Abstract
Background:
Both the World Health Organization and the Intergovernmental Panel for Climate Change project that malnutrition will be the greatest contributor to climate change-associated morbidity and mortality. Although there have been several studies that have examined the potential effects of climate change on human health broadly, the effects on malnutrition are still not well understood. We conducted a systematic review investigating the role of three climate change proxies (droughts, floods, and climate variability) on malnutrition in children and adults.
Methods and findings:
We identified 22 studies examining the effects of droughts, floods, and climate variability on at least one malnutrition metric. We found that 17 out of 22 studies reported a significant relationship between climate change proxies and at least one malnutrition metric. In meta-analysis, drought conditions were significantly associated with both wasting (Odds Ratio[OR] 1.46, 95% Confidence Interval[CI] 1.05-2.04) and underweight prevalence (OR 1.46, 95% CI 1.01-2.11).
Conclusions:
Given the long-term consequences of malnutrition on individuals and society, adoption of climate change adaptation strategies such as sustainable agriculture and water irrigation practices, as well as improving nutritional interventions aimed at children aged 1-2 years and older adults, should be prioritized on global policy agendas in the coming years.
Introduction
Global climate change poses some of the most pressing global health challenges of our time. Due to rapid increases in greenhouse gas emissions over the past century, temperatures are increasing, precipitation patterns are changing, and weather events such as floods and droughts are becoming more frequent and more intense.1, 2 These changes affect human health by a number of different pathways, including altered crop production3, 4; increases in heat stroke5, 6; changes in access to fresh water7; violence in areas with limited environmental resources8; altered distribution of certain infectious diseases such as malaria, dengue, and cholera9, 10; and reduced productivity of aquatic ecosystems due to ocean acidification11, 12.
Climate change is estimated to have caused approximately 5.5 million DALYs and 154,000 deaths in the year 2000 -- approximately half of which were due to malnutrition.13, 14 But while there has been considerable research into the potential effects of climate change on human health broadly, the effects of climate change on malnutrition are still not well understood. This is especially important given that malnutrition further affects individual and population health through reduced child survival, decreased immune function, increased maternal mortality, increased susceptibility to infectious diseases, and stunted growth.15, 16
Climate change refers to long-term changes in temperature and precipitation that occur over the timespan of centuries or millennia.17 The Intergovernmental Panel on Climate Change indicates that human-induced climate change caused by increased greenhouse gas emissions has already increased average surface temperatures by about 0.17°C per decade since 1970 and will continue to increase global mean surface temperatures by 1.8°C to 4.0°C by the year 2100.18 Climate change is distinct from climate variability, which refers to natural fluctuations in temperature and precipitation that occur or periods of months to years, such as the El Niño Southern Oscillation.19, 20 The primary difference between the two centers around their temporal scales: climate variability typically occurs on the scale of months to years while climate change occurs on the scale of decades to millennia.21, 22
A previous literature review mainly focusing on articles before the year 2000 examined the association between climate variability and childhood stunting and found variable associations.23 Specifically, it found that extreme weather events and fluctuations in temperature and precipitation were associated with childhood stunting in 12 out of 15 studies. Here, we aimed to provide a more comprehensive, updated, and quantitative systematic review of the literature by assessing the effects of floods, droughts, and fluctuations in temperature and precipitation on anthropometric measurements such as wasting, stunting, and underweight prevalence among both pediatric and adult populations. As a secondary goal, we also sought to identify additional factors that could mediate or moderate this relationship.
Methods
Inclusion Criteria
We included any studies that: (a) were published in English during or after the year 2000, (b) had study objectives related to the relationship between climate change and malnutrition, (c) relied on quantitative clinical metrics for malnutrition, and (d) included the presence of drought, flooding, or climate variability.
Study Selection
We performed a systematic search within Web of Science, SCOPUS, and PubMed using the following keywords: [“climate change” or “global warming” or “flooding” or “drought” or “greenhouse gases” or “extreme weather” or “climate variability”] AND [“malnutrition” or “undernutrition” or “nutrition” or “food security” or “body-mass index” or “wasting” or “stunting” or “anemia” or “underweight”]. We limited papers to during or after the year 2000 to ensure that the data was recent and consistent with contemporary trends in climate change research. We reviewed the grey literature using the same search terms in Google Scholar, Eldis, and OAISTER to ensure that all relevant articles were included.
