Abstract
Neutrophilic dermatosis of the hands (NDH) is a rare localized acral variant of Sweet syndrome. NDH predominantly involves the dorsal hands with characteristic dense dermal neutrophilic infiltrate with an upper dermal edema observed on histopathology. Unusual findings like palmar involvement and predominant lymphomononuclear dermal infiltration in our case with NDH, makes it an interesting read.
Key Words: Acral Sweet sysndrome, lymphocytic infiltration, neutrophilic dermatosis of the hands, palmar involvement
Introduction
Neutrophilic dermatosis of the hands (NDH), a rare localized acral variant of Sweet syndrome,[1] is characterized by tender erythematous plaques, pustules, bullae, and/or ulcers usually limited to the dorsal hands. Typically, dense dermal neutrophilic infiltrate with an upper dermal edema are observed on histopathology. Extensive search in PubMed and MedLine databases revealed NDH with palmar involvement along with dermal lymphocytic infiltration to be rarely described in literature. Here, we describe a case of NDH involving the palms which on histopathological examination, showed predominantly dermal lymphomononuclear cell infiltrate.
Case Report
An otherwise healthy 45-year-old gentleman presented with fever and abrupt onset multiple painful reddish bumps over both hands and feet for the past one week. Prior to his present consultation, he had been prescribed a course of systemic antibiotic (azithromycin) and antiviral (acyclovir) by his family physician without significant response. He had no complaints of cough, respiratory distress, joint pain, altered bowel habit, preceding drug ingestion, any drug allergy, or other features suggestive of systemic involvement. His family history was not significant.
Examination revealed multiple tender, erythematous to slightly violaceous plaques symmetrically distributed over palmar surfaces of both hands and the dorsal areas of feet; few lesions showed mild desquamation while a pseudo-vesicular appearance could be appreciated over larger plaques [Figure 1]. Other muco-cutaneous sites were unaffected and systemic examination was unremarkable.
Figure 1.

Multiple erythematous to violaceous plaques symmetrically distributed over both palms and the dorsa of feet. Larger lesions showing pseudo-vesicular appearance
Laboratory analysis was notable for leukocytosis (14.3 × 109/L, reference range 4 – 11 × 109/L) with neutrophilia (10.4 × 109/L, reference range 2.5 – 7.7 × 109/L), elevated erythrocyte sedimentation rate (48 mm/hr, range 0-15 mm/hr) and elevated C–reactive protein level. Antinuclear antibody (ANA) titer in Hep2 cell line and serology for viral hepatitis markers, herpes simplex virus 1, 2 antibodies and human immunodeficiency virus were negative. Routine urine examination, skiagram chest, ultrasound whole abdomen failed to detect any abnormality. Skin biopsy was done from a 6-day old lesion over palm. Histopathological examination showed marked edema of the papillary dermis with upper and mid-dermal perivascular infiltrate comprising predominantly lymphomononuclear cells with extravasation of erythrocytes; no feature of vasculitis was elicited [Figure 2a and b].
Figure 2.
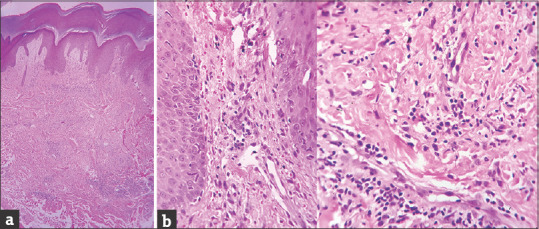
(a): Histopathological examination showing marked papillary dermal edema with upper and mid-dermal lymphomononuclear cell infiltrate (H&E, 40×). (b): Higher magnification showing papillary dermal and perivascular infiltrate, consisting of predominantly lymphocytes, very few neutrophils with few extravasated erythrocytes. No features of vasculitis seen (H&E, 400×)
Significant improvement of the lesions [Figure 3] and subsidence of symptoms were observed after 7-day treatment with oral prednisolone (40 mg/day).
Figure 3.

Significant improvement of the lesions following treatment with systemic corticosteroid
Based on the clinico-pathological findings and the response to treatment, a diagnosis of NDH was established.
