Highlights
-
•
Mathematical model capabilities to explore complex systems now enable priority-setting to consider local resource constraints.
-
•
Common objectives of model-based analyses incorporating constraints are to assess real-world feasibility or allocate resources efficiently.
-
•
Constraints may be incorporated via (i) model-based estimation; (ii) linkage of mathematical and health system models; or (iii) optimisation.
-
•
Models can then project constrained intervention effects and costs and resource requirement s for delivering interventions at full scale.
-
•
'Health system constraints' should be systematically defined for routine operationalisation in model-based priority-setting.
Keywords: Health system, Constraints, Mathematical models, Infectious disease, Systematic review
Abstract
Priority setting for infectious disease control is increasingly concerned with physical input constraints and other real-world restrictions on implementation and on the decision process. These health system constraints determine the ‘feasibility’ of interventions and hence impact. However, considering them within mathematical models places additional demands on model structure and relies on data availability. This review aims to provide an overview of published methods for considering constraints in mathematical models of infectious disease.
We systematically searched the literature to identify studies employing dynamic transmission models to assess interventions in any infectious disease and geographical area that included non-financial constraints to implementation. Information was extracted on the types of constraints considered and how these were identified and characterised, as well as on the model structures and techniques for incorporating the constraints.
A total of 36 studies were retained for analysis. While most dynamic transmission models identified were deterministic compartmental models, stochastic models and agent-based simulations were also successfully used for assessing the effects of non-financial constraints on priority setting. Studies aimed to assess reductions in intervention coverage (and programme costs) as a result of constraints preventing successful roll-out and scale-up, and/or to calculate costs and resources needed to relax these constraints and achieve desired coverage levels. We identified three approaches for incorporating constraints within the analyses: (i) estimation within the disease transmission model; (ii) linking disease transmission and health system models; (iii) optimising under constraints (other than the budget).
The review highlighted the viability of expanding model-based priority setting to consider health system constraints. We show strengths and limitations in current approaches to identify and quantify locally-relevant constraints, ranging from simple assumptions to structured elicitation and operational models. Overall, there is a clear need for transparency in the way feasibility is defined as a decision criteria for its systematic operationalisation within models.
1. Introduction
The launch of the Sustainable Development Goals, with their focus on Universal Health Coverage, has accelerated a shift in priority setting for health care interventions. The traditional focus on comparing the incremental cost-effectiveness of finite sets of interventions is being complemented with ranking and optimisation exercises across diseases and, in some cases, the whole health sector. Examples include defining essential benefits packages, disease-specific strategic plans and national health insurance coverage schemes for expanding access to health care and avoiding catastrophic costs for patients and households (Jamison et al., 2018). At the same time, it is being increasingly recognised that priority setting should take into account a range of non-financial constraints in any given setting and intervention area (Vassall et al., 2016) while considering multiple objectives alongside efficiency and effectiveness, such as equity and social protection.
Traditionally, the health care budget is the sole constraint considered in resource allocation models. However, policy-makers contend with several other constraints affecting feasibility of implementation, both on the supply (health system) and demand (patient) sides, when selecting interventions. These constraints may limit the pace of intervention scale-up (e.g. human resources scarcity in the short run); may be insurmountable even with increased resourcing (e.g. prioritisation of specific population groups, or an ethical obligation to provide treatment to all those in need); or may incur costs that are not observable when interventions are tested in research settings. Failure to account for such setting- and intervention-specific influences on the priority setting process itself and on the implementation of the resulting recommendations can result in unfeasible health interventions being recommended and, ultimately, in evidence being disregarded by decision-makers (Hauck et al., 2016; Mikkelsen et al., 2017).
Mathematical models exploring complex systems have made a vital contribution to advancements in priority setting for infectious diseases. The recent development of user-friendly dynamic transmission models to prioritise new health technologies for infectious disease control increasingly allows policy-makers to account for setting-specific variations in factors such as epidemiological characteristics and input types and prices (Houben et al., 2016; Lubell et al., 2008; Stegmuller et al., 2017). Moreover, model-based priority setting may allow analysts to consider other country- and intervention-specific non-financial constraints that bind resource allocation decisions. For example, while transmission modelling analyses recommend intensified screening of all clinic patients for reaching the End TB Strategy targets in South Africa, this intervention is highly human resource (HR) intensive and increases the use of diagnostics downstream in the tuberculosis (TB) care cascade (Menzies et al., 2016). Thus, it might be a sub-optimal option compared to others in the TB portfolio when constraints on these inputs are taken into account. In this example, the effect of the constraints on intervention impact is parametrised in the model through changes in the rates of transitions between different compartments or states (the example of human resource constrains for TB care in South Africa is illustrated graphically in the Supplementary File 1 (Fig. 1A)). However, this may not be the only existing approach to the inclusion of constraints in these analyses.
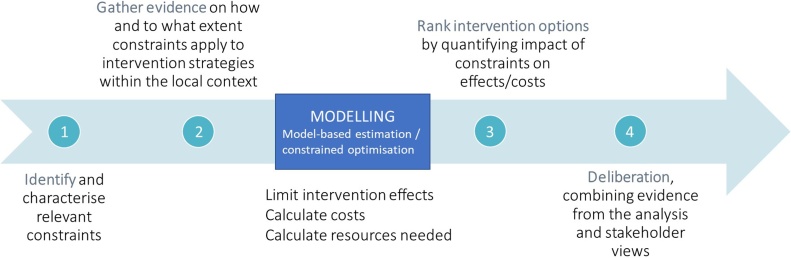
Fig. 1.
Framework for incorporating health system constraints in priority setting.
The aim of this review is to establish how locally relevant non-financial constraints have been incorporated in model-based impact and cost-effectiveness analyses of infectious disease control interventions. In particular, we describe the constraints considered and how these were characterised and quantified in the models. Ultimately, we aim to discuss suitable model structures and techniques for implementing the constraints within them.
2. Materials and methods
A systematic search of the published literature was conducted to identify studies published before November 2020, that employ dynamic transmission models to assess infection control interventions in any disease and geographical area and that consider non-financial constraints to implementation. Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement and checklist (Liberati et al., 2009).
2.1. Search strategy
The MEDLINE and Embase databases were searched via the OvidSP platform for English language, full text studies on human subjects. The Scopus database was also searched without imposing any limits. The search strategy combined keywords on infectious diseases, dynamic transmission modelling, economic evaluation, priority setting and health systems research, including constraints and feasibility of health interventions. The following Medical Subject Heading (MeSH) terms were ‘exploded’ in MEDLINE and Embase: “Infectious Disease Transmission”, “Public Health Systems Research”, “Systems Analysis”, “Theoretical Models”, “Economic Models”, “Decision Support Techniques”. The full search strategy for each database and number of records retrieved (with and without limits, where applicable) are presented in Supplementary File 1B. A hand search of the reference lists of retained articles was also conducted to identify other potentially relevant literature.
2.2. Screening, data extraction and analysis
Search results were exported to EndNote (v. × 8) to eliminate duplicates. The abstract and titles of all unique records were then screened and articles were further excluded based on the following criteria: (i) language other than English; (ii) topic not related to human health; (iii) no reference to the application of health system constraints and infectious disease models; (iv) ineligible article type (clinical and/or pragmatic trials, feasibility or pilot or demonstration studies, editorials, conference proceedings, comments, letters and notes). The full texts of remaining articles were then reviewed and retained if they made reference to a formal method of applying non-financial constraints in priority setting using a mathematical model of infectious disease transmission. Articles using ‘static’ mathematical models or other model types and those that did not consider any constraints other than the budget or financial constraint were discarded.
Data was extracted from the retained records in the following categories: geographical and disease area of interest, type of intervention and level of the health system at which implementation occurred, transmission model structure, model population and projection timeframe, presence and type of economic analysis (including optimisation under a budget constraint), demand- and supply-side non-financial constraints considered as well as methods for identifying and quantifying the constraints, aim of the modelling exercise and formal method of incorporating the constraints in the analysis. The data was summarised using descriptive statistics and a thematic analysis of the contents of the articles was carried out to answer the study question.
For characterising how health system constraints were incorporated in models we drew on the work of Vassall and colleagues, who distinguished between proximal constraints, such as HR and pharmaceutical shortages, and distal constraints, such as cultural norms, values and regulations (Vassall et al., 2016). We then described how these constraints were analysed at different stages in the priority setting process using the framework shown in Fig. 1. Steps 1 and 2 refer to the identification and characterisation of health system constraints that apply to the intervention of interest in the specific context; steps 3 and 4 refer to the assessment of the constraints’ impact on intervention effects and/or costs, and to how this evidence is used in the deliberation process, highlighting how the views of stakeholders may still play a role alongside the quantitative evidence from modelling.
