Abstract
Background:
Exercise is widely regarded to improve pain and function in patients with knee osteoarthritis (OA) through building supportive muscle mass, facilitating weight loss, and through the other beneficial effects associated with it.
Purpose:
To explore literature that presents clinical guidelines for the use of exercise in the treatment of knee OA to inform an evidence-based position statement for the Arthroscopy Association of Canada.
Study Design:
Position statement.
Methods:
PubMed, MEDLINE, Embase, and Cochrane databases were searched for guidelines commenting on the role of exercise for knee OA. The search was limited to guidelines published in the last 10 years. Articles were screened for relevance, focusing on recently published research with clinical guidelines. Inclusion criteria involved all articles providing clinical guidelines for exercise and knee OA.
Results:
Eight guidelines were identified. All eight recommended exercise as an important component of treatment for knee OA, with 6/8 strongly recommending it.
Conclusion:
Exercise is an effective and important component of the non-pharmacological management of knee OA. The Arthroscopy Association of Canada strongly recommends the use of exercise in the management of knee OA.
Keywords: knee, osteoarthritis, exercise, strengthening, joint loading, inflammation
Background
Osteoarthritis (OA) is one of the most common chronic medical disorders worldwide. 26 Its prevalence is increasing globally and is associated with an aging population as well as increases in risk factors such as obesity and a sedentary lifestyle. 26 In Canada, OA is an unfortunately common chronic condition, affecting more than 10% of the population according to official Canadian estimates. 6 The productivity cost from loss of work associated with OA is rising and is estimated in a recent study to cost the Canadian economy $17.5 billion annually by 2031. 31 OA can occur in many joints, however the knee in particular is one of the most commonly affected, associated with 29% of all OA cases in Canadians. 17
Through appropriate treatment, knee OA symptoms can be managed to prevent disability, increase mobility, and reduce pain. 6 Knee OA is multifactorial - a complex interplay of various factors including joint integrity, genetic predisposition, local inflammation, joint loading forces, and cellular and biochemical processes. 19 For most patients, treatment is largely focused on managing symptoms through nonoperative therapies including weight loss, strength training, bracing, anti-inflammatory drugs, and injectable medications or therapies. Total knee joint replacement (arthroplasty) represents the only definitive treatment for end-stage knee OA and there are a few other relatively minor procedures that can be performed. However, these options should generally be pursued after all nonoperative options have been exhausted.
The most common modifiable risk factor for knee OA is obesity, which increases risk through various mechanisms including increased joint loading forces, changing body composition which can increase inflammation, and changing behaviors such as decreased exercise subsequently leading to the loss of protective muscle strength. 19 Biomechanical studies demonstrate that every pound (0.45 kg) of body weight gained adds 2 lbs to 4 lbs (0.9 kg - 1.8 kg) of load across the knee. 19 Studies have also demonstrated that physical activity is lower among patients with OA and it varies depending on the location of the affected joint. 9 Patients with knee OA have an especially lower level of physical activity due to the physical limitations of the legs. 9
There are many reasons why incorporating exercise in treatment plans for patients with knee OA may be beneficial. First, exercise has repeatedly been shown to be associated with multiple health benefits and an overall better quality of life. Lack of physical activity has been shown to worsen maximal function of the heart, peripheral circulation, skeletal muscle strength, bone strength and more 30 . It is not surprising then that OA is among 40 chronic diseases which are associated with a higher incidence and worse progression in people who are physically inactive. 30 Second, certain strengthening exercises can increase the muscle mass of quadriceps, hamstrings, and peripheral muscles surrounding the knee which play a key role in stability. 9 It has been shown that exercise reduces pain, improves quality of life, and improves the physical function of the knee in patients with knee OA. 8 Finally, accompanied by a change in diet, exercise plays a role in weight loss and muscle strengthening which reduces joint load on the knee and may also improve its biomechanical function. When regular exercise is incorporated with a change in diet for weight loss in obese patients, more fat mass is lost and lean skeletal muscle mass is retained leading to improved cardiovascular fitness, strength, and functional capacity of joints required to perform regular daily activities. 22
There is sufficient evidence that suggests exercise is beneficial to incorporate in the treatment of knee OA. This systematic review evaluates the latest clinical guidelines surrounding the use of exercise as a treatment option for patients with knee OA to come to a position statement for the Arthroscopy Association of Canada (AAC).
