout (Fig. 3, Panel c).
Fig. 3.
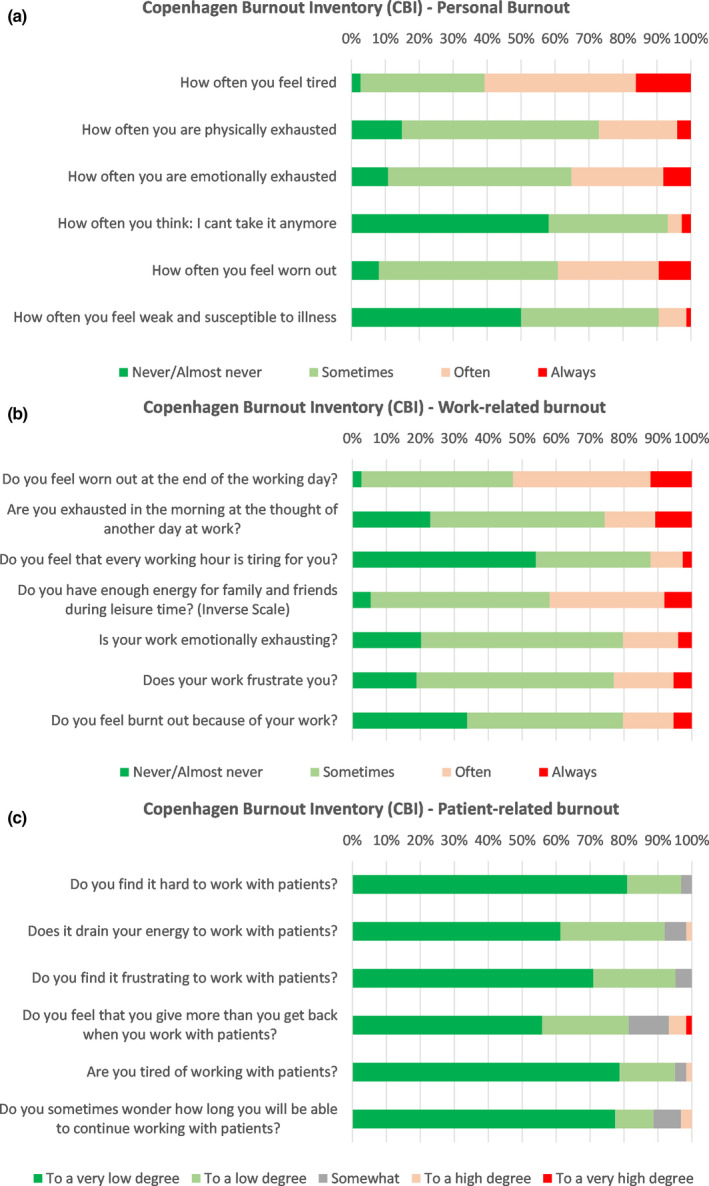
Responses to Copenhagen Burnout Inventory (CBI), Personal Burnout (Panel a), Work‐related burnout (Panel b) and patient‐related burnout (Panel c).
The different modes of communication that were utilised as part of the changes to work arrangements were well received by staff, who were confident in their use (Fig. 4), although some modes were viewed more favourably than others for specific purposes (Panels a–f). For example, phone and/or video conferencing were viewed as effective for communicating thoughts clearly and efficiently, compared to email, text or chat channels. Microsoft Teams chat channels were rated effective when sending messages to other staff members, and when receiving messages in real time. For those communicating directly with patients, phone was rated by far the most effective form of communication, where face‐to‐face contact was not possible or feasible. Electronic Medical Systems (Mosaiq and Aria), which both contain messaging systems, were least effective in communicating clearly or efficiently. The availability of colleagues was also assessed (Fig. 5) with Radiation Oncologists being the most unavailable.
Fig. 4.
