Abstract
Background
Although tenotomy and tenodesis are frequently used for long head of the biceps tendon lesions, controversies remain as to which technique is superior regarding pain, functionality, complications, and cosmetic appearance.
Questions/purposes:
(1) For long head of biceps tendon lesions, does tenotomy or tenodesis result in greater improvements in VAS score for pain? (2) Which approach has superior results when evaluating function outcome (Constant) scores? (3) Does tenotomy or tenodesis have fewer complications? (4) Does tenotomy or tenodesis result in better cosmesis (Popeye sign)?
Methods
A systematic review was performed in the Cochrane Library, Embase, PubMed, and Literatura Latino Americana e do Caribe em Ciências da Saúde (LILACS) using the keywords “long head of the biceps tendon,” “biceps tenodesis,” and “tenotomy.” We completed the search in June 2020. The inclusion criteria were randomized controlled trials and quasirandomized controlled trials that investigated tenodesis and tenotomy with no language restriction and evaluation of adult patients who presented with a long head of the biceps tendon lesion, associated with other lesions or not, without previous shoulder surgeries and who had no response to nonoperative treatment. The initial search yielded 239 studies, 40 of which were duplicates. We assessed the titles and abstracts of 199 articles and excluded all studies that were not randomized controlled trials (literature reviews) or that compared different techniques. We assessed the full text of 14 articles and excluded the ones that were protocols and cohort studies. We evaluated the risk of bias using the Cochrane Collaboration tool. We included eight studies in this systematic review and meta-analysis, with a total of 615 participants, 306 of whom were treated with tenotomy and 309 with tenodesis. The median duration of follow-up was 2 years. Overall, the included studies had a low risk of bias. The complications evaluated were adhesive capsulitis, biceps brachii tear, cramps, and a subsequent second surgical procedure. We used a random model in this meta-analysis so that we could generalize the results beyond the included studies. In this study, we only reported differences between the groups if they were both statistically valid and larger than the minimum clinically important difference (MCID).
Results
Comparing tenotomy and tenodesis, we observed no difference between the groups regarding pain in the long term (mean difference 0.25 [95% confidence interval -0.29 to 0.80]; p = 0.36). There was no difference in Constant score in the long-term (mean difference -1.45 [95% CI -2.96 to 0.06]; p = 0.06). There were no differences when evaluating for major complications (odds ratio 1.37 [95% CI 0.29 to 6.56]; p = 0.70). There were not enough papers evaluating adhesive capsulitis, cramping, and risk of revision surgery. Popeye sign was more frequent in the tenotomy group than in the tenodesis group (OR 4.70 [95% CI 2.71 to 8.17]; p < 0.001).
Conclusion
This systematic review demonstrated that tenotomy and tenodesis offer satisfactory treatment for long head of the biceps tendon lesions. In terms of pain improvement and Constant score, there was no difference between the techniques, but patients undergoing tenotomy have worse cosmetic results. Therefore, surgeons should choose the technique based on their skills and the patient’s expectations of surgery, such as cosmesis and time to recovery. More studies are needed to evaluate complications such as adhesive capsulitis and cramping, as well as to compare duration of surgery and recovery time for each technique.
Level of Evidence
Level I, therapeutic study.
Introduction
Long head of the biceps tendon lesions cause anterior shoulder pain [12, 17]. In most patients, the initial treatment for a long head of the biceps tendon lesion is nonoperative and includes lifestyle modifications, rest, rehabilitation, NSAID use, and corticosteroid injections. Surgical treatment may be indicated if these measures are ineffective [12, 24]. Tenotomy and tenodesis are the most common surgical techniques for long head of the biceps tendon lesions [6, 14]. Surgeons who perform tenotomy think it is technically easier and allows for earlier return to activities [5, 6, 9, 21]. On the other hand, advocates of tenodesis propose that this technique reduces cosmetic deformities and results in better supination strength, less cramping, and less tendon retraction [1, 5, 6, 25, 26]. Cosmetic complications resulting from tenotomy (Popeye sign) occur in 3% to 70% of patients [10, 16]. In addition, persistent pain, subjective weakness, and discomfort may be associated with this technique [12, 16].
There is no evidence of the superiority of either technique [5, 7, 8]. Furthermore, although there are systematic reviews on the subject, none have investigated the evidence based on clinical trials alone [2, 18, 22, 23]. Nevertheless, it has been suggested that tenotomy is better suited for patients older than 55 to 60 years, while patients younger than 50 years or those involved in heavy labor receive greater benefit from tenodesis [1, 6, 16]. Because of the uncertainty about the best treatment option, we conducted this systematic review.
We asked: (1) For long head of biceps tendon lesions, does tenotomy or tenodesis result in greater improvements in VAS score for pain? (2) Which approach has superior results when evaluating function outcome (Constant) scores? (3) Does tenotomy or tenodesis have fewer complications? (4) Does tenotomy or tenodesis result in better cosmesis (Popeye sign)?
Materials and Methods
This review was performed at the Departamento de Ortopedia e Traumatologia—Disciplina de Cirurgia da Mão e Membro Superior da Universidade Federal de São Paulo—Escola Paulista de Medicina. It is a systematic review of randomized controlled or quasirandomized (with an inadequate method of randomization) controlled trials that compared tenodesis and tenotomy as treatments for long head of the biceps tendon injuries. This study was registered in PROSPERO by the protocol CRD42020166638.