Methods
This study was conducted using the methods outlined in the Cochrane Handbook for Systematic Reviews of Interventions. 11 The findings are presented according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 23 A single reviewer (SM) searched PubMed, MEDLINE, Embase, and Cochrane databases with the terms “guideline”, “exercise”, “knee”, and “osteoarthritis”, using the “related articles” function. The search was limited to articles published in the last 10 years (Aug 31, 2010 - Aug 28, 2020).
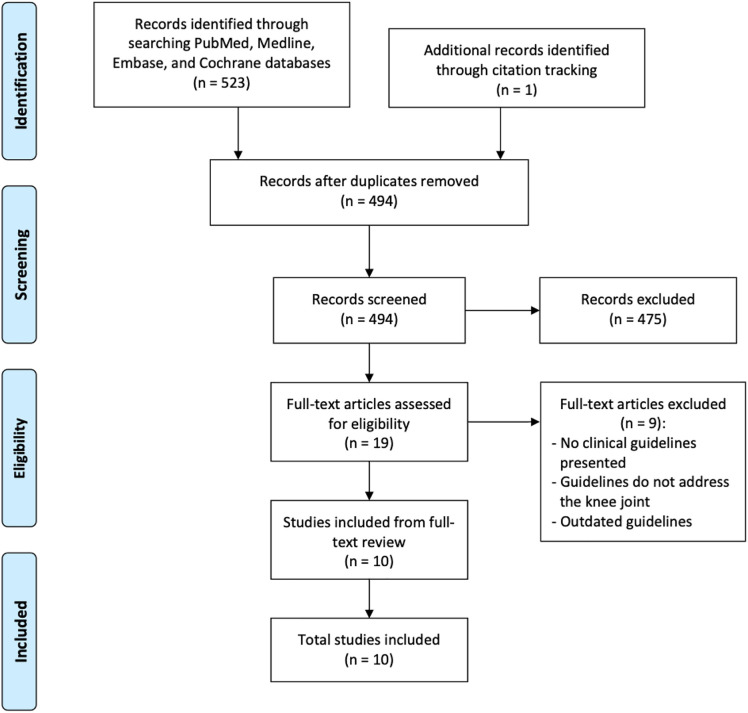
Articles were screened by a single reviewer (SM) for relevance, focusing on recently published research with clinical guidelines including systematic reviews, meta-analyses, and randomized controlled trials. Inclusion criteria involved all clinical articles that provided guidelines for exercise and knee OA. All basic science studies, case series, case reviews, studies reporting on OA in joints other than the knee, and studies with outdated guidelines were excluded (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 23 diagram of article selection.
Results
Clinical Guidelines
From the ten included studies, eight clinical guidelines were found as one of the reporting bodies (Ottawa Panel) published their guideline over a three-part study assessing different categories of exercise. All clinical guidelines recommended that exercise be incorporated into the treatment regimen for knee OA, with six of them strongly recommending it. All of the guidelines recommended general aerobic and strength training exercises. The recommendations for the method of supervision were not unanimous across the guidelines. All papers recommended exercise as beneficial over no exercise. The results of the clinical guidelines have been summarized in Table 1.
Table 1.
Current clinical practice guidelines for the treatment of knee osteoarthritis with exercise
| Organization | Guideline | Types of Exercises Recommended | Supervision Recommended | System for Recommendation | Year Published |
|---|---|---|---|---|---|
| OARSI 1 | Exercise is strongly recommended* | Land based aerobic, strength, and mind-body exercises | No recommendation | Strong or conditional recommendation based on consensus from voting panel | 2019 |
| Ottawa 2 , 3 , 4 | Exercise is strongly recommended** | Mind-body, aerobic and strength exercises | Both self-directed and therapist supervised | ABCD grading system based on statistical (P<0.5) and clinical (>15% improvement) significance and consensus from voting panel | 2017 |
| ESCEO 5 | Exercise is strongly recommended | Aerobic, strength and resistance exercises | No recommendation | Strong or weak recommendation based on consensus from voting panel | 2019 |
| ACR 18 | Exercise is strongly recommended | Aerobic, strength, aquatic and resistance exercises based on patient preferences | Both self-directed and therapist supervised | Strong or conditional recommendation based on ratings from voting panel of various health professionals and patients | 2019 |
| AAOS 21 | Exercise is recommended | Low-impact aerobic and strength exercises | Both self-directed and therapist supervised | Appropriate, may be appropriate, or rarely appropriate recommendations based on ratings from voting panel of multi-disciplinary specialist physicians separate from editorial and review teams | 2013 |
| NICE 25 | Exercise is recommended | Aerobic and strength exercises | No recommendation | Recommendations drafted by UK Department of Health and stakeholders collaborating with NICE and are reviewed and updated with scientific evidence | 2014 |
| EULAR 28 | Exercise is strongly recommended | Aerobic and strength exercises | Both self-directed and therapist supervised | ABCD grading system based on consensus from voting panel | 2018 |
| TLAR 33 | Exercise is strongly recommended | Aerobic and strength exercises | No recommendation | 0-10 scale rating based on consensus from voting panel | 2017 |
Note: OARSI = Osteoarthritis Research Society International, Ottawa = The Ottawa Panel, ESCEO = The European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases, ACR = American College of Rheumatology/Arthritis, AAOS = American Academy of Orthopaedic Surgeons, NICE = National Institute for Health and Care Excellence, EULAR = European League Against Rheumatism, TLAR = Turkish League Against Rheumatism
* OARSI in general had a strong recommendation for general land-based and mind-body exercises, however aquatic exercises and exercises incorporated in cognitive behaviour therapy were given conditional recommendations due to considerations for comorbidities and the financial situation of patient.
