Abstract
Introduction:
Although various measures are taken to create awareness about the epidemiological features of leprosy and encourage health-seeking behavior, they have seldom been able to tackle the high incidence of new leprosy cases in India.
Objective:
To determine Leprosy-related knowledge, attitude, and health seeking behavior among the urban population in Kancheepuram district of Tamil Nadu.
Materials and Methods:
This community-based cross-sectional study was conducted among a sample size of 640 people above 18 years of age residing in the study area, selected by multistage random sampling. A structured pretested questionnaire was used for data collection, and the data analysis was done using SPSS version 22.
Results:
Among the study participants, 54.7% of the participants had adequate knowledge and 23.3% had favorable attitude towards leprosy. With regard to knowledge, 66% of the participants believe that leprosy is a serious disease, and 71.2% of them were aware of transmission of leprosy from person to person. With regard to attitude, 57.7% were afraid of being diagnosed with leprosy, and 57% felt compassion and desire to help those diagnosed with leprosy. With regard to health-seeking behavior, around 83% preferred treatment from government hospitals and allopathic treatment. Male sex, occupation, education, and marital status were found to be having statistically significant association with knowledge, while the latter two were found to be associated with favorable attitude towards leprosy.
Conclusion:
Unfavorable attitude and inadequate knowledge regarding leprosy was found among the study participants. Behavior change communication programs have to be enhanced at community level to improve the knowledge and attitude regarding leprosy among the population.
Keywords: Awareness, Hansen's disease, NLEP, social stigma
Introduction
Leprosy is one of the oldest diseases of mankind and yet persists as a public health problem in many parts of the world. It is an infectious disease caused by Mycobacterium leprae and primarily affects the skin and peripheral nerves.[1] The mode of transmission is believed to occur through droplet spread or prolonged skin contact with an untreated leprosy patient. Patients with leprosy who present at later stages of the disease usually develop irreversible disabilities and disfigurement.[2] Physical deformities in addition to socio-cultural misconceptions about leprosy have led to social stigma and discrimination of “People With Leprosy” (PWL) throughout history. Social stigma has been a major factor contributing to delay in seeking treatment by leprosy patients. This has been a significant obstacle to early detection, prompt treatment, and cure of leprosy patients.[3]
Despite advances in the treatment of leprosy and a significant reduction in the disease burden worldwide, further reduction in the burden poses enormous challenges. In India, the National Leprosy Control Programme (NLCP) was launched in the year 1955, which was later modified into the National Leprosy Eradication Programme (NLEP) in 1983. India achieved a leprosy elimination target of less than one case per 10,000 population at the national level in December 2005 following which leprosy services were integrated with the General Health Services and Information Education & Communication (IEC) activities pertaining to leprosy lost its importance. Funds allocation for leprosy also got reduced as more money was channelized for diseases such as HIV and TB.[4]
The current global prevalence of leprosy is estimated by the World Health Organization (WHO) to be 0.2 per 10,000 population (2018). India, Brazil, and Indonesia were the only countries in the world where more than 10,000 new cases were reported per year. Out of the 202,226 new leprosy cases detected globally in the year 2019, about 56.6% were from India. The WHO global leprosy strategy (2016-20) envisions to create a leprosy-free world with zero disease, zero transmission, zero stigma and discrimination, and zero disability due to leprosy.[5] In spite of the great achievement and progress towards elimination of leprosy, there is still apprehension, fear, and ignorance about leprosy among the common man in our country, which needs to be addressed in order to educate the public about the possibilities of eliminating leprosy soon.
The involvement of communities plays a significant role in bringing down the incidence of leprosy. The population should have the correct knowledge about the disease, symptoms, transmission, and they should be aware of when and where to take treatment for leprosy. Even though one of NLEP's main objectives is to create awareness about the early identification of signs and symptoms of leprosy and to encourage health-seeking behavior, the community level reality is far from encouraging which is reflected in the high incidence of new cases of leprosy in India. In this background, the study was conducted with an aim to determine leprosy-related knowledge, attitude, and health-seeking behavior among the urban population in Kancheepuram district of Tamil Nadu State.
Methods
Study design, area, and population: This community-based cross-sectional descriptive study was conducted in the urban field practice area attached to our Medical College in Anakaputhur in the Kancheepuram district of Tamil Nadu. Anakaputhur is a municipality consisting of 18 wards with a total population of 48,050 as per census 2011.[6] The study period was from December 2019 to February 2020.