Search Methods
The search was performed in the Cochrane Library, Embase, PubMed, and LILACS on June 15, 2020. We searched Current Controlled Trials (http://www.isrctn.com/), WHO’s international registry of clinical trials (http://apps.who.int/trialsearch/), and Clinicaltrials.gov (http://clinicaltrials.gov/) for clinical trials currently in progress or recently completed (Table 1). We did not set a time interval for the searches.
Table 1.
Search strategy for each database
| Database | Search strategy |
| Cochrane Library | (long head of the biceps tendon/exp OR long head of the biceps tendon) AND (biceps tenodesis/exp OR biceps tenodesis) AND (tenotomy/exp OR tenotomy) |
| Embase | (long head of the biceps tendon/exp OR long head of the biceps tendon) AND (biceps tenodesis/exp OR biceps tenodesis) AND (tenotomy/exp OR tenotomy) |
| PubMed | (long head of the biceps tendon/exp OR long head of the biceps tendon) AND (biceps tenodesis/exp OR biceps tenodesis) AND (tenotomy/exp OR tenotomy) |
| LILACS | (long head of the biceps tendon/exp OR long head of the biceps tendon) AND (biceps tenodesis/exp OR biceps tenodesis) AND (tenotomy/exp OR tenotomy |
Study Selection
Two authors (JPD, DYN) independently selected and assessed studies that were potentially eligible for inclusion in the review. Any differences in opinion were resolved through discussions and, when needed, a third author intervened.
The inclusion criteria were randomized and quasirandomized controlled trials with no language restriction and assessment of adult patients presenting with a long head of the biceps tendon lesion, associated with other injuries or not, without previous shoulder surgeries and in whom nonoperative treatment did not work. The two surgical interventions described for the treatment of long head of the biceps lesions were tenodesis and tenotomy. We did not determine a minimum follow-up duration nor a maximum percentage of loss to follow-up. The exclusion criteria were animal studies, observational studies, case reports, and letters to the editor.
The initial search yielded 239 studies, 40 of which were duplicates. We assessed the titles and abstracts of 199 articles and excluded all studies that were not randomized controlled trials (literature reviews) or that compared different techniques. We assessed the full-text of 14 articles, and excluded protocol and cohort studies.
Data Management and Extraction
Two authors (JPD, DYN) extracted the following information from the studies using a form for data extraction: characteristics of the methods, including the design and duration of the study and whether the protocol was published before patients were recruited, financial sources, and details of the experimental registry; characteristics of the participants, including the location of study, number of participants recruited, number of participants evaluated, inclusion criteria, exclusion criteria, age of the participants, and type of lesions; characteristics of the interventions, including the duration of intervention, type of surgical intervention, and any complications; results, including the duration and loss to follow-up; and methodologic domains and assessment of the risk of bias.
Outcomes
The outcomes evaluated were pain: VAS score for pain in the short-, medium-, and long-term (4 weeks, 6 months, and > 1 year postoperatively); functional results (Constant score) in the short-, medium-, and long-term (4 weeks, 6 months, and > 1 year postoperatively); complications; and cosmetic deformities (evaluated as Popeye sign). If the outcome was evaluated at two points within the same period, we selected the last one.
The VAS score has a range of results from 0 to 10 points, in which higher scores represent more pain. The minimum clinically important difference (MCID) of this score is 2. The Constant score has a range of results from 0 to 100, and higher scores represent better functionality. The MCID of this score is 10.4. Only Lee et al. [17] evaluated the initial VAS, with a relevant difference between the groups.
The VAS for pain was evaluated in five studies [4, 6, 17, 19, 27]. Only one study evaluated short-term results [27]. Medium-term results were evaluated by four studies [4, 6, 17, 19], and long-term results were evaluated by three studies [6, 17, 19].
Belay et al. [4] and MacDonald et al. [19] did not assess the Constant score outcome at any timepoint. Lee et al. [17] did not publish the SDs for the outcome, and we were unable to access these data despite attempting to contact the authors of that study. The data were therefore not included in this meta-analysis. There were 317 patients analyzed for this outcome. No study evaluated the short-term Constant score. Only Castricini et al. [6], Hufeland et al. [15], and Mardani-Kivi et al. [20] evaluated the medium-term score, with no statistical difference during this period.
Five studies [4, 6, 15, 19, 20] evaluated complications. Belay et al. [4] presented complications including adhesive capsulitis and rupture of the biceps brachii. Castricini et al. [6] evaluated retear of the rotator cuff and cramping. Hufeland et al. [15] only evaluated cramping during patient follow-up. MacDonald et al. [19] reported adhesive capsulitis and the need for another surgical approach. Finally, Mardani-Kivi et al. [20] observed cramping in their patients.
All eight studies [4, 6, 7, 15, 17, 19, 20, 27] analyzed in this study evaluated Popeye sign after surgical treatment with tenotomy and tenodesis.
Results of the Search
The search was performed in June 2020; we found 239 studies, 40 of which were duplicates. After evaluating the article titles and eliminating studies that were not clinical trials or did not compare different techniques, we excluded 191 articles. Eight studies were evaluated (Fig. 1).
Fig. 1.