** Ottawa evaluated multiple specific exercise programs and published across three papers. They graded each exercise program individually. They strongly recommended 12 different exercise programs, however 46 exercise programs in total were evaluated
Types of Exercise
General categories of exercises that were recommended have been summarized in Table 1. From all the guideline bodies, only the Ottawa Panel further investigated specific exercise programs for the management of knee OA. The Ottawa Panel included 46 studies on specific exercise programs from which 35 received at least one positive recommendation and were reported. 2 There were 12 programs that received a strong recommendation which included one mind-body program (out of four evaluated), eight strength training programs (out of 26 evaluated), and three aerobic and strength combination programs (out of five evaluated). 2,3,4 The mind-body program is a Tai Chi program recommended for pain relief and improved physical function. 2 The eight strength training programs use a variety of different strategies to strengthen leg muscles and are recommended for pain relief, improved physical function, and improved quality of life. 3 The three combination programs combine aerobic exercises and strength training and are recommended for improved quality of life, pain relief, and improved physical function. 4 The details for all the strongly recommended exercise programs by the Ottawa Panel have been summarized in Table 2. While all of the programs evaluated and recommended by the Ottawa Panel are of a fixed-length, they acknowledge that to receive long-lasting benefits in the management of knee OA therapeutic exercise needs to be continued indefinitely. 3
Table 2.
Summary of exercise programs strongly recommended by the Ottawa Panel
| Exercise Type | Exercise Program | Details of Program | Results* | Recommended for |
|---|---|---|---|---|
| Mind-Body | Sun Style Tai Chi 32 | 20 weeks, 3 sessions/week (20-40 min). Program consists of Sun style tai chi led by certified instructor in a group. |
n=24, 100% participation. WOMAC pain (0-20) avg -2.60, WOMAC physical function (0-68) avg -6.82 No adverse events |
Pain relief, improved physical function |
| Strength Training | Supervised isokinetic, isotonic, and isometric muscle strengthening program 12 | 8 weeks, 3 sessions/week. Program consists of hot packs and stretching, warm-up on stationary bike, then 5 sets 5 reps of one of following strengthening exercises for hamstrings and quadriceps:
After 8 weeks, at-home program was provided |
n=132, 86.4% participation. VAS pain (0-10) avg -2.1, LI physical function (0-24) avg -2.9 Adverse events: 8 people withdrawn due to knee pain |
Pain relief, improved physical function |
| Progressive exercise program 13 | 6 weeks, 2 sessions/week (45 min). In group or individually. Integrate exercise, education, self-management, and coping strategies. Program consists of warm-up and individualized progressive strengthening, balance and motor control exercises devised and supervised by physiotherapist. |
n=418, 82% participation. WOMAC physical function (0-68) avg -5.6 Adverse events: 5 people withdrawn due to knee pain |
Improved physical function | |
| High (HR) and low (LR) resistance strengthening program 15 | 8 weeks, 3 session/week 10% (low resistance: LR) and 60% (high resistance HR) of 1-repetition maximum (RM) leg training for quadriceps. Program consists of warm-up on stationary bike, low intensity (15 reps, 10 sets) or high intensity (8 reps, 3 sets) leg press exercise, and cold packs after. Supervised by therapist |
n=102, 93% participation. WOMAC pain (0-20) avg LR -3, avg HR -3.7, WOMAC physical function (0-68) avg LR -11.3, avg HR -11.7 Adverse events: 3 people withdrawn due to knee pain |
Pain relief, improved physical function | |
| Non-weight (NWB) or weight bearing (WB) exercise program 14 | 8 weeks, 3 sessions/week WB or progressive NWB strength training. Program consists of warm-up on stationary bike, 6 reps, 4 sets WB (one foot leg press) or NWB (one foot leg extension 50% RM + 5% every 2 weeks) for each knee, and cold pack after. Supervised by therapist |
n=106, 92% participation. WOMAC physical function (0-68) avg WB -10.3, avg NWB – 17.2 Adverse events: 5 people withdrawn due to knee pain |
Improved physical function | |
| Quadriceps strengthening program 16 | 24 months, 2 times/day At-home program mostly self-supervised. Program consists of progressive exercises beginning with non-resistant flexibility exercises up to month 2, then continuing with graded therapeutic elastic band strengthening exercises targeting the quadriceps and functional strengthening exercises (e.g. rising from sitting position) twice daily. |
