Abstract
Introduction. Surviving and thriving of newborn is essential to ending extreme poverty. However, the surviving and thriving of new born is depends on where neonates are born. The true feature of neonatal mortality rate and trends is not well known in the study area. Thus, we aimed to estimate a neonatal mortality incidence in each year, and determine factors associated though pregnancy observation cohort study in Eastern Ethiopia. Methods. The study was conducted in Kersa Health Demographic Surveillance System (KHDSS) among 36 kebeles. We extracted all events (38 541 live birth and 776 neonatal death) occurred between January 1, 2008 and December 30, 2019. Neonatal mortality rate was presented by neonatal death per 1000 live birth with 95% confidence interval in each years, and trends of neonatal morality was described with line regression. Cox proportional regression model was used to assess predictors and presented with an adjusted hazard ratio (AHR) and 95% CI. Results. The estimated cumulative average of neonatal mortality rate in this study was 20.3 (95% CI: 18.9-21.8) per 1000 live births. The rate was decline with regression coefficient β = −1.60. Risk of neonatal death was found to be significantly associated with neonate born to mother living in rural Kersa (AHR = 5.31; 95% CI: 3.07-9.18), born to mother not receiving antenatal care (AHR = 1.43; 95% CI: 1.15-1.78), low birthweight (AHR = 2.59; 95% CI: 2.05-3.27), and preterm newborn (AHR = 12.10; 95% CI: 9.23-15.86). Conclusion. Neonatal mortality in the study site is far from reaching the national and global target goals.
Keywords: Ethiopia, Kersa HDSS, neonatal mortality
Introduction
The neonatal mortality rate (NMR) defined as the probability of dying before 28 days per 1000 live births remains a serious global public health concern.1,2 Surviving and thriving of newborn is essential to ending extreme poverty, promoting development and resilience, and achieving Sustainable Development Goals (SDGs).3,4 The first days of birth and the first 28 days of life are the most vulnerable time for a child’s survival and health.2,5
Globally 2.4 million neonate died in 2019 with an average of 6700 deaths per a day. 6 Neonatal mortality rates (NMRs) vary significantly between countries; a huge toll of death is attributed to low income countries. About 80% of neonatal death was contributed by both south Asia and sub-Saharan Africa. The current (2017-2019) estimated neonatal mortality rate was 17 (with 95% CI: 17, 19) in the world, 27.2 in sub-Saharan Africa, 26.4 in low income countries, whereas 7 in upper middle income countries, and 3 in high income countries. The annual NMR in low income countries was 8.8 times higher than the average NMR in high income countries.6-8 Thus, a newborn’s chances of surviving and thriving largely depend on where they are born. 4
Three fourth of neonatal deaths can be prevented by effective interventions delivered along the continuum of care during pre-pregnancy, antenatal, intrapartum, delivery, postpartum, and postnatal periods for mothers and their newborns. 7 Some newborn died because the care they received was of poor quality; others because they received no health care at all. 4 Focusing on improving coverage, quality and equity of obstetric care during labor and childbirth, and care for small and sick newborns accelerate the rate of neonatal mortality reduction.9,10 Providing effective care to all women and babies at the time of birth in facilities could prevent an estimated 113 000 maternal deaths, 531 000 stillbirths, and 1.3 million neonatal deaths annually by 2020.3,11 Maternal health care utilization in Ethiopia is very low which exhibited by only 43% of pregnant women visited ANC 4 and more times, and less than half (48%) of women gave birth at health facilities in 2019. 12 This would exacerbate neonatal mortality in the country.
To realize the neonatal health targets set in the Health Sector Transformation Plan (HSTP) (reducing neonatal mortality from 33 per 1000 live birth to 21 per 1000 live birth by 2025), 13 and the Sustainable Development Goals (SDGs) (reduce neonatal mortality to 12 per 1000 live birth by 2030), 14 Ethiopia has implemented a set of various interventions. These include National Newborn and Child Survival Strategy, Integrated Management of Neonatal and Childhood Illnesses (IMNCI), Neonatal Intensive Care Units (NICU), Kangaroo Mother Care (KMC), strengthening the immunization program, and other high impact interventions.13,15-17 Health extension program has played a great role to reach agrarian, pastoralist and semi pastoralist community, through community base intervention like integrated community-based case management of childhood illnesses (ICCM), and Community-Based Newborn Care (CBNC). 18
With this all efforts, under 5 and infant mortality was significantly reduced from 2005 to 2019. However, the neonatal mortality rate was stagnated between 39 and 30 from 2005 to 2019.12,18 It lags behind the global rate of 18 neonatal death per 1000 livebirth.7,8 With this slow progress of neonatal mortality reduction (NMR), the sustainable development goal would not be met in Ethiopia.
The predictors of neonatal mortality are multiple and represent a complex interaction with sociodemographic, healthcare, and biological variables. 19 These includes family wealth, residence, maternal age, maternal educational status, utilization of obstetrics care, sex of child, gestational age, birth weight, place of delivery, and ANC follow up.20-28
Reliable estimates of numbers, and predictors to newborn deaths are critical for evidence based priority setting and programming. In Ethiopia where civil registration and vital statistics is poorly practice, data related to neonatal mortality and live birth were obtained from household survey or from facility data. The house hold survey suffer with recall bias since the participants were asked about the events that happened 5 years or more preceding the survey.1,12,29 And the study also shares the restrictions of cross-sectional studies and poorly estimate mortality rates and trends. Since majority of neonatal death happens at community level, the facility data do not show the true features of neonatal mortality estimate and do not help to extrapolate the result to other sites. Both methods have their own limitation and unable to indicate the true estimate of neonatal mortality. There is a dearth of research in Ethiopia on the estimate and trends of NMR, and its predictors through pregnancy observation on an open cohort of all individuals permanently living in specific geographical boundary. This is therefore, we aimed to estimate NMR incidence in each year, predict the trends in 12 years, and determine factors associated with NMR. The information obtained from this longitudinal data will inform programmer to track the change to sustainable development goal and to take an action on time to accelerate the reduction per annum.
