Abstract
Aim and Objective:
Our study's objective is to determine the level of awareness in postmenopausal women in Guwahati, Northeast part of India, using the Osteoporosis Health Belief Scale (OHBS).
Settings and Design:
Osteoporosis is the most common silent health problem in postmenopausal Indian women. An awareness level among this subset of women needs to study. The present study is based on a self-explanatory questionnaire.
Methods:
We conducted a self-explanatory questionnaire study on 2000 postmenopausal women in Guwahati, North East region of India. The bone mineral density (BMD) was measured using calcaneum Quantitative ultrasound (QUS) to assess BMD. Baseline characteristics were noted and analyzed.
Results:
The awareness level was noted only in757 (37.85%). Women with education level 12th standard and above have some awareness regarding osteoporosis.
Conclusions:
Based on the present study, we can conclude that there is a lack of awareness in postmenopausal women regarding osteoporosis in India's North-East region. This subset of women is unaware of the condition that can leads to fragility fracture if not address in time. The study emphasizes that health care professionals should conduct frequent awareness programs in the community to prevent this silent disease, and morbidities so arise from osteoporosis can be minimized.
Keywords: Awareness, bone mineral density, calcaneum, osteoporosis, postmenopausal women, Quantitative ultrasound (QUS)
Introduction
Osteoporosis is commonly known as “porous bones” disease because of a decrease in bone mineral density. Postmenopausal women and the aging population are greatly affected. This silent disease affects a large number of the aging population globally and a cause of fragility fracture by trivial injury. Such fractures may increase morbidity and mortality and increase the financial burden on the family.[1,2] Osteoporosis leads to significant morbidity in postmenopausal women and the geriatric population. Before starting the study on the magnitude of health problems, it is prudent to know the awareness level in public about the disease. Its prevention and management require awareness and understanding amongst postmenopausal women and elderly men.
To assess the awareness of osteoporosis among postmenopausal women residing in the North East region of India, we conducted our study based on a self-explanatory questionnaire-Osteoporosis Health Belief Scale (OHBS). We have chosen the Osteoporosis Health Belief Scale (OHBS) for our study because it is simple and understandable easily. The DEXA (dual-energy X-ray absorptiometry) was used for BMD estimation because it is a gold standard test, easily affordable, and provides a reliable estimation of the BMD.[3] However, in our study of covering such a large population, we used calcaneum Quantitative ultrasound (QUS) to assess BMD.
Quantitative ultrasound (QUS) tool was used for assessing bone health that has gained popularity regarding screening of the population. As compared to Dexa, QUS is cost-effective, non-invasive, easy to use, no danger of ionizing radiation, and can be used for the public at large.[4] A quantitative ultrasound tool has been used to assess bone health in men, women, children, and sometimes in, infants.[5,6,7]
The quantitative ultrasound (QUS) tool is based on an ultrasound wave with a frequency of greater than 20 kHz. The frequency used in QUS usually ranges between 200 kHz and 1.5 MHz. The machine has two probes one for emission and another for receiving a signal. The portion of a bone under study is placed between these two probes.[8]
Since there is insufficient data available in the literature from Guwahati, North East region of India, we aimed to find out the association among various components of the OHBS, which are indicators of awareness of osteoporosis. The Osteoporosis Health Belief Scale (OHBS) is consists of 42 questions used for general health, perceived susceptibility to and seriousness of osteoporosis, and beliefs regarding calcium intake and exercise in preventing and treating the said disease.
Material and Methods
The study was conducted in 2000 postmenopausal women who visited our tertiary care hospital in various OPD. The included population of women belonging to different localities of the North East region of India. The study was conducted between Jan 2018 and Feb 2020. After performing relevant hematological and serological tests to rule out metabolic diseases, and autoimmune disease, the volunteer is asked to complete the questioners and answer a few simple questions designed by our expert team.
Have you heard or know about osteoporosis?
Have you heard of fragility fractures occur because of osteoporosis?
In your regular diet do you take milk regularly? If yes, in what quantity?