Sample size and sampling technique: A study done by Indira Danturty et al. found that 44% of the participants were aware of the cause of leprosy.[7] Taking this as a reference value, the sample size for this study was calculated by using the formula Z2pq/l2, where P is 44 and q is 56, at a 95% confidence interval (CI) and keeping the margin of error (l) as 4. The sample size calculated was 592 and adjusting for non-response, the sample size was rounded off to 640.
Among the 18 wards in Anakaputhur, 4 wards were randomly chosen by lottery method, and from the electoral roll names and addresses of each adult member were taken.[8] From each ward, 160 adults above the age of 18 years were chosen using the research randomizer website to get the total number of the required sample size.[9] The names and addresses of persons corresponding to the random numbers were noted and visited for data collection. If the person corresponding to the random number was not available or not willing to participate in the study, the next random number was chosen. A similar technique was followed till the required sample size was reached.
Inclusion and exclusion criteria: Any adult above the age of 18 years, residing in Anakaputhur for a minimum period of 1 year, and willing to participate in the study was included in the study.Those who are chronically ill, known leprosy patients, and those residents whose houses were locked during the visits were excluded from the study.
Data collection: Data were collected from eligible and willing participants using a pretested structured questionnaire by face-to-face interviews visiting their houses by the investigators. The questionnaire contained sections on socio-demographic information, knowledge on the cause, transmission, and symptoms of leprosy, treatment of leprosy, attitude towards the disease, and healthcare-seeking practices of the study participants.
Data analysis: Thedata were entered in Microsoft Excel and analyzed using SPSS software version 22.0. Descriptive statistics were used to summarize the socio-demographic characteristics and their level of knowledge, attitude, and health-seeking behavior. Odds Ratio, Chi square test, and P value were used to assess the association between socio-demographic characteristics and the overall knowledge and attitude about leprosy.
Outcome variables: The outcome variables in this study were knowledge and attitude towards leprosy among the study participants. Each outcome was measured using the correct answers given by the study population to several questions. A pilot study was carried out in a neighboring area among 30 participants using this structured questionnaire through which a scoring system was developed for knowledge and attitude domains based on the responses given by the participants. For these domains, if the overall score was more than 50% (if they answered more than half of the questions correctly), the participant was considered to have adequate knowledge/favorable attitude, respectively, towards the disease.
Ethical approval and informed consent: The study was carried out after obtaining the approval of the Institutional Ethics Committee of our Medical College. [Ref: 002/SBMC/IHEC/2020/1350.] A written informed consent was obtained from all the participants after explaining the purpose of the study.
Results
Socio-demographic characteristics of the study population: Among 640 participants, the majority were between 20 and 70 years and were almost equally distributed among the age groups. The study population had an almost equal number of female (50.2%) and male (49.8%) respondents.
The majority belonged to the Hindu religion (84.5%). Nearly 78.1% of the respondents were married. About 89.2% of the respondents belonged to nuclear families and 26.1% completed high school education while 19.1% were illiterate. About 29.4% were unemployed and 26.3% were employed in semiskilled work. According to the modified BG Prasad socioeconomic classification (2019), 38.1% belong to the upper middle class and 25.5% to the middle class [Table 1].
Table 1.
Socio demographic characteristics of the study population
| Characteristics | Number (n=640) | Percentage |
|---|---|---|
| Age in years | ||
| 20-30 | 166 | 25.9 |
| 31-40 | 131 | 20.5 |
| 41-50 | 126 | 19.7 |
| 51-60 | 93 | 14.5 |
| 61-70 | 124 | 19.4 |
| Sex | ||
| Female | 321 | 50.2 |
| Male | 319 | 49.8 |
| Religion | ||
| Hindu | 541 | 84.5 |
| Christian | 41 | 6.4 |
| Muslim | 58 | 9.1 |
| Marital status | ||
| Single | 110 | 17.2 |
| Married | 500 | 78.1 |
| Divorced/Separated/Widowed | 30 | 4.7 |
| Educational qualification | ||
| Graduate/Post graduate/Professional | 89 | 13.9 |
| Intermediate/Post High school diploma | 96 | 15.0 |
| High school | 167 | 26.1 |
| Middle school | 111 | 17.3 |
| Primary school | 55 | 8.6 |
| Illiterate | 122 | 19.1 |
| Occupation | ||
| Professional/Semi-professional | 123 | 19.3 |
| Clerical/Skilled worker | 82 | 12.8 |
| Semi-skilled worker | 168 | 26.3 |
| Unskilled worker | 79 | 12.3 |
| Unemployed | 188 | 29.4 |
| Type of family | ||
| Nuclear | 571 | 89.2 |
| Joint | 33 | 5.2 |
| Three generation | 36 | 5.6 |
| Socio economic class | ||
| Upper class | 136 | 21.3 |
| Upper middle class | 244 | 38.1 |
| Middle class | 163 | 25.5 |
| Lower middle class | 90 | 14.1 |
| Lower class | 7 | 1.1 |
[Table 1: Socio Demographic Profile of the study population]
Knowledge of the study participants on leprosy: About 54.7% of respondents were found to have adequate knowledge about leprosy. Nearly 39% of them came to know about leprosy through family members, friends, and relatives followed by newspapers (20.2%) and health workers (16.3%). Nearly 58% of the subjects said that they have seen at least one person with leprosy. The majority of the respondents (66%) were aware that leprosy is a serious disease [Table 2].
