Abstract
Aim
To survey nurses' opinions about their work conditions at the onset of the COVID‐19 pandemic in Spain.
Background
For the Spanish General Council of Nursing (the Consejo General de Enfermería de España), it was essential to have information on nursing workforce conditions and nurses' preparedness to wear protective measures at the pandemic's onset. The coronavirus outbreak was believed to have started in China and rapidly spread as a global pandemic requiring policies and actions for planning emergency healthcare delivery.
Methods
A cross‐sectional survey was conducted online. Data were collected during April 2020 and covered social demography, working conditions, training, availability of personal protective equipment, and nurses' health conditions, including the impact of COVID‐19.
Findings
From all national territories in Spain, 11 560 registered nurses from different services completed the questionnaire. Findings indicated that the lack of personal protective equipment was a crucial issue, as well as service planning and organization, and 80.2% reported high or very high psychological impact of COVID‐19. Alarmingly, 29.5% of the nurses reported COVID‐19 symptoms. Of these 23.3% had been tested, and 30.2% were confirmed as being positive to the virus. The nurses deemed proper preparedness for emergencies and disasters as a significant concern.
Conclusion
Nurses’ responses showed evidence of health services deficiencies as a source of damage to their capacity to provide safe patient care and protect themselves and their families' health. The working conditions of the nurses are at critical levels and are unacceptable. The study results provide evidence regarding the necessity of suitable planning and actions being taken to enable safe patient care and safety for nurses.
Implications for Nursing and Health Policy
Our survey gathered nurses' views at the pandemic's onset. The evidence gathered is being used to advise policymakers and nursing organizations to take actions to control public health risks to populations. It is necessary that more investment in growing nursing workforce expertise and health infrastructure for pandemic and epidemic emergencies is provided.
Keywords: COVID‐19, Epidemics, Health and safety, Nurses, Pandemics, Patient safety, Personal protective equipment, Public health emergency, Spain
Introduction and Background
Between December 2019 and February 2020, Spain received news from China and Asia about the novel coronavirus, COVID‐19, a highly infectious disease which caused a significant atypical respiratory syndrome. Within a few weeks, the epidemic escalated exponentially, straining, and collapsing the health system in the areas affected. This scenario, for most of the European population, was only a distant reality. Suddenly, the epidemic spread out from China to neighboring countries in Asia, and swiftly arrived in Europe. Spain was among the first countries where it rapidly expanded, causing a public health emergency. Within two weeks from the first cases, the Spanish Government declared the state of emergency on March 14 to address the expansion of COVID‐19 and cope with its enormous pressure on the health system (Ministry of Health, Consumer Affairs, & Social Welfare 2020a, 2020b, 2020c). The World Health Organization declared COVID‐19 a pandemic episode on March 20 (WHO 2020a,b).
Public health emergencies such as the COVID‐19 pandemic and earlier experience with Ebola, natural disasters and war catastrophe episodes call for urgent strategies and immediate actions to safeguard the population’s health and wellbeing. Most of the evidence analyzed and reported the importance of human resources (Labrague et al. 2018).
COVID‐19 is a beta‐coronavirus, an airborne virus primarily transmitted between people through respiratory droplets (WHO 2020c). This virus transmissibility has been estimated at peak stage to have a reproductive power as high as 4.23 in several countries (Garcia & Moreira 2020; Tang et al. 2020).
Since the outbreak in Europe, the European Union has issued several recommendations considering general scientific knowledge, including all WHO consensus on this matter. These recommendations aimed to support member states in formulating national pandemic plans (European Commission 2020).
Immediate demand for patient care at all levels, especially for critical patients requiring respiratory support, evidenced the profound difficulties and challenges for health services to deliver quality and safe care. The problems stemmed from a lack of materials and equipment such as personal protective equipment (PPE), testing materials, and respirators. Undoubtedly, the most significant challenges pertained to the health workforce, mostly to the fact that members of the two strategic professions—nurses and physicians—were not sufficiently trained to respond to this new situation. As Catton (2020, p.57) acknowledged, this new pandemic is a time of challenge for nursing, but also for "protecting, saving, supporting, and honoring nurses." Earlier emergencies and disasters have shown that health services require human resources relocation in emergencies, moving nurses and physicians in different units to the intensive care unit (ICU) or other strategic services, as well as overtime (Cerón‐Serrano et al. 2016; Li et al. 2017). Previous and current research has also shown a critical spectrum of psychosocial impacts on health professionals and the population (García‐Iglesias et al. 2020; Wang et al. 2020; Wu & Wei 2020).