3. Results
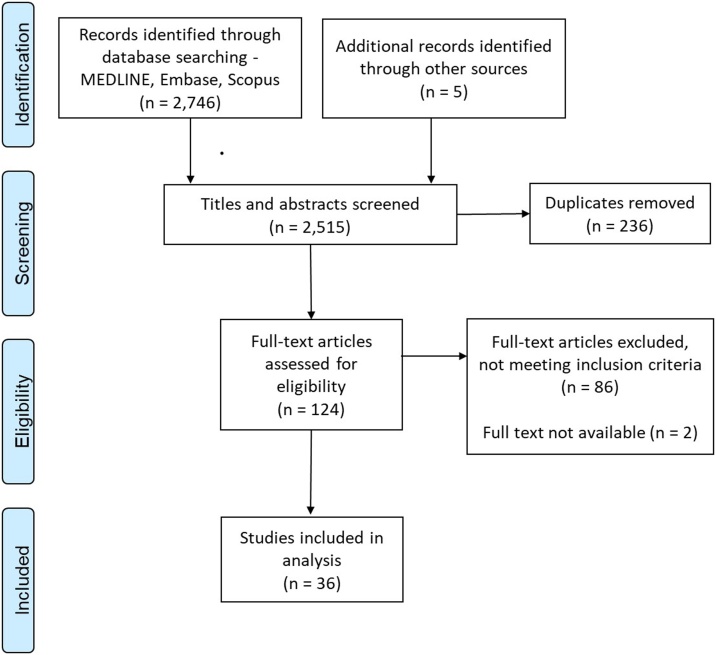
We identified 2751 unique citations, of which approximately one in 20 were eligible for full text screening. The PRISMA flow chart with details of the study screening and selection process is shown in Fig. 2.
Fig. 2.
Flow chart of screening and selection process.
After the selection process was completed, 36 studies were retained for analysis. The study characteristics, aims and model structures of all selected papers are summarised in Table 1. Approximately one third of the studies focused on a single country, predominantly in the low- and middle-income group, while eight studies were global in focus and a further three regional (two from sub-Saharan Africa and one from South-East Asia). Another seven studies, mostly from high-income settings, looked at one single municipality or health facility within a country. The disease area most represented in the literature was pandemic influenza, followed by human immunodeficiency virus (HIV) and TB.
Table 1.
Study characteristics and mathematical models structure.
| Lead author (year) | Setting | Disease area | Intervention | Level of health system | Study aim | Transmission model structure | Economic analysis |
|---|---|---|---|---|---|---|---|
| Adisasmito et al. (2015) | Local - Bali, Indonesia | Influenza | Pandemic influenza case management capabilities strengthening | Decentralised | Simulate influenza spread at the district level given existing resource gaps to inform preparedness planning | Density-dependent deterministic compartmental model (SEAIR) | – |
| Alistar et al. (2013) | Country - not specified | HIV | Multiple, user-defined HIV control interventions | National | Develop a model to guide setting-specific resource allocation across interventions along the HIV cascade | Frequency-dependent deterministic compartmental model (HIV disease stages and treatment status) | Cost-effectiveness analysis |
| Anderson et al. (2014, 2018) | Country - Kenya | HIV | Combination prevention interventions | Decentralised | Model the effect of prioritising key population and of short-term funding cycles on HIV prevention | Frequency-dependent deterministic compartmental model (susceptible, acute-, latent infection, pre-AIDS, AIDS) | Cost analysis |
| Bärnighausen et al. (2016) | Country - South Africa | HIV | Treatment as prevention (TaSP) | National | Model the effects of TaSP on universal ART coverage | Frequency-dependent deterministic compartmental model (susceptible, HIV infection stages) | – |
| Barker et al. (2017) | Regional - sub-Saharan Africa | HIV | ART differentiated care models | National | Model efficiency gains from different service delivery options | Frequency-dependent deterministic compartmental model (AIDS Impact Model, Estimation Projection Package) | Cost analysis |
| Bottcher et al. (2015) | Global | Influenza | Epidemic preparedness | National | Investigate the effects of disease-induced resource constraints on epidemic spreading | Density-dependent deterministic compartmental model (bSIS, recovery rate mediated by resources availability) | – |
| Bozzani et al. (2018, 2020), Sumner et al. (2019) | Country - South Africa | TB | Changes to screening and diagnostic algorithm | National | Develop a pragmatic approach for empirical estimation of health system constraints from routine data to parametrise models | Density-dependent deterministic compartmental model (susceptible, latent infection, active disease) | Cost and cost-effectiveness analysis |
| Chen et al. (2019) | Country – not specified | Sexually transmitted infection epidemic | Epidemic control | National | Model the effects of resource availability on rate of infection | Frequency-dependent deterministic compartmental model (SIS, recovery rate mediated by resources availability) | – |
| Cruz-Aponte et al. (2011) | Global | Influenza | Flu vaccination campaign during outbreak | National | Develop an accurate model of vaccine stockpiles for epidemic preparedness | Density-dependent deterministic compartmental model (SIR-like model including vaccines supply and numbers vaccinated) | – |
| Curran et al. (2016) | Global | General epidemic outbreak | Surge capacity planning | National | Develop a conceptual framework for integrating big data analytics with simulation, to provide real-time analysis of health system capacity during epidemics | Density-dependent deterministic compartmental model (SEIR) | – |
| Dalgiç et al. (2017) | Local - Seattle, US | Influenza | Flu vaccination campaign during outbreak | National | Compare age-specific vaccination strategies derived from agent-based simulation and from a deterministic compartmental model | Agent-based simulation and density-dependent deterministic compartmental model (SEIR), enhanced with mesh-adaptive direct search (MADS) algorithm to iteratively improve intervention strategies | Cost analysis |
| Ferrer et al. (2014) | Local - France | All-cause ICU visits | Strategies to cope with nurses shortages | Service | Explore impact of management strategies against nurse shortages on pathogen transmission within the ICU | Agent-based simulation | – |
| Hecht and Gandhi (2008) | Global | HIV | AIDS vaccination | National | Model determinants of demand, uptake dynamics and potential revenues from vaccine candidates | Discrete deterministic linear predictive model (vaccinated are a fraction of population in need dynamically estimated based on numbers of susceptibles who have access given constraints) | Cost analysis |
| Hontelez et al. (2016) | Regional - sub-Saharan Africa | HIV | ART scale-up (changing eligibility thresholds) | National | Model resource requirements to achieve ART coverage targets | Agent-based simulation | Cost-effectiveness analysis |
| Krumkamp et al. (2011) | Country - Thailand | Influenza | Epidemic preparedness | Decentralised | Simulate characteristics of an influenza outbreak and identify resource needs and gaps | Density-dependent deterministic compartmental model (SEAIR) | – |
| Langley et al., 2014; Lin et al. (2011) | Country - Tanzania | TB | New diagnostic technologies for parasitic disease | National | Model intervention effects on operational performance of the health system to accurately assess impact and cost-effectiveness | Deterministic compartmental model (SIR-like). Active diseases states of the model are expanded to include pathway from onset to diagnosis and linkage to treatment from operational model | Cost-effectiveness analysis |
| Marks et al. (2017) | Global | Yaws | Eradication campaign (mass azythromycin treatment followed by case finding and targeted treatment) | National | Determine the feasibility and optimal strategy for yaws eradication | Stochastic compartmental model (Markov model with susceptibles and primary, latent and secondary infection) | – |
| Martin et al. (2015a, b) | Local - New York state, US | HIV | Policy change to increase HIV testing and linkage to care | Decentralised | Assess health outcomes and health system resources needs under different policy implementation scenarios | Stock and flow model with transmission rates that vary by HIV infection stage and ART status | – |
| Martin et al. (2011) | Country - UK | HCV | Antiviral treatment among injecting drug users | National | Assess optimal treatment strategy for different economic and policy objectives | Frequency-dependent deterministic compartmental model (susceptible, chronically infected, treated) | Cost analysis |
| McKay et al. (2018) | Local - US | HIV | HIV counselling | Service | Describe the relationship between HR, intervention delivery and health outcomes by simulating different HR availability scenarios and observing effects on the other variables | Agent-based simulation | – |
| Peak et al. (2020) | Country – not specified | SARS-CoV-2 | Epidemic preparedness | National | Compare effectiveness of individual quarantine and active monitoring at reducing effective reproductive number to below 1, under different feasibility scenarios | Density-dependent deterministic compartmental model (bSIS, recovery rate mediated by resources availability) | – |
| Putthasri et al. (2009) | Country - Thailand | Influenza | Modest pandemic mitigation | Decentralised | Define and quantify pandemic preparedness resources at the provincial level and estimate gaps under different scenarios | Density-dependent deterministic compartmental model | – |
| Rudge et al. (2012) | Regional - South-East Asia | Influenza | Epidemic preparedness | Decentralised | Estimate and compare resource gaps and their potential consequences in six countries | Density-dependent deterministic compartmental model (SEAIR) | – |
| Salomon et al. (2006) | Global | TB | Introduction of short-course regiments using new drugs | National | Examine the expected benefits of shorter drug regimens | Deterministic compartmental model (SIR-like model with treatment compartments) | – |
| Sébille and Valleron (1997) | Global | Nosocomial bacterial infection | Staff handwashing compliance to prevent transmission from patient contacts | Service | Develop a simulation of resistant pathogens spread in the hospital unit | Agent-based simulation | – |
| Shattock et al. (2016) | Country - Zambia | HIV | Multiple (model guides priority setting across the HIV cascade) | National | Assess time-varying optimal resource allocations for fixed and variable annual budgets and for various time horizons for measuring outcomes | Frequency-dependent deterministic compartmental model | – |
| Shim et al. (2011) | Country - US | Influenza | Seasonal influenza vaccination | National | Investigate age-dependent optimal vaccine distribution against influenza H1N1 influenza from the individual and population perspectives | Density-dependent deterministic compartmental model (SLIR) | Cost analysis |
| Stenberg et al. (2017) | Global | Health-related SDG targets | Multiple - 187 interventions targeting health-related SDGs and health systems strengthening | National | Estimate resource needs for strengthening health systems to reach universal health coverage in the SDG era | One Health tool, incorporating the interlinked epidemiological reference models for various disease areas (AIM, TIME, LiST) | Cost analysis |