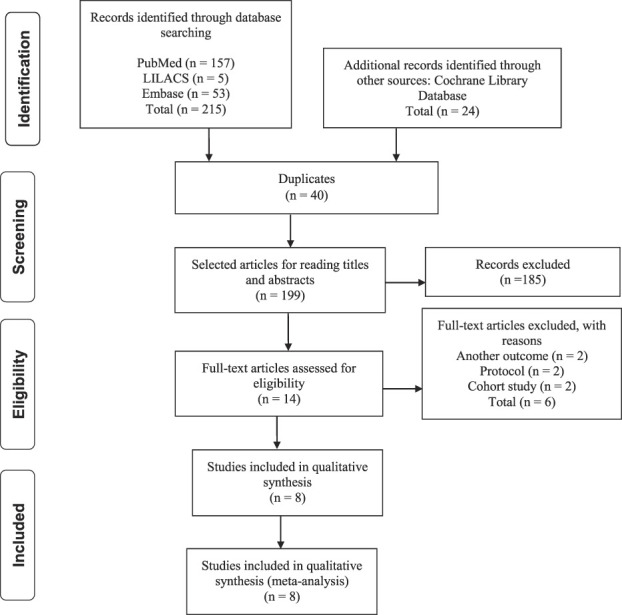
This flowchart shows the number of articles initially identified as well as the exclusion and inclusion steps.
The eight clinical trials included a total of 615 participants [4, 6, 7, 15, 17, 19, 20, 27] (Table 2). Six clinical trials were randomized [4, 6, 7, 19, 20, 27] and two were quasirandomized [7, 15]. These studies were completed without financial incentives.
Table 2.
Characteristics of studies that fulfilled the inclusion criteria for systematic review and meta-analysis
| Author | Type of study | Number of patients/sex/ mean age | Country | Diagnosis | Outcomes and evaluation methods | Tenotomy | Tenodesis | Results | Complications | Quality of evidence Grade |
| Belay et al. [4] | Randomized, prospective, single-blinded study | n = 34 Male (n = 31) Female (n = 3) 56 years |
UK | Disorders of the long head of the biceps | (1) Pain - VAS Reduced pain Nighttime pain (2) Cosmetic deformities (evaluated as Popeye sign) |
n = 20 (1) Reduced pain 8 (42.1) Nighttime pain 8 (44.4) (2) Popeye deformity (n = 5) (none were associated with cramping) |
n = 14 (1) Reduced pain 4 (28.6) Nighttime pain 6 (42.9) |
The mean pain score in 3 months was lower in the tenotomy group There were no statistical differences in pain improvement and night pain |
Adhesive capsulitis in both groups after 3 months | ⊕⊕⊕⊕ High |
| Castricini et al. [6] | Randomized, prospective, single-blinded study | n = 55 Male: (n = 21) Female: (n = 34) Tenotomy: 59 years Tenodesis: 57 years |
Italy | Long head of the biceps tendon lesions | (1) Pain - VAS (6, 24 months) (2) Constant-Murley Scale (3) Complications (4) Cosmetic deformities (evaluated as Popeye sign) - number of events |
n = 31 (1) 1.1 ± 1.9 (6 months), 1 ± 1.9 (24 months) (2) Improvement: 42.9% ± 8.8% (3) Cramps (n = 0), rotator cuff retear (n = 1) (4) 18 |
n = 24 (1) 1.5 ± 2 (6 months); 1± 2 (24 months) (2) Improvement: 44.1% ± 7.8% (3) Cramps (n = 3), rotator cuff retear (n = 1) (4) 5 |
There was no statistical difference in pain, Constant-Murley Scale, and complications There was a higher incidence of Popeye sign deformity in the tenotomy group |
Cramps occurred in tenodesis group at 6-month follow-up One case of rotator cuff retear for each group |
⊕⊕⊕⊕ High |
| De Carli et al. [7] | Quasirandomized, prospective | n = 65 Male: 48 Female: 17 58 years |
Italy | Reparable rotator cuff tears with concomitant long head of the biceps lesions | (1) Constant score (preoperative and postoperative) (2) Cosmetic deformities (Popeye sign) - number of events |
n = 30 (1) 47.4 ± 12.1/94.6 ± 4.9 (2) 5 |
n = 35 (1) 44.1 ± 12.1/ 94.6 ± 4.9 (2) 0 |
There was no statistical difference in Constant Score and Popeye deformities There was a higher incidence of Popeye sign deformity in the tenotomy group |
Not assessed in the study | ⊕⊕⊕◯ Moderate |
| Hufeland et al. [15] | Quasirandomized, prospective, single-blinded study | n = 20 Male: 11 Female: 9 52 years |
Germany | SLAP biceps pulley lesions | (1) Constant score preoperatively, 6 months, and 12 months (2) Popeye |
n = 11 (1) 50.9 ± 8.5; 6 months 68.5 ± 14; 12 months 77.4 ± 11.8 (2) 3 |
n = 9 (1) 60.1 ± 8.5; 6 months 77.7 ± 10.2; 12 months 88.1 ± 7.5 (2) 1 |
There was no significant difference on the Popeye between the groups | Cramping was observed in 2 patients in the tenotomy group at 6-month follow-up. At 12-month follow-up, no patient complained about cramps | ⊕⊕⊕⊕ High |
| Lee et al. [17] | Randomized, prospective, double-blinded study | n = 128 Male: 29 Female: 99 62..9 years (mean age in tenodesis group) |
Korea | Long head of the biceps lesions | (1) Popeye (2) VAS preoperatively and 12 months (3) Constant preoperatively and 12 months |
n = 56 (1) 11 (2) 7.1 ± 1.41; 12 months 2.0 (3) 69.9 ± 7.47; 12 months 88.3 |
n = 72 (1) 4 (2) 6.8 ± 1.27; 12 months 1.8 (3) 69.9 ± 7.19; 12 months 86.5 |
The incidence of Popeye deformity was about 3 times higher in the tenotomy group and was higher in men (5 of 11) than in women (7 of 45) in the tenotomy group | ⊕⊕⊕◯ Moderate |
|
| MacDonald et al. [19] | Randomized, prospective, double-blinded study | n = 114 Male: 92 Female: 22 57.7 years |
