Abstract
Some surgical strategies can maintain or restore thoracic kyphosis (TK); however, next-generation surgical schemes for adolescent idiopathic scoliosis (AIS) should consider anatomical corrections. A four-dimensional correction could be actively achieved by curving the rod. Thus, anatomically designed rods have been developed as notch-free, pre-bent rods for easier anatomical reconstruction. This study aimed to compare the initial curve corrections obtained using notch-free rods and manually bent, notched rods for the anatomical reconstruction of thoracic AIS. Two consecutive series of 60 patients who underwent anatomical posterior correction for main thoracic AIS curves were prospectively followed up. After multilevel facetectomy, except for the lowest instrumented segment, either notch-free or notched rods were used. Patient demographic data, radiographic measurements, and sagittal rod angles were analyzed within 1 week after surgery. Patients with notch-free rods had significantly higher postoperative TK than patients with notched rods (P < .001), but both groups achieved three-dimensional spinal corrections and significantly increased postoperative rates of patients with T6–T8 TK apex (P = .006 for notch-free rods and P = .008 for notched rods). The rod deformation angle at the concave side was significantly lower in the notch-free rods than in the notched rods (P < .001). The notch-free, pre-bent rod can maintain its curvature, leading to better correction or maintenance of TK after anatomical spinal correction surgery than the conventional notched rod. These results suggest the potential benefits of anatomically designed notch-free, pre-bent rods over conventional, manually bent rods.
Subject terms: Outcomes research, Musculoskeletal system
Introduction
The aim of adolescent idiopathic scoliosis (AIS) surgery is to correct the spinal deformity in the three planes. Since typical thoracic AIS shows a thoracic hypokyphosis leading to sagittal imbalance, correction of the thoracic kyphosis (TK) and the main thoracic (MT) curve is an important surgical goal1–4. To resolve further hypokyphosis of the thoracic spine secondary to pedicle screw instrumentations1,5,6, some posterior surgical strategies have been developed in which the TK is maintained or improved4,7,8.
Although these strategies can maintain or restore TK4,7,8, next-generation surgical schemes for patients with AIS should consider anatomical corrections9. Although the apex of the TK is located at T6–T8 in healthy humans10, the postoperative apex of the TK was almost identical with the apex of the preoperative MT scoliosis in some patients with kyphosis10. This non-anatomical TK is mainly generated by the rod-bending procedure, in which the configuration of the rods is approximated by rotation on the alignment of scoliosis before performing maneuvers in curve corrections9. Since the original shape of the rod is straight, intraoperative bending is needed to adapt the TK and lumbar lordosis. The initial shape of the spinal rod significantly affects spinal alignment11–13, and the rod-bending procedure highly depends on surgeons’ knowledge or experience, resulting in different configurations9. When the configuration does not adapt to the spinal deformity, it will lead to not only inadequate correction but also excess stress to the instrumentation and patient’s body. In addition, the manual bending procedure adds notches into the rod, which decreases its mechanical properties14.
From the spatiotemporal point of view, we recently documented that four-dimensional correction could be actively achieved by bending the rod under multilevel facetectomy9. In this surgical strategy, two rods were bent identically to guide postoperative anatomical TK without reference to the intraoperative coronal alignment of the deformity9. Thus, pre-bent configurations were intraoperatively derived from tracings of the rod shapes applied to the technique, and optimized rod configurations were identified to guide the anatomical reconstruction15. These results suggest that anatomically designed rods could be provided as notch-free, pre-bent rods15. The anatomical notch-free rods are created using custom-made rigid bending fixtures, and 11 types of cobalt chrome (CoCr) alloy rods can be utilized based on the curve types and its lengths. This medical device, which is the first in the world, has been approved by a national agency in Japan (Fig. 1).
Figure 1.
Anatomical notch-free, pre-bent rods for scoliosis surgery. Eleven types of rods can be utilized based on the length and curve types. The rod shapes were split up into two shapes: single curve and double curves. If the lowest instrumented vertebra (LIV) is L1 or above, two identical single-curve rods are used (left). If the LIV is L2 or L3, two identical double-curve rods are used.
The hypothesis underlying this study was that patients with notch-free, pre-bent rods would have a significantly higher postoperative TK than patients with conventional, manually bent, notched rods after anatomical spinal correction surgery. In addition, postoperative rod deformation, as a spring-back effect, would be reduced in patients with notch-free rods14. This study aimed to compare initial curve corrections obtained using notch-free rods and manually bent, notched rods for the surgical treatment of thoracic patients with AIS.
Materials and methods
Experimental design
The institutional review board of Hokkaido University Hospital approved the experiments, including any relevant details. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent for this study and publication of identifying information/case study was obtained from all participants and/or their guardians/parents. Data from two consecutive series of patients who underwent posterior instrumentation surgery for Lenke 1 AIS curves were prospectively evaluated; all patients had a MT Cobb angle ≤ 90°. The exclusion criteria were syndromic, neuromuscular, and congenital scoliosis and Lenke 2–6 AIS curves. Manually bent, notched rods were used between 2014 and 2018, and notch-free rods were used between 2019 and 2020. No cases were lost to follow-up.
