Abstract
Sweden has a population-based mammography screening programme for women aged 40–74. The objective of this study was to examine the association between mammography screening attendance and sociodemographic factors in 15 of Sweden's 21 health care regions. Register-based information was collected on all mammography screening invitations and attendance during 2017 and 2018, and linked to individual-level sociodemographic data from Statistics Sweden. Odds ratios (ORs) and 95% confidence intervals (CIs) for attendance were computed by sociodemographic factor. The study sample included 1.5 million women, aged 40–75, with an overall screening attendance of 81.3%. The lowest odds of attending were found for women living without a partner (OR = 0.52, 95% CI: 0.52–0.53), low-income women (OR = 0.57, 95% CI: 0.56–0.57), and non-Nordic women born in Europe (OR = 0.60, 95% CI: 0.59–0.61). Other groups with lower odds of attending were women whose main source of income was social assistance or benefits (OR = 0.62, 95% CI: 0.62–0.63), those not owning their home (OR = 0.66, 95% CI: 0.66–0.67), and those with low level of education (OR = 0.72, 95% CI: 0.71–0.73). Having multiple of these sociodemographic characteristics further lowered the odds of attending. Although overall mammography screening attendance in Sweden is high, sociodemographic inequalities exist, and efforts should be made to address these. Particular attention should be given to low-income women who live without a partner.
Keywords: Mammography, Breast cancer screening, Women's health, Socioeconomic aspects of health
Highlights
-
•
Mammography screening attendance in Sweden was 81% in 2017–2018.
-
•
Sociodemographic inequalities were found for screening attendance.
-
•
Having multiple low attendance risk factors further decreased the odds of attending.
-
•
Lowest attendance among low-income women who live without a partner.
1. Introduction
European guidelines recommended that women aged 45–74 are screened regularly (i.e. every two to three years depending on age group) in organized mammography screening programmes [1], and most European countries have established national population-based programmes [2]. It is important to understand and address the factors influencing attendance in order to ensure high attendance, which is crucial for the positive effect of these programmes on public health. Furthermore, access to health care services on equal and needs-based terms is at the core of Swedish health care [3].
Nationwide population-based mammography screening has been fully implemented in Sweden since 1997 [4] and includes women aged 40–74 years, based on recommendations from the National Board of Health and Welfare [5]. A national quality register for mammography screening is being established in Sweden, but the historical lack of such a register has prevented the monitoring and reporting of attendance on a national level. Thus, annual mammography screening attendance for Sweden is not available in programme-based health statistics presented by either OECD.stat [6] or Eurostat [7]. An international survey among European countries reported a comparatively high overall attendance of 80% for Sweden in both 2010 and 2014 [2]. However, previous studies have found attendance to be lower in groups who may be socioeconomically vulnerable, such as women who were born abroad [[8], [9], [10], [11]], have low income [[9], [10], [11]], are unmarried or live without a partner [8,[10], [11], [12], [13]], are not gainfully employed [[8], [9], [10],13], have lower education, and do not own their home [8]. These studies were limited to two separate health care regions in Sweden (Uppsala and Skåne), and were based on mammography screening data up to 2009.
The objective of this study was to examine the association between mammography screening attendance and sociodemographic factors in 15 of Sweden's 21 health care regions. Attendance by sociodemographic factor are reported.
2. Materials and methods
This cross-sectional population-based register study was conducted in Sweden, where women between the ages of 40 and 74 are invited to mammography screening every 18–24 months depending on age and regional capacity. Each health care region individually conducts and administers screening, and there are thus differences in intervals between screening appointments, the layout and content of the invitation letter, hours of operation, ways of cancelling or rescheduling an appointment, reminders, etc. All invitations are sent by post and offer a pre-booked appointment date and time, which does not need to be confirmed, but can be rescheduled or cancelled.
Individual screening-related data for all women invited to the screening programme between 2014 and 2018 in 15 of 21 health care regions in Sweden (Fig. 1) were initially extracted, with an original study objective of also comparing attendance before and after removal of the out-of-pocket fee in 2016. These regions include about 81% of the women eligible for mammography screening in Sweden. All these regions used the same company (Sectra AB) for the administration and tracking of invitations, attendance and results throughout the entire study period, which enabled high-quality and consistency of screening data between regions. Among the six regions excluded from this study four (Jönköping, Kronoberg, Norrbotten and Uppsala) used other radiological information systems for all or part of the study period, and two (Sörmland and Östergötland) did not grant us permission to extract data. One of the three programmes operating in Stockholm (Karolinska University Hospital) also did not grant permission. This study was approved by the local ethics committee at Lund University (Nos. 2018/576 and 2018/965). Active informed consent as a requirement for data collection was waived.
Fig. 1.
Map of Swedish health care regions showing the population of women aged 40–75 in 2018. Excluded regions are hatched.
The data extracted included the date of the screening appointment, age at the screening appointment, and attendance outcome (attended, cancelled, missed and unavailable), for each regional mammography screening programme separately, and were merged into one dataset. The unique personal identity number assigned to all Swedish residents was used to merge screening data with information on individual-level sociodemographic characteristics obtained from population registers at Statistics Sweden (the Longitudinal Integration Database for Health Insurance and Labour Market Studies (LISA) [14], the Total Population Register [15] and the Geodatabase) [16]. The most recent sociodemographic information for each screening appointment was used. Same-year sociodemographic data were linked to each screening appointment in 2017. In 2018, same-year data were available only for home ownership and type of municipality, and data on income, education and cohabitation from 2017 were used.
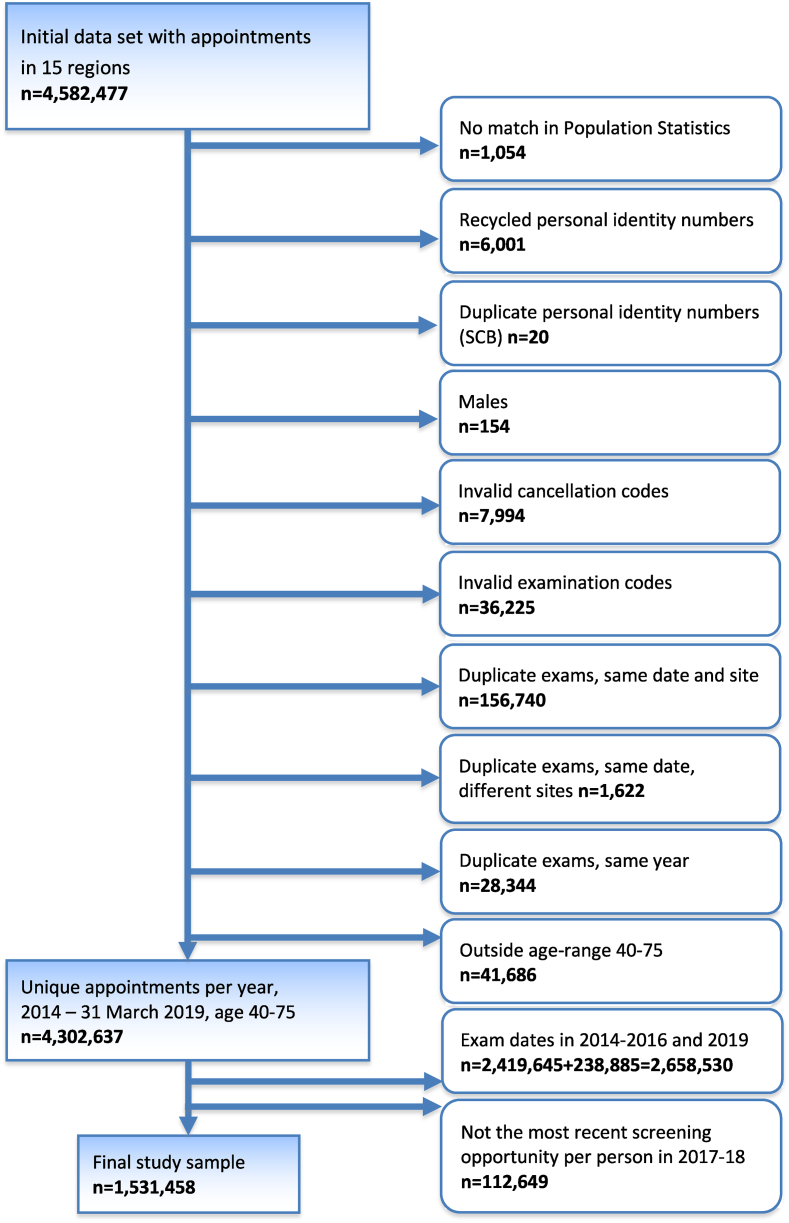
The initial dataset included a total of 4,582,477 appointments for 1,780,164 women. After the exclusions described in Fig. 2, the final study sample included 1,531,458 women. Only the most recent screening appointment for each woman, aged 40–75, within the complete two-year period of 2017-18 was included. Women aged 75 were included to allow for a certain overflow from the age limit of 74 years, due to administrative reasons, e.g., rescheduling. Appointments were excluded when personal identity numbers lacked a match, had duplicates or were suspected to have been recycled according to data from Statistics Sweden. Furthermore, appointments with examination or cancellation codes unrelated to mammography screening were excluded, as were appointments where it was known that the invitation did not reach the recipient (unavailable). Duplicate appointments within the same programme, at different locations and within the same year were also excluded.