Canada | Lesions of the long head of the biceps | (1) Popeye (3 months and 24 months) (2) Cramping (3, 6, and 12 months) (3) Reoperations |
n = 52 (1) 17 and 15 (2) 2.0 ± 2.6; 2.2 ± 2.9; 2.1 ± 2.8; 2.3 ± 2.9 (3) 5 |
n = 48 (1) 5 and 4 (2) 2.5 ± 3; 2.3 ± 2.7; 1.7 ± 2.4; 2.1 ± 2.9 (3) 4 |
There were no differences in cramping between the two groups There was a 3.5-times higher risk of Popeye deformity after tenotomy |
One patient had adhesive capsulitis and underwent reoperation | ⊕⊕⊕⊕ High |
| Mardani-Kivi et al. [20] | Randomized, prospective | n = 62 Male: 42 Female: 20 54.5 years (mean age of tenotomy group) and 55.5 years (mean age of tenodesis group) |
Iran | Disorders of the long head of the biceps with rotator cuff tear | (1) Popeye (2) VAS preoperatively, 6 months, 12 months, 24 months (3) Constant score preoperatively, 6 months, 12 months, 24 months |
n = 29 (1) 7 (2) 1.96 ± 1.22; 6 months 6.38 ± 0.6; 12 months 8.07 ± 0.66; 24 months 9.07 ± 0.58 (3) 61.01 ± 6.12; 6 months 73.07 ± 5.85; 12 months 82.14 ± 7.93; 24 months 88.1 ± 5.4 |
n = 33 (1) 1 (2) 2.01 ± 1.23; 6 months 6.10 ± 0.74; 12 months 8.61 ± 0.66; 24 months 9.53 ± 0.48 (3) 61.76 ± 8.07; 6 months 73.12 ± 6.83; 12 months 83.51 ± 5.13; 24 months 89.94 ± 3.24 |
The Constant score and the VAS increased The only significant difference between the two methods was the Popeye sign, with higher incidence in tenotomy group |
Cramping was measured as a complication and occurred in 9 patients in the tenotomy group | ⊕⊕⊕◯ Moderate |
| Zhang et al. [27] | Randomized, prospective, double-blinded study | n = 151 Male: 71 Female: 80 61 years |
China | Long head of the biceps lesions and reparable rotator cuff tears | (1) Constant score (2) Popeye sign (3) VAS 2 and 4 weeks postoperatively |
n = 77 (1) Improved (2) 7 (3) 2 weeks 3.1 ± 1.8; 4 weeks 2 ± 1.1 |
n = 74 (1) Improved (2) 2 (3) 2 weeks 4.8 ± 1.9; 4 weeks 2.1 ± 1.6 |
The VAS was lower in the tenodesis group in the 2-week postoperative examination There were no differences between other outcomes in the two groups |
Cramping was observed in 9 patients in the tenotomy group and 5 in the tenodesis group and was considered a complication | ⊕⊕⊕⊕ High |
SLAP = superior labrum anterior posterior.
Two studies were conducted in hospitals in Italy [6, 7], one in Korea [17], one in China [27], one in Iran [20], one in Germany [15], one in two centers in Canada [19], and one in the United Kingdom [4]. All of these studies included adults with long head of the biceps tendon lesions who were treated with either tenotomy or tenodesis. Mardani-Kivi et al. [20] included patients who did not undergo physiotherapy previously, but the other seven studies included participants who did not respond to nonoperative treatment. Because only one study excluded patients who previously underwent physiotherapy, we decided to analyze the results with and without this particular study to evaluate whether there would be any difference in the outcome.
Quality of Evidence
We used the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) evidence system to assess the quality of evidence [11]. For each study, the quality of evidence was ultimately assigned one of four grades: high quality, moderate quality, low quality, or very low quality [3]. The classification of the strength of evidence by the GRADE method indicated that the included studies had moderate- to high-quality level of evidence (Table 2).
Evaluation of the Risk of Bias
Two authors (JPD, DYN) independently evaluated the risk of bias of the included studies using the Cochrane Collaboration’s tool for assessing the risk of bias [13]. The following domains were analyzed: randomization sequence, allocation concealment, blinding of participants, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases (such as financial incentives or population imbalance among the studied groups).
Each criterion was judged and classified as having a low risk of bias, high risk of bias, and uncertain risk of bias. Disagreements among the authors regarding the risk of bias for each of the domains were resolved by consensus.