Standing radiographs were taken preoperatively and within 1 week after surgery, and Cobb measurements were obtained. Preoperative curve flexibility was measured using supine bending radiographs4,9. The end vertebrae levels were determined on preoperative radiographs and measured on subsequent radiographs to maintain consistency for statistical comparisons9,16. Coronal balance was evaluated by the lateral displacement of the C7 coronal plumb line from the center sacral vertical line (CSVL), and sagittal balance was measured as the sagittal vertical axis. A positive radiographic shoulder height (RSH) was defined as left shoulder up17. The angle of rotation of the thoracic apical vertebra was obtained on computed tomography (CT) images, as previously described4,9,18. Our internal studies of interrater and intrarater reliability have shown excellent kappa statistics for all continuous measures (0.90–0.98). The number of facetectomy levels was obtained, and screw density was evaluated as the number of screws per level instrumented11.
Surgical technique
The instrumentation levels were primally decided to include the end vertebrae. The upper instrumented vertebra (UIV) was then selected based on the preoperative shoulder balance19 and anatomical TK; T3 was selected if RSH was > − 5 to 0 mm, and T4 was selected if RSH was ≤ − 5 mm9. In case TK was < 20° and the upper-end vertebra was T5 or T6, the UIV selected was T49. The last vertebra touching the CSVL was determined for the lowest instrumented vertebra (LIV) in cases of lumbar modifier A or B19,20. For lumbar modifier C, LIV was selected at L3.
Side-loading polyaxial pedicle screw instruments (USS II Polyaxial; DePuy Synthes, Raynham, MA, USA, for manually bent, notched rods or CVS spinal system; Robert Reid, Tokyo, Japan, for notch-free rods) were placed. All-level facetectomy was performed except for the lowest instrumented segment to avoid pseudoarthrosis at this site9.
For manually bent rods, two titanium alloy rods (φ 6.0 mm) were bent identically to guide the postoperative anatomical TK9. The apex was anticipated to be at T6–T8 for the postoperative TK9. The rod configurations were split into two shapes: single curve and double curves. In case the LIV was L1 or above, the single-curve rods were used9, and the thoracolumbar/lumbar region remained straight. When the LIV was L2 or L3, the double-curve rods were used9. For notch-free rods, CoCr alloy rods (φ 5.5 mm) were used. The rods also have two shapes, and each shape is provided by increments of 3 cm.
The rods were simultaneously rotated after connecting to the screw heads; in situ rod-bending procedure was not performed4,9,11. After the decortication of the laminae, local bones are grafted. Intraoperative monitoring using somatosensory/motor-evoked potentials was performed. None of the patients used brace.
Analysis of rod configuration
For manually bent rods, rod shapes were traced on paper after intraoperative contouring of the rods13,21. The angle between the cranial and caudal tangential lines was measured before implantation (θ1) (Fig. 2)13,21. The postoperative rod angle was similarly measured (θ2) using reconstructed sagittal CT images13. If the rod had both thoracic and lumbar curvatures, the distal tangential line was set based on the inflection point13.
Figure 2.
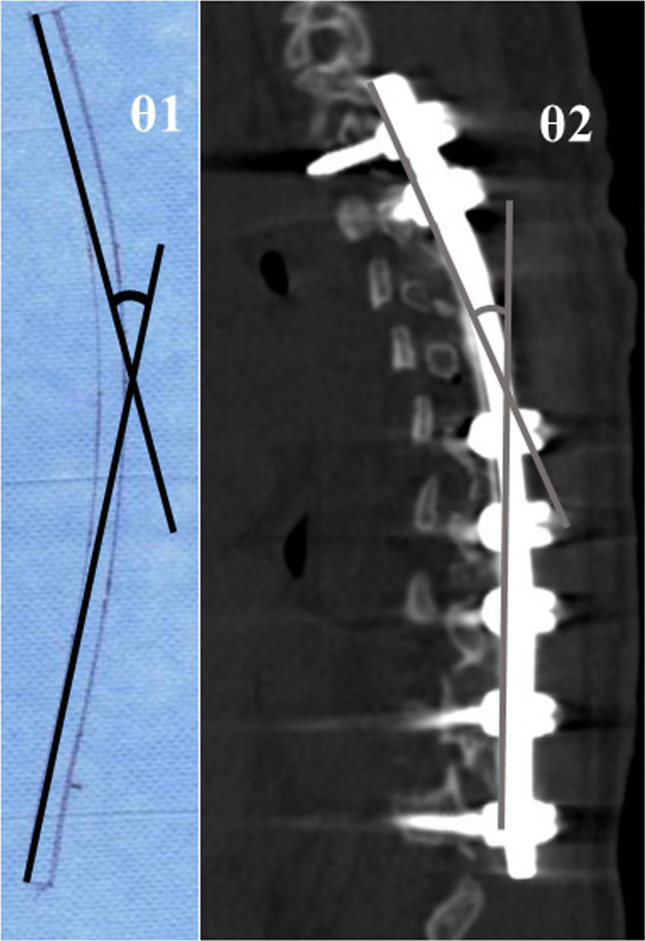
Rod angle before and after implantation. The angle between the proximal and distal tangential lines was measured. In case of notched rod, the surgeon traced the rod shapes on paper before implantation (θ1). The postoperative implant rod geometry (θ2) was obtained after the surgical operation using computed tomography.