In your regular diet do you take curd/paneer regularly?
Do you aware of taking calcium tablets daily?
Do you aware of taking vitamin D supplements?
In your family, any member suffered from a fragility fracture?
Do you perform regular physical exercise?
The included postmenopausal women in the study have explained the questionnaire and the responses were recorded by a team of authors. In addition to OHBS, other demographical characteristics like weight, height, BMI, physical activity, and milk intake were noted. We used calcaneum Quantitative ultrasound (QUS) to assess BMD for such a large population.
Based on the “t” score of BMD assessment by Quantitative ultrasound (QUS), the patients were divided into three groups (a) Normal those have t score ≥−1.0, (b) Osteopenic those have t score between − 1.0 and − 2.5 and, (c) Osteoporotic those have t score ≤−2.5. The data so collected were analyzed using SPSS version 19 (IBM, USA). Ethical approval was taken vide latter no (Ortho/02/EA/2018) dated 11 Oct 2018.
Results
The average age of 2000 enrolled women was 65 years (45-85 years). The awareness level was noted only in 757 women (37.85%). Demographical characteristic of the study population is shown in Table 1. The proportion of women who had heard of osteoporosis before was significantly higher in those who have education up to 12th standard and higher than those of lesser education (860; 43% versus 1140; 57%, respectively, P < 0.001). Similarly, the proportion of women who taking milk were not statistically significant (P-value 0.7815). We noted no significant difference between women who had heard of osteoporotic fracture before and those with physical exercise (each P value 0.782). The early postmenopausal women population who had heard of osteoporotic fracture was significantly higher than the later age of postmenopausal (622; 31.1% at age 45–65 years, P < 0.05). Women with higher education were found to have a better awareness of osteoporosis (P < 0.05). Women with a previous fragility fracture in the family or to herself had better awareness than those without such a history (P < 0.05) [Table 1].
Table 1.
Demographical characteristics of the study population
| Parameters | No of patient n=2000 | Heard or little knowledge of Osteoporosis | Heard or little knowledge of fragility fracture | Taking Milk | Taking curd/paneer | Physical exercise | fragility fracture in family/self |
|---|---|---|---|---|---|---|---|
| Age in years | |||||||
| 45-55 | 1021 | 483* | 219* | 98 | 45 | 102 | - |
| 56-65 | 637 | 139* | 23# | 108 | 143 | 213 | 14 |
| 66-75 | 210 | 79* | 11 | 102 | 136 | 21 | 45* |
| 76-85 | 132 | 56* | 69* | 89 | 101 | 9 | 82* |
| Total | 2000 | 757 (37.85%) | |||||
| Education level | |||||||
| None | 98 | - | 5 | 88 | 88 | 54 | 12 |
| Up to 8 | 252 | 46# | 8 | 148 | 148# | 76 | 31# |
| Up to 10 | 563 | 118 | 11 | 341 | 341 | 85 | 46 |
| Up to 12 | 1074 | 849* | 17* | 751* | 751 | 390* | 486* |
| Graduation and above | 13 | 11* | 9* | 11* | 11* | 7* | 9 |
| BMI in kg/m2 | |||||||
| <18.5 kg/m2 | 234 | 97 | 12 | 17 | 17 | 101 | 32 |
| 18.5-25 kg/m2 | 599 | 49 | 9 | 293 | 293 | 341 | 21 |
| >25 kg/m2 | 1167 | 617* | 519* | 438 | 438 | 612 | 127* |
| BMD t-Score | |||||||
| Normal -1.0 or greater | 238 | 38# | 65 | 111 | 67 | 49 | - |
| Osteopenia 1 -.0 and 0.2.5 | 915 | 49 | 32 | 312 | 402 | 42 | 109* |
| Osteoporosis -2.5 and below | 218 | 28# | 21 | 79 | 113 | 79 | 93* |
| Sever Osteoporosis -2.5 and below + fragility fracture | 629 | 393* | 287* | 282* | 314 | 24 | 419* |
*Denotes P<0.001 #denotes P<0.05
The average BMI was 24.6 ± 3.58. Among 2000 women, 847 (42.35%) women had a “t” score of − 2.5 and below and were osteoporotic, 915 (45.75%) women had “t” score − 1 to − 2.5 and were osteopenic and whereas only 238 (11.9%) women had “t” score − 1 to 1 and were shown normal BMD. The mean scores were 17.28, 16.69, and 19.14 for normal, osteopenic, and osteoporotic individuals respectively (P-value was 0.723 using ANOVA test). In our study, we find no statistically significant difference between the mean susceptibility scores among normal, osteopenic, and osteoporotic women. By ANOVA test the “P” values for other parameters like seriousness, the advantage of taking calcium, exercise, no motivation to exercise, barriers to take calcium, and health motivation were 0.4210, 0.292, 0.383, 0.781, 0.855, and 0.873, respectively, and were not statistically significant. The maximum and minimum scores of various parameters have shown in Table 2.
