Abstract
Hypothermia defined as a core body temperature less than 35°C causes hundreds of deaths annually in the United States. It can occur in a variety of clinical settings, including environmental exposure, shock, infection, metabolic disorders, alcohol, or drug toxicity, and malnutrition. This condition can affect many different organ systems and may lead to serious complications including cardiac arrhythmia. Hypothermia is extremely rare in people living with HIV but can be seen in severely malnourished patients or those who are not receiving antiretroviral therapy (ART). It is a life-threatening situation that should be treated aggressively. To the best of our knowledge, there are only a few cases that have been reported for people living with HIV presenting with hypothermia and sinus bradycardia. Herein, we are reporting a very rare case of people living with AIDS who presented with hypothermia complicated by sinus bradycardia. In addition, we also performed a systematic review of cases based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses guideline, to investigate the clinical characteristics and outcomes associated with this rare complication. This systematic review of cases hopefully can increase the awareness of this rare entity and help improve its outcome.
Keywords: Transient hypothermia, HIV/AIDS, bradycardia, malnutrition, literature review
Introduction
Hypothermia occurs when the core body temperature drops to less than 35°C, and can be subdivided into mild (32°–35°C), moderate (28°–32°C), and severe (<28°C) categories. 1 Owing to the lack of robust evidence to support the various treatment options, the management of hypothermia can be challenging. 2 There are no exact numbers for the incidence and prevalence of hypothermia, but it is noted in the death certificate in around 1500 adults in the United States every year. 1 Although hypothermia is more commonly seen in patients who are exposed to a cold environment, it can also occur in a variety of clinical settings, including shock, infection, metabolic disorders (such as hypothyroidism, adrenal insufficiency, and Wernicke encephalopathy), alcohol, or drug toxicity, and malnutrition. 1 Hypothermia typically resolves with treatment of the underlying disorder. 3 It affects all body organs, but consequences of the cardiovascular system are the most serious because they can lead to complications including lethal arrhythmias such as ventricular fibrillation. 4
AIDS in humans is caused by two lentiviruses, human immunodeficiency virus types 1 and 2 (HIV-1 and HIV-2). 5 Per the global statistics, in 2019, there were approximately 38 million people across the globe with HIV/AIDS. 6 There are only a few cases described in the literature so far for people living with HIV (PLWH) presenting with hypothermia.7–12 The uncontrolled HIV/AIDS seems to be the major contributing factor in hypothermia presentation in PLWH.
Herein, we are reporting a rare presentation of hypothermia associated with sinus bradycardia and Osborn’s wave on electrocardiograph (EKG) in an AIDS patient, likely secondary to severe malnutrition and severe immunosuppression. In addition, we also performed a systematic review of cases based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline, with the aim to investigate the clinical characteristics and outcomes associated with this complication.
Case presentation
A 65-year-old gentleman with past medical history of chronic kidney disease, HIV-1 infection diagnosed 4 years before his admission and opioid use disorder admitted for a witnessed loss of consciousness. On arrival to the emergency department, he was unresponsive, with pinpoint pupils. He became more awake and alert after the administration of Naloxone. His initial vitals showed a blood pressure 124/82 mm Hg, heart rate 88 beats/min, temperature 98.6°F (37.0°C), respiratory rate 12 breaths/min, and saturating 99% on room air. He also has a body mass index (BMI) of 16.9 kg/m2. On physical examination, he was cachectic; the rest of his examination was unremarkable. His initial CD4 count was 6 cells/mL (359–1519 cells/mL), CD4 3% and an HIV viral load was 175,410 copies/mL (reference: undetectable). He was noncompliant and stopped his antiretroviral therapy (ART) 6 months before admission. His kidney function was normal with creatinine 0.7 mg/dL (06–1.2 mg/dL), and the estimated glomerular filtration rate was >60 mL/min/1.73 m2.
Computerized tomography (CT) of the brain without contrast showed chronic findings of remote right frontal infarct with stable chronic ventriculomegaly; however, no acute intracranial findings with no significant change from the CT that was done before 4 years. The white blood cell count was 3.4 × 103/L (4.4–11.0 × 103/L), hemoglobin was 11.6 g/dL (13.5–17.5 g/dl), mean corpuscular volume (MCV) was 83 fL (81.2–95.1 fL), platelet count was 20 × 109/L (150–450 × 103), and albumin level was 1.5 g/dL (3.6–5.1 g/dL). Peripheral blood smear was normal without any evidence of platelet clumping. The urine drug screen was positive to opiates.