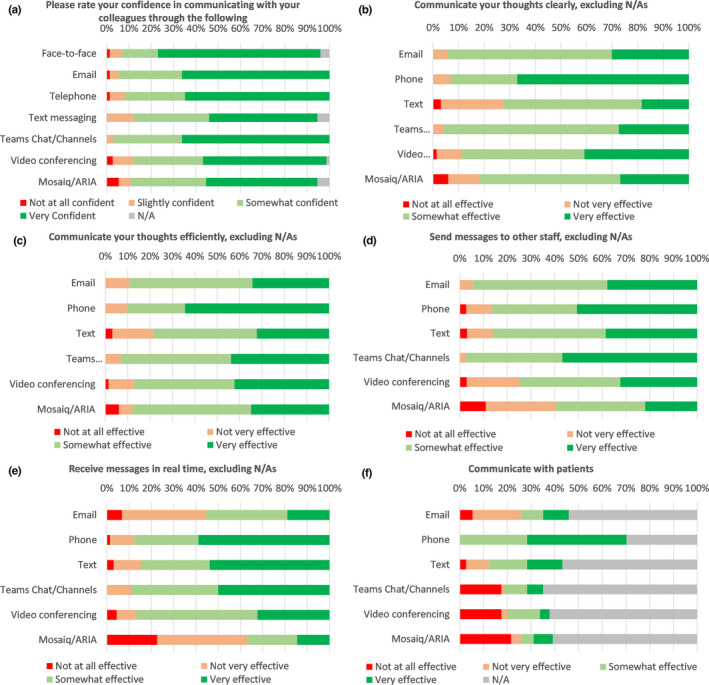
Efficiency of communication platforms for stated purposes (Panels a–f).
Fig. 5.
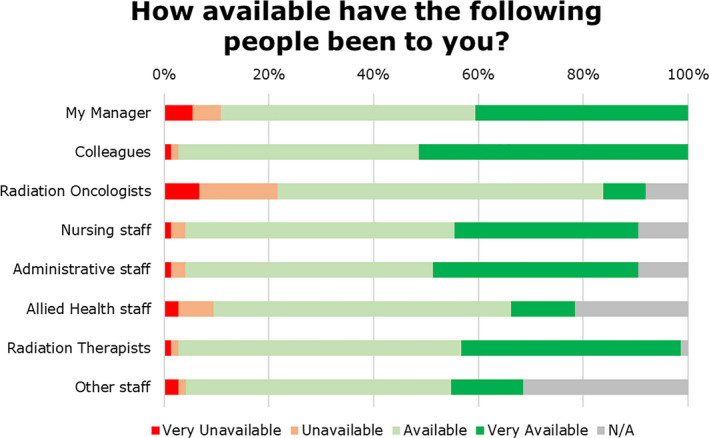
Availability of colleagues.
The majority of staff were either happy, or very happy (73%) with their shift allocation (Fig. 6). Staff with school‐aged children reported being very happy with their allocation of shift (58%) and those without children were very happy (24%). Staff with or without children reported similar levels of happiness with their work‐from‐home/work‐from‐work arrangements and their happiness to continue with such arrangements for another 6 months. Having, or not having, children did not result in any significant differences in survey response.
Fig. 6.
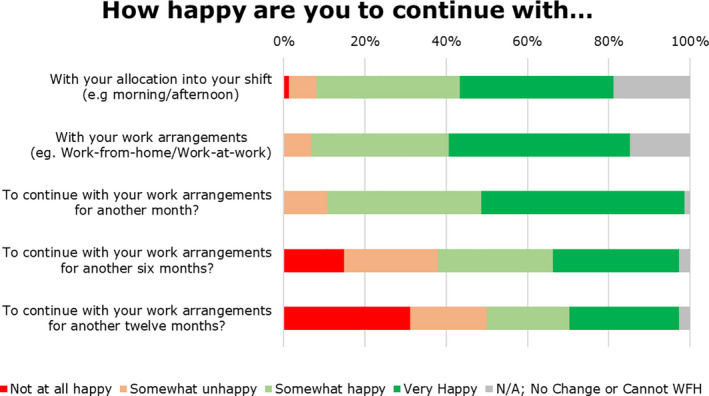
Staff satisfaction with shift, work‐from‐home/work and willingness to continue over one, six and twelve months.
Discussion
The rapidly changing and escalating situation with COVID‐19 across the world has posed many challenges to numerous organisations, particularly those related to healthcare provision, clinical research and education. It was clear, based on experience with SARS, 16 that changes needed to be implemented to minimise risk to cancer patients and staff. An underlying concern was the risk of loss of large numbers of staff due to infection, caring for sick relatives or quarantine due to exposure to an active COVID‐19 case. Service changes, policies and individual patient decision‐making should aim to reduce the risk of COVID‐19 to our patients while maintaining high‐quality oncologic care. Technological changes implemented also reduced staff interactions with other staff and patients.