Methods and Materials
Study Setting and Period
Kersa Health Demographic Surveillance System (HDSS) field site is located in Kersa district in East Hararghe zone. Kersa HDSS was established in 2007, starting with an initial census in 12 kebeles (small administrative unit in Ethiopia) to define the baseline denominator population; the initial census did not contain vital events (birth and death). 30 Thereafter, the HDSS includes continuous longitudinal recordings of demographic data to monitor the population at regular intervals, observing relevant changes that occur in the designated population. HDSS field site was extended to Harari region (Harar town) in 2012 and operates among 6 kebeles. In 2015 each HDSS site (Kersa and Harar town) expanded their coverage and doubled the number of kebeles being monitored. Currently, the HDSS covers 36 kebeles (24 kebeles from Kersa districts, and 12 kebeles from Harar town) which includes 41 056 households and a total population of 197 268. 31
Study Design and Population
Kersa HDSS is an intensive longitudinal data collection linked through time. It is an open dynamic cohort study design that longitudinally follows individuals living within a specific geographical boundary. All individuals who are living in Kersa HDSS has visited every 6 months. During each visit, reproductive age (15-49 years) women from the households are interviewed about their pregnancy, and their birth outcome. Birth outcome was categorized as live birth, still birth, and abortion and miscarriage. Child born alive has followed for other event like death. Those new born who died within 28 days we considered as neonatal death.
Exclusion Criteria
Children with missing information (date of birth, date of death) were excluded from the study.
Sample Size and Sampling Techniques
All events (live birth and neonatal death) occurred from January 1, 2008 through December 30, 2019 were included in this study.
Data Collection Procedure
Data were collected by well-trained regular HDSS staffs through face to face interview using tablet computer with Open Data Kit (ODK) collect application. Supervisors were assigned to supervise data collectors in the field. Field supervisors checked data quality before it was sent to the database system. If supervisors found a data quality problem, it sent back to data collectors for correction. Collected data using a tablet computer in the field was temporarily stored on ODK aggregate. The data manager approved the quality of data and migrated data from temporary storage to the final storage OpenHDS database system.
Researchers extracted 12 years (January 1, 2008-December 30, 2019) data from Kersa HDSS database system. Events which happened between January 1, 2008 and December 30, 2019 were recorded from March 2008 through February 2020. Live birth and neonatal death were retrieved by years, and neonatal mortality rate was calculated by dividing neonatal death per 1000 live births for each year. During the period, a total of 39 369 pregnancy outcome was observed, of which 38 541 were live birth (Figure 1).
Figure 1.
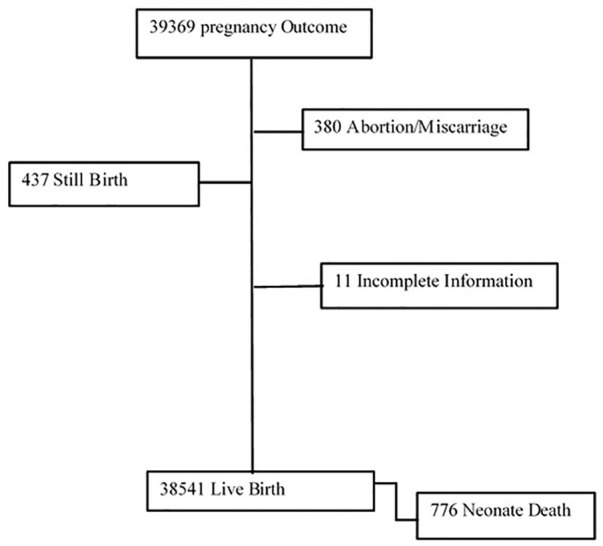
Pregnancy outcome in Kersa HDSS from 2008 to 2019, eastern Ethiopia.
All independent variables were linked to the neonate through location and individual identifiers. Personal identifiers were removed from extracted data.
Measurement and Variables
Women who gave birth during the data collection period were interviewed about the outcome of their pregnancy. Pregnancy outcomes include live birth, still birth, or miscarriage; during each visit data collectors collected information on any deaths of household members and if a death was reported, detailed information regarding the age of the deceased, date of death, sex, perceived cause of death, and place of death was registered. Neonatal mortality rate, the outcome of this study, was calculated as a child death during the first 28 days of life divided by 1000 live births in the same year. The outcome variable was categorized as “death” and “live.” Death was assigned a “1,” and live (censored) was a “0.” Socio-demographic factors (place of residence, education status of mother), maternal factors (age at first child birth), and obstetrics factors (parity, place of delivery, ANC visit), neonatal factors (birth size, term of delivery, and child sex) were considered as explanatory variables for neonatal mortality.
Operational Definition
Time to events: It is the period from starting of observation (birth) until the occurrence of event (death).
Death: In this study, death referred to the study subject who had experienced the interest of event (had died) during the observation period.
Censored: In this study, censored is referred to the study subject who had not experienced death during the follow-up period.
