Atrial fibrillation (AFib) is a heart condition. It happens because the electrical activity of your heart becomes fast and irregular. This causes the small upper chambers of the heart, the atria, to squeeze poorly, slowing blood flow through them. The slow movement of blood can cause blood clots to form within your heart. These blood clots can then travel to your brain and cause a part of it to die, called a stroke. Strokes can be very serious. They may take away your vision, ability to speak, walk, or keep your balance. Some strokes can lead to death.
Anticoagulants, often called “blood thinners”, are medications to prevent these strokes. They prevent harmful blood clots from forming. They also stop helpful blood clots, making you more likely to bleed. While rare, bleeding can be a serious problem. Your provider will help you balance the protection and risk of these medications. This Patient Page will help you learn more about blood thinners so you can make an informed decision.
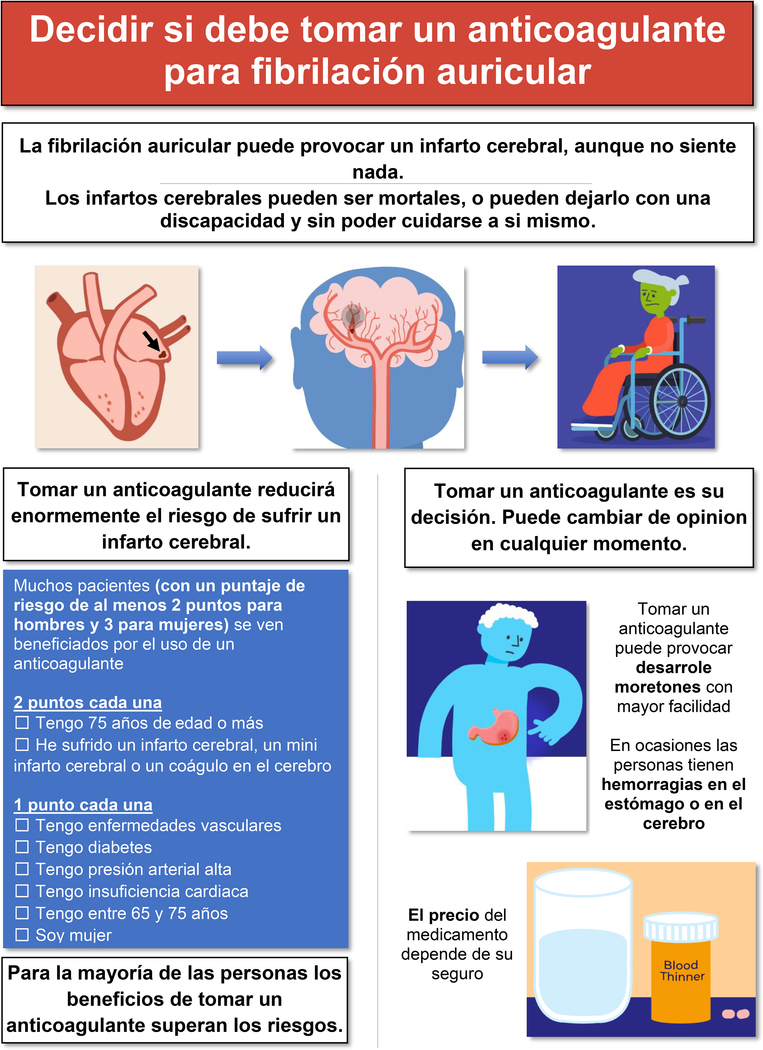
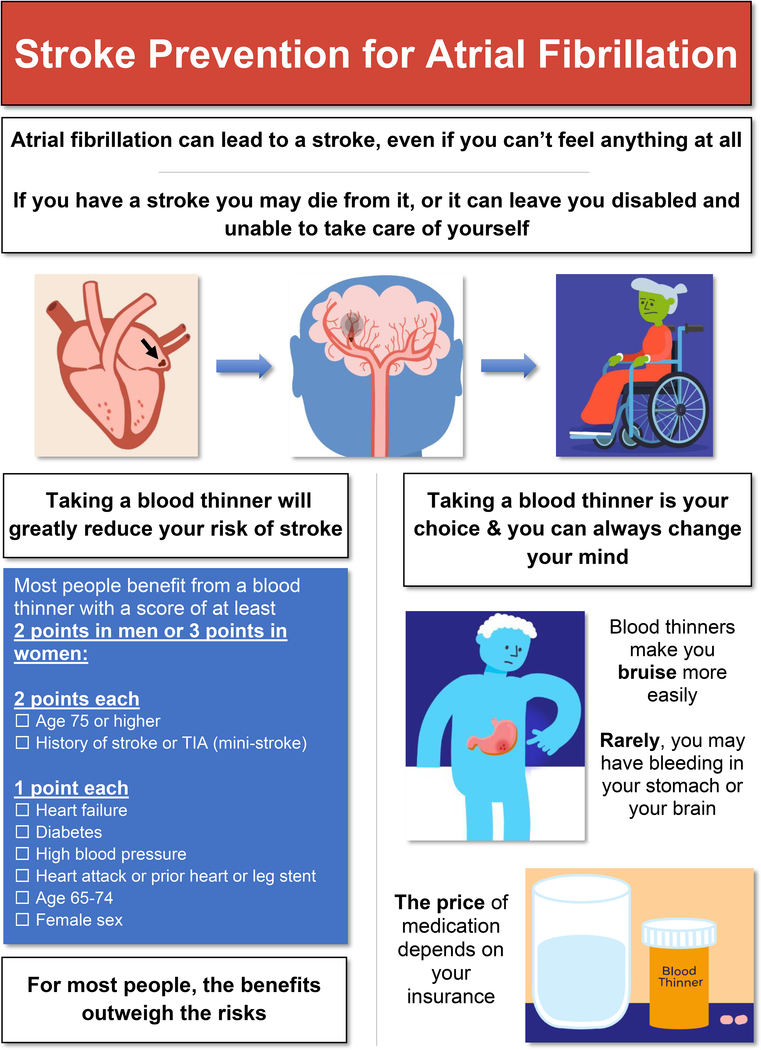
Who Should Take a Blood Thinner?