Table 2.
Knowledge on epidemiology, clinical features, treatment, and preventive measures of leprosy
| Knowledge on leprosy | Frequency n=640 | Percentage |
|---|---|---|
| Sources of information about leprosy | ||
| Newspapers/Magazines/Banners/Posters | 144 | 22.5 |
| Radio, TV | 91 | 14.2 |
| Social Media | 38 | 5.9 |
| Doctor/Health worker | 104 | 16.3 |
| Family members/friends/neighbors/teachers | 249 | 39 |
| Others (hospital/public/temple/books) | 14 | 2.1 |
| Seen someone with leprosy | ||
| Yes | 371 | 58 |
| No | 269 | 42 |
| Leprosy is a serious disease | ||
| Yes | 422 | 66 |
| No | 218 | 34 |
| Leprosy is a serious problem in India | ||
| Yes | 369 | 57.7 |
| No | 271 | 42.3 |
| Causes of leprosy | ||
| Germs/bacteria | 304 | 47.5 |
| Poor hygiene | 191 | 29.8 |
| Living in close contact with a leprosy patient | 76 | 11.9 |
| Curse or spell/Punishment from God for sin | 22 | 3.4 |
| Runs in family (Heredity) | 26 | 4.1 |
| Marrying from a family that has leprosy patient | 5 | 0.8 |
| Do’t know | 16 | 2.5 |
| Transmission of leprosy from person to person | ||
| Yes | 456 | 71.2 |
| No | 184 | 28.8 |
| Mode of transmission of leprosy (n=456) | ||
| Through close contact/handshakes | 304 | 66.7 |
| Through the air when a person with Leprosy coughs or sneezes | 88 | 19.3 |
| Through sharing dishes & eating from the same plate | 14 | 3.1 |
| Through touching/using items used by the patients | 50 | 10.9 |
| Signs and symptoms of Leprosy | ||
| Numbness | 64 | 10 |
| Loss of sensation [touch/pain/temperature] | 166 | 26 |
| Skin patches | 281 | 44 |
| Skin ulcers | 59 | 9.2 |
| Nerve thickening | 1 | 0.1 |
| Muscle weakness | 20 | 3.1 |
| Paralysis | 33 | 5.1 |
| Don’t know | 16 | 2.5 |
| Leprosy is a treatable disease | ||
| Yes | 351 | 54.8 |
| No | 289 | 45.2 |
| Preventive measures for leprosy | ||
| Avoid close contacts andnd sharing their belongings | 334 | 52.1 |
| Maintaining personal hygiene | 156 | 24.4 |
| Through good nutrition | 46 | 7.2 |
| By praying | 5 | 0.8 |
| Do not know | 99 | 15.5 |
[Table 2: Knowledge on epidemiology, clinical features, treatment, and preventive measures of leprosy]
The major causes of leprosy as informed by participants were germ/bacteria (47.5%), poor hygiene (29.8%), and close contact with an affected individual (11.9%). Awareness about leprosy as a contagious disease was informed by 71.2% of the participants, of which about 19.3% of the respondents informed that the mode of transmission is through airborne droplets. The majority of the participants believed that handshake/close contact (66.7%) was the mode of transmission, while the remaining responses were through sharing utensils (3.1%), and fomite transmission (10.9%) [Figure 1].
Figure 1.