n=389, 74% participation. WOMAC pain (0-20) avg Exercise groups -1.78 with 44% of participants achieving >30% pain reduction. (Dietary intervention groups also evaluated but no effects on pain), 45% self-reported high compliance to exercise program No adverse events |
Pain relief | |
| Home-based physiotherapist supervised quadriceps strengthening program 20 | 12 weeks, 5 sessions/week Home-based partially supervised (physiotherapist interventions usually 1x/week). Program consists of 5 quadriceps exercises that use ankle weights and therapeutic elastic bands (ankle weight knee extension while sitting, ankle weight knee extension supine, ankle weight full leg extension, ankle weight isometric knee extension sitting, TheraBand knee extension sitting). Exercise dosage determined and adjusted by physiotherapist as comfortable for patients. |
n=107, 91% participation. WOMAC pain (0-100) avg neutrally aligned -13, avg maligned -4.6 (Study evaluated patients with maligned vs neutrally aligned knee joints), 87% compliance based on exercise journal completion Adverse events: 2 people withdrawn due to knee pain 1 person withdrawn due to neck pain |
Pain relief | |
| Lower extremity strengthening program 24 | 6 months, 1 time/day Home-based partially supervised (Therapist interventions at beginning, after 2 weeks, 6 weeks, and 3 months). Program consists of 5 quadriceps exercises (isometric quadriceps contraction, isotonic quadriceps contraction, isotonic hamstrings contraction, isotonic quadriceps contraction with TheraBand, stair step up and down). Exercises are progressively increased to a max of 20 reps each. |
n=191, 94% participation. HADS anxiety (0-21) avg -0.57, HADS depression (0-21) avg -0.57. No adverse events |
Improved quality of life | |
| Mechanical diagnosis and therapy (MDT) program 29 | 2 weeks, 10 reps/2-3 hrs Home-based, partially supervised. Program consists of exercises targeting quadriceps, either modified leg flexion or extension (if patient has directional preference of joint) or regular strengthening exercises like stationary biking (if patient doesn’t have directional preference of joint). Mackenzie MDT certified physiotherapists taught and monitored through 2-3 interventions. |
n=180, 69% participation. P4 pain (0-40) avg -2, KOOS pain (0-100) +7, KOOS physical function (0-100) +5, compliance not measured Adverse events: people withdrawn due to knee pain |
Pain relief, improved physical function | |
| Aerobic + Strength Combination | Individual or group aerobic and strengthening program 7 | 8 weeks, 2 sessions/week (1 hr) Individual or group supervised. Program consists of stretching (quadriceps, hamstring, gastrocnemius), stationary bike 20 mins, NWB leg extensions 20-40 reps, WB resistance climber 100 steps, NWB eccentric and concentric quadriceps exercises 20-40 reps, WB eccentric controlled step down. Home exercise program also provided which was stretches and 20 mins walking/biking. |
n=126, 85% participation. WOMAC pain reversed (100-0) avg +10.6 No adverse events |
Pain relief |
| Community physiotherapy exercise program 10 | 10 weeks, 3-6 sessions (20 mins) Program consists of individualised aerobic and strengthening exercise program and advice leaflet about activity and pacing delivered and supervised by physiotherapist. Exercises are progressively increased in intensity. |
n=325, 54% participation. WOMAC pain (0-20) avg -1.56, WOMAC physical function (0-68) avg -4.79 No adverse events |
Pain relief, improved physical function | |
| Aerobic and strengthening exercise and OA educational program 27 | 3 months, 3 sessions/week (1 hr) Program consists of stretching, aerobic exercises (brisk walking, medium intensity), and strengthening exercises (starting with isometric, going to isotonic with increasing reps and intensity, using thera band). Exercises are progressively increased in intensity and supervised by therapist. |
n=137, 91% participation. AIMS2 pain (0-10) avg -1.44 AIMS2 physical function (0-10) avg -1.5 Compliance avg 86% Adverse events: 1 person withdrawn due to knee pain |
Pain relief, improved physical function |
Note: WOMAC = Western Ontario and McMaster universities osteoarthritis index, VAS = Visual and analogue scale of pain, LI = Lequesne index, HADS = Hospital anxiety and depression Scale, P4 = 4 item pain measure (pain in morning, afternoon, evening, and with activity), KOOS = Knee injury and OA outcome score, AIMS2 = Arthritis impact measurement scale 2
* n is total number of participants in all study groups including control, participation calculated as percentage of people who participated until end of study including follow-up, only outcome values relevant to recommendations shown, all outcome values are averages and are at least P<0.05, 95% CI, adverse events are people who left/were stopped from study due to excessive pain or other effects related to study interventions.