Table 2.
Maximum and minimum scores for each parameter of the Osteoporosis Health Belief Scale questionnaire
| Parameters | 95% Cl for mean | Minimum | Maximum | |
|---|---|---|---|---|
| Upper | Lower | |||
| Susceptibility | ||||
| Normal | 21.28 | 17.32 | 11 | 12 |
| Osteopenia | 18.34 | 17.92 | 13 | 16 |
| Osteoporosis | 19.34 | 18.82 | 14 | 16 |
| Advantage of calcium intake | ||||
| Normal | 20.75 | 17.92 | 18 | 23 |
| Osteopenia | 25.23 | 19.39 | 21 | 26 |
| Osteoporosis | 27.92 | 25.56 | 24 | 26 |
| Non motivated for exercise | ||||
| Normal | 24.72 | 18.96 | 25 | 28 |
| Osteopenia | 27.39 | 26.35 | 29 | 24 |
| Osteoporosis | 31.42 | 26.66 | 28 | 32 |
| Health motivation | ||||
| Normal | 22.82 | 19.92 | 23 | 29 |
| Osteopenia | 27.99 | 25.75 | 32 | 35 |
| Osteoporosis | 32.72 | 28.69 | 38 | 43 |
| Non motivated to calcium intake | ||||
| Normal | 23.98 | 21.56 | 27 | 32 |
| Osteopenia | 32.69 | 29.88 | 35 | 39 |
| Osteoporosis | 31.82 | 29.19 | 34 | 39 |
| Health motivation | ||||
| Normal | 18.92 | 16.79 | 19 | 25 |
| Osteopenia | 19.24 | 18.29 | 24 | 29 |
| Osteoporosis | 21.29 | 19.24 | 31 | 37 |
| Seriousness | ||||
| Normal | 23.34 | 21.80 | 15 | 18 |
| Osteopenia | 21.57 | 19.29 | 19 | 23 |
| Osteoporosis | 34.28 | 31.82 | 18 | 21 |
After data collection in Microsoft Excel 2019, Pearson's correlation analysis was performed using SSPS software and the association between parameters of OHBS was compared to each other, which was found to be significant. Based on our results level of awareness regarding the parameters of OHBS is varying widely. A spearman's rho analysis was showing the same and we did not record any significance.
Women with normal BMD constitute about 238 (11.1%), women who were osteopenic constitute 915 (45.75%), and women who were osteoporosis was 847 (42.35%) Table 3.
Table 3.
Number of participants with BMD and their BMI
| BMI | No of women | Normal BMD | Osteoporosis | Osteopenia |
|---|---|---|---|---|
| <18.5- (underweight) | 234 | 11 | 138 | 85 |
| 18.5 up to 25 kg/m2 (Normal weight) | 607 | 92 | 271 | 244 |
| >25 (overweight) | 1159 | 135 | 438 | 586 |
| Total | 2000 | 238 (11.9%) | 847 (42.35%) | 915 (45.75%) |
The distribution of BMD and BMI with the number of the study population has shown in Figures 1 and 2 respectively.
Figure 1.

BMD and the number of the study population
Figure 2.