Statistical analysis
All data are presented as means ± standard deviation and range. Comparisons of demographic data, radiographic quantitative variables, and rod angles were performed using a Mann–Whitney U test or a paired t-test. Chi-square tests were used to assess sex and lumbar modifier. All statistical analyses were conducted using JMP Pro version 14.0 statistical software (SAS Institute, Cary, NC, USA). A P value < 0.05 was considered statistically significant.
Results
Patient demographic data
There was no significant difference in age, sex, curve type, number of instrumented vertebrae, screw density, number of facetectomy levels, or operative time between the groups (Table 1).
Table 1.
Patient demographic data.
| Notched rods | Notch-free rods | P | |
|---|---|---|---|
| Number of patients (no.) | 33 | 27 | |
| Age at surgery (years) | 15.2 ± 2.4 (12–20) | 14.3 ± 2.5 (11–20) | 0.173 |
| Sex (no. and % of female)* | 32 (97%) | 24 (89%) | 0.207 |
| Risser sign (grade) | 3.5 ± 1.5 (0–5) | 3.7 ± 1.1 (0–5) | 0.640 |
| Cobb length (segments) (upper end to lower end vertebra) | 8.3 ± 1.1 (7–10) | 8.0 ± 1.2 (6–11) | 0.183 |
| Lumbar modifier (no. and %)* | |||
| A | 17 (52%) | 17 (63%) | |
| B | 6 (18%) | 3 (11%) | |
| C | 10 (30%) | 7 (26%) | 0.622 |
| Number of instrumented vertebrae (segments) | 10.7 ± 1.2 (9–13) | 10.8 ± 1.2 (8–13) | 0.866 |
| Screw density at concave side (no. of screws/ levels instrumented) | 0.9 ± 0.1 (0.7–1) | 0.9 ± 0.1 (0.6–1) | 0.479 |
| Screw density at convex side (no. of screws/ levels instrumented) | 0.8 ± 0.1 (0.5–1) | 0.8 ± 0.1 (0.6–1) | 0.261 |
| Number of facetectomy levels (no.) | 8.4 ± 1.3 (6–11) | 8.7 ± 1.0 (7–10) | 0.343 |
| Operative time (min) | 261.5 ± 47.6 (170–360) | 251.6 ± 39.8 (190–322) | 0.401 |
All data expressed as means ± SD and range. Mann–Whitney U test or Chi-square test*.
Radiographic findings
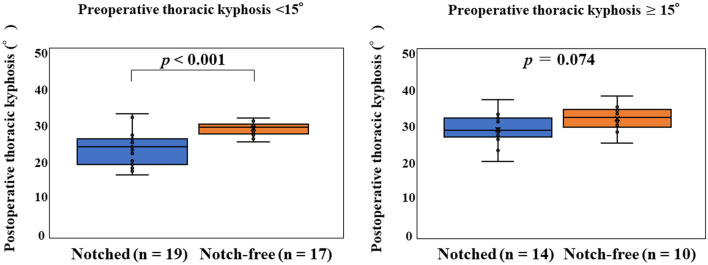
There was no significant difference between the groups in terms of preoperative and postoperative coronal plane radiographic data (P > 0.05; Table 2). Sagittal plane analysis showed no significant difference between the groups in preoperative TK. However, postoperative TK and the change in TK were significantly higher in the notch-free rod group than in the notched rod group (P < 0.001 and P < 0.001, respectively). When the cohorts were divided into two groups based on preoperative TK, postoperative TK was significantly higher in the notch-free group than in the notched group in patients with preoperative TK < 15° (P < 0.001, Fig. 3), but both groups had similar baseline demographic data except for preoperative TK. There was no significant difference between the groups in terms of preoperative and postoperative lumbar lordosis, balance parameters, and translational data (P > 0.05).
Table 2.
Radiographic parameters.