Faced with this scenario, the Spanish General Council of Nursing (SGCN) launched actions to inform policymakers and stakeholders to ensure safe work and health conditions for nurses. The SGCN, as a regulatory body, was concerned that the impact of the pandemic on nurses could affect their ability to provide quality and safe care to the populations. This scenario implies the vulnerability of nurses to infection and poses ethical dilemmas. The limited resources and protection equipment, the absence of standards and guidelines, and lack of full knowledge of coronavirus behavior are issues underlying psychological distress and ethical problems. This leads to low morale associated with workplace difficulties to provide care, burnout and other emotional issues (Oh & Gastmans 2015; Rushton et al. 2017).
The earliest initiatives taken by the SGCN pertained to information and guidelines documents, as well as videos for nurses and the general population channeled through the institutional website of SGCN in 2020 (see these documents on https://www.consejogeneralenfermeria.org/covid‐19). Simultaneously, the SGCN launched a national survey to establish the work conditions of nurses involved in COVID‐19 care and their impact. As is widely acknowledged, a survey is a reliable and fast instrument to obtain information from a large population within a limited space of time (Pinsonneault & Kramer 1993). The primary purpose of the SGCN was to learn how the Spanish Health Services were managing their commitment to delivering safe nursing care. It was essential to acquire knowledge of nurses’ working conditions, preparedness, and the possible effect on their health.
Aim
The aim of the study was to gather nurses’ opinion during the onset of the COVID‐19 in Spain about their working conditions and experiences.
Methods
Design, participants and settings
This study involved a cross‐sectional survey to assess the immediate view of the impact of COVID‐19 on Spanish nursing using an anonymous online questionnaire. The surveyed population consisted of nurses working in the Spanish Health Services in specialized and primary healthcare settings at the onset of the pandemic outbreak. Through all institutional communication media (email, social networks, and web posts), all nurses registered with the SGCN and actively working in care settings and who had formally accepted to receive news and information were invited to participate in the survey through a link to this. The Spanish Ministry of Health declared that 255 000, or 90% of the total nurses in Spain, were active in the workforce. Full questionnaire answers from 11 156 nurse respondents were finally included in the survey. These respondents may well characterize a typical simple sample size with an estimated global error of ± 0.93% for a confidence level of 95.5%.
Procedure
Information about the survey was posted on all SGCN communication tools. Through the Computer‐assisted Web Interview (CAWI), the online questionnaire is an Internet surveying technique in which the interviewer follows a script provided on a website. Data collection took place between 9 and 20 of April 2020, three weeks after the first declaration of the state of emergency in Spain.
Instrument
The SGCN consulted with nursing experts and technical advisors with experience in or knowledge of nursing care in emergencies and epidemic episodes for reference, and to support the questionnaire design. The questionnaire covered the following content areas: (a) demographic data: gender, years of experience, work setting, province of employment; (b) working conditions: workstation related to COVID‐19, daily schedule; (c) training: the amount of content on coronavirus, handling of protective equipment (past and current); (d) equipment availability: PPE, instruments, and other materials; (e) health effects: infection among nurses, family, or friends; influence on psychological status; and (f) pandemic evolution: expectations and appraisal of actions carried out by decision‐makers. The final tool included 22 multiple‐choice items. The questionnaire was pilot proofed for suitability for the purpose of the survey and clear language. However, formal validity and reliability testing were not conducted due to the timelines under the epidemic.
Respondents were asked to select multiple‐choice options or give a rating according to their feelings, evaluate statements given in the instrument, and fill in the open fields with personalized comments.
Adjustments for territorial distribution
Adjustments for the total number of nurses were weighted for territorial distribution by province within each Autonomous Region (Spanish legal territory). This adjustment used the nurse distribution reported by the National Institute of Statistics (INE 2020) and the SGCN register (Table S1: Rebalance of nurse respondents by Spanish region).