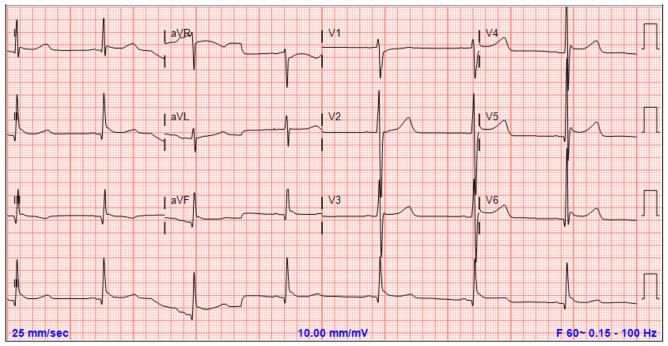
On day 2 of the hospital stay, he became hypothermic with a rectal temperature of 68.2°F (20.1°C). Telemetry showed sinus bradycardia with a heart rate of 30–40 beats/min and a blood pressure of 90/56 mmHg. His EKG is as shown in Figure 1. He was conscious and oriented but very lethargic. His morning cortisol level was 25 µg/dL (2.0–25 µg/dL) on the upper range of normal. His thyroid function tests (TSH, FT4, FT3) were normal, and glucose levels were also within normal limits. Insulin-like growth factor-1 (IGF-1) levels were significantly decreased 29 ng/mL (49–188 ng/mL). A purified protein derivative test was negative, and immunologic studies such as ANA, c-ANCA, p-ANCA, antidouble-stranded DNA, and rheumatoid factor were all negative. Septic workup was also found to be negative at this time. Active external rewarming, with a combination of warm blankets and heating pads was done in addition to active internal rewarming with intravenous (IV) administration of warmed normal saline at (40°C–42°C). He was started on Bictegravir/Emtricitabine/Tenofovir alafenamide, and atovaquone for Pneumocystis jiroveci prophylaxis. On day 3 of admission, the patient clinically improved and his rectal temperature improved to 98.7°F (37.1°C). He was started on nasogastric tube feeds with careful monitoring for signs of re-feeding syndrome. The feeding was later changed to oral feeding with protein supplements over the next day. On day 5, he was discharged home in a stable condition.
Figure 1.
EKG showing evidence of sinus bradycardia and J waves or (Osborn wave).
Discussion
A systematic review of the literature was performed using the PRISMA guidelines, 13 to extract all cases of hypothermia associated with HIV infections. A literature search was conducted in databases such as PubMed and Google Scholar from 1995 to 2020. Search item included the keywords of “Human immunodeficiency virus AND hypothermia,” “Human immunodeficiency virus AND hypothermia AND bradycardia,” “ HIV AND hypothermia,” “HIV AND hypothermia AND bradycardia,” “Acquired immunodeficiency syndrome AND hypothermia,” “Acquired immunodeficiency syndrome AND hypothermia AND bradycardia,” “AIDS AND hypothermia,” and “AIDS AND hypothermia AND bradycardia.” All study designs included case reports and case series were eligible for final analysis. We excluded guidelines that (1) were not published in English and (2) articles published before 1995.
Full text of the articles was obtained and assessed for eligibility by two independent reviewers. Any discrepancies were resolved through discussion to reach a consensus in the presence of the third reviewer. A PRISMA flowchart of study selection is shown in Figure 2.
Figure 2.
PRISMA flowchart of study selection.
For each eligible study, demographic data were extracted including number of patients, age, sex, ethnicities, and clinical characteristics (medical history, medications, presenting symptoms and CD4 counts, HIV viral load, septic workups, and clinical outcome). We also included the EKG findings. The data were tabulated, and outcomes were cumulatively analyzed.
Six studies were included in the final analysis, with a total of eight patients (including the one we presented here). The detailed demographic, clinical characteristics and outcome are shown in Table 1. The average age was 45.63 years old (range 21–65). There was a male preponderance with six males and two females.
Table 1.
Detailed demographic, clinical characteristics, and outcome.
| Study | Age | Gender | Ethnicity | Temperature ( F) | Prior hypothermic | Bradycardia | Hypotension | CD4 count | HIV viral load | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Simpson et al. 7 | 38 | Male | Blacks | Too low to record | No | Yes (38 bpm) | Yes (79) | 38 | 1,030,000 | Complete recovery |
| Choi and McNeal 8 | 49 | Male | Blacks | 91 | No | No | No | 265–>125 | 4,900,000 –>9000000 | Complete recovery |
| Okechukwu and Pesanti 9 | 48 | Male | Unknown | 94.5 | No | No | No | 624 | Unknown | Frequency and intensity of attacks reduced after clonidine |
| Okechukwu and Pesanti 9 | 48 | Male | Unknown | 95.4 | No | No (87) | No (133/88) | <10 | Unknown | Frequency and intensity of attacks reduced after clonidine |
| Moulignier et al. 10 | 47 | Male | Blacks | 83.1 | Yes (21 times) | No | No (210/140) | 480 | 115,000 | Complete recovery |
| Rerolle et al. 11 | 21 | Female | Unknown | 89.6 | No | Yes | Yes (90/50) | 371 | 800,000 | Complete recovery |
| Malhotra et al. 12 | 49 | Female | Unknown | 89.5 | No | No | No | Unknown | Unknown | Complete recovery |
The average temperature on admission was 30.7 C, with one of the studies having a temperature too low to document. Uncontrolled HIV with CD4 counts <500 cell/mL and high viral loads were observed in six of the patients (one of the case reports had no documented CD4 count and viral loads). Almost all patients had good clinical outcome with complete recovery. There were only two patients that still presented with frequent hypothermia attacks, which was reduced with the use of clonidine.