Selection Criteria
ML initially screened potentially relevant articles based on the title and abstract to determine if they met the inclusion criteria for full-text review. Final inclusion was assessed by two reviewers (ML and KK). Reviewers discussed any discrepancies of inclusion, and we obtained consensus on final inclusion.
We defined malnutrition using anthropometric metrics including wasting, stunting, and underweight. Stunting and underweight were measured exclusively in children and defined using height-for-age and weight-for-age z-scores, respectively, more than two standard deviations below the WHO growth standards median. Wasting was measured among both children and adults: in children, it was defined as weight-for-height or mid-upper arm circumference z-scores greater than two standard deviations below the WHO child growth standards median, while among adults, it was defined as a body-mass index (BMI) less than 18.5 kg/m2. We excluded articles that focused exclusively on food security metrics, such as agricultural output, rather than nutritional outcomes.
We conceptualized climate variability as fluctuations in temperature and precipitation based on a long-term mean (i.e. climate variability) and extreme weather events as droughts and floods. While it is possible – even likely -- that the floods and droughts covered in this review were not themselves caused by climate change, they serve as proxies for the future effects of climate change since both floods and droughts are projected to increase in frequency and intensity due to climate change.1, 24, 25 We excluded qualitative studies, reviews of studies, commentaries, editorials, and opinion articles. We also excluded modeling papers that project the future effects of climate change on malnutrition but used some as supporting documents (figure 1).
Figure 1.
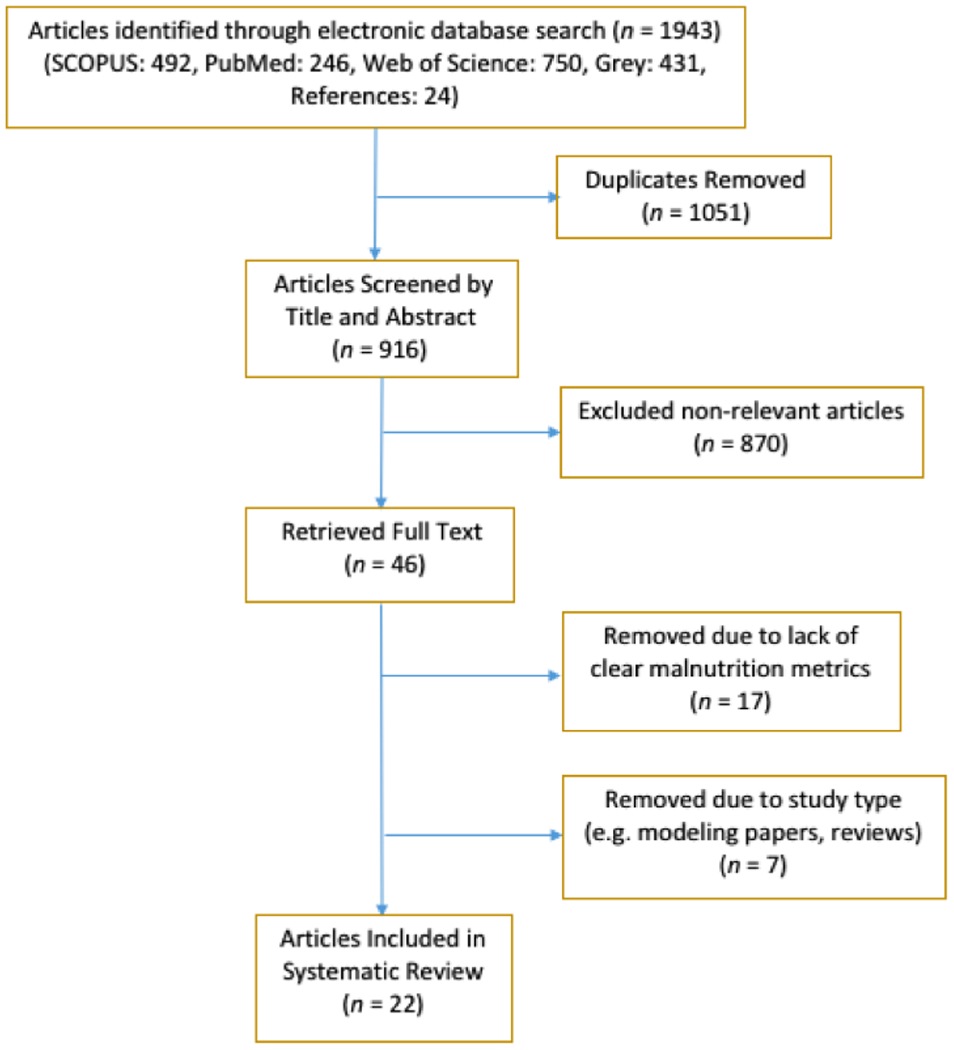
PRISMA Flow Diagram
Data Extraction
Following the initial search, we developed a standardized form to extract the following data: (1) study period, (2) study population, (3) study type, (4) age of participants, (5) climate change proxy, (6) malnutrition metric, (7) presence/absence and degree of significant changes in malnutrition prevalence, and (8) moderating or mediating variables.