| Notched rods | Notch-free rods | P | |
|---|---|---|---|
| Coronal plane data | |||
| Preoperative main thoracic curve (°) | 58.5 ± 8.0 (45–77) | 55.9 ± 6.8 (45–75) | 0.211 |
| Preoperative flexibility of main thoracic curve (%) | 67.4 ± 16.8 (23–91) | 65.9 ± 17.0 (32–96) | 0.505 |
| Postoperative main thoracic curve (°) | 8.6 ± 4.0 (1–20) | 8.2 ± 4.4 (1–18) | 0.182 |
| Correction rate of main thoracic curve (%) | 85.1 ± 7.1 (68–99) | 85.5 ± 7.1 (71–98) | 0.246 |
| Preoperative thoracolumbar/lumbar curve (°) | 26.2 ± 13.8 (1–46) | 27.9 ± 10.2 (4–51) | 0.953 |
| Postoperative thoracolumbar/lumbar curve (°) | 7.8 ± 6.5 (0–23) | 6.9 ± 5.1 (0–20) | 0.848 |
| Sagittal plane data | |||
| Preoperative thoracic kyphosis (T5 to T12) (°) | 13.4 ± 6.5 (3–34) | 14.2 ± 7.1 (2–31) | 0.623 |
| Postoperative thoracic kyphosis (T5 to T12) (°) | 23.6 ± 5.3 (13–34) | 30.0 ± 3.0 (25–38) | < 0.001 |
| 95% confidence interval | (21.8, 25.4) | (28.8, 30.9) | |
| Change in thoracic kyphosis (T5 to T12) (°) | 10.1 ± 4.8 (0–20) | 16.0 ± 5.6 (4–27) | <0.001 |
| 95% confidence interval | (8.7, 12.0) | (14.0, 18.2) | |
| Preoperative lumbar lordosis (L1 to S1) (°) | 50.4 ± 9.7 (35–73) | 47.0 ± 8.5 (30–65) | 0.330 |
| Postoperative lumbar lordosis (L1 to S1) (°) | 47.3 ± 8.0 (29–62) | 44.7 ± 7.5 (33–64) | 0.097 |
| Balance parameters and translational data | |||
| Preoperative C7 translation from central sacral vertical line (mm) | 11.7 ± 8.3 (0–27) | 12.3 ± 7.2 (0–28) | 0.929 |
| Postoperative C7 translation from central sacral vertical line (mm) | 10.2 ± 8.9 (0–26) | 11.8 ± 7.0 (0–24) | 0.532 |
| Preoperative sagittal vertical axis (mm) | − 2.4 ± 19.8 (− 54 to 30) | − 7.7 ± 20.8 (− 50 to 28) | 0.274 |
| Postoperative sagittal vertical axis (mm) | − 4.4 ± 17.4 (− 37 to 40) | − 9.6 ± 11.7 (− 28 to 23) | 0.136 |
| Preoperative thoracic apical vertebral translation* (mm) | 52.0 ± 12.9 (31–95) | 50.5 ± 12.5 (27–77) | 0.766 |
| Postoperative thoracic apical vertebral translation* (mm) | 7.8 ± 6.0 (0–27) | 9.6 ± 4.6 (1–18) | 0.148 |
| Preoperative thoracolumbar/lumbar apical vertebral translation* (mm) | 8.4 ± 7.9 (0–22) | 9.3 ± 6.6 (0–23) | 0.440 |
| Postoperative thoracolumbar/lumbar apical vertebral translation* (mm) | 6.2 ± 5.9 (0–25) | 6.5 ± 5.9 (0–21) | 0.928 |
| Shoulder balance data | |||
| Preoperative radiographic shoulder height (mm) | − 10.4 ± 8.1 (− 28 to 5) | − 9.4 ± 8.0 (− 23 to 9) | 0.899 |
| Postoperative radiographic shoulder height (mm) | 7.4 ± 5.5 (0 to 18) | 8.0 ± 5.0 (1 to 20) | 0.956 |
All data expressed as means ± SD and range. Mann–Whitney U test.
*Distance between the geometric center of the apical vertebrae and the C7 plumb line or the center sacral vertical line.
Figure 3.
Postoperative thoracic kyphosis in patients with preoperative thoracic kyphosis < 15° and ≥ 15°.
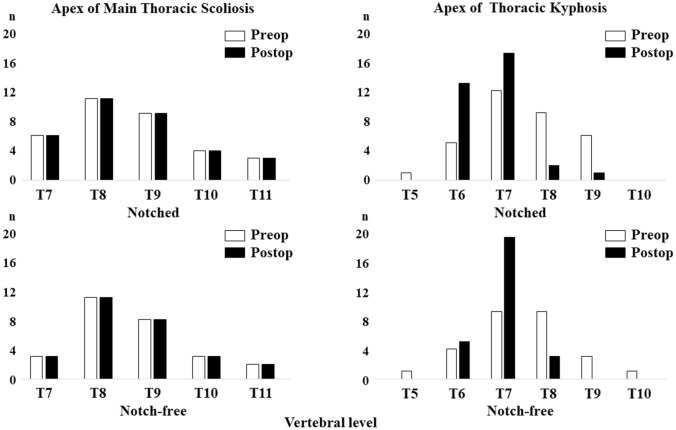
The preoperative levels of the MT scoliosis and TK apices were different in 24 cases (73%) in the notched rod group and in 22 cases (81%) in the notch-free rod group, respectively (Fig. 4). The preoperative levels of the apex in MT scoliosis were the same postoperatively in both groups. The preoperative rates of patients with T6–T8 TK apex significantly increased from 76 to 97% postoperatively in the notched rod group (P = 0.008) and from 81 to 100% in the notch-free rod group (P = 0.006). There were no significant differences in the postoperative percentage of patients with T6–T8 TK apex between the groups (P = 0.271).
Figure 4.
Apex of the main thoracic scoliosis and thoracic kyphosis.