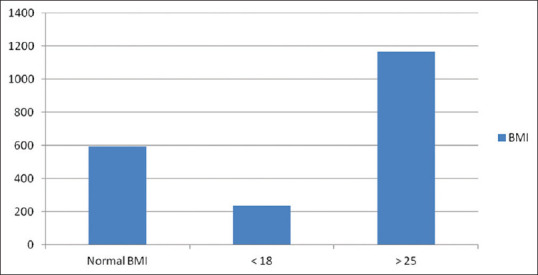
BMI distribution in the study population
BMD and BMI correlation distribution in the study population has been shown in Figure 3.
Figure 3.

BMD and BMI correlation distribution in the study population
Discussion
There are very few such studies from the Northeastern part of India regarding this silent epidemic. Awareness campaigns have been launched in few countries on osteoporosis at national levels a few decades ago.[9,10] To our knowledge, there has not been any population-based questioner and interventional approach in this part of India to know the public awareness of this silent and common disease.
To raise awareness, we must know the level of the present awareness amongst the general population.[11] The present study assessed the level of awareness of osteoporosis among postmenopausal women more than 45 years and older. Our results suggest that awareness of osteoporosis is very low among our study population. In addition, many women taking milk without any knowledge of osteoporosis and are having low BMD scores.
In general society and at the community level, losing weight with age is acceptable and considered as a sign of aging. Being a “silent disease” without any pain or other worrying symptoms is not widely accepted as a disease in the community until a fragility fracture occurs. That is why only 37.85% of our study population knows little about osteoporosis. Recent studies on awareness of osteoporosis have been summarized in Table 4.
Table 4.
Summary of studies on awareness of osteoporosis
| Author | Study type and population | Country | Awareness level/heard of osteoporosis |
|---|---|---|---|
| Yeap et al.[12] | attendees of health-related public forums | Malasia | 87.1% |
| Gemalmaz et al.[13] | 768 women | Turkey | 60.8% |
| Saw et al.[14] | 1376 women | Singapur | 58% |
| Xu J et al.[15] | 9983 | China | 30.7% |
| Shawa et al.[16] | 130 men | Chicago | 77% |
| Alexandraki et al.[17] | 99 women | Greek | 96% |
| Gopinathan et al.[18] | A questionnaire based study in 100 postmenopausal women | India | Great lack of awareness was observed in postmenopausal Indian women. |
| Present study | 2000 women | India | 37.85% |
It has been observed that the selection of the population, age sex, and menopausal status, residing in rural or urban, and socioeconomic status may influence the degree of awareness.
It was noted that and consistent with other studies, older women with a low BMI have low BMD (T score). Women with some education have better BMD, because of their increased awareness and taking preventive measures to improve bone health. It was observed that women believe that taking a glass of milk is associated with better bone health and had better BMD score as compared to who did not have heard of osteoporosis. Many women in India may not be taking milk, as many cannot afford it because of other family requirements. More recently few authors have reported a high prevalence rate of osteoporosis in Indian postmenopausal women.[19,20]
There is limited data regarding awareness of osteoporosis in this area is available.
Cline et al., noted that women were more susceptible to osteoporosis and can improve by taking calcium and Vit D supplements as compared to men.[21] Few authors from India reported poor awareness of osteoporosis in postmenopausal women are noted.[18,22,23,24]
The study done by Johnson et al.[25] found that men older than 50 years had significantly lower perceived susceptibility scores compared to women of the same age, supporting the thought that osteoporosis is a disease of women. His results indicate that women should be more aware than men about osteoporosis.
Castel et al., in their study, noted that osteoporosis was rarely recognized until fragility low impact fracture.[26] Sedlak et al., suggested that physicians could play an important role to improve knowledge regarding osteoporosis and fragility fractures.[27] It has been suggested in the literature that the prevention of osteoporosis be started at an early age in both sexes. We should educate our community about osteoporosis, its prevention, and the reduction of risk factors if any. Another important issue is the prevention of osteoporosis and osteoporotic fractures. In the management of chronic disease, increased knowledge about the disease is associated with improved patient compliance with its treatment.