Statistical analysis
Descriptive statistics were calculated for the real data obtained from the questionnaire. The response percentages were based on the number of respondents per item with respect to the total number of responses per question and given in cross‐frequency and straightforward tabulation. The analysis was conducted using Gandia Barbwin, a statistical processor for the recording and tabulation of survey data.
Ethical considerations
Under the current legislation in Spain, Law 14/2007, of 3 July on Biomedical Research, this type of survey‐based study did not require the supervision of an ethics committee. However, the SGCN Executive Committee approved this study and notified all levels of the Spanish professional nursing associations through Memorandum 59/2020 on 9 April 2020.
The anonymity and confidentiality of the responses were guaranteed, assuring respondents that all their information would only be used to develop the tables and the analysis. Taking and returning the online questionnaire was assumed as agreement to participate in the survey.
Findings
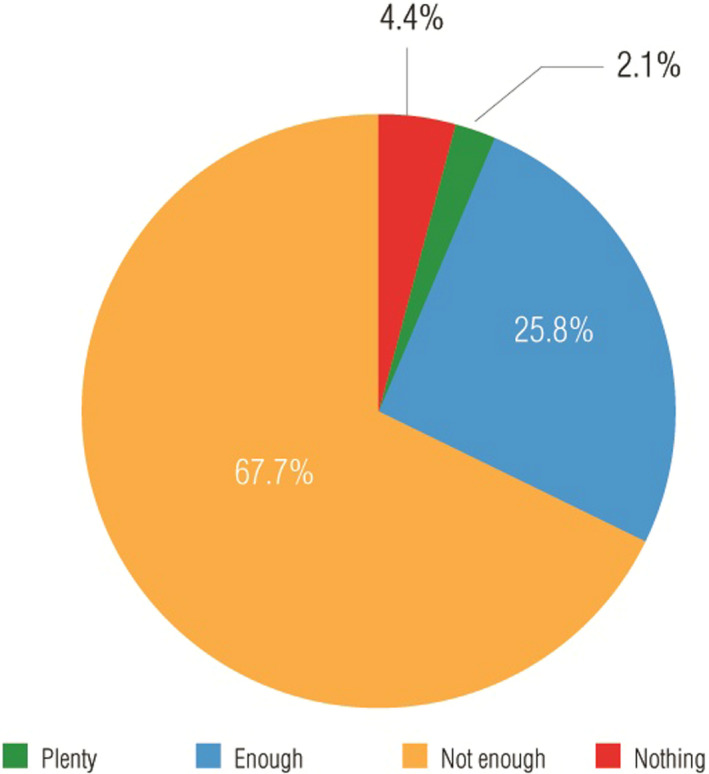
Table 1 shows the respondents’ demographic characteristics and their work conditions at the onset of the pandemic in Spain. The 11,156 complete questionnaires were included. The majority of respondents were female (81.3%), which matched the female nurse ratio in the National Institute of Statistics data. A majority (64%) of nurses had 16 or more years’ experience, and a small proportion (9.1%) had less than 10 years’ experience. Respondent distribution in hospital working settings was spread evenly between the intensive care unit (ICU) and the A&E services (12.2% and 11.2% respectively), with 34.4% stationed in clinical wards, and 18.9% of respondents working in primary healthcare services. Social healthcare includes nursing homes and palliative care units, where participation was lower (5.4%). The remaining 15% included positions that amounted to less than 2.5% of participation, such as hemodialysis departments, outpatient specialty services, day hospital teaching/university, laboratories, and a nursing school. Concerning their working conditions, most respondents (73.4%) reported that their workstation had remained the same as before the pandemic; only 22.7% were either transferred from a ward or another center or had a new work contract. The work schedule of the majority (77.6%) was committed full time to COVID‐19 care, and 22.5% reported little or no involvement with such care. Specific training on the virus and the use of PPE was extremely low or non‐existent for 76.2% and 82.2%, respectively. The availability of PPE was more frequent for masks (73.9%), protection overalls (55.3%), protective gowns 49.2%; and the availability of the remaining PPE was under 50% (Fig. 1 reflects the availability of material resources). Of all respondents, a minority reported little or no psychological impact of COVID‐19 (18.1% and 1.7% respectively), in contrast with a large majority (80.2%) who described a very high or high psychological impact.
Table 1.