After reviewing the literature, most of the reported cases had a low CD4 cell count with an average of 265 cell/mL with high viral load. There are a few different hypotheses and elements that may explain how HIV can cause hypothermia. One of these assumptions is malnutrition. Malnutrition itself is a well-known cause of hypothermia and at the same time is common in HIV-infected patients. Four of the reported cases including our patient were cachectic and had low body mass index before their presentation. HIV can cause immune impairment which leads to malnutrition and further immune deficiency allowing for the rapid progression of HIV infection to AIDS. 14 Also, patients with HIV infection frequently experience loss of appetite. This may be due to sores in the mouth, an acute illness, or because HIV infection itself can cause a loss of appetite. Opportunistic infections such as candida, cytomegalovirus (CMV), and others can affect the mouth and the esophagus and may also play a role in malnutrition. Other factors that may contribute to a patient’s malnutrition include the neuropsychiatric effects of HIV and socioeconomic factors. 15
It is important to conduct a full endocrine workup for PLWH who are presenting with hypothermia. HIV can affect the neuroendocrine pathways leading to hormone axis’s disturbances. In all the cases that we reviewed, a full endocrine workup was done. In two cases, there were hormone disturbances noted. One of these hormones is the growth hormone and the insulin-like growth factor-1 axis (GH/IGF-1), which was severely reduced in two cases. IGF-1 is a very sensitive indicator of nutritional status. Different nutritional deficiencies including calories, proteins, and specific micronutrients such as zinc can cause a reversible reduction in the IGF-1 concentrations. 16
Another hypothesis that may explain the hypothermia presentation is the disruption in the circadian rhythmicity of several functions, including body temperature that HIV can cause. Huitron-Resendiz et al. 17 conducted a study on monkeys infected with simian immunodeficiency virus (SIV) and reported progressive pathological alterations in the circadian rhythms of body temperature and gross locomotor activity in SIV-infected monkeys. Moulignier et al. 10 describes another possible theory for hypothermia in HIV patients, which is the neurodegenerative effects of the virus in the central nervous system that may affect the thermoregulatory centers. Besides, it has been reported that HIV patients who develop AIDS have a reduced number of vasopressin- and oxytocin-expressing neurons in the suprachiasmatic nucleus and paraventricular nucleus, respectively, indicating that hypothalamic neurons are compromised during the progression of the HIV disease. 18
The main treatment for hypothermia is treating the underlying cause. All the reported cases were started on HIV treatment, six of them improved significantly after the initiation of the medications with viral load decreasing and CD4 count increasing. Two cases still had episodes of hypothermia after the treatment and their symptoms were improved with clonidine. Clonidine is an alpha-agonist vasodilator that can abort the hypothermia symptoms including the vasoconstriction and the shivering response. 19 In addition, rewarming plays a crucial role in patient management. Rewarming techniques include passive external rewarming, active external rewarming, active internal rewarming, or a combination of these methods. 20 Active external rewarming, like heated air or warm water immersion, is necessary for moderate to severe hypothermia. Some severe cases may require invasive methods ranging from airway rewarming with humidified air to full cardiopulmonary bypass including warm fluid infusion, Pleural and peritoneal lavages with warm fluids, extracorporeal rewarming methods, and others. 21
Herein, we are reporting a case of a gentleman with uncontrolled HIV who presented with hypothermia associated with sinus bradycardia. This condition was most likely secondary to severe malnutrition which was confirmed by a significant decrease in the IGF-1 levels, and a very high viral load with severe immunosuppression likely causing an additive effect. He was initially started on active external and internal warming along with the introduction of the highly active antiretroviral therapy (HAART) and oral feeds leading to a significant improvement in his body temperature and normalization of his heart rate.
Conclusion
Hypothermia is a very rare presentation in HIV patients. Uncontrolled disease with low CD4 cell count and high viral load is the main risk factor for hypothermia in PLWH. The treatment relies mainly on the initiation of HAART and good nutrition in addition to the passive and active warming. The aim of this case report and literature review is to increase awareness about this entity in PLWH.