The assessment of the risk of bias is important to determine problems with the execution of the studies, which could compromise their findings and applicability.
Randomization Sequence
Two studies that were considered randomized [6, 19] used randomization software. Belay et al. [4] and Lee et al. [17] reported the use of a randomization chart. Mardani-Kivi et al. [20] used randomization blocks of four. One study used randomized numbers [27]. Two studies did not specify how the randomization was performed [7, 15].
Allocation Concealment
Six studies [4, 6, 15, 17, 19, 20] reported secrecy of allocation with sealed envelopes that were opened only in the operating room. However, the studies did not state whether the envelope was opaque. Mardani-Kivi et al. [20] and De Carli et al. [7] did not describe how patients were allocated between the two groups.
Blinding of Participants and Personnel
Two studies did not describe whether there was blinding of patients [7, 20]. Mardani-Kivi et al. [20], however, mentioned that the rehabilitation protocol of the two groups was equal. Belay et al. [4] and Castricini et al. [6] reported that the patients were blinded during follow-up, but they did not specify whether the evaluator was blinded. Hufeland et al. [15] mentioned that the examiner was blinded but did not mention whether the patient was also blinded. Zhang et al. [27], Lee et al. [17], and MacDonald et al. [19] blinded both the patient and the examiner.
Measurement of Treatment Effects
Regarding measurement of the treatment effects, dichotomous data were analyzed by calculating the relative risk, with a confidence interval of 95%. We used the Mantel-Haenszel statistical method. Continuous data are presented as the mean and SD.
When the primary studies expressed the same variables for different instruments or units of measurement, the standard difference of means was used.
Units for Analysis Matters
The randomization unit used in the included studies was generally the individual participant. In exceptional instances, such as in studies with patients with bilateral involvement, data were evaluated by involvement instead of by individual patient.
Dealing with Lack of Data
An intention-to-treat analysis was performed to include every randomized participant for any intervention. Therefore, when faced with inadequate information regarding the expected effects, such as the number of patients, means, uncertainty measurements (SD or error), or number of events, we contacted the authors of the primary studies.
Three aspects of the studies were analyzed separately: whether the intention-to-treat principle was used, whether data losses were less than 20%, and whether these losses were unequal between the compared groups. Four evaluated studies [4, 7, 17, 19] were classified as having a low risk of bias for this item; the study by Zhang et al. [27] was classified as having an intermediate risk of bias because it did not address whether there was loss of data during the study period.
Selective Reporting
Four studies published their protocols before data collection, which could be a source of bias for the other studies [6, 19, 20, 27]. However, most of the outcomes evaluated in this review were assessed in the eight studies, with the exception of the VAS pain scale, which was not assessed by De Carli et al. [7], Hufeland et al. [15], and Mardani-Kivi et al. [20]; and the Constant score, which was not assessed by Belay et al. [4] and MacDonald et al. [19]. Lee et al. [17] assessed the Constant score but did not include data with SD.
Other Outcomes
None of the included studies mentioned having any financial incentive. There was also a concern about obtaining a balanced and homogeneous population between the two groups in all studies, which generated a low risk of bias. Overall, the selected studies had a low risk of bias (Fig. 2). It is possible to analyze each study according to the type of bias (Fig. 3).
Fig. 2.
This chart shows the risk of bias of the included studies.
Fig. 3.
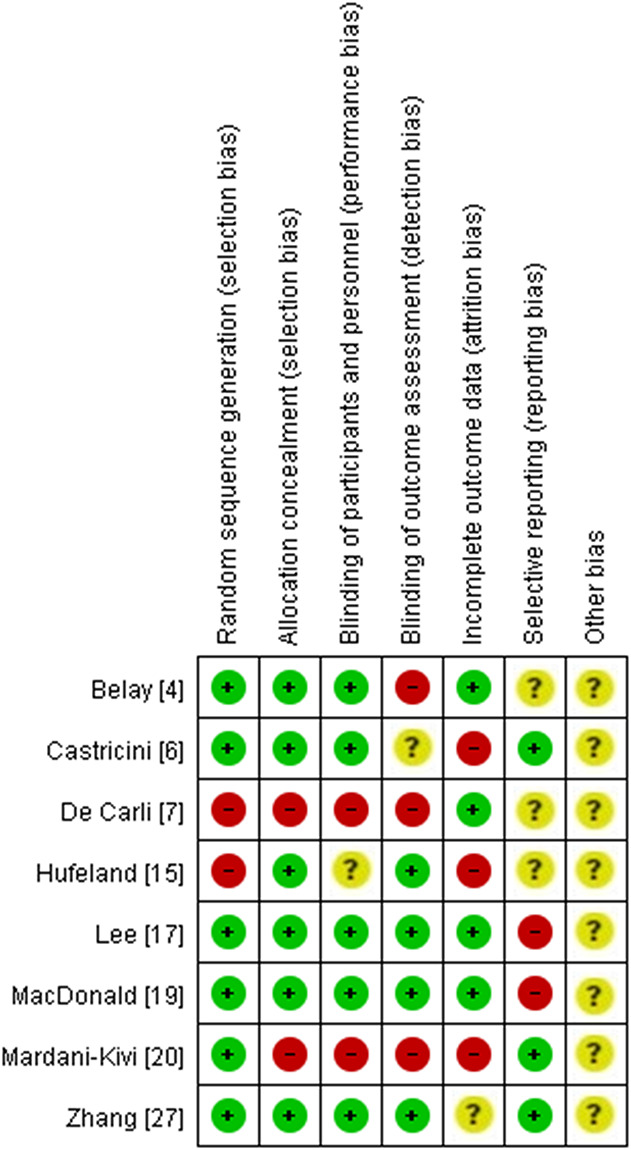
This chart shows a summary of the risk of bias.