Role of primary and family physician
As the number of postmenopausal women is on the constant rise in India and with a poor health care system, it is time to raise an alarm regarding osteoporosis in this subset of women. The primary physician can educate each woman attending the hospital.
Limitation of our survey
There are a few limitations to our study. First, India being a developing country with varied socio-economical status. Although the sample size was adequate our data collected from a particular region of India and are not necessarily representative of the whole country. Second, the daily milk, intake cannot be quantified and was not clear, and the type, frequency, of physical exercise was not explored.
Conclusions
The present study indicates majorities of postmenopausal women do not have any awareness regarding osteoporosis. Many women even do not know the entity, and many of them were clueless regarding osteoporosis and its prevention. The study suggested that healthcare givers should organize camps and awareness programs in their area of responsibility so that the prevalence of this silent disease can be reduced and, in turn, can reduce the health burden arising from osteoporosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the Department of Orthopaedics, Family OPD, and Radiology for supporting the study. The authors also want to express their gratitude toward all participants who help in recording the responses from patients.
References
- 1.Osteoporosis Canada, “About Osteoporosis,” Retrieved on 2010. Available from: http://www.osteoporosis.ca/
- 2.World Health Organization. Assessment of Fracture Risk and Its Application to Screening for Postmenopausal Osteoporosis. Geneva: WHO; 1994. [PubMed] [Google Scholar]
- 3.U.S. Preventive Services Task Force. Screening for osteoporosis in postmenopausal women: Recommendations and rationale. Ann Intern Med. 2002;137:526–8. doi: 10.7326/0003-4819-137-6-200209170-00014. [DOI] [PubMed] [Google Scholar]
- 4.Laugier P. An overview of bone sonometry. Int Congr Ser. 2004;1274:23–32. [Google Scholar]
- 5.Miura S, Saavedra OL, Yamamoto S. Osteoporosis in urban post-menopausal women of the Philippines: Prevalence and risk factors. Arch Osteoporos. 2008;3:17–24. [Google Scholar]
- 6.Meszaros S, Toth E, Ferencz V, Csupor E, Hosszu E, Horvath C. Calcaneous quantitative ultrasound measurements predicts vertebral fractures in idiopathic male osteoporosis. Joint Bone Spine. 2007;74:79–84. doi: 10.1016/j.jbspin.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 7.Mimura K, Yamamoto T, Nakatuka K, Yoh K, Arai T. Infant bone quantity measurement-Hoping for the growth of smooth bone. Clin Calcium. 2008;18:1014–27. [PubMed] [Google Scholar]
- 8.Guglielmi G, de Terlizzi F. Quantitative ultrasound in the assessment of osteoporosis. Eur J Radiol. 2009;71:425–31. doi: 10.1016/j.ejrad.2008.04.060. [DOI] [PubMed] [Google Scholar]
- 9.Edwards L, Fraser M. How do we increase awareness of osteoporosis? Baillieres Clin Rheumatol. 1997;11:631–44. doi: 10.1016/s0950-3579(97)80024-6. [DOI] [PubMed] [Google Scholar]
- 10.Foundation for Osteoporosis Research and Education The national osteoporosis awareness plan. [Last accessed on 2004 May 24]. Available from: http://www.fore.org/pdf/AOA_REPORT.pdf .