Fig. 2.
Selection of the final study sample.
2.1. Outcome variable
The outcome variable was mammography screening attendance (yes/no) at the most recent screening appointment, irrespective of whether it was the original or a rescheduled appointment date, for each woman during the period 2017-18. A two-year period was chosen to allow for longer screening cycles which are common in several health care regions.
2.2. Sociodemographic and programme-related variables
Table 1 presents the sociodemographic variables, including age group, cohabitation (in which only couples who had children together were categorized as cohabiting), level of education, income (individual share of equivalized disposable household income in SEK), main source of income, home ownership, country of birth, and type of municipality (based on categorization by the Swedish Association of Local Authorities and Regions) [17]. The programme-related variables included were region and year of screening appointment. Categorizations of data were based on the way in which variables were provided by Statistics Sweden, and by logically and conceptually combining categories without affecting important differences in the attendance outcome, in order to minimize the number of categories. Information on specific country of birth were only retreived for larger groups living in Sweden (n > 20,000 in 2018). Thus, it was necessary to analyze country of birth in larger aggregate categories. Missing data constituted less than 0.3% of the data for all variables except education (1.2%) and home ownership (1.7%), and were excluded from the analyses. All variables were analyzed as categorical variables.
Table 1.
Sociodemographic and other characteristics of the study sample at the time of the most recent mammography screening appointment in Sweden 2017-18 (N = 1,531,458).
| Characteristic | All regions |
Stockholm |
Other |
|
|---|---|---|---|---|
| n | % | % | % | |
| Mean age (SD) | 56.00 | (10.09) | 54.75 | 56.37 |
| Age group (years) | ||||
| 40-44 | 252,903 | 16.51 | 19.80 | 15.57 |
| 45-49 | 234,095 | 15.29 | 16.86 | 14.83 |
| 50-54 | 242,434 | 15.83 | 15.81 | 15.84 |
| 55-59 | 208,768 | 13.63 | 13.47 | 13.68 |
| 60-64 | 203,443 | 13.28 | 12.75 | 13.44 |
| 65-69 | 197,702 | 12.91 | 10.20 | 13.22 |
| 70-75 | 192,113 | 12.54 | 11.11 | 13.43 |
| Cohabitation (living with partner) | ||||
| Yes | 906,451 | 59.19 | 53.99 | 60.68 |
| No | 620,828 | 40.54 | 45.69 | 39.06 |
| Missing | 4179 | 0.27 | 0.32 | 0.26 |
| Level of education | ||||
| Low (elementary school, ≤9 years) | 213,497 | 13.94 | 12.34 | 14.40 |
| Intermediate (secondary school) | 673,218 | 43.96 | 38.22 | 45.61 |
| High (post-secondary) | 625,993 | 40.88 | 47.86 | 38.87 |
| Missing | 18,750 | 1.22 | 1.58 | 1.12 |
| Income category | ||||
| Lowest (decile 1): ≤98,300 SEK | 152,581 | 9.96 | 9.11 | 10.21 |
| Low-medium (deciles 2–4): 98,400–162,700 SEK | 458,409 | 29.93 | 23.71 | 31.72 |
| Medium-high (deciles 5–10): ≥162,800 SEK | 916,293 | 59.83 | 66.86 | 57.81 |
| Missing | 4175 | 0.27 | 0.32 | 0.26 |
| Main source of income | ||||
| Employment | 939,067 | 61.32 | 65.32 | 60.23 |
| Retirement pension | 368,554 | 24.07 | 20.33 | 25.14 |
| Student financing | 6075 | 0.40 | 0.52 | 0.36 |
| Care of a sick child or relative | 8974 | 0.59 | 0.84 | 0.51 |
| Social assistance and benefits: | ||||
| Sickness benefit | 32,413 | 2.12 | 1.94 | 2.17 |
| Sickness compensation | 81,781 | 5.34 | 4.16 | 5.68 |
| Unemployment insurance/benefit | 8767 | 0.57 | 0.72 | 0.53 |
| Labour market measure | 19,130 | 1.25 | 1.42 | 1.20 |
| Financial assistance | 30,033 | 1.96 | 2.03 | 1.94 |
| No income | 32,489 | 2.12 | 2.60 | 1.98 |
| Missing | 4175 | 0.27 | 0.32 | 0.26 |
| Home ownership | ||||
| Yes (house or apartment) | 1,106,844 | 72.27 | 65.65 | 74.18 |
| No | 398,585 | 26.03 | 32.38 | 24.20 |
| Missing | 26,029 | 1.70 | 1.97 | 1.62 |
| Country of birth | ||||
| Sweden | 1,213,909 | 79.26 | 68.63 | 82.32 |
| Other Nordic countries | 57,226 | 73.74 | 5.21 | 3.31 |
| Other European countries | 111,140 | 7.26 | 9.68 | 6.56 |
| Other | 149,076 | 9.73 | 16.48 | 7.80 |
| Missing | 107 | 0.01 | 0.01 | 0.01 |
| Region | ||||
| Blekinge | 33,110 | 2.16 | ||
| Dalarna | 60,682 | 3.96 | ||
| Gotland | 13,832 | 0.90 | ||
| Gävleborg | 60,775 | 3.97 | ||
| Halland | 65,874 | 4.30 | ||
| Jämtland/Härjedalen | 26,699 | 1.74 | ||
| Kalmar | 50,630 | 3.31 | ||
| Skåne | 271,723 | 17.74 | ||
| Stockholm | 341,925 | 22.33 | ||
| Värmland | 59,993 | 3.92 | ||
| Västerbotten | 49,076 | 3.20 | ||
| Västernorrland | 50,988 | 3.33 | ||
| Västmanland | 47,125 | 3.08 | ||
| Västra Götaland | 348,371 | 22.75 | ||
| Örebro | 50,655 | 3.31 | ||
| Type of municipality | ||||
| Large cities (>200,000)a | 624,598 | 40.78 | 93.22 | 25.71 |
| Mid-sized cities (50,000–200,000)b | 472,790 | 30.87 | 6.34 | 37.92 |
| Smaller cities, towns and rural areas | 430,520 | 28.11 | 0.18 | 36.14 |
| Missing | 3550 | 0.23 | 0.26 | 0.22 |
| Year of scheduled appointment | ||||
| 2017 | 723,788 | 47.26 | 52.99 | 45.61 |
| 2018 | 807,670 | 52.74 | 47.01 | 54.39 |
Includes commuting zone.