Mind-body exercises were explored by the Ottawa Panel as they can have beneficial effects on both physical and psychological health. From the four programs evaluated, one was strongly recommended which is a 20 week Sun style Tai Chi program with three 20-40 min sessions per week. 2 It was noted that regularity of exercise may have a greater positive effect on pain relief in patients with knee OA than quantity, as the same Sun style Tai Chi in a 12-week, one 60 min session a week program only showed neutral results. 2 This mind-body program was recommended for pain relief and improved physical function and may also help to reduce stress, anxiety, depression, and increase self-esteem among patients with knee OA. 2
Strength exercises were also explored by the Ottawa Panel as they can have beneficial effects on joint stability by improving joint function and reducing loading forces and direct stress on the joint. From the 26 programs evaluated, eight were strongly recommended which are an eight-week supervised isokinetic/isotonic/isometric exercise program with three sessions a week, a six-week progressive exercise program with two 45 min sessions a week, an eight-week high or low resistance strengthening exercise program with three sessions a week, an eight-week non-weight or weight bearing exercise program with three sessions a week, a 24-month quadriceps strengthening program with two sessions daily, a 12-week home-based physiotherapist supervised quadriceps strengthening program with 5 sessions per week, a six-month lower extremity strengthening program with one session a day, and a two-week mechanical diagnosis and therapy program with 10 repetitions every two to three hours. 3 It was noted that muscle strengthening exercises are recommended with or without other therapeutic types of exercises as being an effective non-pharmacological intervention for managing knee OA. 3 There are a variety of different ways strength training can be incorporated and these exercises were recommended for pain relief, improved physical function, and improved quality of life among patients with knee OA. 3
Aerobic exercises were evaluated as well by the Ottawa Panel for their potential to improve cardiopulmonary function and overall quality of life. From the five programs they evaluated, three were strongly recommended which were an eight-week individual or group aerobic and strengthening program with two one-hour sessions a week, a 10-week community physiotherapy exercise program with three to six 20 min physiotherapist intervention sessions over the 10 weeks, and a three-month aerobic and strength exercise and osteoarthritis educational program with three one-hour sessions a week. 4 It was noted that the aerobic exercises evaluated were in combination programs with strength training and that presently, no recommendations of aerobic-only exercise programs could be made. 4 These aerobic and strength combination programs may be beneficial for pain relief, improved physical function, and improved quality of life among patients with knee OA.
Supervision
General supervision recommendations have been summarized in Table 1. From all the studies included, only EULAR and ACR further investigated the outcomes of interventions by various healthcare professionals on exercise treatment for knee OA. EULAR gave a total of 10 recommendations out of which the two strongest recommendations were to incorporate general self-directed physical activity (PA) in treatment plans and for healthcare providers (HCPs) to plan and deliver PA activity interventions that include behavioral and self-monitoring techniques (e.g. physician provides an OA information and basic exercise program pamphlet to patient and follows-up with patient). 28 The rest of the eight recommendations were given a weaker strength due primarily to a lack of quality evidence to support them. 28 Briefly, these recommendations are that all HCPs should promote PA, PA interventions should be delivered by appropriate HCPs, PA level of patients should be routinely evaluated, general and disease specific contraindications should be considered, PA should be personalised to patient goals, general and disease specific barriers should be addressed, PA should be adapted (if there are adverse reactions), behavioral changing interventions should be used, and a variety of modes of delivery should be considered. 28
In addition, ACR determined that generally exercise programs are more effective if supervised either by a provider such as a physical therapist or in a class rather than performed individually at home. 18 However, ACR also mentions that exercise should be focused on patient preference and regardless of the mode of delivery exercise is beneficial over no exercise. 18 Finally, if a patient does not find a certain form of exercise acceptable, cannot afford it, or cannot arrange transport to take part in it then it will not be beneficial for them. 18
Discussion
From all eight guidelines evaluated, it is clear that the incorporation of exercise is beneficial in the management of knee OA. While there isn’t enough evidence to support the recommendation of a specific exercise program, there are some findings from the literature that may guide clinical judgement for determining an exercise plan for patients.