- 11.Werner P. Knowledge about osteoporosis: assessment, correlates and outcomes. Osteoporos Int. 2005;16:115–27. doi: 10.1007/s00198-004-1750-y. [DOI] [PubMed] [Google Scholar]
- 12.Yeap SS, Goh EM, Das Gupta E. Knowledge about osteoporosis in a Malaysian population. Asia Pac J Public Health. 2010;22:233–41. doi: 10.1177/1010539509343948. [DOI] [PubMed] [Google Scholar]
- 13.Gemalmaz A, Oge A. Knowledge and awareness about osteoporosis and its related factors among rural Turkish women. Clin Rheumatol. 2008;27:723–8. doi: 10.1007/s10067-007-0777-9. [DOI] [PubMed] [Google Scholar]
- 14.Saw SM, Hong CY, Lee J, Wong ML, Chan MF, Cheng A, et al. Awareness and health beliefs of women towards osteoporosis. Osteoporos Int. 2003;14:595–601. doi: 10.1007/s00198-003-1403-6. [DOI] [PubMed] [Google Scholar]
- 15.Xu J, Sun M, Wang Z, Fu Q, Cao M, Zhu Z, et al. Awareness of osteoporosis and its relationship with calcaneus quantitative ultrasound in a large Chinese community population. Clin Interv Aging. 2013;8:789–96. doi: 10.2147/CIA.S45874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shawa H, Favela E, Diaz J. Knowledge of osteoporosis among men in the primary care setting. South Med J. 2011;104:584–8. doi: 10.1097/SMJ.0b013e3182241da1. [DOI] [PubMed] [Google Scholar]
- 17.Alexandraki KI, Syriou V, Ziakas PD, Apostolopoulos NV, Alexandrakis AI, Piperi C, et al. The knowledge of osteoporosis risk factors in a Greek female population. Maturitas. 2008;59:38–45. doi: 10.1016/j.maturitas.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 18.Gopinathan NR, Sen RK, Behera P, Aggarwal S, Khandelwal N, Sen M. Awareness of osteoporosis in postmenopausal Indian women: An evaluation of Osteoporosis Health Belief Scale. J Midlife Health. 2016;7:180–4. doi: 10.4103/0976-7800.195697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kadam NS, Chiplonkar SA, Khadilkar AV, Khadilkar VV. Prevalence of osteoporosis in apparently healthy adults above 40 years of age in Pune City, India. Indian J Endocrinol Metab. 2018;22:67–73. doi: 10.4103/ijem.IJEM_438_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rajan R, Paul J, Kapoor N, Cherian KE, Paul TV. Postmenopausal osteoporosis-An Indian perspective. Curr Med Issues. 2020;18:98–104. [Google Scholar]
- 21.Cline RR, Worley MM. Osteoporosis health beliefs and self-care behaviors: An exploratory investigation. J Am Pharm Assoc. 2006;46:356–63. doi: 10.1331/154434506777069534. [DOI] [PubMed] [Google Scholar]
- 22.Senthilraja M, Cherian KE, Jebasingh FK, Kapoor N, Paul TV, Asha HS. Osteoporosis knowledge and beliefs among postmenopausal women: A cross-sectional study from a teaching hospital in southern India. J Family Med Prim Care. 2019;8:1374–8. doi: 10.4103/jfmpc.jfmpc_95_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Varghese A, Siva R, Paul TV, Selvaraj KG. Risk factors and knowledge of osteoporosis in rural pre-menopausal women. Indian Journal of Continuing Nursing Education. 2019 Jan 1;20:22. [Google Scholar]
- 24.Thakur P, Kuriakose C, Cherian KE, Asha HS, Kapoor N, Paul TV. Knowledge gap regarding osteoporosis among medical professionals in Southern India. J Eval Clin Pract. 2020;26:272–80. doi: 10.1111/jep.13164. [DOI] [PubMed] [Google Scholar]
- 25.Johnson CS, McLeod W, Kennedy L, McLeod K. Osteoporosis health beliefs among younger and older men and women. Health Educ Behav. 2008;35:721–33. doi: 10.1177/1090198107301331. [DOI] [PubMed] [Google Scholar]
- 26.Castel H, Bonneh DY, Sherf M, Liel Y. Awareness of osteoporosis and compliance with management guide-lines in patients with newly diagnosed low-impact fractures. Osteoporos Int. 2001;12:559–64. doi: 10.1007/s001980170077. [DOI] [PubMed] [Google Scholar]
- 27.Sedlak CA, Doheny MO, Jones SL. Osteoporosis prevention in young women. Orthop Nurs. 1998;17:53–60. [PubMed] [Google Scholar]