Ethical Approval
Ethical approval for this study was waived by Plataforma Brasil.
Statistical Analyses
The meta-analysis was completed using Review Manager (RevMan version 5.3, the Nordic Cochrane Centre, The Cochrane Collaboration), thereby combining the relevant effects of interest from our identified studies [13]. Continuous and dichotomous variables were analyzed using the weighted mean difference. The precision of the effect sizes is reported as 95% CIs.
The heterogeneity of estimated effects among the included studies was visually analyzed through forest graphics and the I2 test. Heterogeneity was considered relevant when I2 was greater than 50%. For the VAS, the I2 was smaller than 50% in each subgroup, but the test for subgroup differences was 77.6%. For the Constant score, the I2 of each subgroup was smaller than 50%, and the test for subgroup differences was 0%. Complications had an I2 of 57% and the Popeye 0%. All of the outcomes used a random effects model.
Results
VAS for Pain
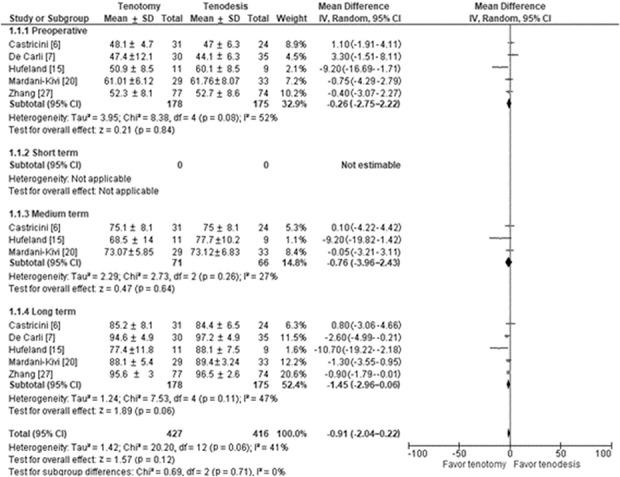
There were no differences in VAS scores for pain in the short-term (mean difference -0.10 [95% CI -0.54 to 0.34]; p = 0.66), medium-term (mean difference -0.57 [95% CI -1.21 to 0.07]; p = 0.08), and long-term (mean difference 0.25 [95% CI -0.29 to 0.80]; p = 0.36) (Fig. 4).
Fig. 4.
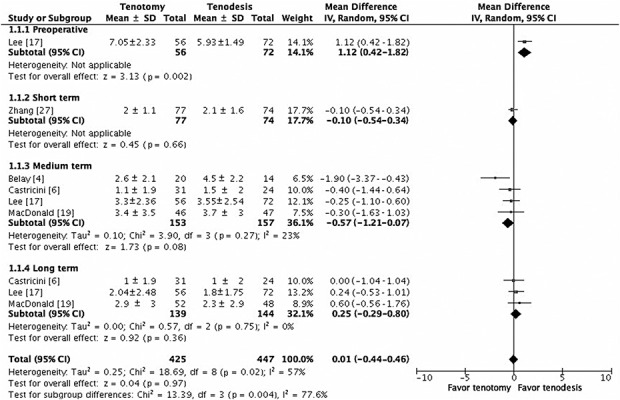
This figure shows a comparison of VAS scores for pain among the included studies.
Constant Score
There were no differences in Constant scores in the medium-term (mean difference -0.76 [95% CI -3.96 to 2.43]; p = 0.64), and no differences in long-term functional (Constant) scores (mean difference -1.45 [95% CI -2.96 to 0.06]; p = 0.06) (Fig. 5).
Fig. 5.
This figure shows a comparison of the Constant score among the included studies.
Complications
There were no differences in the risk of major complications between tenotomy and tenodesis (OR 1.37 [95% CI 0.29 to 6.56]; p = 0.70) (Fig. 6).
Fig. 6.
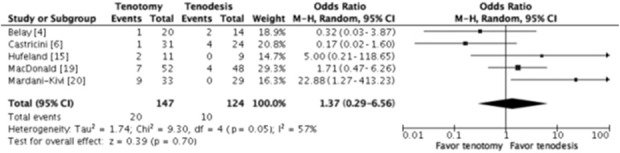
This figure shows a comparison of general complications among the included studies.
We separately evaluated recurrent complications (adhesive capsulitis, cramping, and revision surgeries), but there were not enough papers evaluating those outcomes.
Cosmetic Results (Popeye Sign)
Tenodesis resulted in better cosmesis then tenotomy did (OR 4.70 [95% CI 2.71 to 8.17]; p < 0.001) (Fig. 7).
Fig. 7.