Discussion
Acute febrile neutrophilic dermatosis (Sweet syndrome), as described by R.D. Sweet way back in 1964, is characterized by a dermal neutrophilic infiltration and leukocytoclasis, without any evidence of vasculitis.[2] In 1995, Strutton described six cases with eruption involving the dorsal of the hands.[3] These lesions clinically simulated Sweet Syndrome (SS) but in all the cases evidence of leukocytoclastic vasculitis was evident. This prompted the authors to propose a new entity called “Pustular Vasculitis of the Hands”.[4] In 2000, Galaria et al. reported three cases with similar clinical features but histology showed neutrophilic infiltration and leukocytoclasis without vasculitis features. Owing to the overlapping clinical and histopathological presentation of these two conditions, Galaria et al. offered a unified designation of “neutrophilic dermatosis of the dorsal hands”, suggesting that it be a subset of SS. However, as per few previous case reports[1] and palmar involvement as seen in our patient, we excluded the term “dorsal” from our diagnosis. A comparison between the clinico-histopathological features of classic Sweet syndrome, NDH, and the present case has been depicted in Table 1.[5,6,7]
Table 1.
Comparison between the clinico-histological features of classic Sweet syndrome, neutrophilic dermatosis of hands and the present case
| Classic Sweet syndrome[5] | Neutrophilic Dermatosis of Hands[6] | Our Case | |
|---|---|---|---|
| Clinical features | Non-pruritic, tender, erythematous papules and plaques with pseudo-vesiculation (mammillated surface). Atypical presentation: biopsy, taken from a well-developed lesion, showed predominantly, pyoderma gangrenosum-like, erysipelas-like. Face, neck, and upper extremities usually involved. Accompanied by constitutional symptoms. |
Morphologically identical to classic Sweet syndrome Mostly restricted to the dorsal hands. Rarely involve palms and dorsa of feet. Constitutional symptoms can be seen. |
Multiple tender, erythematous to violaceous plaques with pseudo-vesicular appearance involving both palms and dorsa of feet. Accompanied by constitutional symptoms. |
| Histopathological features | Epidermis- usually normal. Spongiosis and subcorneal pustules may be seen. Papillary dermal edema with diffuse and perivascular infiltrate, predominantly neutrophilic, with occasional features of leukocytoclastic vasculitis. Infiltration may occasionally involve the subcutaneous tissue. Atypical variants: histiocytoid, lymphocytic, and eosinophilic. |
Basic histopathology is similar to classic Sweet syndrome. Only one case of lymphocytic variant reported previously.[7] |
Epidermis- not involved Papillary dermal edema, upper and mid-dermal perivascular infiltrate predominantly lymphocytic, with extravasation of erythrocytes. No vasculitis or subcutaneous tissue involvement. |
| Associated conditions | Infections Malignancy: hematological and solid organ Inflammatory bowel disease Drugs Pregnancy Autoimmune disorders: autoimmune connective tissue disorders, sarcoidosis, Behcet’s disease |
Haematological disorders Infection Solid organ tumour Inflammatory bowel disease |
Nothing found |
NDH has been reported to be associated with solid organ malignancies (lung, larynx, kidney, and colon), hematological disorders (myelodysplastic syndrome, monoclonal gammopathy, multiple myeloma, acute myeloid leukemia, and polycythemia), autoimmune diseases, inflammatory bowel disease (ulcerative colitis, Crohn's disease), infections (mostly respiratory), and drugs.[6,7] Our patient was thoroughly evaluated but no such underlying association was found.
In most of the reported cases of NDH, histopathology showed predominantly upper dermal neutrophilic and perivascular infiltrate with or without features of leukocytoclastic vasculitis. In a recent case report, Peteln et al. described a case of NDH with perivascular and interstitial lymphocytic infiltration where biopsy was taken from a 1- to 2-day-old pustule.[7] Similar histopathological findings were also corroborated by Kazlouskaya et al.[8] and Jordaan[9] in a few cases of SS. Jordaan postulated that the lymphocytes appeared initially, generated lymphokines that attracted the neutrophils, resulting in a more robust neutrophilic component in the more developed elevated lesions.[9] But in our case the biopsy, taken from a well-developed lesion, showed predominantly lymphomononuclear cell infiltrate without features of vasculitis.