Sociodemographic characteristics, COVID 19 working conditions, training and psychological effects (N = 11 044)
| Content areas | Respondents | |
|---|---|---|
| n | % | |
| Demographic data | ||
| Gender | ||
| Male | 2066 | 18.70 |
| Female | 8978 | 81.30 |
| Work experience (years) | ||
| 0–5 | 1005 | 9.10 |
| 06–10 | 1049 | 9.50 |
| 11–15 | 1844 | 16.60 |
| >16 | 7101 | 64.60 |
| Student | 22 | 0.20 |
| Work setting | ||
| Hospital | ||
| ICU | 1347 | 12.20 |
| General wards | 3799 | 34.40 |
| Operating theater | 298 | 2.70 |
| A&E services | 1237 | 11.2 |
| PHC | 2082 | 18.9 |
| Health & social care | 596 | 5.4 |
| Others | 1678 | 15.2 |
| COVID‐19 working conditions | ||
| Workstation | ||
| Same as previous | 8228 | 73.4 |
| Transfer from wards/centers | 1989 | 18.0 |
| New work contract | 519 | 4.7 |
| Other | 298 | 3.9 |
| Daily schedule for COVID‐19 care | ||
| Full time | 5047 | 45.7 |
| Half time | 3523 | 31.9 |
| Little/None | 1369 | 22.4 |
| Training | ||
| COVID‐19 program content | ||
| Significant | 331 | 3.0 |
| Enough | 1685 | 20.8 |
| Little | 5964 | 54.7 |
| None | 3081 | 21.5 |
| Use of PPE | ||
| Plenty | 287 | 2.6 |
| Enough | 1668 | 15.2 |
| Little | 5997 | 54.3 |
| None | 3081 | 27.9 |
| Psychological impact of COVID‐19 | ||
| Very high | 2938 | 26.6 |
| High | 5920 | 53.6 |
| Little | 1999 | 18.1 |
| None | 187 | 1.7 |
A&E, Accident and Emergency Services; ICU, Intensive Care Unit; PCR, Polymerase Chain Reaction; PHC, Primary Health care; PPE, Personal Protective Equipment
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Figure 1.
Availability of material resources and personal protective equipment in the workplace. Source: COVID‐19 Impact on nursing. Spanish General Council of Nursing. April 2020.
The availability of PPEs was more frequent for masks (73.9%), protective gowns (55.3%), protective overall gowns 49.2%, while all remaining PPE was under 50% (Fig. 1 Illustrates the availability of material resources).
Verbatim testimonials collected through the open response option "Other Materials" in the survey provided qualitative comments, describing the respondents’ feelings and conditions in their arduous work scenarios. These are some representative examples:
We received material from the population; it is not the same kind as the material distributed by the supply center.
What we receive is of poor quality.
We spent the 14‐hour shift wearing the same masks.
The supply center informs of their plan to sterilize the PPE2 if it becomes scarce, and they ask you to save what you have for the next shift in case they run out.
We have to use single‐use protective equipment, and we are using it for as long as a week or more.
PPE 2/3 masks are required because I consider their reuse for one week unacceptable. It is stressful when I take off my mask, put it in an envelope in my locker, and reuse it the next day, the same happens with previously disinfected waterproof gowns. These conditions do not provide safety. I stay at my workplace throughout my shift without even going to the toilet, as the PPE I have is for my entire shift, and I see a time of potential contamination when I take it off and put it back on.
Re‐sterilize gowns and wear masks for several shifts, We're buying the stuff ourselves. PPE 2 masks and gowns are worn for six shifts.
Waterproof boots/shoes are unsuitable, what we receive covers the only the sole, and when you take the first step it’s left behind.
Operating theatre protocols are now overlooked, and you have to use what is available at the moment.
We don't have and haven't had a single protective gown.
Alarmingly, over a quarter of respondents (29%) reported COVID‐19 symptoms. This meant that potentially around 73 950 nurses of 255 000 in the total nursing workforce in the health services had been infected at the time of this study. Only 23.3% of symptomatic respondents had been tested for the virus, and 30.2% of these tested positive. The details are given in Table 2.
Table 2.