Neonatal death: An infant death within the first 28 days of life reported by the mother participating in the study.
Neonatal survival is defined as being alive up to the end of follow-up period (28 days).
Term pregnancy is a pregnancy between 37 completed weeks gestation to 42 completed weeks of gestation.
Neonate size at birth is defined as the size of the newborn at birth according to the perception of the mother. For this study, the mother’s perception of the newborns size is defined as small being equivalent to less than 2500 g, normal(average) 2500 to 4000 g, and large greater than 4000 g. This estimate was obtained because birth weight is unknown for most newborns in Ethiopia.
Mother educational status was categorized as “literate” if she attended any formal school, and had literacy and numeracy skills; if she has no formal education but can read and write, she was labeled as “can read and write”; if the mother was not able to read nor write she was labeled as “neither read nor write.”
Parity refers to the number of children born to the women; if she gave birth to only 1 child she was categorized as “prim parous” and if she gave birth to more than 1 child, she was labeled as “multipara.”
Age at first childbirth: If the women gave birth to her first child at 20 years old or less, it was categorized as “≤20 years” otherwise labeled as “>20 years.”
Place of delivery: The place where the child is born; if the child is born at a health center, health post, or hospital, then it is labeled as “deliver at health facility,” if the women gave birth at home, it was labeled as “deliver at home.”
Ante natal care (ANC): If the pregnant women attended the ANC unit during her pregnancy at least once, researchers categorized it as “Yes” otherwise “No.”
Place of Residence: A place where individuals live; individuals living in Harar City were labeled as “urban,” those living in the small town in Kersa were labeled as “semi urban” and those living in Kersa rural area were labeled as “rural.”
Ethical Clearance
Kersa HDSS has obtained ethical clearance from national ethical review committee and from Haramaya University College of health and medical science and institutional health research ethical review committee (IHRERC).
Data Management and Statistical Analysis
STATA version 14 (StataCorp 2015, College Station, TX) statistical software was utilized for data analysis. Before analysis, data were cleaned and edited. Neonatal mortality rate was calculated by neonatal death per 1000 live births. Neonatal mortality rate was described in each year with 95% CI. Kaplan–Meier survival curve was used to show patterns of neonatal death in 28 days, and log rank test was used to compare the survival curves among independent variables.
Independent and adjusted relationships of different predictors with neonatal mortality were assessed with Cox proportional regression model. The assumption of cox proportional regression model was assessed using graphic techniques, goodness of fit, and time dependent variables. Bi-variable Cox regression model was fitted for each explanatory variable. Explanatory variable at bivariate analysis with a P-value less than .2 were included to the subsequent model building. The Hazard Ratio (HR) and 95% Confidence Intervals (95% CI) were calculated for each variable. In the final Cox proportional regression model, the HR was adjusted for all the selected variables within that level and the variables of farther levels as follows. Model-I was built to examine the association of socio-demographic characteristics (maternal education and residence) with neonatal mortality. Subsequently, reproductive and maternal health variables (Parity, Receive Antenatal care, Place of delivery, Age at first child birth) were included in Model-II to assess their relationship with neonatal mortality when controlling for socio-demographic variables. Model-III was fitted to examine association of neonate related variable (birth weight, gestational age, and sex of newborn) when controlling for sociodemographic and maternal health variables retained in model 2 with neonatal mortality
The results were reported in an adjusted Hazard ratio (AHR) with 95% confidence interval. Multi-collinearity was assessed using variance inflation factors (VIF). We exclude gravida from the model for it has collinearity with parity (VIF = 10.41). In the multivariable analysis, variables having P-value <.05 were considered as significant predictors of mortality.
Result
Characteristics of Study Participants
The sex ratio of neonates in this study was 111 males per 100 females, with the majority 30 135 (78.21%) of neonates from rural Kersa. About two-thirds (24 598) of mothers were unable to read or write. The majority 25 195 (65.39 of births took place at home). Eighty percent of the mothers had their first birth at 20 years of age (Table 1). The mean age and standard deviation of mother was (28 ± 7.2).
Table 1.
Socio Demographic, Maternal, and Obstetrics Characteristics of Study Participants at Kersa HDSS from 2008 to 2019.