Between April and November 2020, during which two COVID‐19 surges occurred, patient treatment was prioritised over other activities. Staff deployment was focussed on treatment delivery, with clinical and technical staff involved in research, development and education transferred to treatment delivery. Research, development and education activities were curtailed. The service moved to longer clinical days using a segregated workforce paired with segregated patient groups. With these strategies, overall treatment activity levels were maintained at levels similar to those of pre‐COVID‐19 times. Some treatment regimens were hypo‐fractionated, with fewer hospital visits, but with the same cancer control outcome. These treatment regimen changes reduced the number of per patient visits into the hospital. Many of the treatment regimens are standard of care in European centres and have been recommended for use in the Australian (Victorian) setting during COVID‐19. 18 , 32 These changes were explained to patients by their Oncologist. This approach also aligns with strategies developed to optimise limited resources in a time of heightened risk for patients and staff. 18 Staff input to proposed changes was actively sought, and a formal, yet rapid change implementation strategy was adopted.
This was an exploratory study of staff reactions to these changed work practices. There are some limitations in the evaluation of the changes. Our staff were not asked specifically about challenges of participation from home such as access to privacy or competing childcare/home schooling responsibilities. The findings from this study will clearly not be applicable to all types of healthcare settings and, although Victorian health facilities were impacted by COVID‐19, it is important to be aware that the community case load never approached those seen in the peaks in North America or Europe.
There are limitations to the data presented in this study. First, the changes were rapidly instituted and wider consultation and planning may have improved staff experience and acceptance of changes. The study surveys were developed and implemented quickly without pilot testing. Our response rate of 57%, while reasonable, may reflect the lockdown period and multiple demands on staff time. As with all surveys, there is risk of responder bias, given not all staff members completed the survey. It is possible that those who did not complete the survey may have held different views to those reported here. The study was instigated after the start of the COVID‐19 pandemic; consequently, baseline scores on the measures of interest were not available and changes to these following COVID‐19 could not be measured. Nonetheless, the descriptive analysis of the responses to individual questions reported here provided a snapshot of employee responses to the changes and associated wellbeing.
Notwithstanding the limitations described above, with the rapidly evolving COVID‐19 pandemic it is important to highlight the impacts of COVID‐19 on staff in an Australian Radiation Oncology Setting.
In conclusion, the exploratory study findings identify and provide support for operational changes within a Radiation Oncology service that effectively maintains staff satisfaction and full patient activity during a COVID‐19 pandemic. Descriptive data obtained from staff confirmed high levels of happiness with the changes made and identify operational efficiencies that can be retained in a post‐COVID‐19 environment.
K Rykers PhD, MACPSEM; M Tacey MBiostat, BSc; J Bowes BSc; K Brown B.AppSci; E Yuen MSc, PhD; C Wilson BA (Hons), MBA, PhD; R Khor MBBS, BMedSc, FRANZCR, DMedSc; F Foroudi MBBS (Hon 1), MPA, DMedSc, FRANZCR.
Conflict of interest: The authors have no conflicts of interest to declare.
References
- 1. Holshue ML, DeBolt C, Lindquist S et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382: 929–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu F, Zhao S, Yu B et al. A new coronavirus associated with human respiratory disease in China. Nature 2020; 579: 265–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wu F, Zhao S, Yu B et al. Author Correction: a new coronavirus associated with human respiratory disease in China. Nature 2020; 580: E7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Australia Government Department of Health. [Cited 2020 24 Dec 2020.] Available from URL: https://www.health.gov.au/news/health‐alerts/novel‐coronavirus‐2019‐ncov‐health‐alert/coronavirus‐covid‐19‐current‐situation‐and‐case‐numbers#cases‐active‐cases‐and‐deaths‐by‐state‐and‐territory2020
- 5. Victorian coronavirus (COVID‐19) data. Department of Health and Human Services, State Government of Victoria, Australia. [Cited 2020 24 Dec 2020.] Available from URL: https://www.dhhs.vic.gov.au/victorian‐coronavirus‐covid‐19‐data