Respondents results for COVID‐19 symptomatic condition, PCR test, positive results by Spanish regions (N 11 043)
| Autonomous regions | Respondents | Symptomatic | PCR | ||||
|---|---|---|---|---|---|---|---|
| Tested | Positive | ||||||
| Yes | Yes | ||||||
| N | n | % | n | % | n | % | |
| Andalucía | 1590 | 332 | 20.9 | 64 | 19.2 | 9 | 13.7 |
| Aragón | 353 | 75 | 21.3 | 12 | 16.0 | 2 | 17.6 |
| Asturias | 265 | 64 | 24.2 | 14 | 21.2 | 1 | 4.8 |
| Baleares, Islas | 254 | 59 | 23.4 | 11 | 17.9 | 1 | 7.7 |
| Canarias | 144 | 35 | 24.1 | 7 | 20.9 | 1 | 11.1 |
| Cantabria | 530 | 107 | 20.2 | 42 | 39.5 | 3 | 7.8 |
| Castilla y León | 464 | 132 | 28.5 | 29 | 21.9 | 10 | 35.3 |
| C. la Mancha | 674 | 270 | 40.1 | 67 | 24.7 | 40 | 60.4 |
| Catalunya | 1855 | 577 | 31.1 | 170 | 29.5 | 48 | 28.4 |
| C. Valenciana | 1016 | 233 | 22.9 | 40 | 17.1 | 7 | 18.6 |
| Extremadura | 287 | 74 | 25.8 | 18 | 24.0 | 4 | 23.9 |
| Galicia | 563 | 99 | 17.5 | 20 | 20.2 | 3 | 14.1 |
| Madrid | 1756 | 841 | 47.9 | 257 | 30.6 | 138 | 53.7 |
| Murcia | 265 | 39 | 14.6 | 3 | 8.5 | 0 | 14.3 |
| Navarra | 232 | 61 | 26.2 | 13 | 21.1 | 4 | 32.4 |
| País Vasco | 674 | 183 | 27.1 | 37 | 20.0 | 12 | 32.9 |
| Rioja, La | 77 | 20 | 25.9 | 7 | 32.7 | 2 | 29.2 |
| Ceuta | 22 | 3 | 13.9 | 1 | 19.4 | 0 | 42.9 |
| Melilla | 22 | 4 | 20.2 | 1 | 24.0 | 0 | 0.0 |
| Total | 11043 | 3208 | 29.05 | 761 | 257 | ||
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Discussion
The purpose of this SGCN survey was to inform health policymakers and the professional nursing associations about nurses’ working conditions at the onset of the COVID‐19 pandemic in Spain. The evidence obtained suggests that nurses were working under stress and frightened by the scarcity of proper PPE. Moreover, there was a lack of specific knowledge and training to care for COVID‐19 patients and the correct use of PPE.
At the onset of the pandemic, international institutions, governments, and nursing organizations issued guidelines for workforce protection, guided by four main principles: maintenance of social distance; covering mouth and nose; ensuring hand hygiene; and surface cleaning (OSHA 2020; Organisation for Economic Co‐operation and Development 2020; International Council of Nurses 2020,2020).
In addition, numerous studies recently published about nurses and other health professionals working during emergencies mention workforce health protection issues, clearly stressing specific training and psychological impact (Choi & Kim 2016; Labrague et al. 2018; Park et al. 2018). In this survey, the evidence also demonstrated similar issues, emphasizing the lack of equipment. The huge extent of this pandemic has shown that the working conditions of the nursing workforce are critical (Garcia‐Iglesias et al. 2020; Waslton et al. 2020; Wu & Wei 2020) and inacceptable.
This SGCN survey shows a higher degree of participation from experienced nurses. This could be attributed to greater professional awareness or likelihood of being placed in general wards, or a higher degree of engagement in SGCN activities. The literature on emergencies does refer to more preparedness and awareness among more experienced nursing personal in emergencies and catastrophes (Choi & Kim 2016; Li et al. 2017; Noto et al. 2013; Richardson et al. 2013; Ruymán et al. 2020).
The high proportion of daily care hours spent on COVID‐19 patients by respondents is also reported in other emergencies and disasters experienced by nurses in Japan, China, and Turkey, among other recent events (Labrague 2018; Yane 2015). Preparedness for emergencies and disasters is an essential concern for nurses all over the world, and training for these events is an important area of nursing specialization. Nevertheless, some specific characteristics of a new transmissible disease outbreak such as the COVID‐19 pandemic, where there is no direct knowledge about the virus and how to most effectively organize immediate safe care, make the results ambiguous (Tay et al. 2020). Respondents reported a lack of knowledge about the COVID‐19 and training in proper use of PPEs, which added to the high level of stress suggested by the survey.