Includes neighbouring municipalities.
2.3. Statistical analysis
Odds ratios (ORs) and 95% confidence intervals (CIs) were determined for mammography screening attendance by sociodemographic factor. Unadjusted estimates were calculated, as well as estimates adjusted for the potential confounding effect of region and age group. In multivariable analyses the effect of sociodemographic factors on attendance was further examined, both in the total sample and stratified by region (Stockholm vs. all other regions) and type of municipality.
Combinations of sociodemographic characteristics associated with lower likelihood of mammography screening attendance were also analyzed in order to identify groups with particularly low attendance. The statistical software used for the analyses was SPSS, version 25.
A sensitivity analysis was conducted among the 1,488,224 women whose primary appointment date (i.e., the one set in the invitation) was scheduled for 2017-18, to examine whether the results changed when using an alternative outcome of attendance within 90 days from the primary appointment date. Appointments up to March 31, 2019 were included in the sensitivity analysis. A cut-off of 90 days has been used in other studies examining screening attendance [[18], [19], [20], [21]].
3. Results
A total of 1,531,458 women were included in the study sample. The distribution of demographic characteristics is presented in Table 1 and shows that 59% of the study sample lived with a partner, 14% had a low level of education, social assistance and benefits was the main source of income in 11%, and employment or retirement income was the main source of income in 85%, 72% owned their own home, 79% were born in Sweden, 41% lived in a large city or surrounding commuting areas, and 28% lived in smaller cities, towns, or rural areas. The mean age at the time of the screening appointment was 56 years. The regions with the largest proportions of the study sample were Västra Götaland (23%), Stockholm (22%) and Skåne (18%).
Screening attendance per region and by sociodemographic factor are presented in Table 2. The overall attendance was 81.3% for all regions combined. Stockholm had the lowest attendance (71.7%), followed by Örebro (80.7%), while the highest attendance was observed in the northern regions of Västernorrland (87.1%) and Västerbotten (86.7%), and in the southern regions of Blekinge and Halland (86.7%). Screening attendance was lower among women living in large cities (77.0%) than among those living in mid-sized cities (83.7%) or smaller cities, towns or rural areas (85.3%). Attendance according to age group varied from 79.6% among women in their forties, to 84.4% among women 65–69 years of age. The lowest attendance was found among women whose main source of income was social assistance or benefits (66.7%), non-Nordic women born in Europe (68.0%) or elsewhere (68.6%), and among women in the lowest income decile (68.5%). Other sociodemographic groups with attendance below 75% were women who did not own their home (70.8%), women with low level of education (73.8%), and women living without a partner (74.4%).
Table 2.
Mammography screening attendance in Sweden in 2017–18 by sociodemographic factor.
| Variable | Total |
Attenders |
|||
|---|---|---|---|---|---|
| N | All regions |
Stockholm |
Other |
||
| n | % | % | % | ||
| Total | 1,531,458 | 1,244,938 | 81.29 | 71.66 | 84.06 |
| Age group | |||||
| 40-44 | 252,903 | 201,431 | 79.65 | 70.93 | 82.84 |
| 45-49 | 234,095 | 186,377 | 79.62 | 70.35 | 82.64 |
| 50-54 | 242,434 | 193,850 | 79.96 | 70.11 | 82.79 |
| 55-59 | 208,768 | 169,263 | 81.08 | 70.93 | 83.95 |
| 60-64 | 203,443 | 167,181 | 82.18 | 71.08 | 85.20 |
| 65-69 | 197,702 | 166,772 | 84.36 | 75.13 | 85.13 |
| 70-75 | 192,113 | 160,064 | 83.32 | 75.53 | 86.45 |
| Cohabitation | |||||
| Yes | 906,451 | 781,575 | 86.22 | 77.16 | 88.54 |
| No | 620,828 | 461,840 | 74.39 | 65.46 | 77.38 |
| Level of education | |||||
| Low | 213,497 | 157,628 | 73.83 | 60.66 | 77.08 |
| Intermediate | 673,218 | 550,772 | 81.81 | 70.95 | 84.43 |
| High | 625,993 | 528,040 | 84.35 | 76.27 | 87.21 |
| Income | |||||
| Lowest decile | 152,581 | 104,481 | 68.48 | 53.09 | 72.42 |
| Deciles 2-4 | 458,409 | 362,576 | 79.09 | 66.49 | 81.80 |
| Deciles 5-10 | 916,293 | 776,360 | 84.73 | 76.23 | 87.55 |
| Main source of income | |||||
| Employment/retirement | 1,307,621 | 1,100,981 | 84.20 | 74.91 | 86.87 |
| Student financing | 6075 | 4463 | 73.47 | 65.82 | 76.64 |
| Care of sick child/relative | 8974 | 6170 | 68.75 | 60.85 | 72.50 |
| Social assistance/benefits | 172,124 | 114,721 | 66.65 | 54.89 | 69.67 |
| No income | 32,489 | 17,082 | 52.58 | 41.12 | 56.89 |
| Home ownership | |||||
| Yes | 1,106,844 | 946,146 | 85.48 | 76.84 | 87.68 |
| No | 398,585 | 282,183 | 70.80 | 62.14 | 74.13 |
| Country of birth | |||||
| Sweden | 1,213,909 | 1,023,765 | 84.34 | 76.15 | 86.30 |
| Other Nordic countries | 57,226 | 43,331 | 75.72 | 69.42 | 78.56 |
| Other European countries | 111,140 | 75,561 | 67.99 | 59.28 | 71.68 |
| Other | 149,076 | 102,220 | 68.57 | 60.94 | 73.21 |
| Region | |||||
| Blekinge | 33,110 | 28,715 | 86.73 | ||
| Dalarna | 60,682 | 51,165 | 84.32 | ||
| Gotland | 13,832 | 11,368 | 82.19 | ||
| Gävleborg | 60,775 | 50,837 | 83.65 | ||
| Halland | 65,874 | 57,119 | 86.71 | ||
| Jämtland/Härjedalen | 26,699 | 22,963 | 86.01 | ||
| Kalmar | 50,630 | 42,708 | 84.35 | ||
| Skåne | 271,723 | 222,339 | 81.83 | ||
| Stockholm | 341,925 | 245,025 | 71.66 | ||
| Värmland | 59,993 | 51,355 | 85.60 | ||
| Västerbotten | 49,076 | 42,554 | 86.71 | ||
| Västernorrland | 50,988 | 44,425 | 87.13 | ||
| Västmanland | 47,125 | 40,509 | 85.96 | ||
| Västra Götaland | 348,371 | 292,982 | 84.10 | ||
| Örebro | 50,655 | 40,874 | 80.69 | ||
| Type of municipality | |||||
| Large cities | 624,598 | 481,078 | 77.02 | 72.27 | 81.98 |
| Mid-sized cities | 472,790 | 395,641 | 83.68 | 65.05 | 84.58 |
| Smaller cities, towns and rural areas | 430,520 | 367,119 | 85.27 | 62.28 | 85.31 |
The results of the logistic regression analysis of attendance data are presented in Table 3. Generally, the associations between sociodemographic factors and attendance were slightly weakened when adjusting for region and age group, with the exception of education and income, where the association between low and intermediate level of education, as well as the four lower deciles of income, and attendance became stronger. The effect size of having social assistance and benefits as the main source of income also increased. In the multivariable model all associations were reduced compared to both unadjusted estimates and those adjusted for region and age. However, each sociodemographic factor was still independently associated with attendance. The odds of attending were lowest among women who were living without a partner (OR = 0.52, 95% CI: 0.52–0.53), among those with the lowest income (OR = 0.57, 95% CI: 0.56–0.57), and among non-Nordic women born in Europe (OR = 0.60, 95% CI: 0.59–0.61). Furthermore, attendance was less likely among women whose main source of income was social assistance or benefits (OR = 0.62, 95% CI: 0.62–0.63), among those not owning their home (OR = 0.66, 95% CI: 0.66–0.67), and among those with low level of education (OR = 0.72, 95% CI: 0.71–0.73).