In clinico-histopathological evaluation of hand lesions, consideration of neutrophilic eccrine hidradenitis (neutrophilic infiltrates around eccrine glands with vacuolar alteration and necrosis), chilblain lupus (positive ANA, vacuolar interface dermatitis with dermal mucin, positive direct immunofluorescence test), perniosis (lesions precipitated with cold exposure), arthropod bite reaction (self-limited, visible bite mark, dermal eosinophils), erysipelas (systemic symptoms, vascular ectasia, sparse dermal infiltrate, response to antibiotics), and a drug reaction (anamnesis) ought to be made and ruled out.[7]
NDH is usually responsive to moderate doses of systemic corticosteroids or dapsone,[10] though few cases have reported successful treatment with topical corticosteroids, colchicine, tetracycline, or potassium iodide.[6,11] Our patient responded well to short-course systemic corticosteroid without any recurrence on 6-month follow-up.
Conclusion
The purpose of documenting this case is to highlight the unusual findings of palmar involvement and predominantly lymphomononuclear cell infiltration in NDH, which to the best of our knowledge has not yet been described.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understood that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this article have no conflict of interest.
References
- 1.Wolf R, Tüzün Y. Acral Manifestations of Sweet syndrome (Neutrophilic dermatosis of the hands) Clin Dermatol. 2017;35:81–4. doi: 10.1016/j.clindermatol.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Sweet RD. An acute febrile neutrophilic dermatosis. Br J Dermatol. 1964;76:349–56. doi: 10.1111/j.1365-2133.1964.tb14541.x. [DOI] [PubMed] [Google Scholar]
- 3.Strutton G, Weedon D, Robertson I. Pustular vasculitis of the hands. J Am Acad Dermatol. 1995;32:192–8. doi: 10.1016/0190-9622(95)90125-6. [DOI] [PubMed] [Google Scholar]
- 4.Duquia RP, Almeida HL, Jr, Vettorato G, Souza PR, Schwartz J. Neutrophilic dermatosis of the dorsal of the hands: Acral sweet syndrome? Int J Dermatol. 2006;45:51–2. doi: 10.1111/j.1365-4632.2005.02652.x. [DOI] [PubMed] [Google Scholar]
- 5.Villarreal-Villarreal CD, Ocampo-Candiani J, Villarreal-Martínez A. Sweet syndrome: A review and update. Actas Dermosifiliogr. 2016;107:369–78. doi: 10.1016/j.ad.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Micallef D, Bonnici M, Pisani D, Boffa MJ. Neutrophilic dermatosis of the dorsal hands: A review of 123 cases. J Am Acad Dermatol. 2019 doi: 10.1016/j.jaad.2019.08.070. doi: 10.1016/j.jaad. 2019.08.070. [DOI] [PubMed] [Google Scholar]
- 7.Peteln I, Dolenc-Voljč M, Jurčić V. Neutrophilic dermatosis of the dorsal hands (acral Sweet syndrome) with predominantly lymphocytic dermal infiltrate. J Cutan Pathol. 2020;47:104–7. doi: 10.1111/cup.13589. [DOI] [PubMed] [Google Scholar]
- 8.Kazlouskaya V, Junkins-Hopkins JM. Lymphocytes in Sweet syndrome: A potential diagnostic pitfall. J Cutan Pathol. 2018;45:217–22. doi: 10.1111/cup.13096. [DOI] [PubMed] [Google Scholar]
- 9.Jordaan HF. Acute febrile neutrophilic dermatosis. A histopathological study of 37 patients and a review of the literature. Am J Dermatopathol. 1989;11:99–111. [PubMed] [Google Scholar]
- 10.Weenig RH, Bruce AJ, McEvoy MT, Gibson LE, Davis MD. Neutrophilic dermatosis of the hands: four new cases and review of the literature. Int J Dermatol. 2004;43:95–102. doi: 10.1111/j.1365-4632.2004.01845.x. [DOI] [PubMed] [Google Scholar]
- 11.Bubna AK, Veeraraghavan M, Anandan S, Rangarajan S. Palmoplantar pseudovesicles: An unusual presentation of sweet's syndrome. Indian J Dermatol. 2015;60:94–6. doi: 10.4103/0019-5154.147819. [DOI] [PMC free article] [PubMed] [Google Scholar]


