Sir,
Porokeratosis is a genetically heterogeneous, autosomal dominant, chronic progressive disorder of keratinization, presenting as hyperkeratotic papules or plaques surrounded by distinct peripheral keratotic ridge.[1] Table 1 mentions its clinical variants.[1]
Table 1.
Clinical variants
| Types | Clinical features |
|---|---|
| Porokeratosis of Mibelli (classical form) | Seen in infancy/childhood as small brown to skin-colored annular papules with raised border |
| Disseminated superficial porokeratosis (DSP) | Presents as more generalized processes and involves the extremities in a bilateral, symmetric fashion |
| Disseminated superficial actinic porokeratosis (DSAP) | Most common, presents with multiple, photo distributed, symmetrically distributed papules |
| Linear porokeratosis | Seen at birth/childhood with lesions along the Blaschko’s lines |
| Punctate porokeratosis | Presents as 1-2 mm papules on palms/soles, during or after adolescence |
In all variants (except for punctate type), a thin column of parakeratotic cells (coronoid lamella) corresponds to the hyperkeratotic border and extends throughout the stratum corneum.[1] Porokeratosis is asymptomatic, but pruritic variant,[2] is rare and atypical and is also known as inflammatory DSP, eruptive pruritic papular porokeratosis (EPPP), eruptive disseminated porokeratosis (EDP).[3] Two cases of pruritic porokeratosis, reported for the first time from India, are highlighted. Case 1, a 17-year-old female presented with multiple, itchy, dark raised lesions on neck, upper/lower extremities and buttocks since 4 months, which had aggravated on stress. Cutaneous examination revealed mutiple, hyperpigmented papules, nodules and plaques arranged bilaterally symmetrically on upper and lower limbs with koebnerization on right knee [Figure 1] and on buttocks with excoriations. Isolated discrete papules were seen on chest, back and nape of neck. Biopsy from papule showed coronoid lamella [Figure 2a], hyperkeratosis, irregular acanthosis and superficial lymphocytic infiltrate in upper dermis [Figure 2b]. Diagnosis of EPPP was made on clinicopathological correlation. Case 2, a 28-year-old female presented with dark raised itchy lesions on face, elbow, bilateral buttocks, thighs and lower legs since 5 months, with aggravation on stress. Cutaneous examination revealed multiple, hyperpigmented scaly papules and plaques over face, elbows, thighs, lower limbs [Figure 3a] and buttocks [Figure 3b] with few discrete lesions on the upper back. Biopsy from papule showed similar coronoid lamella [Figure 4] as in case 1, confirming diagnosis of EPPP. Topical 5 Flurouracil was planned for both.
Figure 1.
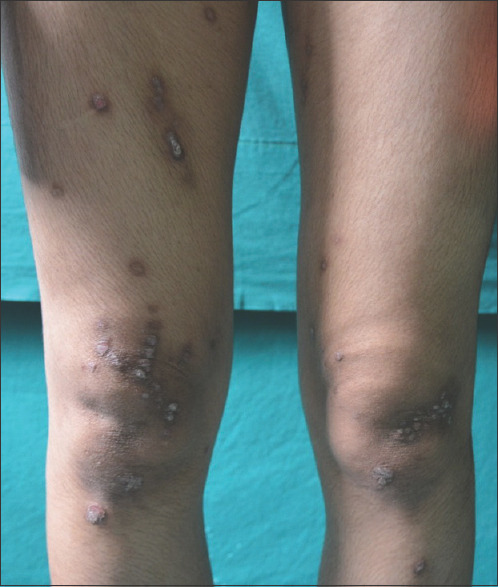
Hyperpigmented papules, nodules and plaques arranged bilaterally symmetrically on lower limbs with koebnerization on right knee
Figure 2.
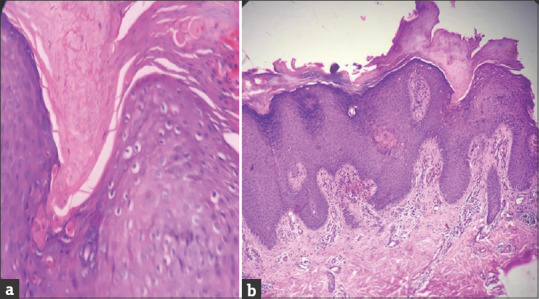
(a) Coronoid lamella. (b) Compact hyperkeratosis, irregular acanthosis with perivascular lymphocytic infiltrate in upper dermis, vertically oriented collagen in papillary dermis and coronoid lamella
Figure 3.