Table 3.
Logistic regression analysis of mammography screening attendance by sociodemographic factor in Sweden in 2017–18, with stratification by region (Stockholm vs. other regions). Odds Ratios (ORs) and 95% Confidence Intervals (CIs).
| Variable | Unadjusted |
Adjusted for age and regiona,b |
Multivariatec All regions (N = 1,490,880) |
Multivariate Stockholm (N = 330,867) |
Multivariate Other regions (N = 1,160,013) |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Cohabitation | |||||
| Yes | Ref | Ref | Ref | Ref | Ref |
| No | 0.46 (0.46–0.47) | 0.47 (0.46–0.47) | 0.52 (0.52–0.53) | 0.59 (0.58–0.60) | 0.49 (0.49–0.50) |
| Level of education | |||||
| Low | 0.52 (0.52–0.53) | 0.45 (0.45–0.46) | 0.72 (0.71–0.73) | 0.70 (0.69–0.72) | 0.72 (0.71–0.74) |
| Intermediate | 0.83 (0.83–0.84) | 0.76 (0.75–0.77) | 0.88 (0.87–0.89) | 0.85 (0.84–0.87) | 0.89 (0.88–0.90) |
| High | Ref | Ref | Ref | Ref | Ref |
| Income | |||||
| Lowest decile | 0.39 (0.39–0.40) | 0.36 (0.36–0.36) | 0.57 (0.56–0.57) | 0.59 (0.57–0.61) | 0.55 (0.54–0.56) |
| Decile 2-4 | 0.68 (0.68–0.69) | 0.61 (0.60–0.61) | 0.74 (0.74–0.75) | 0.74 (0.73–0.76) | 0.74 (0.73–0.75) |
| Decile 5-10 | Re | Ref | Ref | Ref | Ref |
| Main source of income | |||||
| Employment/retirement | Ref | Ref | Ref | Ref | Ref |
| Student finance | 0.52 (0.49–0.55) | 0.58 (0.54–0.61) | 0.82 (0.77–0.87) | 0.94 (0.86–1.06) | 0.75 (0.69–0.81) |
| Care of sick child/relative | 0.41 (0.39–0.43) | 0.46 (0.44–0.48) | 0.61 (0.58–0.64) | 0.70 (0.64–0.75) | 0.57 (0.54–0.61) |
| Social assistance/benefits | 0.38 (0.37–0.38) | 0.36 (0.35–0.36) | 0.62 (0.62–0.63) | 0.71 (0.69–0.73) | 0.60 (0.59–0.61) |
| No income | 0.21 (0.20–0.21) | 0.21 (0.21–0.22) | 0.37 (0.36–0.38) | 0.40 (0.38–0.42) | 0.36 (0.35–0.37) |
| Home ownership | |||||
| Yes | Ref | Ref | Ref | Ref | Ref |
| No | 0.41 (0.41–0.42) | 0.43 (0.43–0.44) | 0.66 (0.66–0.67) | 0.71 (0.70–0.72) | 0.65 (0.64–0.65) |
| Country of birth | |||||
| Sweden | Ref | Ref | Ref | Ref | Ref |
| Other Nordic countries | 0.58 (0.57–0.59) | 0.61 (0.60–0.62) | 0.74 (0.73–0.76) | 0.79 (0.76–0.82) | 0.72 (0.70–0.74) |
| Other European countries | 0.39 (0.39–0.40) | 0.43 (0.42–0.43) | 0.60 (0.59–0.61) | 0.65 (0.63–0.66) | 0.58 (0.57–0.59) |
| Other | 0.41 (0.40–0.41) | 0.47 (0.46–0.47) | 0.80 (0.79–0.81) | 0.76 (0.74–0.77) | 0.83 (0.81–0.84) |
| Age group | |||||
| 40-44 | 0.73 (0.71–0.74) | 0.77 (0.76–0.78) | 0.81 (0.79–0.82) | 0.80 (0.77–0.82) | 0.81 (0.80–0.83) |
| 45-49 | 0.72 (0.71–0.74) | 0.76 (0.74–0.77) | 0.76 (0.75–0.77) | 0.76 (0.73–0.78) | 0.77 (0.75–0.78) |
| 50-54 | 0.74 (0.73–0.75) | 0.76 (0.75–0.77) | 0.76 (0.75–0.78) | 0.76 (0.74–0.78) | 0.77 (0.75–0.78) |
| 55-59 | 0.79 (0.78–0.81) | 0.81 (0.80–0.82) | 0.85 (0.84–0.87) | 0.83 (0.80–0.86) | 0.87 (0.85–0.88) |
| 60-64 | 0.86 (0.84–0.87) | 0.87 (0.85–0.88) | 0.93 (0.92–0.95), | 0.84 (0.82–0.87) | 0.97 (0.95–1.00) |
| 65-69 | Ref | Ref | Ref | Ref | Ref |
| 70-75 | 0.93 (0.91–0.94) | 0.92 (0.90–0.93) | 0.97 (0.95–0.99) | 1.00 (0.96–1.03) | 0.96 (0.94–0.98) |
| Region | |||||
| Blekinge | 0.97 (0.93–1.01) | 0.97 (0.93–1.01) | 1.03 (0.99–1.08) | 1.04 (0.99–1.08) | |
| Dalarna | 0.79 (0.77–0.82) | 0.79 (0.77–0.82) | 0.82 (0.79–0.85) | 0.82 (0.79–0.85) | |
| Gotland | 0.68 (0.65–0.72) | 0.68 (0.65–0.71) | 0.68 (0.65–0.72) | 0.68 (0.65–0.72) | |
| Gävleborg | 0.76 (0.73–0.78) | 0.75 (0.73–0.78) | 0.82 (0.79–0.85) | 0.83 (0.80–0.86) | |
| Halland | 0.96 (0.93–1.00) | 0.97 (0.94–1.01) | 0.97 (0.94–1.01) | 0.97 (0.94–1.01) | |
| Jämtland/Härjedalen | 0.91 (0.87–0.95) | 0.91 (0.87–0.95) | 0.92 (0.88–0.96) | 0.92 (0.88–0.97) | |
| Kalmar | 0.80 (0.77–0.83) | 0.80 (0.77–0.83) | 0.83 (0.80–0.87) | 0.83 (0.80–0.87) | |
| Skåne | 0.67 (0.65–0.68) | 0.67 (0.65–0.69) | 0.78 (0.76–0.80) | 0.79 (0.76–0.81) | |
| Stockholm | 0.37 (0.36–0.38) | 0.38 (0.37–0.39) | 0.42 (0.41–0.44) | ||
| Värmland | 0.88 (0.85–0.91) | 0.88 (0.85–0.91) | 0.95 (0.92–0.99) | 0.96 (0.92–0.99) | |
| Västerbotten | 0.96 (0.93–1.00) | 0.96 (0.93–1.00) | 0.93 (0.90–0.97) | 0.93 (0.90–0.97) | |
| Västernorrland | Ref | Ref | Ref | Ref | |
| Västmanland | 0.90 (0.87–0.94) | 0.91 (0.88–0.94) | 1.02 (0.98–1.06) | 1.02 (0.98–1.06) | |
| Västra Götaland | 0.78 (0.76–0.80) | 0.78 (0.76–0.81) | 0.87 (0.85–0.90) | 0.88 (0.85–0.90) | |
| Örebro | 0.62 (0.60–0.64) | 0.62 (0.60–0.64) | 0.68 (0.66–0.71) | 0.69 (0.66–0.71) | |
| Type of municipality | |||||
| Large cities | 0.58 (0.57–0.58) | 0.85 (0.84–0.87) | |||
| Mid-sized cities | 0.89 (0.88–0.90) | 0.94 (0.93–0.95) | |||
| Smaller cities, towns and rural areas | Ref | Ref | |||
Estimates for region are adjusted for age group and estimates for age group are adjusted for region.