There was no significant difference between the groups in terms of preoperative and postoperative MT apical vertebral rotation angle (P > 0.05; Table 3).
Table 3.
Vertebral rotation angle of main thoracic apical vertebra.
| Notched rods | Notch-free rods | P | |
|---|---|---|---|
| Preoperative vertebral rotation (°) | 17.9 ± 5.0 (8–32) | 16.9 ± 5.1 (3–29) | 0.134 |
| Postoperative vertebral rotation (°) | 11.5 ± 4.7 (0–24) | 10.7 ± 4.8 (3–21) | 0.111 |
All data expressed as means ± SD and range. Mann–Whitney U test.
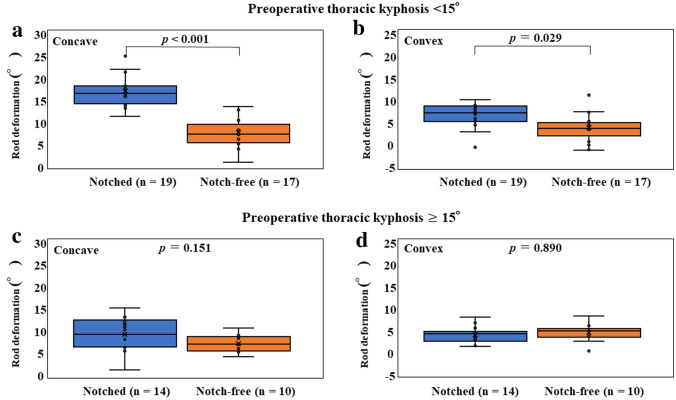
Implant rod angles of curvature
The rod deformation angle at the concave side was significantly lower in the notch-free rod group than in the notched rod group (P < 0.001; Table 4). When the cohorts were divided into two groups based on preoperative TK, this significant difference was seen at both the concave and convex sides in patients with preoperative TK < 15° (P < 0.001 and P = 0.029, respectively), but not in patients with preoperative TK ≥ 15° (P = 0.151 and P = 0.890, respectively, Fig. 5).
Table 4.
Implant rod angle of curvature at the concave and convex side of deformity.
| Notched rods | Notch-free rods | P | |
|---|---|---|---|
| Preoperative rod angle (θ1) at concave side (°) | 41.7 ± 4.4 (31.0–53.5) | 40.2 ± 5.1 (33.6–46.0) | 0.732 |
| Preoperative rod angle (θ1) at convex side (°) | 41.0 ± 4.9 (28.6–54.9) | 40.2 ± 5.1 (33.6–46.0) | 0.941 |
| Postoperative rod angle (θ2) at concave side (°) | 28.2 ± 5.4 (16.8–39.8) | 33.1 ± 4.2 (26.4–40.1) | 0.001 |
| Postoperative rod angle (θ2) at convex side (°) | 35.7 ± 5.2 (27.2–50.8) | 36.6 ± 4.9 (27.2–42.8) | 0.381 |
| Rod deformation angle (Δθ) at concave side (°) | 13.5 ± 5.2 (0.8–25.0) | 7.1 ± 2.9 (0.3–13.3) | < 0.001 |
| Rod deformation angle (Δθ) at convex side (°) | 5.0 ± 2.6 (− 1.1 to 9.8) | 3.7 ± 2.8 (− 1.8 to 10.9) | 0.073 |
All data expressed as means ± SD and range. Mann–Whitney U test. Δθ was defined as the difference between θ1 and θ2 (θ1–θ2).
Figure 5.
Rod deformation angles in patients with preoperative thoracic kyphosis < 15° (a,b) and ≥ 15° (c,d).
Surgical complications
There were no surgical complications such as implant breakage or neurologic deficits in either group.
Case presentation
A 14-year-old girl underwent anatomical spinal reconstruction using notch-free, pre-bent rods (Fig. 6); the MT Cobb angle was 63° (T7–L2), and the TK angle was 9° (T5–T12). The apex of the scoliosis was at T10. Postoperative radiographs obtained 1 week after surgery showed that the MT scoliosis and TK angles were 9° and 28°, respectively. The apex of the TK was at T6.
Figure 6.
Anatomical spinal reconstruction using notch-free, pre-bent rods in a patient with Lenke 1A-thoracic adolescent idiopathic scoliosis.
Discussion
The most important findings of the present study were that patients with notch-free, pre-bent rods had a significantly higher postoperative TK than patients with conventional, manually bent, notched rods and that both groups achieved three-dimensional spinal corrections and significantly increased postoperative rates of patients with T6–T8 TK apex. The rod deformation angles were significantly lower in the notch-free rods than in the notched rods. These results suggest that the notch-free rod can maintain its curvature, leading to better correction or maintenance of TK after anatomical spinal correction surgery than the notched rod.