| Freq. | Percent | |
|---|---|---|
| Sex of neonate (n = 38 541) | ||
| Female | 18 265 | 47.39 |
| Male | 20 276 | 52.61 |
| Residence (n = 38 529) | ||
| Harar | 5659 | 14.69 |
| Kersa rural | 30 135 | 78.21 |
| Kersa semi urban | 2735 | 7.10 |
| Maternal education (n = 38 376) | ||
| Literate | 13 064 | 34.04 |
| Read and write | 714 | 1.86 |
| Neither read nor write | 24 598 | 64.10 |
| Mothers occupation (n = 38 415) | ||
| Housewife | 31 085 | 80.92 |
| Unemployed | 4408 | 11.47 |
| Paid employee | 1159 | 3.02 |
| Merchant | 1081 | 2.81 |
| Daily Laborer | 682 | 1.78 |
| Gravida (n = 38 410) | ||
| Primi gravid | 7604 | 19.80 |
| Multi gravida | 30 806 | 80.20 |
| Ante natal care follow up (n = 27 101) | ||
| Yes | 12 336 | 45.52 |
| No | 14 765 | 54.48 |
| Parity (n = 36 844) | ||
| Primi para | 6559 | 17.80 |
| Multi para | 30 285 | 82.20 |
| Place of delivery (n = 38 529) | ||
| At home | 25 195 | 65.39 |
| At health facility | 13 334 | 34.61 |
| Duration of pregnancy (n = 38 514) | ||
| Term | 27 912 | 72.47 |
| Pre-term | 524 | 1.36 |
| Post term | 10 078 | 26.17 |
| Birth weight (n = 26 847) | ||
| Small | 2384 | 8.88 |
| Normal | 21 294 | 79.32 |
| Big | 3169 | 11.80 |
| Age at 1st child birth (n = 38 443) | ||
| 20 and below | 30 860 | 80.27 |
| Above 20 | 7583 | 19.73 |
Neonatal Mortality Rate and Trends
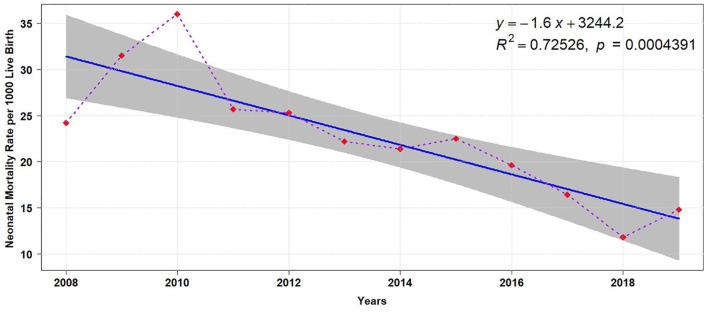
Among 39 369 pregnancy followed between 2008 and 2019, 480 of them were ended with miscarriage/abortion, 437were stillborn, and 11 of them had incomplete information. Finally, we get 38, 541 live births of which 776 died within 28 days (Figure 1). The cumulative average of neonatal mortality rate in this study was 20.3 (95% CI: 18.9-21.8) per 1000 live birth. The highest neonatal mortality rate 36.0 (95% CI: 28.7-45.1) per 1000 was registered in 2010 and the lowest 11.8 (95% CI: 9.2-15.1) was observed in 2018 (Table 2). The overall regression model showed a significant decline in neonatal mortality rate with regression coefficient β = −1.60, P = 000 (Figure 2).
Table 2.
Twelve Years’ Neonatal Mortality Rate Per 1000 Live Births in Kersa HDSS, Eastern Ethiopia.
| Years | Live birth | Neonatal death | Neonatal mortality rate per 1000 live birth with 95% CI |
|---|---|---|---|
| 2008 | 1568 | 39 | 24.2 (17.7-32.9) |
| 2009 | 1714 | 56 | 31.5 (24.3-40.7) |
| 2010 | 1927 | 72 | 36.0 (28.7-45.1) |
| 2011 | 1585 | 41 | 25.7 (19.0-34.7) |
| 2012 | 1888 | 49 | 25.3 (19.2-33.3) |
| 2013 | 2840 | 66 | 22. 3 (17.6-28.3) |
| 2014 | 2776 | 60 | 21.4 (16.6-27.5) |
| 2015 | 3721 | 87 | 22.5 (18.3-27.7) |
| 2016 | 4791 | 94 | 19.6 (16.0-23.9) |
| 2017 | 5284 | 88 | 16.4 (13.3-20.2) |
| 2018 | 5320 | 63 | 11. 8 (9.2-15.1) |
| 2019 | 4077 | 61 | 14.8 (11.5-18.9) |
| Overall mortality rate | 37 495 | 776 | 20.3 (18.9-21.8) |
Figure 2.
Trends of neonatal mortality rate per 1000 live birth at Kersa HDSS, from 2008 to 2019.
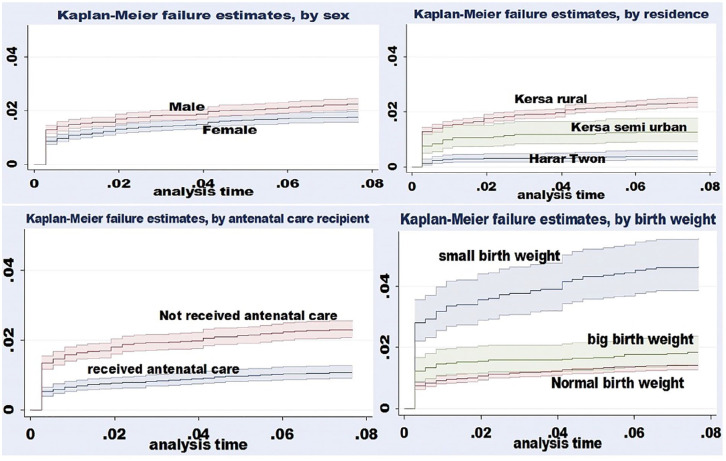
Kaplan-Meier failure estimate function curve showed variation of death probability among variables (baby’s sex, baby’s birthweight, mother’s receiving ANC, and place of residence). The probability of death is higher among neonates residing in rural Kersa, neonates whose mother received no ANC, male infants, and low birthweight infants. Log rank test showed statistical difference among ANC recipients (x2 = 60.24; P < .000), sex of infant (x2 = 11.06; P < .0016), place of residence (x2 = 100.98; P < .000), and infants birthweight (x2 = 130.42; P < .00) (Figure 3).
Figure 3.
Kaplan-Meier failure estimate function curve with 95% CI by sex, baby’s birth weight, ante natal recipient, and place of residence.