As mentioned by Ranney et al. (2020), the lack of adequate PPEs for healthcare workers on the frontline yielded high rates of infections in this survey, which suggests a relatively high level of symptomatic nurses who that continued working (Raurell‐Torredà 2020).
Limitations
This survey has limitations. Given the need for direct evidence related to the real conditions and the safety of nurses working in the Spanish Health Services, the instrument could not be refined or undergo specific reliability and validity tests. There was no sampling system, so respondents were not randomly selected and may not reflect to the actual population of working nurses in Spain. For anonymity, confidentiality, and ethical reasons, the survey respondents were not contacted to add information or clarify their remarks. Due to all these issues, the evidence cannot be generalized. However, despite these problems, the survey served the purpose sought by the SGCN of gathering to gather evidence that would inform political decision‐makers and stakeholders, leading them to take immediate actions to improve working conditions of nurses.
Conclusions
The SGCN launched a quick survey to be able to inform decision‐making and the actions taken to assist working nurses in their commitment to care. Therefore, this survey is an instrument to draft guidelines, protocols, provide safe ways to deal with the conditions of scarcity of PPEs and specific instruments, and modify the work environment to ensure safe care and protection.
Implications for Nursing and Health Policy
In general, surveys provide essential evidence and enable immediate understanding of an ongoing situation. The SGCN provided the nurses with an opportunity to express their real working conditions and their fears, gathering the necessary information to advise policymakers, nursing associations, and other nursing groups. The results suggest that the lack of personal protection equipment was crucial, and authorities should focus on providing this material. Another issue was the need to organize the work, which required special attention from a profession focusing on care of COVID patients.
This pandemic poses ethical challenges for nurses on a daily basis. Even though incidence has decreased, the virus is still present, and new cases continue to emerge. The supply of essential safety equipment and instruments to combat the virus remains critical. Nurses need to keep their guard up to meet their commitments to quality patient care while protecting their families and themselves. Medical technologies in the health system remain precarious; medical providers struggle to balance their duties to their patients, their families, and themselves.
Author contributions
Study conception/design: FPR, PFF, JARG
Data collection/analysis: AS, DAM, JLCS
Manuscript Writing: JLCS, AS, PFF, FPR
Critical revisions for important intellectual content: AS, JLCS, DAM, PFF, JARG.
Supporting information
Table S1. Survey respondents rebalanced to specific weight of active nurses distribution by autonomous community.
Acknowledgements
The authors would also like to thank Spanish nurses at the health services in all national territories who, in a time of hardworking conditions and stress, completed the survey. All the Nursing Official Provincial Colleges members of the Spanish Collegial Organization assisted in the dissemination of the information about the survey in their territories.
Pérez‐Raya F., Cobos‐Serrano J.L., Ayuso‐Murillo D., Fernández‐Fernández P., Rodríguez‐Gómez J.A. & Almeida Souza A. (2021) COVID‐19 impact on nurses in Spain: a considered opinion survey. Int. Nurs. Rev. 68, 248–255
Funding: This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors.
Conflict of interest: No conflict of interest has been declared by the authors.