The diameter and material of rods play significant roles in deformity surgery and its maintenance over time22,23. Using the same titanium (φ 6.0 mm) and CoCr alloy rods (φ 5.5 mm) used in the present study, we previously demonstrated that the yield load of the manually bent CoCr alloy rods was almost identical to that of the manually bent titanium alloy rods, but the titanium alloy straight rods showed a significantly higher yield load than the straight CoCr alloy rods14. In addition, the previous study demonstrated that the notch-free, CoCr rods had a significantly higher ultimate load than the notched CoCr rods while having the same stiffness, indicating that the notch-free, curved CoCr alloy rod will likely maintain its shape compared with the notched rod14. Although the present study used different rod diameters and materials in the notched and notch-free rods, respectively, the results can be mainly explained based on the mechanical property induced by the notches within the rods. Notches result in local stress that surpasses the yield strength of the material, leading to plastic deformation14,24,25. The other possible mechanism of the observed better control in sagittal plain may be explained by inherent material property. Titanium alloy rods have a low work hardening ability while CoCr alloy rods have high work hardening ability and shape retention strength14. Although the two rods can yield at similar points, the curve to get there are different given different modulus. Thus, when yielded during the bending process, this will be stain hardened, and the when attempted to yield again (spring back) the yielding values will be higher for the stiffer material14,25.
When stress concentrations are introduced in the form of notches within rods, they play a considerable role in fatigue because rod fracture mainly occurs at the points of increased stress14,24–26. Rod contouring with a French bender significantly decreased the fatigue strength of both titanium and CoCr alloy rods14,24,25. In the current study, there was no implant breakage after surgery in either group; however, the notch-free rods developed for an adult spinal deformity would be more durable than the conventional notched rod.
Although it is unclear whether notch-free rods were supplied, industrially supplied pre-bent rods based on patient-specific data were reported to be effective in treating AIS patients27. Solla et al.27 treated 37 AIS patients with patient-specific rods that were pre-bent according to a protocol based on pelvic incidence. The rod contouring angles were determined using the pelvic incidence criteria (25° to 40° for the rod on the convex side and the same value plus 10° for the concave side), and CoCr rods were ordered before the date of surgery27. Although the postoperative overall TK was reported to be normal27, issues regarding the reconstruction of the anatomical TK remain. In addition, Solla et al.27 suggested that overbending the concave rod by ≥ 10° should be continued for patients with hypokyphosis because loss of sagittal correction related to rod flattening during correction is unavoidable.
In our surgical strategy, two rods were bent identically without reference to the preoperative spinal alignment9. This strategy is based on previous reports11,13,28–30. To overcome further lordosis of the thoracic spine after pedicle screw placements in thoracic AIS patients, we developed a surgical procedure wherein two rods are rotated simultaneously to correct the scoliosis while the TK is maintained or improved4,9,11. We previously evaluated changes in rod contour from before implantation to after this surgical correction, suggesting that the multilevel facetectomy and/or screw density at the concave side reduce the rod deformation13. Mobilization of the spine by releasing the facet joint is more important than using a rigid implant9,31. The present results indicate that neither a customized patient-specific rod nor overbending the concave rod is necessary for AIS surgery. Rod flattening is unavoidable, but the present results showed that the rod deformation angle was significantly lower in the notch-free rods than the notched rods in patients with preoperative hypokyphosis.
Since thoracic AIS patients have a preexistent hypokyphosis of the thoracic spine and the rods tend to flatten after surgery in these patients, anatomical rods have been developed for thoracic AIS patients. The rods can be particularly suitable for Lenke 1AR, in whom the apex of scoliosis is located at a lower thoracic spine9. However, we currently use these rods for other Lenke 2–6 curves except for Lenke 5 curve. Eleven rods are regarded as appropriate for pre-bent rods15. Although the configurations were obtained from Japanese patients, the algorithm to identify anatomical rod configurations can be applied for other races15. The algorithm to produce a pre-bent rod can also be utilized for Lenke 5 curve since the initial configuration leads to a certain sagittal alignment of the spine15. Another expected advantage of pre-bent rods is decreased operative time; however, the operative time was not significantly different between the groups in the present study.
There are limitations we must address. First, patient clinical outcome scores were not obtained since this study aimed to compare initial curve correction, as Gehrchen et al.32 compared the initial curve correction within 1 week after surgery using either circular rods or beam-like rods. The fact that notch-free pre-bent rods lead to improved sagittal control is purely a mechanical consideration. Although the notching within the rod could play a considerable role in fatigue performance, this would be relevant only if fusion did not occur after immediate correction. However, we previously reported that the average total Scoliosis Research Society questionnaire score significantly increased from 3.5 preoperatively to 4.5 at 2-year follow-up in the anatomical spinal reconstruction using manually bent rods9. In addition, the present preoperative and postoperative radiographic measurements in the manually bent rod group were almost identical to those of the previous study9. Second, the present study used different rod diameters and materials in the notched and notch-free rods, respectively. Few studies have evaluated mechanical properties of the curved rod14,21. In addition, to our knowledge, except for our previous study14, no studies have considered notch-free curved rods. As mentioned above, static four-point bending tests demonstrated similar load–displacement curves between the manually bent titanium 6.0 mm and CoCr 5.5 mm rods14. Based on the previous mechanical results14 and ethical reasons, we conducted the present study to compare the clinical results using manually bent titanium 6.0 mm rod and newly developed, notch-free curved CoCr 5.5 mm rod instead of manually bent CoCr 5.5 mm rods. However, even if similar yield and ultimate load were found for the manually bent titanium 6.0 mm and CoCr 5.5 mm rods, they share different stress–strain profiles to change the shape of the rod. In addition, both techniques used different screw hardware.