From the many exercise programs strongly recommended by the Ottawa panel there were a few key findings. First, regularity of exercise seems to be associated with its beneficial effects. This was the specific variable that gave the 20 week Sun style Tai Chi program that had shorter but more frequent sessions a strong recommendation over the same program delivered over 12 weeks with fewer but longer sessions. 2 Second, aerobic exercise should be performed in combination with strengthening exercises as there is insufficient evidence to determine if aerobic only exercise has significant benefit to patients with knee OA. 4 Strength training exercises on the other hand have been shown to be effective regardless of whether they are combined with other exercises or not. 3 Finally, regardless of what exercise program patients follow, the retention of beneficial effects do not last if exercise is stopped. Therefore to retain these benefits long-term, regular exercise needs to be continued indefinitely. 3 All of these elements are useful when creating effective exercise programs for patients.
Another aspect to consider is mode of administration. There is some evidence to suggest that exercises delivered through healthcare providers such as physiotherapists may be more beneficial to patients. 18,28 Several factors may contribute to this including structure, motivation, access to specialized equipment and exercises, supervision to ensure correct form, and individual adjustments for maximal effects. However, there may be barriers related to accessing therapist-supervised exercise, chiefly financial and transport. A few more points to consider when determining both types of exercises and mode of delivery are the frailty of the patient, comorbidities, and risk of injury, especially in patients who are >60 years of age and who are morbidly obese. These factors need to be taken into consideration when determining if supervised exercise programs will be beneficial for patients.
The following general parameters for an effective exercise program can be inferred. First, there should be multiple sessions per week, at least 2-3 sessions/ week as frequency of exercise was observed by the Ottawa panel to be associated with its beneficial effects and almost all their strongly recommended programs had more than 2 sessions/week. 2 Second, the majority of exercises should be strength-training as all eight guideline bodies recommend strength training and the Ottawa Panel could not recommended any aerobic only programs, only as combination with strengthening exercises. 3 The strengthening exercises should be focused on the quadriceps and hamstring muscles as most of the strengthening exercises in programs strongly recommended by the Ottawa Panel target these muscles. 3,4 Third, there should be some aerobic exercise included (likely the warm-up component or a general incorporation). There are many reasons for this but a big one is because all eight guideline bodies also recommended aerobic exercises. Many of the exercise programs strongly recommended by the Ottawa panel also had some aerobic component, commonly warm up on a stationary bike. 3,4 Additionally, many activities patients commonly enjoy (e.g. walking, biking, swimming) are aerobic which ACR notes should be a focus of treatment. 18 Also, EULAR strongly promotes general PA which includes many aerobic exercises. 28 Fourth, the strength exercises should consist of a variety of exercises including isometric, isotonic, WB, NWB, and therapeutic band resistance exercises such as leg extensions, leg press, leg lifts, stair climb, wall sit etc…All of these exercises were commonly used in strongly recommended exercise programs by the Ottawa Panel. 3,4 Fifth, there should be around 5-20 reps and 5-10 sets for strength exercises and a maximum of 50-60% one-repetition maximum (RM) for intense exercises as found in the literature from the strongly recommended exercise programs from the Ottawa panel. 7,12,14,15,24,29 These should be adjusted for total number of exercises, patient tolerance, and intensity of exercise. Finally, exercise programs should be supervised or have some HCP intervention as it has been noted by ACR and EULAR to be more effective and most of the Ottawa Panel programs had some type of HCP supervision. 2,3,4,18,28
While all of these parameters can be deduced, there isn’t sufficient evidence across all eight guideline bodies to make a firm recommendation. As noted by the Ottawa panel, retention of beneficial effects does not last if exercise is stopped and ACR notes the best way to keep patients consistent is to have exercises focused on patient preference. 2,18 A rigid exercise program as described above can usually be sustained for a limited period and provide short-term improvement for symptoms of knee OA, as shown in all exercise programs strongly recommended by the Ottawa Panel. This has its place in immediately improving the patient’s knee pain and function, allowing them to initially pursue a more concrete exercise program. However, focusing on long-term benefits for patients requires an exercise regimen integrated into the patient’s daily life.