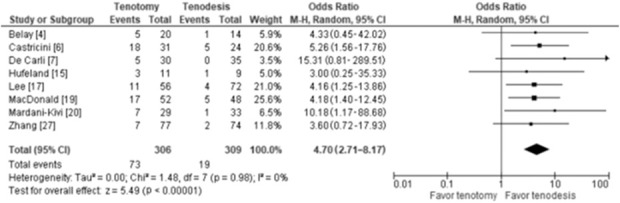
This figure shows a comparison of Popeye sign among the included studies.
Discussion
There are several controversies about which technique is superior to treat lesions of the long head of the biceps tendon. It is believed that tenotomy has a shorter rehabilitation, but tenodesis results in fewer complications. In this review, we evaluated which technique (tenotomy or tenodesis) is more effective for treating those injuries regarding pain, functionality, cosmesis, and complications. We found eight randomized or quasirandomized controlled trials that compared the results of surgical treatment for this lesion using the two main techniques. These studies were small and involved 615 patients, and some of the outcomes could not be grouped for comparison because they were not measured in the same period or were not considered in the original study.
Limitations
Our findings should be interpreted in light of some limitations. Our main limitation is the total number of patients included, which may have limited our ability to observe differences between the groups. Another limitation is the nonstandardization between studies regarding the postoperative timepoint for assessing outcomes, which made the data difficult to compare. Stratifying the results as short-, medium-, and long-term allowed us to assess the outcomes despite this obstacle.
We chose to include the study by Mardani-Kivi et al. [20] because of the scarcity of randomized controlled trials on the subject, even though they excluded patients who had undergone nonoperative treatment. We performed the meta-analysis with and without this study and obtained similar results, so we chose to keep the study in our review.
To assess the VAS, Belay et al. [4] stratified the results separating groups with and without rotator cuff repair, therefore, we were unable to extract all data in the meta-analysis.
VAS for Pain
There was no difference in pain as assessed by the VAS. Lee et al.’s [17] study showed a difference between groups preoperatively, with higher VAS scores in the tenotomy group than in the tenodesis group. Belay et al. [4] presented results supporting tenotomy for earlier pain improvement; however, those findings were not what we observed in our meta-analysis. As pain improvement is not a parameter to choose between the two techniques, surgeons should consider other points, such as cosmetic deformities that might not be well tolerated in young patients, or duration of the surgery.
Constant Score
Regarding the Constant functional score, we found no differences in the group that underwent tenotomy and those who underwent tenodesis. Therefore, the Constant score should not be a determinant for surgical technique selection, and surgeons should consider other parameters, again, such as cosmetic issues and surgery duration.
Complications
We observed no difference in the risk of complications between tenotomy and tenodesis. However, some complications reported by the studies, such as rotator cuff retear, are not directly related to the techniques in question. Belay et al. [4] reported one rupture of the biceps after tenodesis, which is a complication that has a greater relationship with the selected treatment method. Nonetheless, owing to the limitations of the sample, we were unable to observe any differences between the techniques regarding complications. Postoperative complications are not a good parameter to use for choosing a technique, and surgeons should consider other outcomes when selecting a surgical technique.
Cosmetic Results (Popeye Sign)
Popeye sign occurred more often in patients undergoing tenotomy than in those undergoing tenodesis. Considering that this outcome may not be well accepted, it is important to explain to the patient the increased risk of deformity in tenotomy surgery. On the other hand, tenotomy is usually a shorter surgery, has less restrictive rehabilitation, and may be more cost effective.
Conclusion
The studies in this review revealed that both tenotomy or tenodesis offer satisfactory treatment for long head of the biceps tendon lesions, but patients undergoing tenotomy have worse cosmetic results. In terms of pain improvement, functionality, and complications, there were no differences between the techniques. Therefore, surgeons should make their procedure choice based on their skills and the patient’s expectations of surgery, such as cosmesis and time to recovery. More studies are needed to evaluate complications such as adhesive capsulitis and cramping, as well as to compare duration of surgery, recovery, and the costs of each technique.
Acknowledgments
We thank all the staff of Departamento de Traumatologia e Ortopedia – Escola Paulista de Medicina, for the opportunity to conduct this study and their support of our research.
Footnotes
Each author certifies that neither he nor she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was waived by Plataforma Brasil.
The first two authors contributed equally to this manuscript.
Contributor Information
Dan Yuta Nagaya, Email: nagaya_yuta@hotmail.com.
Fabio Teruo Matsunaga, Email: fteruo@gmail.com.
Marcel Jun Sugawara Tamaoki, Email: marceltamaoki@gmail.com.