In conclusion, patients with notch-free, pre-bent rods had a significantly higher postoperative TK than patients with conventional, manually bent, notched rods after anatomical spinal correction surgery. These results suggest the potential benefits of anatomically designed notch-free, pre-bent rods over conventional, manually bent rods.
Author contributions
H.S. conceived and designed the study. H.S., H. T., T. K., K.Y., A. I., and Y. A. performed the experiment. H.S. and H.T. analysed the results. H.S., H.T., T.E., M.,T., and N.I. contributed to discussions throughout the study. H.S. wrote and edited the manuscript. All authors have read and approved the final submitted manuscript.
Data availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hideki Sudo and Hiroyuki Tachi.
References
- 1.Sucato DJ, et al. Restoration of thoracic kyphosis after operative treatment of adolescent idiopathic scoliosis: a multicenter comparison of three surgical approaches. Spine (Phila Pa 1976) 2008;33:2630–2636. doi: 10.1097/BRS.0b013e3181880498. [DOI] [PubMed] [Google Scholar]
- 2.Newton PO, et al. Preservation of thoracic kyphosis is critical to maintain lumbar lordosis in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35:1365–1370. doi: 10.1097/BRS.0b013e3181dccd63. [DOI] [PubMed] [Google Scholar]
- 3.Lonner BS, et al. Multivariate analysis of factors associated with kyphosis maintenance in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2012;37:1297–1302. doi: 10.1097/BRS.0b013e318247e9a6. [DOI] [PubMed] [Google Scholar]
- 4.Sudo H, et al. Surgical treatment of Lenke 1 thoracic adolescent idiopathic scoliosis with maintenance of kyphosis using the simultaneous double-rod rotation technique. Spine (Phila Pa 1976) 2014;39:1163–1169. doi: 10.1097/BRS.0000000000000364. [DOI] [PubMed] [Google Scholar]
- 5.Lowenstein JE, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: A comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine (Phila Pa 1976) 2007;32:448–452. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 6.Kim YJ, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:291–298. doi: 10.1097/01.brs.0000197865.20803.d4. [DOI] [PubMed] [Google Scholar]
- 7.Clement JL, Chau E, Kimkpe C, Vallade MJ. Restoration of thoracic kyphosis by posterior instrumentation in adolescent idiopathic scoliosis: Comparative radiographic analysis of two methods of reduction. Spine (Phila Pa 1976) 2008;33:1579–1587. doi: 10.1097/BRS.0b013e31817886be. [DOI] [PubMed] [Google Scholar]
- 8.Demura S, et al. Maintenance of thoracic kyphosis in the 3D correction of thoracic adolescent idiopathic scoliosis using direct vertebral derotation. Spine Deform. 2013;1:46–50. doi: 10.1016/j.jspd.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Sudo H, et al. Impact of multilevel facetectomy and rod curvature on anatomical spinal reconstruction in thoracic adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2018;43:E1135–E1142. doi: 10.1097/BRS.0000000000002628. [DOI] [PubMed] [Google Scholar]
- 10.Hasegawa K, et al. Standing sagittal alignment of the whole axial skeleton with reference to gravity line in humans. J. Anat. 2017;230:619–630. doi: 10.1111/joa.12586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sudo H, et al. Correlation analysis between change in thoracic kyphosis and multilevel facetectomy and screw density in main thoracic adolescent idiopathic scoliosis surgery. Spine J. 2016;16:1049–1054. doi: 10.1016/j.spinee.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Salmingo RA, Tadano S, Abe Y, Ito M. Influence of implant rod curvature on sagittal correction of scoliosis deformity. Spine J. 2014;14:1432–1439. doi: 10.1016/j.spinee.2013.08.042. [DOI] [PubMed] [Google Scholar]
- 13.Kokabu, T. et al. Effects of multilevel facetectomy and screw density on postoperative changes in spinal rod contour in thoracic adolescent idiopathic scoliosis surgery. PLoS One. 11, e0161906 (2016). [DOI] [PMC free article] [PubMed]
- 14.Yamada K, Sudo H, Iwasaki N, Chiba A. Mechanical analysis of notch-free pre-bent rods for spinal deformity surgery. Spine (Phila Pa 1976) 2020;45:E312–E318. doi: 10.1097/BRS.0000000000003269. [DOI] [PubMed] [Google Scholar]
- 15.Kokabu T, Kanai S, Abe Y, Iwasaki N, Sudo H. Identification of optimized rod shapes to guide anatomical spinal reconstruction for adolescent thoracic idiopathic scoliosis. J. Orthop. Res. 2018;36:3219–3224. doi: 10.1002/jor.24118. [DOI] [PubMed] [Google Scholar]
- 16.Sudo, H., Ito, M., Kaneda, K., Shono, Y. & Abumi, K. Long-term outcomes of anterior dual-rod instrumentation for thoracolumbar and lumbar curves in adolescent idiopathic scoliosis: a twelve to twenty-three-year follow-up study. J. Bone Jt. Surg. Am. 95, e49 (2013). [DOI] [PubMed]
- 17.Kuklo TR, et al. Correlation of radiographic, clinical, and patient assessment of shoulder balance following fusion versus nonfusion of the proximal thoracic curve in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2002;27:2013–2020. doi: 10.1097/00007632-200209150-00009. [DOI] [PubMed] [Google Scholar]
- 18.Di Silvestre M, et al. Apical vertebral derotation in the posterior treatment of adolescent idiopathic scoliosis: Myth or reality? Eur. Spine J. 2013;22:313–323. doi: 10.1007/s00586-012-2372-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim, Y.J. & Lenke, L.G. Posterior surgery for thoracic scoliosis. in Spinal Deformities: The Essentials (ed. Heary, R.F. & Albert, T.J.) 154–170 (Thieme Medical Publishers, 2007).