- 6. Gehrie E, Tormey CA, Sanford KW. Transfusion service response to the COVID‐19 pandemic. Am J Clin Pathol 2020; 154: 280–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McCabe R, Schmit N, Christen P et al. Adapting hospital capacity to meet changing demands during the COVID‐19 pandemic. BMC Med 2020; 18: 329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tey J, Ho S, Choo BA et al. Navigating the challenges of the COVID‐19 outbreak: perspectives from the radiation oncology service in Singapore. Radiother Oncol 2020; 148: 189–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Valand P, Lloyd N, Robson M, Steele J. Trauma transformed: a positive review of change during the COVID‐19 pandemic. J Plast Reconstr Aesthet Surg 2020; 73: 1357–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wei W, Zheng D, Lei Y et al. Radiotherapy workflow and protection procedures during the Coronavirus Disease 2019 (COVID‐19) outbreak: experience of the Hubei Cancer Hospital in Wuhan, China. Radiother Oncol 2020; 148: 203–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kang JJ, Wong RJ, Sherman EJ et al. The 3 Bs of cancer care amid the COVID‐19 pandemic crisis: "Be safe, be smart, be kind"‐a multidisciplinary approach increasing the use of radiation and embracing telemedicine for head and neck cancer. Cancer 2020; 126: 4092–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wakefield DV, Sanders T, Wilson E et al. Initial impact and operational responses to the COVID‐19 pandemic by American Radiation Oncology practices. Int J Radiat Oncol Biol Phys 2020; 108: 356–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Romani C, Conlon M, Oliver M et al. The operation of Canada’s only virtually operated radiation oncology service during the COVID‐19 pandemic. Adv Radiat Oncol 2021; 6: 100634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Anderson N, Thompson K, Andrews J et al. Planning for a pandemic: mitigating risk to radiation therapy service delivery in the COVID‐19 era. J Med Radiat Sci 2020; 67: 243–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liang W, Guan W, Chen R et al. Cancer patients in SARS‐CoV‐2 infection: a nationwide analysis in China. Lancet Oncol 2020; 21: 335–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mukherjee RK, Back MF, Lu JJ, Shakespeare TP, Wynne CJ. Hiding in the bunker: challenges for a radiation oncology department operating in the Severe Acute Respiratory Syndrome outbreak. Australas Radiol 2003; 47: 143–5. [DOI] [PubMed] [Google Scholar]
- 17. Yu J, Ouyang W, Chua MLK, Xie C. SARS‐CoV‐2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol 2020; 6: 1108–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Thomson DJ, Palma D, Guckenberger M et al. Practice recommendations for risk‐adapted head and neck cancer radiotherapy during the COVID‐19 pandemic: an ASTRO‐ESTRO consensus statement. Radiother Oncol 2020; 151: 314–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chen Y‐L, Hsu F‐M, Tsai CJ, Cheng JC‐H. Efforts to reduce the impacts of COVID‐19 outbreak on radiation oncology in Taiwan. Adv Radiat Oncol 2020; 5: 534–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang L, Zhu F, Xie L et al. Clinical characteristics of COVID‐19‐infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol 2020; 31: 894–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Whitaker M, Kron T, Sobolewski M, Dove R. COVID‐19 pandemic planning: considerations for radiation oncology medical physics. Phys Eng Sci Med 2020; 43: 473–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Turner S, Pham T, Robledo K, Turner S, Brown C, Sundaresan P. Rapid adaptation of cancer education in response to the COVID‐19 pandemic: evaluation of a live virtual statistics and research skills workshop for oncology trainees. J Cancer Educ 2020: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McDowell L, Goode S, Sundaresan P. Adapting to a global pandemic through live virtual delivery of a cancer collaborative trial group conference: the TROG 2020 experience. J Med Imaging Radiat Oncol 2020; 64: 414–21. [DOI] [PubMed] [Google Scholar]
- 24. Horsley PJ, Back M, Lamoury G, Porter B, Booth J, Eade TN. Radiation oncology during COVID‐19: strategies to avoid compromised care. Asia Pac J Clin Oncol 2021; 17: 24–8. [DOI] [PubMed] [Google Scholar]
- 25. Besson J, McNamara C, Brown E. Pivots and pirouettes: adapting a robust departmental CPD and training program to the COVID‐19 crisis. J Med Radiat Sci 2020; 67: 356–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Papachristofilou A, Finazzi T, Kohler G, Dott C, Zimmermann F. Contingency plans in a radiation oncology department amid the 2019‐nCoV outbreak in Switzerland. Adv Radiat Oncol 2020; 5: 577–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Krengli M, Ferrara E, Mastroleo F, Brambilla M, Ricardi U. Running a radiation oncology department at the time of coronavirus: an Italian experience. Adv Radiat Oncol 2020; 5(Suppl 1): 3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Combs SE, Belka C, Niyazi M et al. First statement on preparation for the COVID‐19 pandemic in large German Speaking University‐based radiation oncology departments. Radiat Oncol 2020; 15: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress 2005; 19: 192–207. [Google Scholar]
- 31. Ahorsu DK, Lin C‐Y, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID‐19 scale: development and initial validation. Int J Ment Health Addiction 2020; 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yahalom J, Dabaja BS, Ricardi U et al. ILROG emergency guidelines for radiation therapy of hematological malignancies during the COVID‐19 pandemic. Blood 2020; 135: 1829–32. [DOI] [PMC free article] [PubMed] [Google Scholar]