Predictors of Neonatal Mortality
Using the bivariate cox regression model, 9 variables (mother’s educational status, place of residence, parity, recipient of ANC, age at first child birth, place of delivery, baby’s birthweight, term of pregnancy, and baby’s sex) were tested to predict neonatal mortality. In multivariable cox regression model, place of residence, recipient of ANC, parity, baby’s birthweight, and term of pregnancy were maintaining their significant association with neonatal mortality. The risk of NM among neonates residing in rural Kersa was 5.31 time higher compared to neonates residing in Harar town (AHR = 5.31; 95% CI: 3.07-9.18). The risk of neonatal mortality among neonate residing in Kersa semi urban was 2.5 times higher as compared to neonate residing in Harar town (AHR = 2.52; 95% CI: 1.28-4.98). The risk of neonatal mortality rate was 60% higher among neonate born to primiparous mothers compared to neonate born to multiparous mother (AHR = 1.61; 95% CI; 1.30-1.98). The risk of NM among neonates born to mothers with no ANC was 45% higher than those with ANC (AHR = 1.43; 95% CI; 1.15-1.78). Likewise, low birthweight babies had 2.59 times higher risk of neonatal mortality compared with normal birthweight neonates (AHR = 2.59; 95% CI: 2.05-3.27) (AHR = 2.59; 95% CI: 2.0-3.2). Moreover, large birth weight babies were 2 times more likely to die (AHR = 2.29; 95% CI: 1.70-3.08) compared to babies with normal birth weight. Pre-term neonate were 12 times more likely to die as compared to term neonate (ARH = 12.10; 95% CI: 9.23-15.86) (Table 3).
Table 3.
Cox Proportional Hazard Regression to Predict Neonatal Mortality in Kersa HDSS from 2008 to 2019.
| Variable | Neonatal mortality |
Model 0 |
Model I |
Model II |
Model III |
|
|---|---|---|---|---|---|---|
| Censored | Death | Cured hazard ratio | Adjusted Hazard ratio | Adjusted Hazard ratio | Adjusted Hazard ratio | |
| Maternal education | ||||||
| Literate | 12 878 (98.58) | 186 (1.42) | 1.00 | 1.00 | 1.00 | 1.000 |
| Read and write | 698 (97.76) | 16 (2.24) | 1.57 (0.94-2.62) | 1.10 (0.66-1.84) | 1.30 (0.70-2.42) | 1.42 (0.76-2.64) |
| Neither read nor write | 24 036 (97.72) | 562 (2.28) | 1.60 (1.36-1.89) | 1.06 (0.89-1.27) | 1.24 (1.12-1.55) | 1.18 (0.94-1.47) |
| Residence | ||||||
| Harar town | 5637 (99.61) | 22 (0.39) | 1.00 | 1.00 | 1.00 | 1.000 |
| Kersa rural | 29 428 (97.65) | 707 (2.35) | 6.07 (3.97-9.28) | 5.78 (3.72-8.97) | 4.53 (2.63-7.79) | 5.31 (3.07-9.18)* |
| Kersa semi urban | 2700 (98.72) | 35 (1.28) | 3.30 (1.93-5.63) | 3.22 (1.89-5.51) | 2.32 (1.18-4.57) | 2.52 (1.28-4.98)* |
| Parity | ||||||
| Prim para | 6400 (97.58) | 159 (2.42) | 1.37 (1.15-1.64) | 1.64 (1.33-2.02) | 1.61 (1.30-1.98)* | |
| Multi para | 29 751 (98.24) | 534 (1.76) | 1.00 | 1.00 | 1.00 | |
| Receive antenatal care | ||||||
| Yes | 12 204 (98.93) | 132 (1.07) | 1.00 | 1.00 | 1.00 | |
| No | 14 424 (97.69) | 341 (2.31) | 2.16 (1.77-2.65) | 1.62 (1.30-2.02) | 1.43 (1.15-1.78)* | |
| Place of delivery | ||||||
| At home | 24 647 (97.82) | 548 (2.18) | 1.34 (1.14-1.57) | 0.72 (0.58-0.88) | NA | |
| At health facility | 13 118 (98.38) | 216 (1.62) | 1.00 | 1.00 | NA | |
| Age at 1st child birth | ||||||
| 20 and below | 30 193 (97.84) | 667 (2.16) | 1.73 (1.39-2.14) | 1.19 (0.91-1.56) | 1.21 (0.92-1.59) | |
| Above 20 | 7488 (98.75) | 95 (1.25) | 1.00 | 1.000 | 1.00 | |
| Birth weight | ||||||
| Small | 2273 (95.34) | 111 (4.66) | 3.29 (2.65-4.10) | 2.59 (2.05-3.27)* | ||
| Normal | 20 990 (98.57) | 304 (1.43) | 1.00 | 1.00 | ||
| Large | 3111 (98.17) | 58 (1.83) | 1.28 (0.97-1.70) | 2.29 (1.70-3.08)* | ||
| Sex of neonate | ||||||
| Female | 17 943 (98.24) | 322 (1.76) | 1.000 | 1.00 | ||
| Male | 19 822 (97.76) | 454 (2.24) | 1.27 (1.10-1.46) | 1.19 (0.98-1.43) | ||
| Duration of pregnancy | ||||||
| Term | 27 484 (98.47) | 428 (1.53) | 1.00 | 1.00 | ||
| Pre-term | 404 (77.10) | 120 (22.90) | 16.34 (13.35-20.02) | 12.10 (9.23-15.86)* | ||
| Post term | 9862 (97.86) | 216 (2.14) | 1.40 (1.18-1.64) | 0.95(0.69-1.32) | ||
Abbreviation: NA = not applicable. The first color indicate “sociodemographic” variable under model “1”;The second color indicate “reproductive health variable” under model “2”; The 3rd color indicate “Child related Variable” under model “3”.