| Stopard et al. (2019) | Country – provinces across Tanzania (Benin, South Africa limited implementation) | HIV | Multiple - behavioural change communication, pre-exposure prophylaxis, voluntary medical male circumcision and universal test-and-treat services | National | To investigate the impact of ‘real-world’ constraints on the resource allocation and possible health gains nationally | Frequency-dependent deterministic compartmental model | Optimisation |
| Verma et al. (2020) | Country – India | SARS-CoV-2 | Treatment | National | Forecast need for hospital resources and assess surge capacity of health system | Density-dependent deterministic compartmental model (modified SEIR model with age-specific mixing patterns) | – |
| Zhang et al. (2020) | Country – not specified | Generic epidemic outbreak | Vaccination | National | Assess optimal vaccination policy in a resource-limited environment | Density dependent deterministic compartmental model (SIR with vaccination compartment) | – |
AIM: AIDS Impact Model; AIDS: Acquired Immunodeficiency Syndrome; ART: Anti-Retroviral Therapy; CEA: Cost-Effectiveness Analysis; FTE: Full-Time Equivalent; HCV: Hepatitis C Virrus; HR: Human Resources; ICU: Intensive Care Unit; LiST: Lives Saved Tool; QALY: Quality-Adjusted Life-Years; SDG: Sustainable Development Goals.
3.1. Model structures
The majority of included studies used deterministic compartmental models of disease transmission, as shown in Table 1. However, all mathematical model structures commonly used to characterise the epidemiology of disease transmission were represented in the review, including agent-based simulations and stochastic models. Choice of model structure was determined by the characteristics of the disease, intervention and setting under study, rather than by the characteristics and objectives of the constrained analysis. For example, agent-based models were best suited for investigating nosocomial pathogen transmission (Ferrer et al., 2014; Sébille and Valleron, 1997), while stochastic models were used for cohort analyses assessing the impact of eradication campaigns (Marks et al., 2015) or measures to contain SARS-Cov-2 outbreaks (Peak et al., 2020). The structural decision may have been different if the focus had been the constrained analysis. For example, a compartmental model where the compartments reflect different levels of the health system in addition to disease progression and transmission could improve the analysis of human resource constraints. More details on the model structures represented are provided in the Supplementary File 1C.
3.2. Health system constraints and policy objectives
The types of health system constraints considered in the models and the objectives of the constrained analyses are described in Table 2. These ranged from constraints on service delivery inputs, mostly human resources and supplies, but also capital constraints such as equipment and hospital beds, to constraints on the demand for services (e.g. vaccine hesitancy) and other constraints on decision-making that affect the resource allocation process.
Table 2.
Constrained analyses characteristics.
| Lead author (year) | Constrained analysis objective | Non-financial constraints | Constraints identification | Constraints parametrisation and data sources | Approach for modelling constraints | Constraints implementation, details | Scenarios description |
|---|---|---|---|---|---|---|---|
| Adisasmito et al. (2015) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | HR, bed space, equipment, pharmaceutical supplies | Literature | Literature and secondary data analysis (AsiaFluCap survey) | Transmission model-based estimation - Calculate resource requirements | Transmission model linked to resource calculator to estimate requirements during outbreak. Model calculates depletion rate of resources based on average requirements to treat one case, estimated through a mix of data from literature and routine sources. Needs are compared to capacity, estimated through a survey administered as part of AsiaFluCap project | Two scenarios with different hospitalization and mortality rates |
| Alistar et al. (2013) | Efficient resource allocation - maximising impact given health system constraints | Political constraint on decision-making | Assumption | Assumption | Transmission model-based estimation - Limit effects and calculate costs along the cascade | REACH is an Excel-based user-friendly model helping policy makers allocate resources across different HIV control interventions. It comprises transmission dynamics and optimisation function. Optimisation done under budget constraint only, but political/social/ethical constraints on allocation of resources can be specified in the user interface. Outputs sheet includes estimates of health care resources needed to support the allocations | – |
| Anderson et al. (2014, 2018) | Feasibility assessment and efficient resource allocation - produce realistic intervention impact estimates and maximise impact given health system constraints | Political constraint on decision-making, demand side barriers to access | Assumption | Assumption | Transmission model-based estimation - Limit effects and calculate costs along the cascade | Constraints determine the way funds are allocated to key populations (MSM, other men, FSW, other women), geographical areas and throughout 5-year funding cycles (fully flexible, frontloaded, constant or back-loaded). Intervention choice optimised under the different resulting budget constraints. Constraints to implementation also parametrised in the form of uptake limits to certain intervention components | For key populations and districts (paper 1), all possible intervention scenarios compared by constructing health production functions for a given cost. For spending cycle (paper 2), 5 scenarios: 2 with complete spending flexibility (one of which with intervention change at 10 years), choices optimised over 30-year period; 3 with front-loaded, equal and back-loaded funding cycles, respectively, and choices optimised over each 5-year cycle |
| Bärnighausen et al. (2016) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | HR | Assumption | Literature | Transmission model-based estimation - Limit effects and calculate resource requirements along the cascade | Given current HR supply, number of patients treated is computed assuming fixed ratios for each cadre to patient. Model projects the impact of reallocating scarce HR to varying patient distributions in the different HIV disease stages and can estimate potential shortages | 200 scenarios varying assumptions around HIV transmission probabilities, ART effect, retention and adherence. Two sets of constraints scenarios: one where allocation of HR is proportional to number of patients in TaSP and standard ART (treatment for advanced disease stages) pools, respectively; one where more HR allocated to pool with patients at more advanced disease stages |
| Barker et al. (2017) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | HR | Assumption | Secondary analysis of data from Tanzania and Mozambique on time spent by facility health workers delivering ART | Transmission model-based estimation - Calculate resource requirements | Model estimates total facility staff FTE needed for different ART differentiated care models, based on previous estimates of time spent delivering ART in Africa. An analysis of constraints is not presented because differentiated care models are expected to lead to cost and HR savings | – |
| Bottcher et al. (2015) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | Political constraint on decision-making, recurrent supplies | Assumption | Assumption | Transmission model-based estimation - Limit intervention effects | Model projects a global budget that increases by one unit with each additional healthy individual per unit of time and partially constrains recovery when available budget is insufficient for covering 'costs of healing' | – |
| Bozzani et al. (2018, 2020), Sumner et al. (2019) | Feasibility assessment and efficient resource allocation - produce realistic intervention impact estimates and maximise impact given health system constraints | HR, diagnostic equipment | Expert opinion | Secondary data collection from routine sources including district health information system (DHIS) and other Department of Health and Nursing Council records | Transmission model-based estimation - Limit effects and calculate resource requirements along the cascade | Unit costs and staff FTE to deliver different services are attached to model outputs to limit intervention effects once threshold of available resources is exceeded. Diagnostic constraint parametrised as maximum ratio of tests to TB notifications. Costs of 'relaxing' the constraints to achieve target coverage is calculated. | 3 scenarios (least limiting, medium and most limiting) considered for each constraint (budget, diagnostic and HR), respectively, based on projections of future resource availability |
| Chen et al. (2019) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | Resources that are necessary to contain an epidemic (not specified) | Assumption | Assumption | Transmission model-based estimation - Limit intervention effects | A value Rc, representing the level of resources in the system, is identified, whereby the epidemic can be effectively contained. If R < Rc the disease becomes widespread, recovery rate varies with time depending on average amount of resources that each infected individual receives | Scenarios explored with different levels of health system resourcing |
| Cruz-Aponte et al. (2011) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | Vaccine stockouts | Assumption | Assumption | Transmission model-based estimation - Limit intervention effects | Vaccine administration limited by daily maximum number. Vaccination campaign ends a) after some prescribed duration of time; or b) when stockpile is depleted. Results are compared with those from alternative model that ends campaign when target proportion of population is vaccinated. | Three scenarios varying the number of vaccines administered in a time period (56-, 28-, and 3-day campaign with different daily administration limits) |