For numbers included please refer to Table 1, All Regions, 2017–2018.
The multivariate model includes all variables in the table.
A separate analysis was conducted to examine the impact of specific countries of birth on screening attendance (Appendix A). With very few exceptions a statistically significant improvement in the odds of attending was seen for all countries of birth compared to Sweden when adjusting for other sociodemographic factors. Among women born in Iraq and Syria, two of the largest groups in Sweden (1.3% and 1.0% of the study sample, respectively), the odds of attending surpassed those of women born in Sweden after adjusting for other sociodemographic factors. This was also the case for women born in Afghanistan. Other countries were the odds of attending increased by over 100% were African countries, Lebanon and Turkey.
When the multivariable model was stratified by region (Stockholm vs. all other regions) the associations between sociodemographic factors and screening attendance were generally somewhat weaker in Stockholm compared to other regions in Sweden (Table 3). Exceptions were having an intermediate level of education and being born outside of Europe, where women in Stockholm had lower odds of attending mammography screening than women in other regions. Stratification by type of municipality (Table 4) showed that the effect of living without a partner was weaker in large cities, which is partly explained by Stockholm being included in this analysis. The effect of low and intermediate education was weaker in small cities and rural areas. Having an income from other main sources than employment or retirement pension was not as strongly associated with low attendance in large cities, and was more strongly associated with low attendance in small cities and rural areas. The association between country of birth and screening attendance was weaker among women born in a Nordic country and living in large cities, stronger among women born in a European country and living in small cities, and stronger among women born in countries outside of Europe and living in large cities. Stratifying by either region or type of municipality did not change the direction or remove statistical significance for any of the associations between sociodemographic factors and mammography screening attendance.
Table 4.
Multivariable logistic regression analysisa of mammography screening attendance in Sweden in 2017–18, by sociodemographic factor and stratified by type of municipality. Odds ratios (ORs) and 95% Confidence intervals (CIs).
| Variable | Large cities (N = 607,794) |
Mid-sized cities (N = 461,921) |
Small cities/rural areas (N = 421,165) |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Cohabitation | |||
| Yes | Ref | Ref | Ref |
| No | 0.56 (0.56–0.57) | 0.50 (0.49–0.51) | 0.48 (0.47–0.49) |
| Level of education | |||
| Low | 0.71 (0.70–0.73) | 0.67 (0.65–0.68) | 0.77 (0.75–0.80) |
| Intermediate | 0.86 (0.85–0.87) | 0.83 (0.82–0.85) | 0.98 (0.96–1.00) |
| High | Ref | Ref | Ref |
| Income | |||
| Lowest decile | 0.57 (0.56–0.59) | 0.56 (0.54–0.58) | 0.53 (0.52–0.55) |
| Decile 2-4 | 0.74 (0.73–0.75) | 0.74 (0.72–0.75) | 0.74 (0.72–0.76) |
| Decile 5-10 | Ref | Ref | Ref |
| Main source of income | |||
| Employment/retirement | Ref | Ref | Ref |
| Student finance | 0.90 (0.83–0.98) | 0.77 (0.69–0.87) | 0.67 (0.59–0.77) |
| Care of sick child/relative | 0.68 (0.63–0.72) | 0.55 (0.50–0.61) | 0.53 (0.48–0.60) |
| Social assistance/benefits | 0.68 (0.66–0.69) | 0.61 (0.60–0.63) | 0.56 (0.54–0.57) |
| No income | 0.41 (0.39–0.43) | 0.34 (0.32–0.36) | 0.34 (0.32–0.36) |
| Home ownership | |||
| Yes | Ref | Ref | Ref |
| No | 0.67 (0.66–0.68) | 0.65 (0.64–0.67) | 0.68 (0.67–0.70) |
| Country of birth | |||
| Sweden | Ref | Ref | Ref |
| Other Nordic countries | 0.81 (0.79–0.84) | 0.72 (0.70–0.75) | 0.67 (0.64–0.70) |
| Other European countries | 0.62 (0.60–0.63) | 0.63 (0.61–0.65) | 0.56 (0.54–0.58) |
| Other | 0.73 (0.72–0.75) | 0.96 (0.93–0.99) | 0.91 (0.88–0.95) |
The model includes all variables in the table, age group and region.
When sociodemographic characteristics, for which the likelihood of attending mammography screening were low (living without a partner, low level of education, lowest income, having social assistance or benefits as the main source of income, not owning one's home and non-Nordic country of birth) were combined in a summary risk factor index, ranging from zero to six (Table 5), attendance declined significantly with each additional risk factor up to four (OR = 0.15, 95% CI: 0.15–0.16), and then increased somewhat. The only specific pairs of risk factors where attendance was lower than for each individual risk factor were low income and living without a partner (OR = 0.23, 95% CI: 0.23–0.24), and living on social assistance and without a partner (OR = 0.30, 95% CI: 0.29–0.30). Only some of the women whose main source of income is social assistance or benefits also fall into the lowest income category (17.9%).
Table 5.
Mammography screening attendance in Sweden in 2017–18 by sum and specific combinationsa of sociodemographic risk factors for low attendance. Odds Ratios (ORs) and 95% Confidence Intervals (CIs).
| Variable | Total |
Attenders |
Adjusted for age and region |
|
|---|---|---|---|---|
| n (%)b | n | % | OR (95% CI) | |
| Sum of risk factorsc | ||||
| 0 risk factors | 554,971 (36.24) | 501,109 | 90.29 | Ref |
| 1 | 470,700 (30.74) | 392,860 | 83.46 | 0.55 (0.55–0.56) |
| 2 | 297,837 (19.45) | 222,148 | 74.59 | 0.33 (0.32–0.33) |
| 3 | 135,373 (8.84) | 85,692 | 63.30 | 0.19 (0.19–0.19) |
| 4 | 53,229 (3.48) | 31,162 | 58.54 | 0.15 (0.15–0.16) |
| 5 | 17,570 (1.15) | 10,859 | 61.80 | 0.17 (0.17–0.18) |
| 6 | 1778 (0.12) | 1108 | 62.32 | 0.16 (0.14–0.17) |
| Low income + living alone | 42,674 (2.79) | 21,745 | 50.96 | 0.23 (0.23–0.24) |
| Social assistance + living alone | 98,524 (6.43) | 58,710 | 59.59 | 0.30 (0.29–0.30) |
Combinations of two specific risk factors are presented where attendance for the combination of factors is at least ten percent lower than for each individual risk factor.