Footnotes
Author contributions: I.F., K.H.C., and H.A. contributed to the conception and design, acquisition, analysis, and interpretation of data, as well as participated in drafting and revision of the article. T.D., B.V., and A.R. actively participated in analysis of data and drafting and revision of article. A.S. and J.S. contributed to idea design and data analysis, critically revised the article, as well as approved the final submission of the article.
Availability of data and materials: Data have been presented in the text.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Consent for publication: The patient has given written informed consent to publish the case including publication of images.
ORCID iD: Kok Hoe Chan  https://orcid.org/0000-0002-2550-1122
https://orcid.org/0000-0002-2550-1122
References
- 1. Gelb D. Hypothermia. In: Aminoff MJ, Daroff RB. (eds) Encyclopedia of the neurological sciences. Cambridge, MA: Elsevier Inc., 2014, pp. 657–658. [Google Scholar]
- 2. Weinberg AD. Hypothermia. Ann Emerg Med 1993; 22(2 Part 2): 370–377. [DOI] [PubMed] [Google Scholar]
- 3. Blondin NA. Diagnosis and management of periodic hypothermia. Neurol Clin Pract 2014; 4(1): 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Osborn JJ. Experimental hypothermia; respiratory and blood pH changes in relation to cardiac function. Am J Physiol 1953; 175(3): 389–398. [DOI] [PubMed] [Google Scholar]
- 5. Seitz R. Human immunodeficiency virus (HIV). Transfus Med Hemother 2016; 43(3): 203–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. HIV.gov. Global statistics, https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics (accessed 14 October 2020).
- 7. Simpson SJ, Ratnappuli A, Porte ME, et al. Hypothermia—an unusual initial presentation of human immunodeficiency virus infection. Int J STD AIDS 2020; 31(12): 1219–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Choi CH, McNeal T. Transient hypothermia in HIV-1 with insulin-like growth factor-1 deficiency and severe protein calorie malnutrition. Proc (Bayl Univ Med Cent) 2015; 28(1): 29–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Okechukwu CN, Pesanti E. Episodic spontaneous hyperhidrosis hypothermia in human immunodeficiency virus-positive patients. Clin Infect Dis 1999; 29: 210. [DOI] [PubMed] [Google Scholar]
- 10. Moulignier A, Guiard-Schmid JB, Gbadoe AH, et al. HIV-1-related spontaneous episodic hypothermia. Neurology 2003; 61(3): 418–419. [DOI] [PubMed] [Google Scholar]
- 11. Rerolle JP, Canaud G, Fakhouri F, et al. Thrombotic microangiopathy and hypothermia in an HIV-positive patient: importance of cytomegalovirus infection. Scand J Infect Dis 2004; 36(3): 234–237. [DOI] [PubMed] [Google Scholar]
- 12. Malhotra I, Shenoy MA, Shankar S, et al. Persistent hypothermia and non-convulsive seizures in human immunodeficiency (HIV) virus positive patient. Am J Respir Crit Care Med 2017; 195: A5582. [Google Scholar]
- 13. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6(7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Duggal S, Chugh TD, Duggal AK. HIV and malnutrition: effects on immune system. Clin Dev Immunol 2012; 2012: 784740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Piwoz E, Preble E. HIV/AIDS and nutrition: a review of the literature and recommendations for nutritional care and support in Sub-Saharan Africa, 2000, http://www.sidalc.net/cgi-bin/wxis.exe/?IsisScript=BINCA1.xis&method=post&formato=2&cantidad=1&expresion=mfn=001451 (accessed 14 October 2020).
- 16. Hawkes CP, Grimberg A. Insulin-like growth factor-I is a marker for the nutritional state. Pediatr Endocrinol Rev 2015; 13(2): 499–511. [PMC free article] [PubMed] [Google Scholar]
- 17. Huitron-Resendiz S, Marcondes MCG, Flynn CT, et al. Effects of simian immunodeficiency virus on the circadian rhythms of body temperature and gross locomotor activity. Proc Natl Acad Sci U S A 2007; 104(38): 15138–15143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Purba JS, Hofman MA, Portegies P, et al. Decreased number of oxytocin neurons in the paraventricular nucleus of the human hypothalamus in AIDS. Brain 1993; 116(4): 795–809. [DOI] [PubMed] [Google Scholar]
- 19. Weant KA, Martin JE, Humphries RL, et al. Pharmacologic options for reducing the shivering response to therapeutic hypothermia. Pharmacotherapy 2010; 30(8): 830–841. [DOI] [PubMed] [Google Scholar]
- 20. Lloyd EL. Accidental hypothermia. Resuscitation 1996; 32(2): 111–124. [DOI] [PubMed] [Google Scholar]
- 21. Danzl DF, Pozos RS. Accidental hypothermia. N Engl J Med 1994; 331(26): 1756–1760. [DOI] [PubMed] [Google Scholar]