| Curran et al. (2016) | Efficient resource allocation - maximising impact given health system constraints | HR, supplies and infrastructure | Group model building - System dynamics modelling techniques | Assumption | Transmission and system dynamics models linkage - Limit effects system-wide | The paper outlines possible ways of integrating transmission dynamics modelling with data generated from population surveys and sentinel surveillance and with system dynamics models to predict resource capacity during epidemic outbreaks and assist with resource allocation based on predicted pathogen spread | Multiple scenarios with varying disease transmission rates and health system capacity can be analysed |
| Dalgiç et al. (2017) | Efficient resource allocation - maximising impact given health system constraints | Vaccine stockouts | Assumption | Assumption | Constrained optimisation - Limit intervention effects | Optimise vaccine allocation in different age groups subject to constrained availability. Different objectives (minimise total costs, total infections, total deaths, total years of life lost) | Several vaccine coverage and delayed response time scenarios |
| Ferrer et al. (2014) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | HR | Assumption | Primary data collection at 5 ICUs on bed occupancy and staffing conditions | Transmission model-based estimation - Limit intervention effects | Model includes estimates of nurses' contact time with patients, which has an effect on pathogen spread. Daily rate of nurse absenteeism varied to adopt a fixed value between 10−40% and different coping mechanisms modelled | Systematic analysis of pathogen dissemination under different scenarios of pathogens circulating, level of nurses shortage and shortage management strategy |
| Hecht and Gandhi (2008) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | Political constraint on decision-making, demand side barriers to access | Literature and expert opinion | Assumptions based on expert consultation | Transmission model-based estimation - Limit intervention effects | Global demand for vaccine forecast by adding up demand estimates for individual country profiles | Four vaccine profile scenarios based on variations in efficacy, duration of protection and cost |
| Hontelez et al. (2016) | Efficient resource allocation - maximising impact given health system constraints | HR, infrastructure, demand-side barriers to access | Assumption | Assumptions made on effects of constraints on ART coverage. Costs of one-off investment needed to relax constraints calculated from routine AIDS spending reports | Transmission model-based estimation - Limit effects and calculate costs system-wide | Model calculates total investment needs, population health gains and cost-effectiveness of scaling-up new ART eligibility guidelines, including removal of health system constraints | Scenarios reflecting pessimistic, realistic and optimistic future health system developments, in which constraints apply to different extents |
| Krumkamp et al. (2011) | Efficient resource allocation - maximising impact given health system constraints | HR, pharmaceuticals supplies and other consumables | Assumption | Expert opinion and primary data collection (AsiaFluCap survey) | Transmission model-based estimation - Limit effects and calculate resource requirements along the cascade | Model constrains epidemic containment based on availability of resources and calculates resource depletion per hospital case. Resource usage data and impact of constraints estimated from a mix of survey data and expert opinion | Different epidemic control strategies modelled (antivirals stockpiling for critical cases, contact reductions) |
| Langley et al. (2014), Lin et al. (2011) | Efficient resource allocation - maximising impact given health system constraints | HR, diagnostic pathway bottlenecks, demand-side barriers to access | Group model building - Operational modelling techniques | Primary data collected from two diagnostic centres in Tanzania and calibrated using National TB programme reports | Transmission and operational models linkage - Limit intervention effects | Operational model outputs used to parametrise transmission model and vice versa. Operational component uses discrete-event simulation approach to model patient and sputum sample pathways | Different diagnostic algorithms modelled |
| Marks et al. (2017) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | Demand-side barriers to access | Assumption | Assumption | Transmission model-based estimation - Limit intervention effects | Eradication modelled under a range of plausible targeted treatment coverage estimates (65 %–95 %). Mass treatment compliance modelled as a random non-systematic process where every patient has the same, independent likelihood of receiving treatment | 3 transmission scenarios modelled (low, medium, high) based on literature and expert opinion |
| Martin et al. (2015a, b) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | Implementation' constraints, demand-side barriers to access | Group model building - System dynamics modelling techniques | Literature and expert opinion | Transmission and system dynamics models linkage - Limit intervention effects | Scenario analysis where the flow of patients along the HIV testing and care cascade is determined by different sets of assumptions regarding policy implementation. These were defined in consultation with experts and based on the literature, by developing a system dynamics model that assesses the impact and relationships of different policy components | 3 policy 'implementation' scenarios (low, high, perfect) and 3 testing policy scenarios (annual, five-year and no repeat offer of testing) combined to generate 9 unique combinations of policy conditions in addition to the base case |
| Martin et al. (2011) | Efficient resource allocation - maximising impact given health system constraints | Political constraint on decision-making | Assumption | Assumption | Constrained optimisation - Limit effects and calculate costs along the cascade | Optimal treatment strategy for HCV is examined under different economic and policy objectives: 1) minimise costs and QALY loss; 2) minimise prevalence; 3) minimise costs and QALY loss while achieving 20 % time prevalence reduction; 4) minimise costs while achieving 20 % time prevalence reduction | Analysis is repeated for a combination of annual budget constraints and two HCV baseline prevalences (30 % and 45 %) |
| McKay et al. (2018) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | HR | Assumption | Model parametrised with trial and implementation studies data and informed by published organizational and intervention sustainability models | Transmission model-based estimation - Limit effects and calculate resource requirements along the cascade | Model predicts the level of preventive services a health agency can provide given different combinations of i) staff positions; ii) turnover rates; iii) timing in training. | N/A |
| Peak et al. (2020) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | Barriers to effective contact tracing and quarantine interventions, including untrained monitoring of symptoms | Assumption | Assumption | Transmission model-based estimation - Limit intervention effects | R0 is estimated based on the implementation of quarantine and active monitoring in high- vs low-feasibility settings | Analysis compares a high- (90 % contacts traced and quarantined or monitored, reducing infectiousness by up to 90 %) and a low-feasibility setting (delays in locating contacts, imperfect quarantine) |
| Putthasri et al. (2009) | Efficient resource allocation - maximising impact given health system constraints | HR, supplies and infrastructure | Expert opinion | Expert opinion | Transmission model-based estimation - Calculate resource requirements | Actual and projected resources per case multiplied by the number of case-patients estimated by previous modelling exercises under different scenarios. Resource gaps estimated at the provincial level | 3 epidemic (human-to-human transmission) scenarios analysed, with specific numbers of index cases and contacts: 1) from case-patients to caregivers; 2) localised clusters; 3) transmission resulting in substantial number of cases |
| Rudge et al. (2012) | Feasibility assessment and efficient resource allocation - produce realistic intervention impact estimates and maximise impact given health system constraints | HR, bed space, equipment, pharmaceutical supplies | Multi-criteria decision analysis - Delphi consensus process with a panel of 24 experts integrated with literature review | Primary data collection at health facilities to enumerate available resources. Gaps estimated based on literature on resource needs | Transmission model-based estimation - Calculate resource requirements | Available quantities of resources estimated through a survey sent out to hospitals, district health offices and ministries of health. Additional model parameters describing clinical pathway of infected individuals, conditional upon availability of resources | Model runs: i) available resources; ii) unlimited resources (to calculate gaps and compare with availability data from survey) |
| Salomon et al. (2006) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | HR, infrastructure | Assumption | Assumption | Transmission model-based estimation - Limit intervention effects | Constraints not explicitly modelled, but scenarios are analysed where it is assumed that the intervention reduces constraints to case detection, thus improving case detection rates | Scenarios were modelled with varying assumptions about case detection coverage (including one where constraints are relaxed), cure rates and DOTS scale-up |
| Sébille and Valleron (1997) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | Pharmaceutical supplies, political constraint on decision-making | Assumption | Assumption | Transmission model-based estimation - Limit intervention effects | Scenarios with different risk of patient-to-staff transmission based on whether procurement of two essential antibiotics is simultaneous (both available), sequential (only one available at a given time, then the other) or a mix of the two | Software allows for different assumptions to be specified before running simulations (e.g. drug procurement policy, staff handwashing compliance) |