In this systematic review all literature available containing clinical guidelines for the use of exercise in treating patients with knee OA was evaluated. Eight clinical guidelines were found which all recommended to incorporate exercise, with 6/8 strongly recommending it. In addition, specific exercises and methods of supervision were explored to find details that may be beneficial for clinical use, and the structure of an ideal exercise program was theorized. From this investigation, there is no conclusive evidence to recommend specific exercises or specific exercise programs beyond a combination of aerobic exercises and strength training targeting quadriceps and hamstring muscles. Exercise interventions should have multiple regularly scheduled sessions every week. The specific exercises should be something that the patient enjoys and can continue long-term to reap continual benefit from. If suitable for the patient, an exercise program that is supervised by a physical therapist or trainer may be beneficial. All of these factors should be discussed with the patient to create the most effective plan for them. The incorporation of any consistent exercise is better than none.
Position Statement
After evaluating all recent guidelines available, the Arthroscopy Association of Canada (AAC) strongly recommends incorporating a combination of aerobic and strength training exercises that work the quadriceps and hamstring muscles at regular intervals that can be continued long-term into treatment regimens for patients with knee OA. Whether self-directed or therapist supervised, exercise implemented alongside with patient education and other non-surgical treatments plays a significant role in managing the symptoms of knee OA. This position statement is endorsed by the Canadian Academy of Sport and Exercise Medicine (CASEM).
Limitations
This review was carried out by a single reviewer. This review assessed papers that presented clinical guidelines regarding exercise and knee OA only. There was no risk of bias analysis performed. There were very few guidelines and a limited number of quality studies especially regarding specific of types of exercise and methods of supervision. Each guideline also used a different method to assign strength to their recommendation.
References
- 1. Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–1589. [DOI] [PubMed] [Google Scholar]
- 2. Brosseau L, Taki J, Desjardins B, et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part one: introduction, and mind-body exercise programs. Clin Rehabil. 2017;31(5):582–595. [DOI] [PubMed] [Google Scholar]
- 3. Brosseau L, Taki J, Desjardins B, et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part two: strengthening exercise programs. Clin Rehabil. 2017;31(5):596–611. [DOI] [PubMed] [Google Scholar]
- 4. Brosseau L, Taki J, Desjardins B, et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part three: aerobic exercise programs. Clin Rehabil. 2017;31(5):612–624. [DOI] [PubMed] [Google Scholar]
- 5. Bruyère O, Honvo G, Veronese N, et al. An updated algorithm recommendation for the management of knee osteoarthritis from the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Semin Arthritis Rheum. 2019;49(3):337–350. [DOI] [PubMed] [Google Scholar]
- 6. Chapter one: Life with arthritis in Canada: a personal and public health challenge — What is arthritis and how common is it? Ottawa: Public Health Agency of Canada. 2010. https://www.canada.ca/en/public-health/services/chronic-diseases/arthritis/life-arthritis-canada-a-personal-public-health-challenge/chapter-one-what-is-arthritis-and-how-common-is-it.html
- 7. Fransen M, Crosbie J, Edmonds J. Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. J Rheumatol. 2001;28(1):156–164. [PubMed] [Google Scholar]
- 8. Fransen M, McConnell S, Harmer AR, et al. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;1: CD004376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gay C, Chabaud A, Guilley E, Coudeyre E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Ann Phys Rehabil Med. 2016;59(3):174–183. [DOI] [PubMed] [Google Scholar]
- 10. Hay EM, Foster NE, Thomas E, et al. Effectiveness of community physiotherapy and enhanced pharmacy review for knee pain in people aged over 55 presenting to primary care: pragmatic randomised trial. BMJ. 2006;333(7576):995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane. July 2019. www.training.cochrane.org/handbook.