Significantly associated with P < .05.
Discussion
Despite numerous innovations and interventions made to improve the survival of newborns, NM remains a serious global public health concern, notably in LMICs.32,33 Neonatal mortality rate remains unacceptably high in Ethiopia. Neonatal mortality rate reduction is not promising to reach the goal of sustainable development; the neonatal mortality rate was reported to be 29 per 1000 live births as of EDHS 2016 and was targeted to reduce to 10 per 1000 live births in 2019/20, however the 2019 neonatal mortality rate was increased to be 30 per 1000 live birth.34,35
In this study, the cumulative average neonatal mortality rate over the 12-year period was 20.3 (95% CI: 18.9-21.8) per 1000 live births. The current neonatal mortality rate in Kersa HDSS is high; it is 2 times higher than the national goal of reducing the neonatal mortality rate to 11 per 1000 live births by 2020 36 and the global goal of 12 per 1000 live births by 2030. 37 This finding is supported with cross sectional study conducted in Ethiopia. 29 However, the neonatal mortality rate in this study was found to be lower than the national estimate of 30 per 1000 live births. 34 According to a community based cross-sectional study done in Ethiopia, neonatal mortality rate ranges from 24.5 to 44 per 1000 live births.30,38 Reported neonatal mortality from other low-income countries ranges from 25 to 34 per 1000 live births. 39 Variations in neonatal mortality reports may emanate from different types of research and study participants. Even though the Ethiopian government has formulated and implemented several strategies 36 for child survival and safe motherhood, the change in NM is far behind the intended goal. This reflects the quality of care and acceptance of the care at the community level. Since the majority of births take place at home in Ethiopia, 34 they do not receive essential newborn care which is found mainly in the health facilities. Institutional deliveries have improved coverage of the essential newborn care as well as obstetric interventions. 39 A study from the same setting showed only 1 in 4 newborns receive essential newborn care. This is a cue for policymakers and decision making to rethink current policies and programs to better reach the targeted population and maximize neonatal survival.
Neonate born to a family living in rural and semi-urban areas, neonates who born to a primiparous mother and mothers who did not receive ANC were more likely to die as compared to their counter parts; small birthweight, large birth weight, and preterm delivery were significantly associated with neonatal mortality.
Living in rural and semi-urban areas are known risk factors for neonatal mortality. The death hazard is highest among neonates whose families lived in rural and semi-urban areas compared to neonates whose families were lived in urban areas. The difference in mortality indicators between urban and rural underscore the effect of socioeconomic differences and variances in access to health services and medical technology. Geographic isolation, socioeconomic disadvantage, and lack/shortage of healthcare services/providers are likely explanations for this difference. These, coupled with factors such as the cost of care, distance barrier to facilities, and traditional beliefs/practices, may contribute to a higher incidence of neonatal mortality in rural residences. 20
The risk of death was higher among neonates born to mothers who did not receive ANC. This result is in agreement with other similar studies.21,35,40 Neonatal mortality (NM) is particularly sensitive to the lifestyles of the mother during the prenatal period and the care given to mothers and their babies. 41 Neonate survival can be improved by expanding care during the antenatal period. 42 ANC may help to reinforce maternal education and compliance and provide an opportunity for screening for warning signs of pregnancy complications, treatment of infections, and early management of newborn illness. Promoting and strengthening ANC follow-up benefits the wellbeing of the neonate, rather than maternal health. Thus, ANC follow-up is a vital tool for neonatal survival.28,39 However, in this study more than 55% of the women did not receive a single maternal care visit during pregnancy, indicating that this critical service is severely under-utilized in the area.
The death hazard was higher among preterm birth and small birth size (a proxy for low birthweight) neonate. This finding was in agreement with other studies in Ethiopia.19,38-40 Low birthweight and preterm babies were less likely to survive as compared to normal weight neonates and term baby neonates. This is because preterm and low birthweight neonates are more likely to develop various complications during and after delivery. Preterm neonates may be born with immature lungs which result in hypoxia that may lead to death.19,43,44 Low birthweight (LBW) predisposes newborns to increased risk of infections, low blood sugar, and low body temperatures, which increases the risk of death compared to normal size newborns. 45 A large proportion of neonatal deaths can be prevented by effective intervention delivered along the continuum of care during pre-pregnancy antenatal, intrapartum, delivery, postpartum, and postnatal periods for mother and their newborns. Prematurity and low birthweight can be primarily addressed through interventions related to antenatal care, and deliveries occurring in well-equipped facilities with high-quality care.7,46
The risk of dying is higher among neonates born to prim parous mothers; in Ethiopia, 10% of women gave birth during their adolescence, 47 this study revealed 60% of the women gave birth to their first child during this same period . Evidence shows that adolescent mothers are more likely to have babies that are low birthweight or born prematurely,48,49 both of which are essential causes or contributing factors to newborn mortality. Further studies suggest having children at such a young age is associated with physiological and anatomical immaturity which leads to prolonged labor, reduced blood supply to the uterus and cervix which may increase the risk of infection; there is also evidence that adolescents have reduced placental transportation of oxygen. 49
Strengths and Limitation of the Study
The strength of this study includes data was collected for 12 consecutive years which allows for calculation of trends and cumulative NMR; furthermore, information was collected biannually and respondents were not subjected to recall bias for the outcome variable. Thus, the findings provide a reasonable estimate of the neonatal mortality and can be generalized to a large segment of neonate in Ethiopia. The explanatory variables used in this study are not exhaustive because the data is not aimed to collect predictors. Some critical independent variables, such as early initiation of breastfeeding, KMC Kangaroo Mother care, covering the head of the child, and delaying bath, are not included. 50 A proxy measure was used for birthweight which may lead to misclassification of the baby’s weight. Moreover, some women were unsure of their last menstrual period and therefore it was difficult to determine the gestational age. So, the term of pregnancy is also liable to misclassification.