| Shattock et al. (2016) | Efficient resource allocation - maximising impact given health system constraints | Political constraint on decision-making | Assumption | Assumption | Transmission model-based estimation - Limit intervention effects | Time-varying optimization i.e. minimising objective function (cumulative HIV infections) associated with the budget allocation, such that: i) total programme spending equals a pre-defined budget (either constant, front-loaded etc.) at each time point; or ii) total spending across the optimisation period is equal to pre-defined budget, but total spending at each point is optimally determined | 4 optimization scenarios illustrating policy decisions where time considerations matter: 1) optimal 10-years allocation assuming baseline budget is annually available with no constraints to programme-specific allocation; 2) as in 1, but programme-specific funding cannot vary by more than 30% compared to baseline; 3) as in 1, but annual optimal allocation determined based on implementation and ethical constraints; 4) optimal 5-years allocation but cumulative new infections assessed after 5, 10 or 15 years, again within constraints |
| Shim et al. (2011) | Efficient resource allocation - maximising impact given health system constraints | Demand-side barriers to access | Assumption | Assumption | Transmission model-based estimation - Limit intervention effects | Decision to vaccinate characterised as a game, where monetary payoff for different age groups is modelled based on different individual strategies as well as on the average behaviour of the population | Two strategies modelled to calculate payoff to vaccinated and non-vaccinated: Nash and utilitarian |
| Stenberg et al. (2017) | Efficient resource allocation - maximising impact given health system constraints | HR, infrastructure, demand-side barriers to access | Assumption | Assumption | Transmission model-based estimation - Calculate intervention costs | Tracer interventions identified for each of the relevant SDGs, then gap estimated between current provision and universal coverage and country-specific programme costs multiplied by this gap. Costs estimated from the One Health Tool and from the literature. Progress towards 2030 targets adjusted by level of 'strength' of the health system (conflict, vulnerable, low-income, lower middle-income, upper middle-income) | Two financial space scenarios in each country, reflecting uncertainty around health systems' absorption capacity: i) ambitious, strengthening system towards global benchmarks and expanding coverage of full service package to 95%; ii) progress, not all SDG targets met by 2030 but improvements can be achieved by scaling up services delivered through the lower platforms |
| Stopard et al. (2019) | Efficient resource allocation - incidence minimizing | Political constraints on decision making (earmarking, externally imposed targets, minimising change to current program) | Assumption | Assumption | Transmission model-based estimation - Calculate intervention costs and impact | Constraints are modelled through initial conditions in each scenario representing minimum coverage by subgroups within the transmission model | Four scenarios of real-world constraints: 1) earmarking, where the first intervention funded would be PrEP for heterosexual women (excluding FSWs); 2) targets, where 90 % of PLHIV must receive UTT; 3) minimising change, baseline allocation represents an allocation at national level; and 4) all constriants simultaneously |
| Verma et al. (2020) | Feasibility assessment - produce realistic intervention impact estimates given health system constraints | Hospital beds, ICU beds and mechanical ventilation equipment | Assumption | Secondary data | Transmission model-based estimation - Limit effects and calculate resource requirements along the cascade | Available capacity estimated from public records, including for private sector. Capacity needs calculated based on requirements per case and turnover times from the literature. Capacity requirements during surge are based on model projections under different lockdown scenarios. Surge capacity compared to available capacity to estimate gap. | Different lockdown/social distancing scenarios |
| Zhang et al. (2020) | Efficient resource allocation - maximising impact given health system constraints | Vaccines availability | Assumption | Assumption | Constrained optimisation - Limit intervention effects | Optimise allocation of limited vaccines in order to minimise the number of infections | N/A |
AIDS: Acquired Immunodeficiency Syndrome; ART: Anti-Retroviral Therapy; FTE: Full-Time Equivalent; HCV: Hepatitis C Virrus; HR: Human Resources; ICU: Intensive Care Unit; QALY: Quality-Adjusted Life-Years; SDG: Sustainable Development Goals.
The majority of articles relied on assumptions for identifying the constraints that applied to the setting and programme area of interest (n = 25, 66 %) and for quantifying the extent to which the constraints impacted intervention effects (n = 21, 55 %). For constraints identification, other sources were stakeholder elicitation in the form of expert opinion (n = 5), system dynamics modelling (n = 3), the literature (n = 1) and multi-criteria decision analysis using Delphi consensus (n = 1). Finally, two articles by Lin, Langley and colleagues described an operational model of the TB diagnostic pathway in Tanzania to identify bottlenecks and shortages, which was ‘linked’ to a transmission model; i.e. the operational model generated estimates of programmatic variables such as prevalence of treatment default and number of diagnostic centre visits, that were then used to parametrise the transmission model (Langley et al., 2014; Lin et al., 2011). Those studies that relied on data collection for parametrising constraints impact mostly used secondary sources (n = 7) or a mix of primary data collection and routine sources or expert opinion (n = 6). For example, modelling done using the AsiaFluCap simulator identified the resources needed for pandemic influenza response through expert elicitation (Rudge et al., 2012) and estimated available quantities and resource use per patient in the study countries through a survey integrated with data from the published literature (Adisasmito et al., 2015; Krumkamp et al., 2011).
Non-financial constraints influencing health providers’ ability to deliver health services were considered in two thirds of included studies (n = 28) (Adisasmito et al., 2015; Alistar et al., 2013; Bärnighausen et al., 2016; Barker et al., 2017; Bottcher et al., 2015; Bozzani et al., 2018, 2020; Chen et al., 2019; Cruz-Aponte et al., 2011; Curran et al., 2016; Dalgiç et al., 2017; Ferrer et al., 2014; Krumkamp et al., 2011; Langley et al., 2014; Lin et al., 2011; Martin et al., 2011; McKay et al., 2018; Peak et al., 2020; Putthasri et al., 2009; Rudge et al., 2012; Salomon et al., 2006; Sébille and Valleron, 1997; Shattock et al., 2016; Stopard et al., 2019; Sumner et al., 2019; Verma et al., 2020; Zhang et al., 2020), while only two studies considered constraints to the demand for health services (Hecht and Gandhi, 2008; Shim et al., 2011), and six articles considered both demand- and supply-side factors (Anderson et al., 2014, 2018; Hontelez et al., 2016; Marks et al., 2017; Martin et al., 2015a, b; Stenberg et al., 2017). The models that exclusively include demand-side constraints both focus on vaccines: one study projected the public and private demand for an AIDS vaccine candidate under different vaccine characteristics (efficacy, duration of protection, price), performance (acceptability, compliance) and country-level profile scenarios (including political ability and motivation to implement HIV/AIDS prevention programmes) (Hecht and Gandhi, 2008); the second study subdivided model compartments based on individual decisions to vaccinate against seasonal influenza, to assess the effects of vaccine hesitancy on coverage and to derive optimal vaccine allocation across age groups under a Nash (own interest) versus a utilitarian strategy (optimal for the population) (Shim et al., 2011).
Most commonly, the analyses that focussed on limits to the supply of health services incorporated a combination of HR, capital, equipment (infrastructure, hospital beds, logistics, ventilators etc.) and supplies constraints (drugs, vaccines and diagnostic consumables). These physical input constraints are not explicitly defined in a limited number of the analyses. For example, the 3S Surge System model for outbreak capacity planning consists of broadly defined ‘staff, stuff and structure’ (Curran et al., 2016) while three studies talk about non-specific resources necessary for controlling the spread of an epidemic (Bottcher et al., 2015; Chen et al., 2019; Peak et al., 2020) and other analyses refer to generic ‘implementation’ constraints that reduce the achievable coverage of interventions (Hontelez et al., 2016; Martin et al., 2015a, b).
A second set of supply-side non-financial constraints groups are distal factors deriving from political and social values and practices that determine how budgets are allocated, what activities are considered feasible or acceptable, and broader societal policy objectives that the system can pursue. Examples of models that allow for considering these constraints include the Resource Allocation for Controlling HIV tool, which allows users to specify interventions that cannot be implemented due to social, political or ethical concerns, or that have to receive a minimum/maximum level of funding for historical or strategic reasons (Alistar et al., 2013); the Optima model, which lets users analyse different budget allocation scenarios (constant, front-loaded, rear-loaded or initially scaled-up/down then later scaled-down/up over the funding cycle) (Shattock et al., 2016); and model developed by Stopard and colleagues, that examines different constraints to the efficient allocation of resources for HIV prevention, including externally imposed targets or limited capacity to modify existing programmes (Stopard et al., 2019). One set of studies in this group considers policy constraints both on the funding cycle (varying the flexibility of spending and the time horizon over which choices are to be optimised) and on how funds are allocated across key populations and geographical areas (Anderson et al., 2014, 2018).