Not everyone benefits from taking a blood thinner for AFib. Your provider will calculate your risk of having a stroke with a score called CHA2DS2-VASc. A higher score means a higher risk of stroke. It also means you gain more benefit from taking a blood thinner. The last page explains how to calculate the score.
What Blood Thinners Can I Use?
Warfarin
Your body uses Vitamin K to help your blood clot. Warfarin (brand name Coumadin) works by blocking Vitamin K. The daily dose of warfarin can vary from person to person. Your blood’s ability to clot will be tested often using a lab test called “prothrombin time,” used to calculate the International Normalized Ratio (INR).
Your dose of warfarin may change over time. Vitamin K comes from food, like leafy green vegetables. If how much Vitamin K you eat changes often, your INR can become too high or too low. A high INR increases your bleeding risk. A low INR increases your risk of blood clots and stroke. Your health history, age, sex or genes may also make it difficult to keep your INR in the correct range. So, it is important to check your INR as often as recommended by your provider.
Direct Oral Anticoagulants
These medications directly block a protein needed to form blood clots. They include dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa). They have fixed doses and you will not need frequent blood tests.
Adverse Effects
The most common side effect from taking blood thinners is bleeding. Most bleeding is minor, such as bleeding from the gums, easy bruising, or cuts that take longer to clot.
Serious bleeding is rare but can be life threatening. Vomiting blood or having bloody, very dark or black stools may mean bleeding in your stomach or bowels. Sudden headaches or an injury to the head may mean bleeding inside your head. If you notice any of these signs of bleeding, contact your provider or call 911 immediately.
Other bleeding can include nosebleeds, bleeding into a joint, or blood in the urine (red/pink urine).
Your risk of bleeding is higher if your kidneys or liver do not work well or if you have had previous severe bleeding. Some medications, like aspirin or those containing aspirin, can increase bleeding risk when taken by someone who is also taking a blood thinner. Alcohol can also increase bleeding risk. You can lower your bleeding risk by drinking less than 8 alcoholic drinks per week. You should avoid ibuprofen (brand names Advil and Motrin) and other non-steroidal anti-inflammatory drugs (NSAIDs).
How Do I Decide Whether to Take a Blood Thinner?
You and your provider should discuss the benefits and harms of taking a blood thinner. You know your lifestyle best. Share your values, preferences, and activity level so you can decide together.
A stroke can lead to death, leave you disabled, or take away your ability to care for yourself. However, some people prefer to avoid the risk of bleeding. Also, taking a blood thinner might mean more bruising and more lab checks or clinic visits.
If you have AFib, your risk of stroke is higher than normal and will continue to rise as you get older. Your risk also rises if you develop new medical conditions such as high blood pressure, heart disease, or diabetes. Even if you decide not to take a blood thinner at first, it still may be a good idea to start one later.
Which Blood Thinner Should I Take?
Experts recommend direct oral anticoagulants first, because they lead to less harmful bleeding than warfarin. Your provider will explain if your medical conditions or other medications make certain blood thinners safer for you than others.
Additionally:
How much you pay can vary based on your health insurance
Some blood thinners are taken once daily, others twice daily
Can I Change or Stop My Blood Thinner?
You have the choice to change from one blood thinner to another, or you can stop taking a blood thinner. Do not stop your blood thinner without first discussing with your provider.
Other Common Questions
Can I take aspirin instead?
Aspirin and other anti-platelet medications like clopidogrel (Plavix), prasugrel (Effient), or ticagrelor (Brilinta) are not good at preventing strokes from AFib.
Can I stop my blood thinner if I have had an ablation procedure?
Ablation can reduce how much AFib you have or feel, but it does not take away your risk of stroke. Your provider will help guide you.
Can I still exercise?
Most people who take a blood thinner maintain an active lifestyle, and exercise is important for heart health. Avoid contact sports or activities with high risk of injury.
Is there a way to reverse the effects of blood thinners?
Yes, with medications or transfusions.
Additional Resources
The American Heart Association. https://www.heart.org/en/health-topics/atrial-fibrillation
StopAfib.org. https://www.stopafib.org/
My AFib Experience. https://myafibexperience.org/
The Heart Rhythm Society. https://www.hrsonline.org/patient-resources/patient-information-sheets
The Stanford Understanding AFib Series. https://scopeblog.stanford.edu/tag/understanding-afib/
Acknowledgments
Sources of Funding: This study was supported by the Joe and Linda Chlapaty DECIDE Center of the Atrial Fibrillation Strategically Focused Research Network Award from the American Heart Association: 18SFRN34120036. The statements in this publication are solely the responsibility of the authors and do not necessarily represent the views of the American Heart Association (AHA).”
Disclosures: Krishna Pundi receives research grant from American Heart Association. Tina Baykaner receives research grant from NIH (K23 HL145017). Samuel Sears receives honoraria and consulting fees from Medtronic, Abbott, Milestone Pharmaceutical, and Zoll Medical. He also receives research grants from Medtronic, Zoll Medical. All funds are directed to East Carolina University. All others have nothing to declare.
Nonstandard Abbreviations and Acronyms
- AFib
Atrial Fibrillation
- INR
International Normalized Ratio
- NSAID
Non-Steroidal Anti-Inflammatory Drug