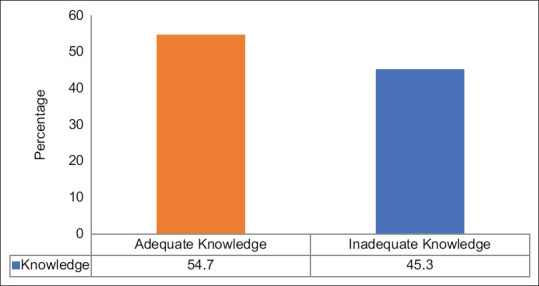
Graph showing the overall level of knowledge related to leprosy
[Figure 1: Graph showing the overall level of knowledge related to leprosy]
The attitude of the study participants towards leprosy: Almost 76.7% of the respondents had an unfavorable attitude towards leprosy. [Figure 2] Almost 81.5% of the subjects refused to be in close contact with leprosy patient and 75.8% of them won't be sharing personal belongings such as clothes and utensils with leprosy patients. Nearly 61.6% said that they will not sit next to a leprosy person. When asked if they would reveal their disease status if they were diagnosed with leprosy, almost 61.6% of them replied negatively. The majority of the study subjects (81.4%) informed that they will not allow their children to play with children of people having leprosy, and nearly 41.9% of the subjects denied marrying a leprosy-affected individual. The respondents gave equal response when enquired about the possibility of providing job opportunities for leprosy patients in the society [Table 3].
Figure 2.
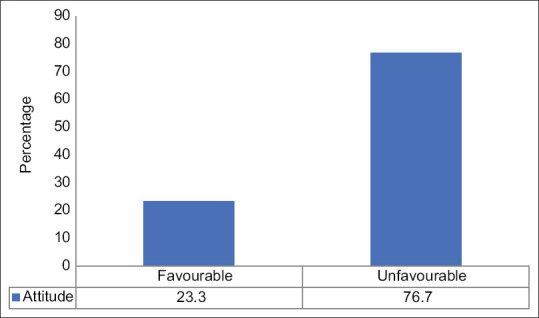
Graph showing the overall level of attitude related to leprosy
Table 3.
Attitude of the study participants towards leprosy patients (n=640)
| Attitude towards leprosy patients | Response: No | Response: Yes | ||
|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | |
| Close contact with leprosy patient | 520 | 81.5 | 120 | 18.5 |
| Share personal belongings like utensils with leprosy patient | 485 | 75.8 | 155 | 24.2 |
| Will sit next to a leprosy patient. | 394 | 61.6 | 246 | 38.4 |
| Reveal disease status | 394 | 61.6 | 246 | 38.4 |
| Children are left to play with children of leprosy patient | 521 | 81.4 | 119 | 18.6 |
| Leprosy patients are difficult to get married | 268 | 41.9 | 372 | 58.1 |
| People with leprosy may participate in activities | 360 | 56.3 | 280 | 43.7 |
| Job opportunities for leprosy patients | 319 | 49.8 | 321 | 50.2 |
[TABLE 3: Attitude of the study participants towards leprosy patients]
[Figure 2: Graph showing overall level of attitude related to leprosy.]
Regarding attitude, if diagnosed with leprosy, the majority replied that they would experience fear (57.7%) followed by hopelessness (13.3%) and surprise (11.7%) and only 6.5% of the participants had a confident attitude [Figure 3].
Figure 3.
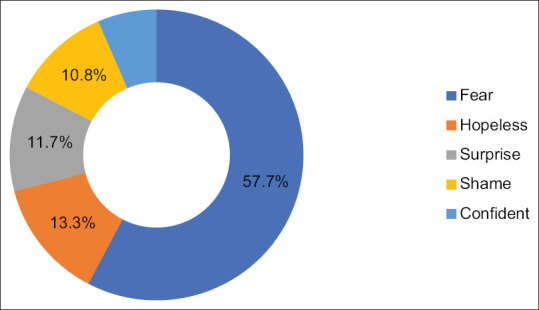
Attitude of participants if being diagnosed with leprosy
[Figure 3: Attitude of participants if being diagnosed with Leprosy]
Regarding attitude towards PWL, the majority had a desire to help (57%) while 26% said they would feel compassionate but still decided to stay away from them [Figure 4].
Figure 4.
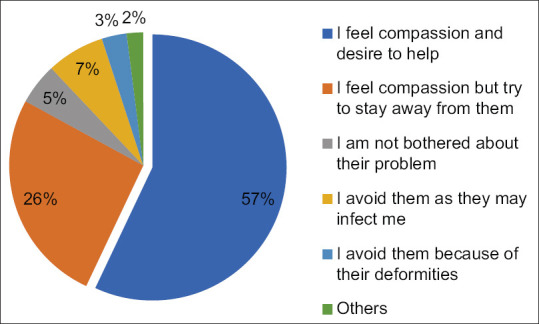
Attitude of participants towards people with leprosy
[Figure 4: Participants Attitude towards People with Leprosy]
Health seeking behavior of the study population towards leprosy: When asked about the choice of place of treatment, almost 82.2% of them informed that they will choose government hospitals followed by private clinics (10.3%). The majority of the study participants (83.6%) responded that they will recommend allopathic treatment for leprosy.