Conclusion
The current neonatal mortality rate in study area continues to be high; the observed trends of neonatal mortality reduction from 2008 to 2019 in this study still did not reach SGD goals. 37 Ethiopia failed to achieve the past and current goals36,51 to reduce neonatal mortality. Modifiable risk factors like ANC under-utilization, low birthweight, and preterm deliveries are attributed to a high level of mortality rate. These factors are preventable if quality-focused antenatal and intrapartum care are provided. Identification of pregnancy complications and facilitation of proper method of delivery is vital to improve the quality of care. Thus, devising practical strategies to reach expectant women through continuum of care that contribute to averting neonatal mortality rate is essential in combating this major public health crisis. We recommend further studies which incorporate some of the variables that are not addressed in this study such as breast feeding, culture of child feeding, birth interval, maternal nutrition, and vaccination. It is also very important if the mixed study design is applied.
Acknowledgments
We would like to thank all individual in Kersa HDSS for responding to mortality survey. We gratefully acknowledge all data collectors, supervisors, and data clerks for their contribution.
Footnotes
Author Contributions: MD and GD contributed equally to this work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Merga Dheresa  https://orcid.org/0000-0003-3404-2682
https://orcid.org/0000-0003-3404-2682
References
- 1. WHO. The Neonatal Mortality Rate (NMR) is Defined as the Probability of Dying before 28 Days per 1000 Live Births. WHO; 2013. [Google Scholar]
- 2. Binns C, Low WY. Neonatal public health: progress and challenges. Asia Pac J Public Health. 2015;27:688-689. [DOI] [PubMed] [Google Scholar]
- 3. United Nations. The Global Strategy for Women’s, Children’s and Adolescents’ Health (2016-2030). United Nations; 2015. [Google Scholar]
- 4. WHO. SURVIVE and THRIVE Transforming Care for Every Small and Sick Newborn. WHO; 2018. [Google Scholar]
- 5. WHO/UNICEF. Reaching the Every Newborn national 2020 milestones country progress, plans and moving forward. 2017. Accessed April 29, 2021. https://www.who.int/maternal_child_adolescent/newborns/every-newborn/enap-progress-report2017-summary.pdf?ua=1
- 6. UNICEF. Levels and Trends in Child Mortality. UNICEF; 2020. [Google Scholar]
- 7. Hug L, Alexander M, You D, Alkema L. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Health. 2019;7:e710-e720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. United Nation. Levels Trends in Child Mortality. United Nation; 2019. [Google Scholar]
- 9. Darmstadt GL, Shiffman J, Lawn JE. Advancing the newborn and stillbirth global agenda: priorities for the next decade. Arch Dis Child. 2015;100:S13-S18. [DOI] [PubMed] [Google Scholar]
- 10. WHO/UNICEF. EVERY NEWBORN ACTION PLAN country-progress-tracking-report. WHO/UNICEF; 2015. [Google Scholar]
- 11. WHO. Strategies Toward Ending Preventable Maternal Mortality (EPMM). WHO; 2015. [Google Scholar]
- 12. FMOH. Ethiopia Mini Demographic and Health Survey 2019. FMOH; 2019. [Google Scholar]
- 13. FMOH. Health Sector Transformation Plan II (HSTP II) 2020/21-2024/25. FMOH; 2021. [Google Scholar]
- 14. United Nation. Transforming our World: The 2030 Agenda for Sustainable Development. United Nation; 2015. [Google Scholar]
- 15. FMOH. Essential Health Services Package of Ethiopia. FMOH; 2019. [Google Scholar]
- 16. FMOH. National Strategy for Newborn and Child Survival in Ethiopia (2015/16-2019/20). FMOH; 2015. [Google Scholar]
- 17. FMOH. Comprehensive Multi- Comprehensive Multi-Year Plan 2016-2020. FMOH; 2015. [Google Scholar]
- 18. FMOH. Annual performance report 2012 EFY (2019/2020). FMOH; 2021. [Google Scholar]
- 19. de Souza S, Duim E, Nampo FK. Determinants of neonatal mortality in the largest international border of Brazil: a case-control study. BMC Public Health. 2019;19:1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Adewuyi EO, Zhao Y. Determinants of neonatal mortality in rural and urban Nigeria: evidence from a population-based national survey. Pediatr Inte. 2017;59:190-200. [DOI] [PubMed] [Google Scholar]
- 21. Roy S, Haque MA. Effect of antenatal care and social well-being on early neonatal mortality in Bangladesh. BMC Pregnancy Childbirth. 2018;18:485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aghai ZH, Goudar SS, Patel A, et al. Gender variations in neonatal and early infant mortality in India and Pakistan: a secondary analysis from the Global Network Maternal Newborn Health Registry. Reprod Health. 2020;17:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tesema GA, Worku MG. Individual-and community-level determinants of neonatal mortality in the emerging regions of Ethiopia: a multilevel mixed-effect analysis. BMC Pregnancy Childbirth. 2021;21:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dhaded SM, Somannavar MS, Moore JL, et al. Neonatal deaths in rural Karnataka, India 2014-2018: a prospective population-based observational study in a low-resource setting. Reprod Health. 2020;17:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sidi-Yakhlef A, Boukhelif M, Aouar Metri A. Socio-demographic determinants of neonatal mortality in Algeria according to MICS4 data (2012-2013). Afr Health Sci. 2021;21:357-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Victora CG, Barros AJD. Socioeconomic inequalities in neonatal mortality are falling: but why? Lancet Global Health. 2014;2:e122-e123. [DOI] [PubMed] [Google Scholar]