References
- Catton, H. (2020) Nursing in the COVID‐19 pandemic and beyond: protecting, saving, supporting, and honouring nurses. International Nursing Review, 57 (2), 157–159. 10.1111/inr.12593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerón‐Serrano, A. , Jiménez‐González, R. & Gómez‐Campos, A.M. (2016) Prevention and nursing care in the first case of Ebola virus disease contracted outside Africa. Enfermeria clínica, 27 (2), 125–131. 10.1016/j.enfcli.2016.11.003. (in Spanish). [DOI] [PubMed] [Google Scholar]
- Choi, J.S. & Kim, K.M. (2016) Crisis prevention and management by infection control nurses during the Middle East respiratory coronavirus outbreak in Korea College of Nursing, The Catholic University of Korea, Seoul, South Korea. American Journal of Infection Control, 44 (4), 480–481. 10.1016/j.ajic.2015.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Commission . (2020) EU recommendations for community measure, 18 March 2020. Available at: https://ec.europa.eu/info/sites/info/files/covid19_‐_eu_recommendations_for_community_measures.pdf (accessed 25 March 2020). [Google Scholar]
- García Iglesias, J.J. , et al. (2020) Impact of SARS‐CoV‐2 (Covid‐19) on the mental health of healthcare professionals: a systematic review. Revitas Española de Salud Pública, 94, 23. de julio e1–20 (in Spanish). [PubMed] [Google Scholar]
- García‐San Miguel, L. & Portela‐Moreira, A. (2020) COVID‐19 Transmissibility. Revista Española de Salud Pública, Píldora científica (Supl.). Available at: https://www.mscbs.gob.es/biblioPublic/publicaciones/recursos_propios/resp/revista_cdrom/Suplementos/Pildoras/pildora29_transmisibilidad_covid_19.pdf. [Google Scholar]
- International Council of Nurses (ICN) (2020) Covid‐19 & International Year of the Nurse and the Midwife 2020. Available at: https://www.2020yearofthenurse.org/ (accessed 5 July 2020) [Google Scholar]
- International Council of Nursing (ICN) (2020) Data on infected healthcare workers and access to protective equipment vital in prevention of the virus. 20 February 2020. Available at: https://www.icn.ch/news/icn‐covid‐2019‐update‐data‐infected‐healthcare‐workers‐and‐access‐protective‐equipment‐vital (accessed 20 March 2020). [Google Scholar]
- Labrague, L.J. , et al. (2018) Disaster preparedness among nurses: a systematic review of literature. International Nursing Review, 65 (1), 41–53. 10.1111/inr.12369. [DOI] [PubMed] [Google Scholar]
- Li, Y.H. , et al. (2017) Disaster Nursing experiences of Chinese nurses responding to the Sichuan Ya’an earthquake. International Nursing Review, 64 (2), 309–317. 10.1111/inr.12316. [DOI] [PubMed] [Google Scholar]
- National Institute of Statistics (INE) (2020) Nursing data. Available at: https://www.ine.es/ accessed 18 June 2020) (in Spanish). [Google Scholar]
- Noto, Y. , et al. (2013) Role of nurses in a nuclear disaster: experience in the Fukushima Dai‐ichi nuclear power plant accident. International Nursing Review, 60 (2), 196–200. 10.1111/inr.12014. [DOI] [PubMed] [Google Scholar]
- Oh, Y. & Gastmans, C. (2015) Moral distress experienced by nurses: a quantitative literature review. Nursing Ethics, 22 (1), 15–31. 10.1177/0969733013502803. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co‐operation and Development (2020) Workforce and Safety in Long‐Term Care during the COVID‐19 pandemic. Available at: http://www.oecd.org/coronavirus/policy‐responses/workforce‐and‐safety‐in‐long‐term‐care‐during‐the‐covid‐19‐pandemic‐43fc5d50/ [Google Scholar]
- Occupational Safety and Health Administration (2020) Protecting Workers during a Pandemic. OSHA Fact Sheet. Available at: https://www.osha.gov/Publications/OSHAFS‐3747.pdf (accessed 20 June 2020). [Google Scholar]
- Park, J.S. , et al. (2018) Mental health of nurses working at a government‐designated hospital during a MERS‐CoV outbreak: a cross‐sectional study. Archives of Psychiatric Nursing, 32 (1), 2–6. 10.1016/j.apnu.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinsonneault, A. & Kraemer, K. (1993) Research methodology in management information systems. Journal of Management Information Systems ‐ Special Section: Strategic and Competitive Information Systems Archive, 10, 75–105. [Google Scholar]