References
- 1.Ahmad CS, El Attrache NS. Arthroscopic biceps tenodesis. Orthop Clin North Am. 2003;34:499-506. [DOI] [PubMed] [Google Scholar]
- 2.Anil U, Hurley ET, Kingery MT, Pauzenberger L, Mullett H, Strauss EJ. Surgical treatment for long head of the biceps tendinopathy: a network meta-analysis. J Shoulder Elbow Surg. 2020;29:1289-1295. [DOI] [PubMed] [Google Scholar]
- 3.Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401-406. [DOI] [PubMed] [Google Scholar]
- 4.Belay ES, Wittstein JR, Garrigues GE, et al. Biceps tenotomy has earlier pain relief compared to biceps tenodesis: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc. 2019;27:4032-4037. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P, Baqué F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747-757. [DOI] [PubMed] [Google Scholar]
- 6.Castricini R, Familiari F, De Gori M, et al. Tenodesis is not superior to tenotomy in the treatment of the long head of biceps tendon lesions. J Bone Joint Surg Am. 2018;26:169-175. [DOI] [PubMed] [Google Scholar]
- 7.De Carli A, Vadalà A, Zanzotto E, et al. Reparable rotator cuff tears with concomitant long-head biceps lesions: tenotomy or tenotomy/tenodesis? Knee Surg Sports Traumatol Arthrosc. 2012;20:2553-2558. [DOI] [PubMed] [Google Scholar]
- 8.Delle Rose G, Borroni M, Silvestro A, et al. The long head of biceps as a source of pain in active population: tenotomy or tenodesis? A comparison of 2 case series with isolated lesions. Musculoskelet Surg. 2012;96(suppl 1):S47-52. [DOI] [PubMed] [Google Scholar]
- 9.Frost A, Zafar MS, Maffulli N. Tenotomy versus tenodesis in the management of pathologic lesions of the tendon of the long head of the biceps brachii. Am J Sports Med. 2009;37:828-833. [DOI] [PubMed] [Google Scholar]
- 10.Gill TJ, McIrvin E, Mair SD, Hawkins RJ. Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg. 2001;10:247-249. [DOI] [PubMed] [Google Scholar]
- 11.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383-394. [DOI] [PubMed] [Google Scholar]
- 12.Hassan S, Patel V. Biceps tenodesis versus biceps tenotomy for biceps tendinitis without rotator cuff tears. J Clin Orthop Trauma. 2019;10:248-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins J, Green SE. Cochrane handbook for systematic reviews of interventions. 4.2.5 (Updated May 2005). In: Higgins J Green SE, eds. The Cochrane Library, Issue 3. John Wiley & Sons Ltd; 2006. [Google Scholar]
- 14.Hsu AR, Ghodadra NS, Provencher MT, Lewis PB, Bach BR. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326-332. [DOI] [PubMed] [Google Scholar]
- 15.Hufeland M, Wicke S, Verde PE, Krauspe R, Patzer T. Biceps tenodesis versus tenotomy in isolated LHB lesions: a prospective randomized clinical trial. Arch Orthop Trauma Surg. 2019;139:961-970. [DOI] [PubMed] [Google Scholar]
- 16.Kelly AM, Drakos MC, Fealy S, Taylor SA, O'Brien SJ. Arthroscopic release of the long head of the biceps tendon: functional outcome and clinical results. Am J Sports Med. 2005;33:208-213. [DOI] [PubMed] [Google Scholar]
- 17.Lee HJ, Jeong JY, Kim CK, Kim YS. Surgical treatment of lesions of the long head of the biceps brachii tendon with rotator cuff tear: a prospective randomized clinical trial comparing the clinical results of tenotomy and tenodesis. J Shoulder Elbow Surg. 2016;25:1107-1114. [DOI] [PubMed] [Google Scholar]
- 18.Leroux T, Chahal J, Wasserstein D, Verma NN, Romeo AA. A systematic review and meta-analysis comparing clinical outcomes after concurrent rotator cuff repair and long head biceps tenodesis or tenotomy. Sports Health. 2015;7:303-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacDonald P, Verhulst F, McRae S, et al. Biceps tenodesis versus tenotomy in the treatment of lesions of the long head of the biceps tendon in patients undergoing arthroscopic shoulder surgery: a prospective double-blinded randomized controlled trial. Am J Sports Med. 2020;48:1439-1449. [DOI] [PubMed] [Google Scholar]
- 20.Mardani-Kivi M, Karimi Mobarakeh M, et al. Treatment of long head of biceps tendon lesions together with rotator cuff tears: which method is preferred? Tenotomy or tenodesis. Tech Shoulder Elb Surg. 2018;19:101-105. [Google Scholar]
- 21.Mariani EM, Cofield RH, Askew LJ, Li GP, Chao EY. Rupture of the tendon of the long head of the biceps brachii. Surgical versus nonsurgical treatment. Clin Orthop Relat Res. 1988;(228):233-239. [PubMed] [Google Scholar]
- 22.Na Y, Zhu Y, Shi Y, et al. A meta-analysis comparing tenotomy or tenodesis for lesions of the long head of the biceps tendon with concomitant reparable rotator cuff tears. J Orthop Surg Res. 2019;14:370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shang X, Chen J, Chen S. A meta-analysis comparing tenotomy and tenodesis for treating rotator cuff tears combined with long head of the biceps tendon lesions. PLoS One. 2017;12:e0185788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slenker NR, Lawson K, Ciccotti MG, Dodson CC, Cohen SB. Biceps tenotomy versus tenodesis: clinical outcomes. Arthroscopy. 2012;28:576-582. [DOI] [PubMed] [Google Scholar]
- 25.Walch G, Edwards TB, Boulahia A, Nové-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14:238-246. [DOI] [PubMed] [Google Scholar]
- 26.Wittstein JR, Queen R, Abbey A, Toth A, Moorman CT, 3rd. Isokinetic strength, endurance, and subjective outcomes after biceps tenotomy versus tenodesis: a postoperative study. Am J Sports Med. 2011;39:857-865. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Q, Zhou J, Ge H, Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2015;23:464-469. [DOI] [PubMed] [Google Scholar]