Around 60.2% of the study subjects responded that they would seek immediate medical attention if they developed any symptoms of leprosy. Nearly 37.9% of the participants said that due to out of pocket expenditure, they would delay medical attention.
[Table 4: Health seeking behavior of participants towards leprosy]
Table 4.
Health seeking behavior of participants towards leprosy
| Health seeking behavior | Frequency n=640 | Percentage |
|---|---|---|
| Choice of treatment | ||
| Govt. hospital | 526 | 82.2 |
| Private clinic/hospital | 66 | 10.3 |
| AYUSH practitioners | 12 | 1.9 |
| Self-medication | 17 | 2.7 |
| Pharmacy | 17 | 2.7 |
| Traditional healers | 2 | 0.2 |
| Suggestion to seek treatment | ||
| Allopathic medicine | 535 | 83.6 |
| AYUSH medicine | 27 | 4.2 |
| Traditional healers | 38 | 5.9 |
| Pharmacy | 3 | 0.5 |
| Self Medication | 7 | 1.1 |
| Don’t know | 30 | 4.7 |
| Choice of contact after being diagnosed with leprosy | ||
| Doctor or other medical worker | 411 | 64.2 |
| Spouse/Parent/Children | 147 | 22.9 |
| Close friend | 22 | 3.4 |
| Other family member | 26 | 4.1 |
| No one | 34 | 5.3 |
| Facility suggested for leprosy management | ||
| Allopathic Health facilities | 544 | 85 |
| AYUSH Health facilities | 19 | 3 |
| Traditional healers | 26 | 4.1 |
| Pharmacist | 11 | 1.7 |
| Self-medication | 12 | 1.9 |
| Don’t know | 26 | 4.1 |
| Church | 2 | 0.3 |
| Time to seek medical attention in case of suspicion | ||
| When treatment on my own doesn’t work | 152 | 23.8 |
| As soon as I realize the symptoms could be due to leprosy | 385 | 60.2 |
| Don’t know | 103 | 16 |
| Reasons for delay in treatment | ||
| Not sure where to go | 275 | 43 |
| High cost involved | 243 | 37.9 |
| Cannot leave work | 34 | 5.3 |
| Do not want to find out that something is really wrong | 51 | 8 |
| Difficulties with transportation/distance to clinic | 24 | 3.7 |
| Do not trust/like medical workers | 13 | 2.1 |
Factors associated with participants' overall knowledge and attitude on leprosy: Table 5. Part-A shows that the factors found to be having a statistically significant association with adequate knowledge were, males when compared to females (OR-1.5, 95% CI: 1.11-2.07, P-0.01), those who completed schooling when compared to those not complete schooling (OR-3.1, 95% CI: 2.14-4.54, P-0.001), professional, skilled, and semiskilled workers when compared to unskilled and unemployed (OR-1.5, 95% CI: 1.13-2.13, Pp-0.007), singles when compared to those married, widowed, or divorced. (OR-1.89, 95% CI: 1.22-2.91, P-0.005).
Table 5.
Association between socio demographic factors with knowledge and attitude towards leprosy
| Part-A: Association of Socio demographic factors and knowledge on leprosy | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Adequate knowledge n=350 | Inadequate knowledge n=290 | OR | 95% CI | Chi square | P | ||
| n | % | n | % | |||||
| Sex | ||||||||
| Male | 191 | 60 | 128 | 40 | 1.5 | 1.11-2.07 | 6.49 | 0.01* |
| Female | 159 | 50 | 162 | 50 | ||||
| Education | ||||||||
| Completed schooling | 136 | 74 | 49 | 26 | 3.1 | 2.14-4.54 | 36.1 | 0.001* |
| Not Completed schooling | 214 | 47 | 241 | 53 | ||||
| Occupation | ||||||||
| Prof/skilled/semiskilled | 221 | 59 | 152 | 41 | 1.5 | 1.13-2.13 | 7.07 | 0.007* |
| Unskilled/unemployed | 129 | 48 | 138 | 52 | ||||
| Marital status | ||||||||
| Single | 74 | 67 | 36 | 33 | 1.89 | 1.22-2.91 | 7.88 | 0.005* |
| Married/divorced/Widowed | 276 | 52 | 254 | 48 | ||||
| Part-B: Association of Socio demographic factors and attitude towards leprosy | ||||||||
| Variables | Favorable attitude n=149 | Unfavorable attitude n=491 | OR | 95% CI | Chi square | P | ||
| Education | ||||||||
| Completed schooling | 55 | 29.8 | 130 | 70.2 | 1.62 | 1.10-2.39 | 5.56 | 0.01* |
| Not Completed schooling | 94 | 20.6 | 361 | 79.4 | ||||
| Marital status | ||||||||
| Single | 42 | 38.1 | 68 | 61.9 | 2.44 | 1.57-3.79 | 16.5 | <0.001* |
| Married/divorced/Widowed | 107 | 2.02 | 423 | 79.8 | ||||
*P<0.05 Statistically Significant at 95% Confidence Interval. OR=Odds Ratio
Table 5 Part-B shows the statistically significant association of factors with the overall attitude of the study participants towards leprosy, which was found among those who completed schooling when compared to those not complete schooling (OR-1.62, 95% CI: 1.10-2.39, P-0.01) and among singles when compared to those married, widowed, or divorced. (OR-2.44, 95% CI: 1.57-3.79, P < 0.001).