- 20.Matsumoto M, et al. Postoperative distal adding-on and related factors in Lenke type 1A curve. Spine (Phila Pa 1976) 2013;38:737–744. doi: 10.1097/BRS.0b013e318279b666. [DOI] [PubMed] [Google Scholar]
- 21.Cidambi KR, et al. Postoperative changes in spinal rod contour in adolescent idiopathic scoliosis: An in vivo deformation study. Spine (Phila Pa 1976) 2012;37:1566–1572. doi: 10.1097/BRS.0b013e318252ccbe. [DOI] [PubMed] [Google Scholar]
- 22.Lamerain M, et al. CoCr rods provide better frontal correction of adolescent idiopathic scoliosis treated by all-pedicle screw fixation. Eur. Spine J. 2014;23:1190–1196. doi: 10.1007/s00586-014-3168-3. [DOI] [PubMed] [Google Scholar]
- 23.Giudici F, et al. Determinants of the biomechanical and radiological outcome of surgical correction of adolescent idiopathic scoliosis surgery: The role of rod properties and patient characteristics. Eur. Spine J. 2017;26(Suppl 4):524–532. doi: 10.1007/s00586-017-5148-x. [DOI] [PubMed] [Google Scholar]
- 24.Dick JC, Bourgeault CA. Notch sensitivity of titanium alloy, commercially pure titanium, and stainless steel spinal implants. Spine (Phila Pa 1976) 2001;26:1668–1672. doi: 10.1097/00007632-200108010-00008. [DOI] [PubMed] [Google Scholar]
- 25.Yamanaka K, et al. Analysis of the fracture mechanism of Ti-6Al-4V alloy rods that failed clinically after spinal instrumentation surgery. Spine (Phila Pa 1976) 2015;40:E767–E773. doi: 10.1097/BRS.0000000000000881. [DOI] [PubMed] [Google Scholar]
- 26.Slivka MA, Fan YK, Eck JC. The effect of contouring on fatigue strength of spinal rods: Is it okay to re-bend and which materials are best? Spine Deform. 2013;1:395–400. doi: 10.1016/j.jspd.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 27.Solla F, et al. Patient-specific rods for thoracic kyphosis correction in adolescent idiopathic scoliosis surgery: Preliminary results. Orthop. Traumatol. Surg. Res. 2020;106:159–165. doi: 10.1016/j.otsr.2019.07.027. [DOI] [PubMed] [Google Scholar]
- 28.Bharucha NJ, Lonner BS, Auerbach JD, Kean KE, Trobisch PD. Low-density versus high-density thoracic pedicle screw constructs in adolescent idiopathic scoliosis: Do more screws lead to a better outcome? Spine J. 2013;13:375–381. doi: 10.1016/j.spinee.2012.05.029. [DOI] [PubMed] [Google Scholar]
- 29.Larson AN, et al. Does higher anchor density result in increased curve correction and improved clinical outcomes in adolescent idiopathic scoliosis? Spine (Phila Pa 1976) 2014;39:571–578. doi: 10.1097/BRS.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 30.Liu H, et al. Main thoracic curve adolescent idiopathic scoliosis: Association of higher rod stiffness and concave-side pedicle screw density with improvement in sagittal thoracic kyphosis restoration. J. Neurosurg. Spine. 2015;22:259–266. doi: 10.3171/2014.10.SPINE1496. [DOI] [PubMed] [Google Scholar]
- 31.Pizones J, Sánchez-Mariscal F, Zúñiga L, Izquierdo E. Ponte osteotomies to treat major thoracic adolescent idiopathic scoliosis curves allow more effective corrective maneuvers. Eur. Spine J. 2015;24:1540–1546. doi: 10.1007/s00586-014-3749-1. [DOI] [PubMed] [Google Scholar]
- 32.Gehrchen M, Ohrt-Nissen S, Hallager DW, Dahl B. A uniquely shaped rod improves curve correction in surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2016;41:1139–1145. doi: 10.1097/BRS.0000000000001504. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author on reasonable request.