Percent of all women (N = 1,531,458).
Living without a partner, lowest level of education, lowest income level, social assistance, not owning a home and Non-Nordic country of birth.
The sensitivity analysis among women with a primary appointment date in 2017-18 resulted in an attendance of 78.9% within 90 days of the primary appointment date. Compared to the estimates presented in Table 2, attendance was consistently lower across all categories of the sociodemographic variables, and logistic regression estimates were very similar to those presented in Table 3 (data not shown). Among women with a primary appointment date in 2017–18, 43% had rescheduled their appointment either to an earlier date (13%), or a later date (30%) (data not shown). Information on the primary appointment date was missing for 4.9% of women with appointment dates in 2017 and for 1.3% of women with appointment dates in 2018.
4. Discussion
In this cross-sectional population-based register study of mammography screening attendance in Sweden in 2017–18, we found that the overall attendance was 81.3%. The lowest odds of attending were found among women living without a partner, low-income women, and non-Nordic women born in Europe. Lower odds of attendance were also observed among women whose main source of income was social assistance or benefits, those not owning their home and among those with low level of education. Having multiple of these sociodemographic characteristics further lowered the odds of attending.
European guidelines state that an attendance over 70% is acceptable, but that an attendance over 75% is desirable [22]. Our study identified unacceptably low attendance among low-income women, women born outside the Nordic countries, and those without employment or retirement pension as the main source of income. Other sociodemographic groups where attendance is below desired level and should be improved are women living without a partner, women with low level of education, and women not owning their home. The markedly lower attendance rate in Stockholm compared to the rest of the country is confirmed by a previous study reporting an attendance rate of 70% in Stockholm in 2012 and historically [20]. The odds of attending did not increase when adjusting for sociodemographic factors in the multivariate analysis, nor did the stratified analysis show stronger associations between sociodemographic factors and screening attendance in Stockholm.
Previous studies have found that socioeconomically vulnerable groups and women born abroad have less favourable breast cancer outcomes and survival rates [[23], [24], [25], [26]], and these factors therefore warrant extra attention. We found that low socioeconomic status, represented by low income, low level of education, not being financially supported mainly by employment or retirement pension, and not being a homeowner, reduced the odds of attending mammography screening. Similar results have been found in previous Swedish and international studies with respect to low income [[9], [10], [11],27], employment status [8,9,13,28], low education [9,27], home ownership [8] and area-level socioeconomic deprivation [9,26,29]. However, some studies found no significant effects of employment status [27,30] or socioeconomic level [30], and no, or a U-shaped, association for education [10,11,28,30]. Our finding of lower odds of attending among women born abroad is supported by studies in Sweden [[8], [9], [10], [11]] and Denmark [28], and a review of US studies found lower adherence among recent immigrants [27]. The effect of country of birth (when three aggregate categories were compared to Sweden) was partly accounted for by socioeconomic status, but an independent association with attendance remained, particularly among non-Nordic women born in Europe. In a more detailed analysis of country of birth, women born in Iraq, Syria and Afghanistan were more likely to attend than women born in Sweden once other sociodemographic factors were accounted for. Our findings suggest that the impact of culture, language and socioeconomic factors vary considerably depending on country of birth.
Furthermore, the finding of lower odds of attending among women living without a partner are corroborated by Swedish and international studies, where lower odds of attending were observed among unmarried women [9,10,13,27,30] and among women living without a partner [8,12,28]. Having a partner may increase the probability of being proactive about one's health, perhaps due to feelings of accountability towards a significant other. Cohabitation may also indicate a higher level of social, emotional and practical support as well as household income, although the effect of cohabitation remained stable and statistically significant when adjusting for equivalized disposable income, which takes the whole household income into consideration.
4.1. Strengths and limitations
This is the first study in Sweden in which individual-level screening attendance data have been collected from the majority of Sweden's health care regions to assess screening attendance nationally, regionally, and by different sociodemographic factors.
The attendance might be somewhat overestimated since our definition of attendance was based on the appointments taking place within the time period 2017-18, whether it was the primary appointment date offered in the invitation or a rescheduled appointment. Attendance within 90 days of primary appointment dates in 2017-18 was 1.5% points lower. Considering that information on primary appointment date was missing for 4.9% of the women with screening dates in 2017 and for 1.3% of those with screening dates in 2018, attendance based on this date may be slightly less reliable. However, the sensitivity analysis showed that both attendance outcomes had very similar associations with sociodemographic factors.
Not all health care regions in Sweden were included in this study, and the overall attendance presented may not be representative of the whole country. However, the 15 regions included are geographically well distributed and represent populations of all sizes and densities, and we have no reason to believe that regions with particularly high or low attendance would have been systematically selected. Assuming that screening attendance of the excluded programme in Stockholm (Karolinska University Hospital) was also 71.7%, and that the attendance of 84.1% observed among the other 14 regions applied to the six regions not included, yields an estimated overall attendance of 81.3%. When instead, for each of the six excluded regions, imputing the proportion of those attending screening in a neighbouring region, a very similar attendance of 81.4% was obtained. More importantly, it is unlikely that the association between sociodemographic factors and screening attendance would have differed in the excluded regions.
Despite these limitations, our population study has many strengths, including its large size. While many studies that rely on self-reported data may suffer from low response rates and selection bias, the data used in this study for both exposure and outcome measures were obtained from high-quality registers, thus minimizing measurement error and misclassification. However, some women categorized as non-attenders may have attended mammography screening at private clinics. These are more common in the largest cities and this may partially explain the lower attendance in those regions, particularly in Stockholm where there are several private clinics [20].
The sociodemographic data used in this study originate from many different official sources with high coverage [14]. Although complete or almost complete data were available for most variables (age, region, country of birth, income and cohabitation), information on education was missing for 1.2% of the study sample and among 3.6% of the non-attenders (data not shown). An evaluation in 2006 showed that the level and type of education was correct for 85% of individuals, with higher validity among individuals born in Sweden, and it was suggested that the proportion with low education was overestimated [14]. Moreover, information on home ownership was missing for 1.7% of the study sample and 3.3% of non-attenders, and it is plausible that those with missing information are less likely to be homeowners. Thus, we may have underestimated the effect of both education and home ownership on attendance.
Furthermore, when interpreting the effect of cohabitation, it is important to consider that common-law partners cannot be linked in Swedish official records on households if they do not have children together. Therefore, the number of women cohabiting is somewhat underestimated. This classification bias would likely have attenuated rather than inflated the effect of cohabitation on screening attendance.
5. Conclusions
Significant variations in the likelihood of attending mammography screening were found for cohabitation, education, income level and main source, home ownership and country of birth. Having combinations of these characteristics further decreased the odds of attending. Although overall attendance in Sweden is high, continuous efforts should be made to address persisting inequalities. Particular attention should be given to low-income women who live without a partner. These finding may apply to similar settings with population-based screening, universal health care, and a high screening uptake.
Declaration of competing interest
None.
Acknowledgement
The authors are grateful to Gabriel Cetin, Erik Fornander and Anna Löfborg at Sectra Sverige AB for their work in extracting the data, Fredrik Sandin at the Regional Cancer Centre Uppsala Örebro, and to all the regional mammography programmes for their assistance in the data collection process.
This study was commissioned and funded by the Swedish Agency for Health and Care Services Analysis. This agency had no involvement in study design, collection, analysis or interpretation of data, nor in the writing of the report or in the decision to submit the article for publication.