[Table 5: Association between Socio Demographic Factors with Knowledge and Attitude towards leprosy]
Discussion
This community-based cross-sectional study on knowledge, attitude, and health seeking behaviour regarding Leprosy among the adult population in an urban area of Kancheepuram district; Tamil Nadu shows very interesting outcomes that are discussed here.
Knowledge of Leprosy: This study showed that nearly 45% of respondents had inadequate knowledge of leprosy. A similar finding was reported by a study conducted by Raju MS et al., where 35%–50% of the participants were noted to have adequate knowledge on leprosy, but the attitude was more in negative.[10] A study done in Eastern Ethiopia found that 56.91% had high knowledge of leprosy.[11] A study conducted by Mohite RV et al. in a rural community in Karad reported that nearly 79% of respondents had good knowledge and 69% had a positive attitude towards leprosy.[12] Singh R et al. in a community-based study in Nepal noted that only 42% of the study population had good knowledge and a favourable attitude on leprosy.[13] This shows that the knowledge and attitude of the population towards leprosy is still low despite the disease being eliminated from the country.
Awareness of signs and symptoms: Regarding awareness of signs and symptoms of leprosy, 44% of the study participants reported that skin patches followed by loss of sensation (26%), numbness (10%), and skin ulcers (9.2%) as signs and symptoms. Tesema AA et al. in their study carried out in Ethiopia, 45% of the study participants reported a loss of sensation as the main symptom, 17% identified skin patches as the presenting symptom, and 70% knew that leprosy can present with deformities.[14] Mohite RV et al. in a similar study reported that around 82% of their study respondents were knowledgeable about the symptoms and signs of leprosy.[12] Singh R et al. also reported a higher proportion (81%) of the participants being aware of the signs and symptoms. Around 46.8% reported involvement of skin as the first symptom/sign, 3.1% reported involvement of nerves, and 31.2% reported both.[13] Stephen T et al. in a study in Tamil Nadu noted that 55% of the patients with leprosy and 73% of their family members were aware of skin patches and loss of sensation as presenting symptoms of the disease.[15] The importance of the knowledge on the symptoms and signs of leprosy is crucial in avoiding the delay in seeking health care.
Cause of leprosy: About 47.5% of the respondents knew the correct cause of leprosy. A similar finding was noted in the study by Tesema AA et al. where 48.3% reported that leprosy is due to bacteria.[14] A study carried out in Mexico reported nearly 60% of the study participants having knowledge on the cause of leprosy.[16] In the study by Mohite RV et al., nearly 66% of respondents had knowledge on the cause of leprosy.[12] Stephen T et al. in their study in Tamil Nadu noted that 32% of leprosy patients and 37% of their family members were aware of the cause of leprosy.[15] Danturty I et al. in a study carried out in Secunderabad reported that 44% of the participants knew the cause of leprosy.[7] Similar findings were noted in studies carried out in Uttar Pradesh and in Nepal.[13,17]
Treatment of Leprosy: Awareness that leprosy is treatable was noted in around 54.8% of the participants in this study. In the study carried out in Secunderabad, only 29% of the respondents were aware that leprosy is treatable and curable.[7] In the Ethiopian study, a higher proportion of the study subjects (93%) responded that leprosy is treatable with modern drugs.[14] Whereas, the study carried out in Mexico reported that only 31% were aware that leprosy is treatable.[16]
Stigma towards leprosy: The various stigmas towards leprosy were avoidance of contact with a diseased person, not sharing personal belongings, refusal to allow children to mingle with the patients' children, or sitting next to the patient. They expressed negative feelings in the form of fear, hopeless reaction, or shame if they were diagnosed with leprosy. These factors could in turn contribute to the cover-up of the symptoms/signs of the disease. Similar findings were noted among the studies carried out by Singh R et al., Adhikari et al. and Hejinders ML et al.[13,18,19] Owing to these stigmas, leprosy patients tend to suffer from psychosocial problems such as depression and anxiety.[20]
Attitude towards patients with leprosy: This study noted that 76.7% of the respondents had an unfavorable attitude towards patients with leprosy. This finding has been supported by studies carried out in countries such as India, Ethiopia, Nepal, and Nigeria.[13,14,21,22] These studies are strong pieces of evidence to show that myths about leprosy is deep-rooted in the socio-cultural milieu of the communities.