3.3. Modelling approaches integrating non-financial constraints
As shown in Table 2, the rationale for considering health system constraints in the modelling studies was two-fold, with studies seeking to do one, or a combination, of the following: i) carry out a feasibility assessment, by producing reaslistic estimates of intervention impact (and costs) given the constraints; ii) guide efficient priority setting, by allocating resources in a way that maximises intervention impact given the constraints. Following from these objectives, the analytical approaches for considering constraints in the modelling studies can be grouped into two categories. The first category includes constrained estimation exercises, where intervention implementation is modelled at the maximum attainable coverage given the constraints. Effects (and costs) are thus limited at the level of the specific intervention, the disease cascade or the health system as a whole (Bottcher et al., 2015; Chen et al., 2019; Cruz-Aponte et al., 2011; Ferrer et al., 2014; Hecht and Gandhi, 2008; Marks et al., 2017; Peak et al., 2020; Salomon et al., 2006; Sébille and Valleron, 1997; Shattock et al., 2016; Shim et al., 2011; Stopard et al., 2019; Zhang et al., 2020).
The second category is unconstrained estimation, where interventions are modelled at full coverage but the gap in current resources for reaching that coverage is quantified in monetary or physical units, such as staff full-time equivalent (FTE) (Adisasmito et al., 2015; Barker et al., 2017; Putthasri et al., 2009; Rudge et al., 2012; Stenberg et al., 2017; Verma et al., 2020). Some of the studies in the review adopted a combination of these approaches, calculating both constrained impact estimates and the costs or resource requirements for relaxing the constraints (Alistar et al., 2013; Anderson et al., 2014, 2018; Bärnighausen et al., 2016; Bozzani et al., 2018, 2020; Hontelez et al., 2016; Krumkamp et al., 2011; McKay et al., 2018; Sumner et al., 2019). For example, Bozzani, Sumner and colleagues presented an analysis of different TB screening and diagnosis algorithms in South Africa under several constraints scenarios limiting effects along the TB prevention and care cascade to varying degrees, then modelled the additional staff FTE and costs of purchasing extra quantities of diagnostic consumables required to relax the constraints and achieve target coverage, observing any differences in the cost-effectiveness ranking of the screening options with and without constraints (Bozzani et al., 2018, 2020; Sumner et al., 2019).
In practice, constrained and unconstrained model-based estimation was most commonly achieved by combining transmission model outputs with unit costs (to address financial constraints) and other input per unit estimates, such as nurse FTE per output, to calculate resource usage at different intervention coverage levels and any additional requirements to relax constraints (Adisasmito et al., 2015; Alistar et al., 2013; Anderson et al., 2018; Bärnighausen et al., 2016; Barker et al., 2017; Bottcher et al., 2015; Bozzani et al., 2018, 2020; Cruz-Aponte et al., 2011; Ferrer et al., 2014; Hecht and Gandhi, 2008; Hontelez et al., 2016; Krumkamp et al., 2011; Marks et al., 2017; McKay et al., 2018; Putthasri et al., 2009; Rudge et al., 2012; Salomon et al., 2006; Sébille and Valleron, 1997; Shattock et al., 2016; Shim et al., 2011; Stenberg et al., 2017; Sumner et al., 2019; Verma et al., 2020). For instance, the agent-based model by McKay et al. analysed the relationship between HIV outcomes and staffing levels at a health agency by simulating changes over time in the number of HR positions, turnover rates and length of time for training newly recruited staff, and observing the effect of this HR constraint on the effectiveness of a prevention intervention (McKay et al., 2018).
A related approach adopted to incorporate constraints was the ‘linkage’ of disease transmission models with health system models, such as system dynamics (Curran et al., 2016; Martin et al., 2015a, b) or operational models (Langley et al., 2014; Lin et al., 2011). In this approach, model-based estimation relied on the health system models to generate estimates of the impact of constraints on intervention effects, which were then used to parametrise the transmission models. As an example, Curran and colleagues illustrated possible ways of integrating transmission models with system dynamics models to regulate the flows impacting on infection dynamics based on system capacity (Curran et al., 2016).
The last approach to integrate constraints was optimisation under a constraint other than the available budget. This approach was followed by two studies that sought to prioritise among different strategies, one for flu vaccine allocation in different age groups and one for HCV treatment, under different policy objectives such as minimising total incidence/prevalence, total deaths or total utility losses (Dalgiç et al., 2017; Martin et al., 2011; Zhang et al., 2020).
4. Discussion and conclusions
Incorporating health system elements that influence the priority setting process for disease control interventions, either by limiting the pace and scale of implementation or by otherwise determining their feasibility (as in the case of political or ethical constraints), is an increasingly common practice in the modelling literature. The main objectives of the studies reviewed were to constrain mathematical model outputs to approximate real-world implementation and to guide efficient resource allocation in the presence of constraints. They thus generated priority setting evidence that is more functional to the country-level planning cycle, in contrast to the ‘perfect implementation’ evidence generated by trials, trial-based economic evaluations and traditional target-driven modelling exercises (Menzies et al., 2019; Mikkelsen et al., 2017). One key advantage of these constrained analyses is that, by comparing target and actual implementation, the models allow analysts to calculate the resources needed for ‘relaxing’ the constraints, thus providing policy-makers with a more accurate estimate of the value for money of investing in a given intervention implemented at full scale.
Although the characteristics of the interventions and of the relative constraints are context-specific, there were patterns across settings in this review. For example, there was no distinction between demand-side and supply-side constraints in terms of the policy questions asked, whether about real-world impact or efficient investments (or both), and of the model structures used to explore them. Disease areas were also equally represented across models and similar objectives were pursued, for instance, by a study using an agent-based simulation to explore the allocation of flu vaccines in the presence of physical stockouts and a study using a SIR-like model to assess antiviral treatment strategies under different policy objectives (Dalgiç et al., 2017; Martin et al., 2011).
Constraints incorporation was achieved in two main ways, both of which can be accommodated by all mathematical model types: (i) model-based estimation, whereby limitations to intervention coverage were applied on the basis of either demand- or supply-side factors; (ii) optimisation, under a non-financial constraint or policy objective. The former was the most common approach overall, while the latter can be exclusively applied in analyses seeking to guide efficient resouce allocation. Approaches for identifying the applicable constraints and quantifying the extent of their impact varied in terms of strength, from unspecified assumptions to primary data collection, for example for building an operational model, and to structured stakeholder elicitation methods such as for systems dynamics modelling. Model-based estimation approaches thus varied according to the constraints quantification methods, and the dynamic transmission models were parametrised either in standard ways, using primary or secondary data, or through ‘linkage’ with the health system models (operational or system dynamics). The examples of model linkage in our sample are all from studies assessing interventions involving policy changes, such as a new HIV testing and linkage to care model, that are amenable to distal constraints more easily identified and quantified through group model building exercises involving a wide range of stakeholders.
This review builds on previous theoretical work on conceptualising and operationalising constraints (Vassall et al., 2016), but does not attempt to define the feasibility decision criterion. This concept and its influence on priority setting have been ill-defined in the literature and may encompass a range of aspects such as affordability, physical constraints that directly restrict access to services or technologies and arbitrary beliefs held by decision-makers and the wider environment that limit implementation in some way (Guindo et al., 2012; Tromp and Baltussen, 2012). In this review, the focus was restricted to non-financial constraints but the definition of constraints was kept deliberatly broad to capture all relevant incorporation approaches. The search strategy returned a number of records dealing with political, social and ethical constraints on the decision-making process, since it contained keywords around priority setting and decision-making criteria. We therefore introduced a working distinction between constraints on physical inputs and political constraints, including policy objectives. This latter category could, for example, include principles such as equity in cases where this objective is treated in the analysis as a de facto constraint to the roll-out or scale-up of an intervention, as in the study assessing the effects of prioritising key populations when delivering combination HIV prevention in Kenya (Anderson et al., 2014).
In conclusion, this review has shown that the inclusion of non-financial health system constraints in mathematical model-based priority setting can be accommodated within all model structures that are commonly used in epidemiological analyses. Despite the additional complexity, the enhanced models produce valuable information, including estimates of the costs of relaxing the constraints i.e. the true cost of the intervention at scale. As modelling techniques become more sophisticated and user-friendly and data availability improves, it will become increasingly possible to parametrise the models using real-time surveillance data, thus making the identification and quantification of constraints more viable and making models more locally-relevant and accessible for decision-makers within the policy timeframe (Alistar et al., 2013; Masoodian and Luz, 2017). However, further research is needed to categorise health system constraints, to assist their systematic operationalisation in models.