- 27. Doku DT, Neupane S. Survival analysis of the association between antenatal care attendance and neonatal mortality in 57 low- and middle-income countries. Int J Epidemiol. 2017;46:1668-1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Arunda M, Emmelin A, Asamoah BO. Effectiveness of antenatal care services in reducing neonatal mortality in Kenya: analysis of national survey data. Glob Health Action. 2017;10:1328796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mitiku HD. Neonatal mortality and associated factors in Ethiopia: a cross-sectional population-based study. BMC Womens Health. 2021;21:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Assefa N, Lakew Y, Belay B, et al. Neonatal mortality and causes of death in Kersa Health and Demographic Surveillance System (Kersa HDSS), Ethiopia, 2008-2013. Mater Health Neonatol Perinatol. 2016;2:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Assefa N, Oljira L, Baraki N, et al. HDSS profile: the Kersa health and demographic surveillance system. Int J Epidemiol. 2016;45:94-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ministry of Health. National Adolescent and Youth Health Strategy (2016-2020). Ministry of Health; 2016. [Google Scholar]
- 33. Nakimuli A, Mbalinda SN, Nabirye RC, et al. Still births, neonatal deaths and neonatal near miss cases attributable to severe obstetric complications: a prospective cohort study in two referral hospitals in Uganda. BMC Pediatr. 2015;15:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. EPHI. Ethiopia Mini Demographic and Health Survey: Key Indicators. Rockville, Maryland, USA: EPHI and ICF. EPHI; 2019. [Google Scholar]
- 35. Alebel A, Wagnew F, Petrucka P, et al. Neonatal mortality in the neonatal intensive care unit of Debre Markos referral hospital, Northwest Ethiopia: a prospective cohort study. BMC Pediatr. 2020;20:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ministry of Health. National Strategy for Newborn and Child Survival in Ethiopia. Ministry of Health; 2015. [Google Scholar]
- 37. United Nations Children’s Fund. Levels & Trends in Child Mortality. United Nations Children’s Fund; 2019. [Google Scholar]
- 38. Debelew GT, Afework MF, Yalew AW. Determinants and causes of neonatal mortality in Jimma Zone, Southwest Ethiopia: a multilevel analysis of prospective follow up study. PLoS One. 2014;9:e107184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dhaded DM, Somannavar MS, Vernekar SS, et al. Neonatal mortality and coverage of essential newborn interventions 2010-2013: a prospective, population-based study from low-middle income countries. Reprod Health. 2015;12:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wolde HF, Gonete KA, Akalu TY, Baraki AG, Lakew AM. Factors affecting neonatal mortality in the general population: evidence from the 2016 Ethiopian Demographic and Health Survey (EDHS)—multilevel analysis. BMC Res Notes. 2019;12:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dallolio L, Lenzi J, Fantini MP. Temporal and geographical trends in infant, neonatal and post-neonatal mortality in Italy between 1991 and 2009. Ital J Pediatr. 2013;39:1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Roy S, Haque MA. Effect of antenatal care and social well being on early neonatal mortality in Bangladesh. BMC Pregnancy Childbirth. 2018;18:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bayih WA, Assefa N, Dheresa M, Minuye B, Demis S. Neonatal hypothermia and associated factors within six hours of delivery in eastern part of Ethiopia: a cross-sectional study. BMC Pediatr. 2019;19:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Griffin JB, McClure EM, Kamath-Rayne BD, et al. Interventions to reduce neonatal mortality: a mathematical model to evaluate impact of interventions in sub-Saharan Africa. Acta Paediatr. 2017;106:1286-1295. [DOI] [PubMed] [Google Scholar]
- 45. Kananura RM, Tetui M, Mutebi A, et al. The neonatal mortality and its determinants in rural communities of Eastern Uganda. Reprod Health. 2016;13:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Singh K, Brodish P, Haney E. Postnatal care by provider type and neonatal death in sub-Saharan Africa: a multilevel analysis. BMC Public Health. 2014;14:941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Central Statistical Agency. Demographic and Health Survey Addis Ababa. Central Statistical Agency; 2017. [Google Scholar]
- 48. Gibbs CM, Wendt A, Peters S, Hogue CJ. The impact of early age at first childbirth on maternal and infant health. Paediatr Perinat Epidemiol. 2012;26:259-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Neal S, Channon AA, Chintsanya J. The impact of young maternal age at birth on neonatal mortality: evidence from 45 low and middle income countries. PLoS One. 2018;13:e0195731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Safari K, Saeed AA, Hasan SS, Moghaddam-Banaem L. The effect of mother and newborn early skin-to-skin contact on initiation of breastfeeding, newborn temperature and duration of third stage of labor. Int Breastfeeding J. 2018;13:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Assefa Y, Van Damme W, Williams OD, Hill PS. Successes and challenges of the millennium development goals in Ethiopia: lessons for the sustainable development goals. BMJ Glob Health. 2017;2:e000318. [DOI] [PMC free article] [PubMed] [Google Scholar]