Association of socio-demographic factors: Education, male gender, and employment status were found to have a statistically significant association with knowledge on leprosy, whereas education and marital status were having statistically significant association with attitude on leprosy. Almost similar findings pointing to the importance of better education status were noted in the studies conducted in Ethiopia and Uttar Pradesh, India.[14,17]
The Global Leprosy Strategy 2016-2020 focuses on strengthening the awareness of patients and community on leprosy, promotion of interventions for preventing infection, address all forms of stigma and discrimination and involving communities in the improvement of leprosy services.[5] Recently, India is showing a declining trend in the number of new leprosy cases, pediatric cases, and cases with grade II disability.[23]
The major findings from this study are that more than half of the study participants have inadequate knowledge and an unfavorable attitude towards leprosy. Stigma if diagnosed with leprosy and stigma towards the patients were also found to be prevalent. Male sex, occupation, education, and marital status were found to be having a statistically significant association to knowledge, while the latter two were found to be associated with the favorable attitude towards leprosy.
Role of Primary Health Care and Family Physicians: Objectives of enhancing the knowledge/awareness and creating a favorable attitude and practice towards leprosy and appropriate health-seeking behavior of leprosy patients and their families can be better undertaken through the primary health care services. Primary care and family physicians can play a major role in screening and early diagnosis and treatment of leprosy at the family level both in the urban and rural areas linking with NLEP services.
Strengths and Limitations of the study
This study was conducted by following a strict methodological protocol using a good sample size. The outcome of the study results is an eye-opener and can be considered as a pilot for taking up more such bigger studies. A comparative study analyzing the differences in knowledge, attitude, and health-seeking behavior on leprosy among the urban and rural community, could have given more in-depth insight and information about the status of leprosy, which can be generalized in the community.
Conclusion
This study result shows that the knowledge and attitude on leprosy were grossly unfavorable. The awareness and attitude on leprosy is inadequate inspite of the existence of the National Programme for Leprosy since 1955. This highlights the significance of behaviour change communication (BCC) programs in the community, which could bring a steady improvement in the knowledge and attitude of the population. These programs should be redesigned with the involvement of the community, social activists, local leaders, local family physicians, primary health care providers, and the print and visual media. Health education emphasizing early diagnosis and prompt treatment of leprosy as per the standard treatment guidelines based on NLEP needs to be widely carried out both in rural and urban communities.
Ethical approval
The study was approved by the Institutional Ethics Committee, Sree Balaji Medical College and Hospital. [Ref: 002/SBMC/IHEC/2020/1350.]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We express our gratitude to the faculty, postgraduates, and the field staff of the Department of Community Medicine for their support and guidance in carrying out the study. We sincerely thank all the participants for sparing their valuable time by participating in this study.
References
- 1.Han XY, Silva FJ. On the age of leprosy. PLoS Negl Trop Dis. 2014;8:e2544. doi: 10.1371/journal.pntd.0002544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bratschi MW, Steinmann P, Wickenden A, Gillis TP. Current knowledge on Mycobacterium leprae transmission: A systematic literature review. Lepr Rev. 2015;86:142–55. [PubMed] [Google Scholar]
- 3.Tabah EN, Nsagha DS, Bissek K, Njamnshi TN, Njih N, Pluschke G, et al. Community knowledge, perceptions and attitudes regarding leprosy in rural Cameroon: The case of Ekondotiti and Mbonge health districts in the South-west Region. PLoS Negl Trop Dis. 2018;12:e0006233. doi: 10.1371/journal.pntd.0006233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rao PN, Suneetha S. Current situation of leprosy in India and its future implications. Indian Dermatol Online J. 2018;9:83–9. doi: 10.4103/idoj.IDOJ_282_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. The Global Leprosy Strategy [Internet] Geneva: Available from: http://www.who.int/lep/strategy/en/ cited 2020 Aug 25. [Google Scholar]
- 6.Anakaputhur, Kancheepuram District. Population Census 2011 [Internet] cited 2019 Nov 26. Available from: https://www.census2011.co.in/data/town/803353-anakaputhurtamil-nadu.html .