Author contributions
Fiammetta Bozzani: Conceptualization, Methodology, Investigation, Formal Analysis, Writing – Oiginal draft preparation. Gabriela Gomez: Funding acquisition, Conceptualization, Supervision, Writing – Review and editing. Anna Vassall: Conceptualization, Supervision, Writing – Review and editing
Funding
This work was funded by the Bill and Melinda Gates Foundation through the TB Modelling and Analysis Consortium (TB-MAC, grant number OPP1135288).
Declaration of Competing Interest
None. GBG is currently employed by Sanofi Pasteur as Regional Lead for vaccine epidemiology and modelling in Europe. Sanofi Pasteur has not provided funding for this work. GBG’s contribution to this work pertains to PhD supervisory activities as honorary staff at LSHTM.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.epidem.2021.100450.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Adisasmito W., Hunter B.M., Krumkamp R., Latief K., Rudge J.W., Hanvoravongchai P., Coker R.J. Pandemic influenza and health system resource gaps in bali: an analysis through a resource transmission dynamics model. Asia. J. Public Health. 2015;27:NP713–NP733. doi: 10.1177/1010539511421365. [DOI] [PubMed] [Google Scholar]
- Alistar S.S., Brandeau M.L., Beck E.J. International Series in Operations Research and Management Science. Springer New York LLC; 2013. REACH: a practical HIV resource allocation tool for decision makers. [DOI] [Google Scholar]
- Anderson S.J., Cherutich P., Kilonzo N., Cremin I., Fecht D., Kimanga D., Harper M., Masha R.L., Ngongo P.B., Maina W., Dybul M., Hallett T.B. Maximising the effect of combination HIV prevention through prioritisation of the people and places in greatest need: a modelling study. Lancet. 2014;384:249–256. doi: 10.1016/S0140-6736(14)61053-9. [DOI] [PubMed] [Google Scholar]
- Anderson S.J., Ghys P.D., Ombam R., Hallett T.B. Frontloading HIV financing maximizes the achievable impact of hiv prevention. J. Int. AIDS Soc. 2018;21(3) doi: 10.1002/jia2.25087. (no pagination) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker C., Dutta A., Klein K. Can differentiated care models solve the crisis in HIV treatment financing? Analysis of prospects for 38 countries in sub-Saharan Africa. J. Int. AIDS Soc. 2017;20 doi: 10.7448/IAS.20.5.21648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bärnighausen T., Bloom D.E., Humair S. Human resources for treating HIV/AIDS: Are the preventive effects of antiretroviral treatment a game changer? PLoS One. 2016;11(10) doi: 10.1371/journal.pone.0163960. (no pagination) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottcher L., Woolley-Meza O., Araujo N.A., Herrmann H.J., Helbing D. Disease-induced resource constraints can trigger explosive epidemics. Sci. Rep. 2015;5:16571. doi: 10.1038/srep16571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozzani F.M., Mudzengi D., Sumner T., Gomez G.B., Hippner P., Cardenas V., Charalambous S., White R., Vassall A. Empirical estimation of resource constraints for use in model-based economic evaluation: an example of TB services in South Africa. Cost Eff. Resour. Alloc. 2018;16:27. doi: 10.1186/s12962-018-0113-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozzani F.M., Sumner T., Mudzengi D., Gomez G.B., White R., Vassall A. Informing balanced investment in services and health systems: a case study of priority setting for tuberculosis interventions in South Africa. Value Health. 2020;23:1462–1469. doi: 10.1016/j.jval.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Zhou T., Feng L., Liang J., Liljeros F., Havlin S., Hu Y. Nontrivial resource requirement in the early stage for containment of epidemics. Phys. Rev. E. 2019;100 doi: 10.1103/PhysRevE.100.032310. [DOI] [PubMed] [Google Scholar]
- Cruz-Aponte M., Mckiernan E.C., Herrera-Valdez M.A. Mitigating effects of vaccination on influenza outbreaks given constraints in stockpile size and daily administration capacity. BMC Infect. Dis. 2011;11 doi: 10.1186/1471-2334-11-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran M., Howley E., Duggan J. Association for Computing Machinery, Inc; 2016. An Analytics Framework to Support Surge Capacity Planning for Emerging Epidemics; pp. 151–155. [Google Scholar]
- Dalgiç Ö.O., Özaltin O.Y., Ciccotelli W.A., Erenay F.S. Deriving effective vaccine allocation strategies for pandemic influenza: comparison of an agent-based simulation and a compartmental model. PLoS One. 2017;12 doi: 10.1371/journal.pone.0172261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer J., Boelle P.Y., Salomon J., Miliani K., L’hériteau F., Astagneau P., Temime L. Management of nurse shortage and its impact on pathogen dissemination in the intensive care unit. Epidemics. 2014;9:62–69. doi: 10.1016/j.epidem.2014.07.002. [DOI] [PubMed] [Google Scholar]
- Guindo L.A., Wagner M., Baltussen R., Rindress D., Van Til J., Kind P., Goetghebeur M.M. From efficacy to equity: literature review of decision criteria for resource allocation and healthcare decisionmaking. Cost Eff. Resour. Alloc. 2012;10 doi: 10.1186/1478-7547-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauck K., Thomas R., Smith P.C. Departures from cost-effectiveness recommendations: the impact of health system constraints on priority setting. Health Syst. Reform. 2016;2:61–70. doi: 10.1080/23288604.2015.1124170. [DOI] [PubMed] [Google Scholar]
- Hecht R., Gandhi G. Demand forecasting for preventive AIDS vaccines: economic and policy dimensions. PharmacoEconomics. 2008;26:679–697. doi: 10.2165/00019053-200826080-00005. [DOI] [PubMed] [Google Scholar]
- Hontelez J.A.C., Change A.Y., Ogbuoji O., De Vlas S.J., Barnighausen T., Atun R. Changing HIV treatment eligibility under health system constraints in sub-Saharan Africa: investment needs, population health gains, and cost-effectiveness. AIDS. 2016;30:2341–2350. doi: 10.1097/QAD.0000000000001190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houben R.M.G.J., Lalli M., Sumner T., Hamilton M., Pedrazzoli D., Bonsu F., Hippner P., Pillay Y., Kimerling M., Ahmedov S., Pretorius C., White R.G. TIME Impact – a new user-friendly tuberculosis (TB) model to inform TB policy decisions. BMC Med. 2016;14:1–10. doi: 10.1186/s12916-016-0608-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamison D.T., Alwan A., Mock C.N., Nugent R., Watkins D., Adeyi O., Anand S., Atun R., Bertozzi S., Bhutta Z., Binagwaho A., Black R., Blecher M., Bloom B.R., Brouwer E., Bundy D.A.P., Chisholm D., Cieza A., Cullen M., Danforth K., De Silva N., Debas H.T., Donkor P., Dua T., Fleming K.A., Gallivan M., Garcia P.J., Gawande A., Gaziano T., Gelband H., Glass R., Glassman A., Gray G., Habte D., Holmes K.K., Horton S., Hutton G., Jha P., Knaul F.M., Kobusingye O., Krakauer E.L., Kruk M.E., Lachmann P., Laxminarayan R., Levin C., Looi L.M., Madhav N., Mahmoud A., Mbanya J.C., Measham A., Medina-Mora M.E., Medlin C., Mills A., Mills J.A., Montoya J., Norheim O., Olson Z., Omokhodion F., Oppenheim B., Ord T., Patel V., Patton G.C., Peabody J., Prabhakaran D., Qi J., Reynolds T., Ruacan S., Sankaranarayanan R., Sepulveda J., Skolnik R., Smith K.R., Temmerman M., Tollman S., Verguet S., Walker D.G., Walker N., Wu Y., Zhao K. Universal health coverage and intersectoral action for health: key messages from Disease Control Priorities, 3rd edition. Lancet. 2018;391:1108–1120. doi: 10.1016/S0140-6736(17)32906-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumkamp R., Kretzschmar M., Rudge J.W., Ahmad A., Hanvoravongchai P., Westenhoefer J., Stein M., Putthasri W., Coker R. Health Service Resource needs for pandemic influenza in developing countries: a linked transmission dynamics, interventions and resource demand model. Epidemiol. Infect. 2011;139:59–67. doi: 10.1017/S0950268810002220. [DOI] [PubMed] [Google Scholar]