Appendix A. Detailed analysis of the impact of country of birth on mammography screening attendance in Sweden in 2017–18. Odds Ratios (ORs) and 95% Confidence Intervals (CIs)
| Country | Total (N) | Proportion of sample (%) | Attended (N) | Attended (%) | OR (95% CI) | Adjusted OR (95% CI)a | Increase in OR (%) |
|---|---|---|---|---|---|---|---|
| Nordic countries | |||||||
| Sweden | 1,213,909 | 79.26 | 1,023,765 | 84.34 | Ref | Ref | |
| Denmark | 8220 | 0.54 | 6177 | 75.15 | 0.56 (0.53–0.59) | 0.71 (0.67–0.76) | 26.87 |
| Finland | 38,435 | 2.51 | 29,219 | 76.02 | 0.59 (0.58–0.60) | 0.77 (0.75–0.79) | 30.05 |
| Norway | 9501 | 0.62 | 7142 | 75.17 | 0.56 (0.54–0.59) | 0.70 (0.66–0.74) | 24.56 |
| Nordic other | 1070 | 0.07 | 793 | 74.11 | 0.53 (0.46–0.61) | 0.63 (0.54–0.73) | 17.67 |
| European Union (28) | |||||||
| Germany | 7421 | 0.48 | 5028 | 67.75 | 0.39 (0.37–0.41) | 0.48 (0.45–0.50) | 22.31 |
| Poland | 21,062 | 1.38 | 13,217 | 62.75 | 0.31 (0.30–0.32) | 0.48 (0.47–0.50) | 53.67 |
| Romania | 5060 | 0.33 | 3179 | 62.83 | 0.31 (0.30–0.33) | 0.46 (0.43–0.49) | 46.18 |
| United Kingdom | 2856 | 0.19 | 2086 | 73.04 | 0.50 (0.46–0.55) | 0.64 (0.58–0.70) | 26.44 |
| EU28 other | 23,543 | 1.54 | 15,817 | 67.18 | 0.38 (0.37–0.39) | 0.57 (0.56–0.59) | 51.05 |
| Other European countries | |||||||
| Bosnia and Herzegovina | 11,940 | 0.78 | 8705 | 72.91 | 0.50 (0.48–0.52) | 0.68 (0.65–0.71) | 36.20 |
| Yugoslavia | 16,511 | 1.08 | 11,969 | 72.49 | 0.49 (0.47–0.51) | 0.69 (0.67–0.72) | 41.72 |
| Russia | 4860 | 0.32 | 3237 | 66.60 | 0.37 (0.35–0.39) | 0.62 (0.58–0.67) | 68.65 |
| Europe other | 8046 | 0.53 | 5766 | 71.66 | 0.47 (0.45–0.49) | 0.83 (0.79–0.88) | 76.60 |
| USA | 2714 | 0.18 | 1780 | 65.59 | 0.35 (0.33–0.38) | 0.49 (0.45–0.54) | 38.14 |
| North America other | 3164 | 0.21 | 2216 | 70.04 | 0.43 (0.40–0.47) | 0.71 (0.65–0.77) | 62.90 |
| Chile | 6815 | 0.45 | 4512 | 66.21 | 0.36 (0.35–0.38) | 0.66 (0.63–0.70) | 81.32 |
| South America other | 8657 | 0.57 | 6089 | 70.34 | 0.44 (0.42–0.46) | 0.77 (0.73–0.81) | 74.77 |
| Africa | |||||||
| Eritrea (East Africa) | 4249 | 0.28 | 2810 | 66.13 | 0.36 (0.34–0.39) | 1.01 (0.94–1.08) | 178.24 |
| Ethiopia (East Africa) | 3573 | 0.23 | 2142 | 59.95 | 0.28 (0.26–0.30) | 0.63 (0.59–0.68) | 126.62 |
| Somalia (East Africa) | 6377 | 0.42 | 2639 | 41.38 | 0.13 (0.13–0.14) | 0.37 (0.35–0.39) | 180.15 |
| Africa other | 10,758 | 0.70 | 7082 | 65.83 | 0.36 (0.34–0.37) | 0.79 (0.76–0.83) | 120.39 |
| Oceania | 592 | 0.04 | 405 | 68.41 | 0.40 (0.34–0.48) | 0.59 (0.48–0.71) | 45.52 |
| Asia | |||||||
| Afghanistan | 3737 | 0.24 | 2664 | 71.29 | 0.46 (0.43–0.50) | 1.19 (1.09–1.29) | 157.70 |
| China | 4286 | 0.28 | 2998 | 69.95 | 0.43 (0.41–0.46) | 0.77 (0.72–0.83) | 78.70 |
| India | 2792 | 0.18 | 1933 | 69.23 | 0.42 (0.39–0.45) | 0.62 (0.57–0.68) | 47.85 |
| Iran | 13,791 | 0.90 | 10,104 | 73.27 | 0.51 (0.49–0.53) | 0.83 (0.80–0.87) | 63.06 |
| Iraq | 19,807 | 1.29 | 14,102 | 71.20 | 0.46 (0.45–0.47) | 1.08 (1.04–1.12) | 135.29 |
| Lebanon | 5563 | 0.36 | 3863 | 69.44 | 0.42 (0.40–0.45) | 0.89 (0.83–0.94) | 109.95 |
| Syria | 15,003 | 0.98 | 10,659 | 71.05 | 0.46 (0.44–0.47) | 1.15 (1.10–1.19) | 151.54 |
| Thailand | 13,290 | 0.87 | 9494 | 71.44 | 0.47 (0.45–0.48) | 0.83 (0.80–0.87) | 78.28 |
| Turkey | 9841 | 0.64 | 6557 | 66.63 | 0.37 (0.36–0.39) | 0.84 (0.80–0.88) | 126.15 |
| Asia other | 22,266 | 1.45 | 15,694 | 70.48 | 0.44 (0.43–0.46) | 0.74 (0.71–0.76) | 65.54 |
| Soviet Union | 1617 | 0.11 | 1015 | 62.77 | 0.31 (0.28–0.35) | 0.49 (0.44–0.55) | 57.83 |
| Stateless | 2 | 0.00 | 1 | 50.00 | 0.19 (0.01–2.97) | 0.30 (0.01–6.76) | 62.37 |
| Unknown | 23 | 0.00 | 18 | 78.26 | 0.67 (0.25–1.80) | 0.96 (0.34–2.73) | 43.80 |
| Missing | 107 | 0.01 | 61 | 57.01 | 0.25 (0.17–0.36) | 0.58 (0.37–0.91) | 134.96 |
Adjusted for age, region, cohabitation, education, income, main source of income and home ownership.