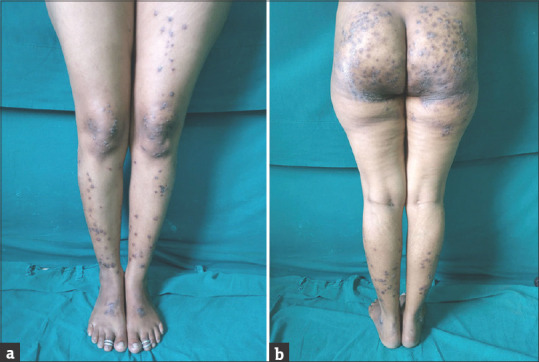
(a) Multiple hyperpigmented scaly papules and plaques bilaterally symmetrical over lower legs. (b) Multiple hyperpigmented scaly papules and plaques on buttocks
Figure 4.
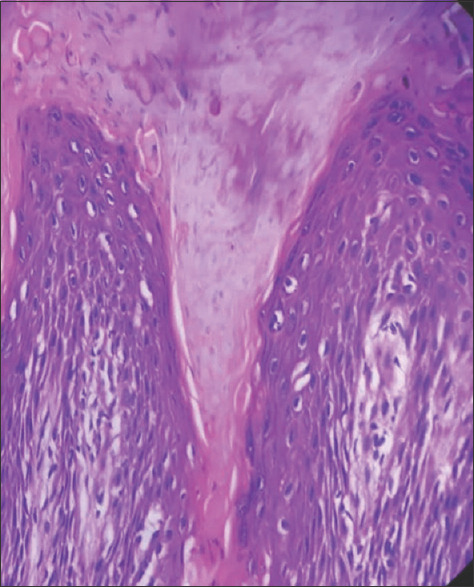
Coronoid lamella
EPPP was first described by Kanzaki et al. as a rare, relapsing, pruritic variant of DSP (which is otherwise asymptomatic). It presents with acute onset of intensely pruritic erythematous papules with repeated flares of intense pruritus and appearance of new lesions and eventual regression.[3] Since the first report, eight patients, with pruritic porokeratosis have been added.[2] Histology shows coronoid lamellae, epidermal spongiosis and perivascular lymphocytic infiltrate.[3] Reed and Leone suggested that localized anomalous keratinocytic clone may lead to epidermal dysplasia.[2] Dermal abnormalities play a role. DNA polyploidy and sensitivity of keratinocytes and fibroblasts to ionizing radiation have been documented in lesional skin. AIDS, ultraviolet exposure and chemotherapy may cause exacerbation.[4] In pruritic variant, inflammation underlying pruritus represents an immunological reaction against abnormal keratinocytic clones suggesting that porokeratosis is a precursor skin manifestation of malignant tumor.[2] Tanaka et al. postulated that regression of lesions is due to CD4+ T-cell-mediated immune reaction against abnormal clones that resided in the epidermis.[3] Table 2 mentions clinical and histopathological differential diagnosis.
Table 2.
Clinical and histopathological differential diagnosis
| Clinical differential diagnosis | Histopathological differential diagnosis |
|---|---|
| Prurigo nodularis | Verruca vulgaris |
| Lichen planus | Actinic keratosis |
Lesions tend to resolve within 12 months.[5] Topical, intralesional and/or systemic steroids may improve pruritus. Topical 5-fluorouracil ointment has also been reported. Etretinate used in one patient led to remission after 1 year. However, response to therapy is variable.[3]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Grainne MR, Alan DI. Porokeratosis. In: Lowell AG, Stephen IK, Barbara AG, Amy SP, David JL, et al., editors. Fitzpatrick's Dermatology in General Medicine. 8th ed. New York: Mc Graw Hill Medical; 2012. pp. 563–8. [Google Scholar]
- 2.Kanekura T, Yoshii N. Eruptive pruritic papular porokeratosis: A pruritic variant of porokeratosis. J Dermatol. 2006;33:813–6. doi: 10.1111/j.1346-8138.2006.00185.x. [DOI] [PubMed] [Google Scholar]
- 3.Kang BD, Kye YC, Kim SN. Disseminated superficial actinic porokeratosis with both typical and prurigo nodularis-like lesions. J Dermatol. 2001;28:81–5. doi: 10.1111/j.1346-8138.2001.tb00094.x. [DOI] [PubMed] [Google Scholar]
- 4.Stork J, Kodetová D. Disseminated superficial porokeratosis: An eruptive pruritic papular variant. Dermatol. 1997;195:304–5. doi: 10.1159/000245971. [DOI] [PubMed] [Google Scholar]
- 5.De Nigris J, Jalalat S, Saco M, Nappi F, Laurain D, Fenske N. Eruptive pruritic papular porokeratosis: A unique presentation of a rare variant. J Am Acad Dermatol. 2016;74:AB 53. [Google Scholar]