- Langley I., Adams E., Doulla B., Squire S.B. Operational modelling to guide implementation and scale-up of diagnostic tests within the health system: exploring opportunities for parasitic disease diagnostics based on example application for tuberculosis. Parasitology. 2014;141:1795–1802. doi: 10.1017/S0031182014000985. [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H.H., Langley I., Mwenda R., Doulla B., Egwaga S., Millington K.A., Mann G.H., Murray M., Squire S.B., Cohen T. A modelling framework to support the selection and implementation of new tuberculosis diagnostic tools. Int. J. Tuberc. Lung Dis. 2011;15:996–1004. doi: 10.5588/ijtld.11.0062. [DOI] [PubMed] [Google Scholar]
- Lubell Y., Hopkins H., Whitty C.J., Staedke S.G., Mills A. An interactive model for the assessment of the economic costs and benefits of different rapid diagnostic tests for malaria. Malar. J. 2008;7:21. doi: 10.1186/1475-2875-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks M.E., Funk S., Mitja O., Fitzpatrick C., Asiedu K., Solomon A.W., Mabey D.C. Mathematical modelling approaches to estimating the optimum strategy for the eradication of yaws. Am. J. Trop. Med. Hyg. 2015;93(4 Supplement):26. [Google Scholar]
- Marks M.E., Funk S., Mitja O., Fitzpatrick C., Asiedu K., Solomon A.W., Mabey D.C. Mathematical modelling approaches to estimating the optimum strategy for the eradication of yaws. Am. J. Trop. Med. Hyg. 2017;93(4 Supplement):26. [Google Scholar]
- Martin N.K., Pitcher A.B., Vickerman P., Vassall A., Hickman M. Optimal control of hepatitis C antiviral treatment programme delivery for prevention amongst a population of injecting drug users. PLoS One [Electron. Resour.] 2011;6 doi: 10.1371/journal.pone.0022309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin E.G., Macdonald R.H., Smith L.C., Gordon D.E., Tesoriero J.M., Laufer F.N., Leung S.Y.J., O’connell D.A. Policy modeling to support administrative decisionmaking on the new york state hiv testing law. J. Policy Anal. Manag. 2015;34:403–423. doi: 10.1002/pam.21797. [DOI] [PubMed] [Google Scholar]
- Martin E.G., Macdonald R.H., Smith L.C., Gordon D.E., Tesoriero J.M., Laufer F.N., Leung S.Y.J., Rowe K.A., O’connell D.A. Mandating the offer of HIV testing in New York: simulating the epidemic impact and resource needs. J. Acquir. Immune Defic. Syndr. 2015;68:S59–S67. doi: 10.1097/QAI.0000000000000395. [DOI] [PubMed] [Google Scholar]
- Masoodian M., Luz S. In: Ecoepidemiological Simulation as a Serious Game Engine Module. Bamidis P.D., Konstantinidis S.T., Rodrigues P.P., editors. Institute of Electrical and Electronics Engineers Inc.; 2017. pp. 193–194. [Google Scholar]
- Mckay V.R., Hoffer L.D., Combs T.B., Margaret Dolcini M. The dynamic influence of human resources on evidence-based intervention sustainability and population outcomes: an agent-based modeling approach. Implement. Sci. 2018;13 doi: 10.1186/s13012-018-0767-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzies N.A., Gomez G.B., Bozzani F., Chatterjee S., Foster N., Garcia Baena I., Laurence Y. Cost-effectiveness and resource implications of aggressive TB control in China, India and South Africa: a combined analysis of nine models. Lancet Glob. Health. 2016;4:e816–e826. doi: 10.1016/S2214-109X(16)30265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzies N.A., Mcquaid C.F., Gomez G.B., Siroka A., Glaziou P., Floyd K., White R.G., Houben R.M.G.J. Improving the quality of modelling evidence used for tuberculosis policy evaluation. Int. J. Tuberc. Lung Dis. 2019;23:387–395. doi: 10.5588/ijtld.18.0660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikkelsen E., Hontelez J.A.C., Jansen M.P.M., Bärnighausen T., Hauck K., Johansson K.A., Meyer-Rath G., Over M., De Vlas S.J., Van Der Wilt G.J., Tromp N., Bijlmakers L., Baltussen R.M.P.M. Evidence for scaling up HIV treatment in sub-Saharan Africa: a call for incorporating health systems constraints. PLoS Med. 2017;14 doi: 10.1371/journal.pmed.1002240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peak C.M., Kahn R., Grad Y.H., Childs L.M., Li R., Lipsitch M., Buckee C.O. Individual quarantine versus active monitoring of contacts for the mitigation of COVID-19: a modelling study. Lancet Infect. Dis. 2020;20:1025–1033. doi: 10.1016/S1473-3099(20)30361-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putthasri W., Lertiendumrong J., Chompook P., Tangcharoensathien V., Coker R. Capacity of Thailand to contain an emerging influenza pandemic. Emerging Infect. Dis. 2009;15:423–432. doi: 10.3201/eid1503.080872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudge J.W., Hanvoravongchai P., Krumkamp R., Chavez I., Adisasmito W., Chau P.N., Phommasak B., Putthasri W., Shih C.S., Stein M., Timen A., Touch S., Reintjes R., Coker R., Asiaflucap Project C. Health system resource gaps and associated mortality from pandemic influenza across six Asian territories. PLoS One [Electron. Resour.] 2012;7 doi: 10.1371/journal.pone.0031800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon J.A., Lloyd-Smith J.O., Getz W.M., Resch S., Sanchez M.S., Porco T.C., Borgdorff M.W. Prospects for advancing tuberculosis control efforts through novel therapies. PLoS Med. 2006;3:e273. doi: 10.1371/journal.pmed.0030273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sébille V., Valleron A.J. A computer simulation model for the spread of nosocomial infections caused by multidrug-resistant pathogens. Comput. Biomed. Res. 1997;30:307–322. doi: 10.1006/cbmr.1997.1451. [DOI] [PubMed] [Google Scholar]
- Shattock A.J., Kerr C.C., Stuart R.M., Masaki E., Fraser N., Benedikt C., Gorgens M., Wilson D.P., Gray R.T. In the interests of time: improving HIV allocative efficiency modelling via optimal time-varying allocations. J. Int. AIDS Soc. 2016;19:20627. doi: 10.7448/IAS.19.1.20627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim E., Meyers L.A., Galvani A.P. Optimal H1N1 vaccination strategies based on self-interest versus group interest. BMC Public Health. 2011;11(Suppl 1):S4. doi: 10.1186/1471-2458-11-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stegmuller A.R., Self A., Litvin K., Roberton T. How is the Lives Saved Tool (LiST) used in the global health community? Results of a mixed-methods LiST user study. BMC Public Health. 2017;17:773. doi: 10.1186/s12889-017-4750-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenberg K., Hanssen O., Edejer T.T.T., Bertram M., Brindley C., Meshreky A., Rosen J.E., Stover J., Verboom P., Sanders R., Soucat A. Financing transformative health systems towards achievement of the health Sustainable Development Goals: a model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob. Health. 2017;5:e875–e887. doi: 10.1016/S2214-109X(17)30263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stopard I.J., Mcgillen J.B., Hauck K., Hallett T.B. The influence of constraints on the efficient allocation of resources for HIV prevention. AIDS. 2019;33:1241–1246. doi: 10.1097/QAD.0000000000002158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumner T., Bozzani F., Mudzengi D., Hippner P., Houben R.M., Cardenas V., Vassall A., White R.G. Estimating the impact of tuberculosis case detection in constrained health systems: an example of case-finding in South Africa. Am. J. Epidemiol. 2019;188:1155–1164. doi: 10.1093/aje/kwz038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tromp N., Baltussen R. Mapping of multiple criteria for priority setting of health interventions: an aid for decision makers. BMC Health Serv. Res. 2012;12:454. doi: 10.1186/1472-6963-12-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vassall A., Mangham-Jefferies L., Gomez G.B., Pitt C., Foster N. Incorporating demand and supply constraints into economic evaluation in low-income and middle-income countries. Health Econ. 2016;25:95–115. doi: 10.1002/hec.3306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma V.R., Saini A., Gandhi S., Dash U., Koya S.F. Capacity-need gap in hospital resources for varying mitigation and containment strategies in India in the face of COVID-19 pandemic. Infect. Dis. Model. 2020;5:608–621. doi: 10.1016/j.idm.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Yang Z., Pawelek K.A., Liu S. Optimal control strategies for a two-group epidemic model with vaccination-resource constraints. Appl. Math. Comput. 2020;371 doi: 10.1016/j.amc.2019.124956. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.