References
- 1.European Commission Initiative on Breast Cancer (2020) European guidelines on breast cancer screening and diagnosis. European Commission; 2020. https://healthcare-quality.jrc.ec.europa.eu/european-breast-cancer-guidelines [Google Scholar]
- 2.Deandrea S., Molina-Barceló A., Uluturk A., Moreno J., Neamtiu L., Peiró-Pérez R., Saz-Parkinson Z., Lopez-Alcalde J., Lerda D., Salas D. Presence, characteristics and equity of access to breast cancer screening programmes in 27 European countries in 2010 and 2014. Results from an international survey. Prev Med. 2016;91:250–263. doi: 10.1016/j.ypmed.2016.08.021. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health and Social Affairs . 2017. Health and medical services act (SFS 2017:30) [Stockholm, Sweden] [Google Scholar]
- 4.Olsson S., Andersson I., Karlberg I., Bjurstam N., Frodis E., Håkansson S. Implementation of service screening with mammography in Sweden: from pilot study to nationwide programme. J Med Screen. 2000;7(1):14–18. doi: 10.1136/jms.7.1.14. [DOI] [PubMed] [Google Scholar]
- 5.National Board of Health and Welfare . National Board of Health and Welfare; Stockholm: 2014. Screening för bröstcancer - rekommendation och bedömningsunderlag [Breast cancer screening - recommendation and basis for decision] [Google Scholar]
- 6.OECD.stat - Health Care Utilisation Screening (2020) Organisation for economic co-operation and development (OECD) https://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_STAT
- 7.Eurostat - breast cancer and cervical cancer screenings [hlth_ps_scre] (2020) Eurostat, the statistical office of the European Union. https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_ps_scre&lang=en
- 8.Lagerlund M., Maxwell A.E., Bastani R., Thurfjell E., Ekbom A., Lambe M. Sociodemographic predictors of non-attendance at invitational mammography screening – a population-based register study (Sweden) Cancer Causes Control. 2002;13(1):73–82. doi: 10.1023/a:1013978421073. [DOI] [PubMed] [Google Scholar]
- 9.Lagerlund M., Merlo J., Vicente R.P., Zackrisson S. Does the neighborhood area of residence influence non-attendance in an urban mammography screening program? A multilevel study in a Swedish city. PloS One. 2015;10(10) doi: 10.1371/journal.pone.0140244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zackrisson S., Andersson I., Manjer J., Janzon L. Non-attendance in breast cancer screening is associated with unfavourable socio-economic circumstances and advanced carcinoma. Int J Cancer. 2004;108(5):754–760. doi: 10.1002/ijc.11622. [DOI] [PubMed] [Google Scholar]
- 11.Zackrisson S., Lindström M., Moghaddassi M., Andersson I., Janzon L. Social predictors of non-attendance in an urban mammographic screening programme: a multilevel analysis. Scand J Publ Health. 2007;35(5):548–554. doi: 10.1080/14034940701291716. [DOI] [PubMed] [Google Scholar]
- 12.Lagerlund M., Sontrop J., Zackrisson S. Psychosocial factors and attendance at a population-based mammography screening program in a cohort of Swedish women. BMC Women’s Health. 2014;14(1):33. doi: 10.1186/1472-6874-14-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lagerlund M., Sparén P., Thurfjell E., Ekbom A., Lambe M. Predictors of non-attendance in a population-based mammography screening programme; socio-demographic factors and aspects of health behaviour. Eur J Cancer Prev. 2000;9(1):25–33. doi: 10.1097/00008469-200002000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Ludvigsson J.F., Svedberg P., Olén O., Bruze G., Neovius M. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol. 2019;34(4):423–437. doi: 10.1007/s10654-019-00511-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ludvigsson J.F., Almqvist C., Bonamy A.K., Ljung R., Michaëlsson K., Neovius M., Stephansson O., Ye W. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol. 2016;31(2):125–136. doi: 10.1007/s10654-016-0117-y. [DOI] [PubMed] [Google Scholar]
- 16.Palmelius S. Det statistiska registrets framställning och kvalietet - geografidatabasen [Rendering and quality of the statistical register - Geodatabase] 2019. https://www.scb.se/contentassets/222e45b854a242aa899111ce753d1a52/ov0100_dokstar_2019_190923.pdf SCB.
- 17.Swedish Association of Local Authorities and Regions . 2016. Classification of Swedish municipalities 2017. [Stockholm] [Google Scholar]
- 18.Alfonzo E., Andersson Ellström A., Nemes S., Strander B. Effect of fee on cervical cancer screening attendance – ScreenFee, a Swedish population-based randomised trial. PloS One. 2016;11(3) doi: 10.1371/journal.pone.0150888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allgood P.C., Maroni R., Hudson S., Offman J., Turnbull A.E., Peacock L., Steel J., Kirby G., Ingram C.E., Somers J., Fuller C., Threlfall A.G., Gabe R., Maxwell A.J., Patnick J., Duffy S.W. Effect of second timed appointments for non-attenders of breast cancer screening in England: a randomised controlled trial. Lancet Oncol. 2017;18(7):972–980. doi: 10.1016/S1470-2045(17)30340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Törnberg S., Lidbrink E., Henriksson R. Avgiftsfri mammografi får fler att komma till undersökning. Studie i Stockholms län visar på bra effekt i socioekonomiskt svaga områden [Free of charge mammography gets more people to the examination. Study in Stockholm County shows good efficacy in socioeconomically disadvantaged areas] Lakartidningen. 2014;111(7):278–281. [PubMed] [Google Scholar]
- 21.Broberg G., Wang J., Ostberg A.L., Adolfsson A., Nemes S., Sparen P., Strander B. Socio-economic and demographic determinants affecting participation in the Swedish cervical screening program: a population-based case-control study. PloS One. 2018;13(1) doi: 10.1371/journal.pone.0190171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perry N., Broeders M., de Wolf C., Törnberg S., Holland R., von Karsa L. European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition – summary document. Ann Oncol : official journal of the European Society for Medical Oncology / ESMO. 2008;19(4):614–622. doi: 10.1093/annonc/mdm481. [DOI] [PubMed] [Google Scholar]
- 23.Abdoli G., Bottai M., Sandelin K., Moradi T. Breast cancer diagnosis and mortality by tumor stage and migration background in a nationwide cohort study in Sweden. Breast. 2017;31:57–65. doi: 10.1016/j.breast.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Eaker S., Halmin M., Bellocco R., Bergkvist L., Ahlgren J., Holmberg L. Social differences in breast cancer survival in relation to patient management within a National Health Care System (Sweden) Int J Cancer. 2009;124(1):180–187. doi: 10.1002/ijc.23875. [DOI] [PubMed] [Google Scholar]
- 25.Halmin M., Bellocco R., Lagerlund M., Karlsson P., Tejler G., Lambe M. Long-term inequalities in breast cancer survival – a ten year follow-up study of patients managed within a National Health Care System (Sweden) Acta Oncol. 2008;47(2):216–224. doi: 10.1080/02841860701769768. doi:787077799 [pii] 10.1080/02841860701769768. [DOI] [PubMed] [Google Scholar]
- 26.Aarts M.J., Voogd A.C., Duijm L.E., Coebergh J.W., Louwman W.J. Socioeconomic inequalities in attending the mass screening for breast cancer in the south of The Netherlands – associations with stage at diagnosis and survival. Breast Cancer Res Treat. 2011;128(2):517–525. doi: 10.1007/s10549-011-1363-z. [DOI] [PubMed] [Google Scholar]
- 27.Schueler K.M., Chu P.W., Smith-Bindman R. Factors associated with mammography utilization: a systematic quantitative review of the literature. J Womens Health (Larchmt) 2008;17(9):1477–1498. doi: 10.1089/jwh.2007.0603. [DOI] [PubMed] [Google Scholar]
- 28.Kristiansen M., Thorsted B.L., Krasnik A., von Euler-Chelpin M. Participation in mammography screening among migrants and non-migrants in Denmark. Acta Oncol. 2012;51(1):28–36. doi: 10.3109/0284186x.2011.626447. [DOI] [PubMed] [Google Scholar]
- 29.Smith D., Thomson K., Bambra C., Todd A. The breast cancer paradox: a systematic review of the association between area-level deprivation and breast cancer screening uptake in Europe. Cancer Epidemiol. 2019;60:77–85. doi: 10.1016/j.canep.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walsh B., Silles M., O'Neill C. The importance of socio-economic variables in cancer screening participation: a comparison between population-based and opportunistic screening in the EU-15. Health Pol. 2011;101(3):269–276. doi: 10.1016/j.healthpol.2011.02.001. [DOI] [PubMed] [Google Scholar]