- 12. Huang M-H, Lin Y-S, Yang R-C, Lee C-L. A comparison of various therapeutic exercises on the functional status of patients with knee osteoarthritis. Semin Arthritis Rheum. 2003;32(6):398–406. [DOI] [PubMed] [Google Scholar]
- 13. Hurley MV, Walsh NE, Mitchell HL, et al. Clinical effectiveness of a rehabilitation program integrating exercise, self-management, and active coping strategies for chronic knee pain: A cluster randomized trial. Arthritis Rheum. 2007;57(7):1211–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jan M-H, Lin C-H, Lin Y-F, Lin J-J, Lin D-H. Effects of weight-bearing versus nonweight-bearing exercise on function, walking speed, and position sense in participants with knee osteoarthritis: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90(6):897–904. [DOI] [PubMed] [Google Scholar]
- 15. Jan M-H, Lin J-J, Liau J-J, Lin Y-F, Lin D-H. Investigation of clinical effects of high- and low-resistance training for patients with knee osteoarthritis: a randomized controlled trial. Phys Ther. 2008;88(4):427–436. [DOI] [PubMed] [Google Scholar]
- 16. Jenkinson CM, Doherty M, Avery AJ, et al. Effects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trial. BMJ. 2009;339: b3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Khan M, Adili A, Winemaker M, Bhandari M. Management of osteoarthritis of the knee in younger patients. CMAJ. 2018;190(3): E72–E79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res (Hoboken). 2020;72(2):149–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lespasio MJ, Piuzzi NS, Husni ME, Muschler GF, Guarino A, Mont MA. Knee Osteoarthritis: A Primer. Perm J. 2017;21:16–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lim BW, Hinman RS, Wrigley TV, Sharma L, Bennell KL. Does knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? A randomized controlled trial. Arthritis Rheum. 2008;59(7):943–951. [DOI] [PubMed] [Google Scholar]
- 21. Members of the Writing, Review, and Voting Panels of the AUC on the Non-Arthroplasty Treatment of Osteoarthritis of the Knee, Sanders JO, Heggeness MH, Murray J, Pezold R, Donnelly P. The American Academy of Orthopaedic Surgeons appropriate use criteria on the non-arthroplasty treatment of osteoarthritis of the knee. J Bone Joint Surg Am. 2014;96(14):1220–1221. [DOI] [PubMed] [Google Scholar]
- 22. Miller CT, Fraser SF, Levinger I, et al. The effects of exercise training in addition to energy restriction on functional capacities and body composition in obese adults during weight loss: a systematic review. PLoS One. 2013;8(11): e81692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–1012. [DOI] [PubMed] [Google Scholar]
- 24. Oreilly SC, Muir KR, Doherty M. Effectiveness of home exercise on pain and disability from osteoarthritis of the knee: a randomised controlled trial. Ann Rheum Dis. 1999;58(1):15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Osteoarthritis: care and management. National Institute for Health and Care Excellence. February 2014. www.nice.org.uk/guidance/CG177. [PubMed] [Google Scholar]
- 26. Palazzo C, Nguyen C, Lefevre-Colau MM, Rannou F, Poiraudeau S. Risk factors and burden of osteoarthritis. Ann Phys Rehabil Med. 2016;59(3):134–138. [DOI] [PubMed] [Google Scholar]
- 27. Péloquin L, Bravo G, Gauthier P, Lacombe G, Billiard JS. Effects of a cross-training exercise program in persons with osteoarthritis of the knee a randomized controlled trial. J Clin Rheumatol. 1999;5(3):126–136. [DOI] [PubMed] [Google Scholar]
- 28. Rausch Osthoff AK, Niedermann K, Braun J, et al. 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 2018;77(9):1251–1260. [DOI] [PubMed] [Google Scholar]
- 29. Rosedale R, Rastogi R, May S, et al. Efficacy of exercise intervention as determined by the McKenzie System of Mechanical Diagnosis and Therapy for knee osteoarthritis: a randomized controlled trial. J Orthop Sports Phys Ther. 2014;44(3):173–181. [DOI] [PubMed] [Google Scholar]
- 30. Ruegsegger GN, Booth FW. Health Benefits of Exercise. Cold Spring Harb Perspect Med. May 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sharif B, Garner R, Hennessy D, Sanmartin C, Flanagan WM, Marshall DA. Productivity costs of work loss associated with osteoarthritis in Canada from 2010 to 2031. Osteoarthritis Cartilage. 2017;25(2):249–258. [DOI] [PubMed] [Google Scholar]
- 32. Tsai P-F, Chang JY, Beck C, Kuo Y-F, Keefe FJ. A pilot cluster-randomized trial of a 20-week Tai Chi program in elders with cognitive impairment and osteoarthritic knee: effects on pain and other health outcomes. J Pain Symptom Manage. 2013;45(4):660–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tuncer T, Cay FH, Altan L, et al. 2017 update of the Turkish League Against Rheumatism (TLAR) evidence-based recommendations for the management of knee osteoarthritis. Rheumatol Int. 2018;38(8):1315–1331. [DOI] [PubMed] [Google Scholar]