- Ranney, M.L. , Griffeth, V. & Jha, A.K. (2020) Critical supply shortages — The need for ventilators and personal protective equipment during the Covid‐19 pandemic List of authors. New England Journal of Medicine, 382 (18), e41. 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- Raurell‐Torredà, M. (2020). Management of ICU nursing teams during the Covid‐19 pandemic. Enferm Intensiva, 31, 49–51 (in Spanish). 10.1016/j.enfie.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson, S. , Ardagh, M. , Grainger, P. & Robinson, V. (2013) A moment in time: emergency nurses and the Canterbury earthquakes. International Nursing Review, 60 (2), 188–195. 10.1111/inr.12013. [DOI] [PubMed] [Google Scholar]
- Rushton, C.H. , Schoonover Shoffner, K. & Kennedy, M.S. (2017) Transforming moral distress into moral resilience in nursing. American Journal of Nursing, 117 (2), 52–56. 10.1097/01.NAJ.0000512298.18641.31. [DOI] [PubMed] [Google Scholar]
- Ruymán Brito, P.R. , Fernández Gutiérrez, D.A. & Cuéllar Pompa, L. (2020) Emotional management of the health crisis by coronavirus: A narrative review. Enferm clín.Enfermería Clínica. 10.1016/j.enfcli.2020.05.010 (in press). (in Spanish). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spain. Ministry of Health, Consumer Affairs, and Social Welfare (2020a). Assessment of the outbreak declaration of the new coronavirus 2019 (n‐CoV) a Public Health Emergency of international importance 2020/01/31. Available at: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov‐China/documentos/Valoracion_declaracion_emergencia_OMS_2019_nCoV.pdf (accessed 17 July 2020) (in Spanish). [Google Scholar]
- Spain. Ministry of Health, Consumer Affairs, and Social Welfare (2020b). Coronavirus. Technical Documents for professionals. Available at: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos.htm?fbclid=IwAR1wNi_voVEhLi4a3Xxs7xMmhrq4GCjfY4_tOvB3YSBrmM8CVyjNXII8Kkk (accessed 24 June 2020) (in Spanish). [Google Scholar]
- Spain. Ministry of Health, Consumer Affairs, and Social Welfare (2020c). Press release. Actual Information about the outbreak. Health Information 2020. Available at: www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov‐China/home.htm (accessed 25 March 2020) (in Spanish). [Google Scholar]
- Spanish General Council of Nursing (2020) COVID‐19. Available at: https://www.consejogeneralenfermeria.org/ accessed March‐Jun 2020. [Google Scholar]
- Tang, B. , et al. (2020) Estimation of the transmission risk of 2019‐nCov and Its implication for public health interventions. SSRN Electronic Journal, 10.2139/ssrn.3525558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tay, M.Z. , et al. (2020) The trinity of COVID‐19: immunity, inflammation, and intervention. Nature Reviews Immunology, 20, 363–374. 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. , et al. (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. Int J Environ Res Public Health, 17 (5), 1729. 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waslton, M. , Murray, E. & Christian, M.D. (2020) Mental health care for medical staff and affiliated healthcare workers during the COVID‐19 pandemic. European Heart Journal: Acute Cardiovascular Care, 9 (3), 241–247. 10.1177/2048872620922795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2020a) WHO Director‐General’s opening remarks at the media briefing on COVID‐19 ‐ 11 March 2020. WHO, Geneva. Available at: https://www.who.int/dg/speeches/detail/who‐director‐general‐s‐opening‐remarks‐at‐the‐media‐briefing‐on‐covid‐19‐11‐march‐2020 (accessed 30 March 2020). [Google Scholar]
- World Health Organization (WHO) (2020b) Timeline of WHO’s response to COVID‐19. January 30 Outbreak declaration. March 11. WHO, Geneva. Available at: https://www.who.int/news‐room/detail/27‐04‐2020‐who‐timeline‐covid‐19?gclid=EAIaIQobChMI9vjl2Kr16gIVE7LVCh0XzgJIEAAYASAAEgLLAfD_BwE (accessed 27 May 2020). [Google Scholar]
- World Health Organization (WHO) (2020c) Naming the coronavirus disease (COVID‐19) and the virus that causes it. WHO, Geneva. Available at: https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/technical‐guidance/naming‐the‐coronavirus‐disease‐(covid‐2019)‐and‐the‐virus‐that‐causes‐it (accessed 27 February 2020). [Google Scholar]
- Wu, K. & Wei, X. (2020) (2020) Analysis of psychological and sleep status and exercise rehabilitation of front‐line clinical staff in the fight against COVID‐19 in China. Med Sci Monit Basic Res., 26, e924085–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yane, Y.E. , et al. (2015) Disaster nursing skills, knowledge and attitudes required in earthquake relief: implications for nursing education. International Nursing Review, 62 (3), 351–359. 10.1111/inr.12175. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Survey respondents rebalanced to specific weight of active nurses distribution by autonomous community.