- 7.Danturty I, Manchala S, Jairaj S. Community based study of knowledge, attitude and practices towards leprosy in an urban slum in Secunderabad, Telangana. J Med Sci Clin Res. 2016;49:13527–31. [Google Scholar]
- 8.Tamil Nadu Government. Election Commission. [Internet] cited 2019 Nov 25. Available from: http//elections.tn.gov.in/DRAFTROLL2018/ac30.htm .
- 9.Research Randomizer. [Internet] cited 2019 Nov 25. Available from: https://www.randomizer.org/
- 10.Raju MS, Kopparty SN. Impact of knowledge of leprosy on the attitude towards leprosy patients: A community study. Indian J Lepr. 1995;67:259–72. [PubMed] [Google Scholar]
- 11.Urgesa K, Bobosha K, Seyoum B, Geda B, Weldegebreal F, Mihret A, et al. Knowledge of and attitude toward leprosy in a leprosy endemic district, Eastern Ethiopia: A community-based study. Risk Manag Healthc Policy. 2020;13:1069–77. doi: 10.2147/RMHP.S254625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohite RV, Mohite VR. Knowledge and attitude of Indian rural community towards leprosy after post elimination phase: A survey from Karad Block, India. Natl J Community Med. 2016;7:797–801. [Google Scholar]
- 13.Singh R, Singh B, Mahato S. Community knowledge, attitude, and perceived stigma of leprosy amongst community members living in Dhanusha and Parsa districts of Southern Central Nepal. PLoS Negl Trop Dis. 2019;13:e0007075. doi: 10.1371/journal.pntd.0007075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tesema AA, Beriso M. Assessment of knowledge and attitude of community on leprosy patients in Kuyera Town, West Arsi Zone, Oromia Region Southeast Ethiopia. Hereditary Genet. 2015;5:156. [Google Scholar]
- 15.Stephen T, Selvaraj I, Parmeswari PJ. Assessment of knowledge, attitude and practice about leprosy among patients and their families in a rural community in Tamil Nadu. Indian J Lepr. 2014:86;7–14. [PubMed] [Google Scholar]
- 16.Graciano Machuca O, Velarde de la Cruz EE, Ramírez Dueñas MG, Alvarado Navarro A. University students' knowledge and attitudes towards leprosy. J Infect Dev Ctries. 2013;7:658–64. doi: 10.3855/jidc.2626. [DOI] [PubMed] [Google Scholar]
- 17.Barkataki P, Kumar S, Rao PS. Knowledge of and attitudes to leprosy among patients and community members: A comparative study in Uttar Pradesh, India. Lepr Rev. 2006;77:62–8. [PubMed] [Google Scholar]
- 18.Adhikari B, Shrestha K, Kaehler N, Raut S, Chapman RS. Community attitudes towards leprosy affected persons in Pokhara municipality of western Nepal. J Nepal Health Res Counc. 2013;11:264–8. [PubMed] [Google Scholar]
- 19.Heijnders ML. The dynamics of stigma in leprosy. Int J Lepr Other Mycobact Dis. 2004;72:437–47. doi: 10.1489/1544-581X(2004)72<437:TDOSIL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Somar PM, Waltz MM, van Brakel WH. The impact of leprosy on the mental wellbeing of leprosy-affected persons and their family members – A systematic review? Glob Mental Health (Camb) 2020;7:e15. doi: 10.1017/gmh.2020.3. doi: 10.1017/gmh.2020.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Stigter DH, de Geus L, Heynders ML. Leprosy: Between acceptance and segregation. Community behaviour towards persons affected by leprosy in eastern Nepal. Lepr Rev. 2000;71:492–8. doi: 10.5935/0305-7518.20000051. [DOI] [PubMed] [Google Scholar]
- 22.Ogban GI, Iwuafor AA, Emanghe UE, Ushie SN, Ndueso EM, Ejemot-Nwadiaro RI, et al. Unfavorable attitude and perceived stigma towards leprosy: A concern for status perpetuation in a community in Cross River State, Nigeria. Asian J Med Health. 2020;18:1–13. [Google Scholar]
- 23.World Health Organization. Leprosy: New data show steady decline in new cases [Internet] Geneva: cited 2020 Aug 25. Available from: http://www.who.int/neglected_diseases/news/Leprosy-new-data-show-steady-decline-in-newcases/en/ [Google Scholar]