Data Analysis
Following data extraction, we divided the articles into three groups based on climate change proxy (droughts, floods, or climate variability) and then subdivided them based on malnutrition metric (wasting, stunting, or underweight). We then compared the results of those studies looking at similar metrics. We assessed the quality of each study using the NIH tool for Observational Cohort and Cross-Sectional Studies.26 Two reviewers agreed upon quality ratings of “Good,” “Fair”,” or “Poor” (ML and KK). Where possible, we pooled data using random effects odds ratio meta-analyses.
Results
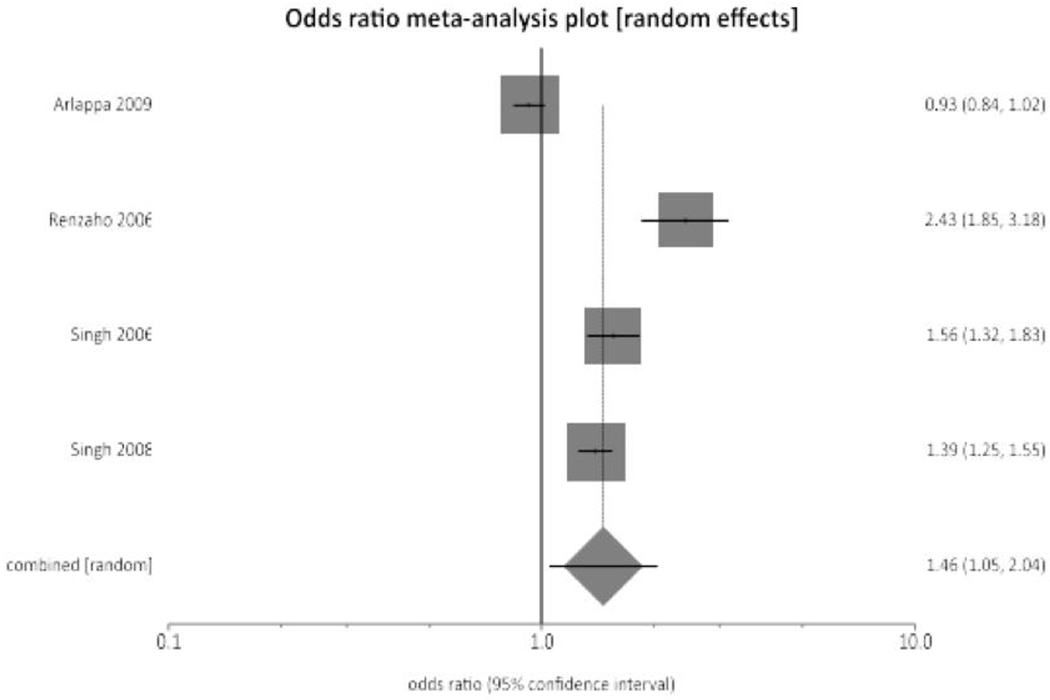
Our initial search yielded 916 studies, of which 22 met criteria for inclusion in this systematic review. The sample sizes of the included studies ranged from 145 individuals to 20,122 households, with a median of 3,657 individuals. Seventeen studies looked exclusively at malnutrition in children, 2 looked exclusively at malnutrition in adults, and 3 looked at malnutrition in both children and adults. Of the final 22 studies, 13 focused on droughts, 4 on floods, and 5 focused on long-term fluctuations in temperature and precipitation (climate variability). With regard to malnutrition metrics, 15 looked at stunting, 15 at wasting, and 12 at underweight.
Overall study quality was variable. Six studies were considered “Good,” 14 were considered “Fair,” and 2 were given a rating of “Poor.” Of those that received a “Fair” or “Poor” rating, 6 were confounded by food aid,27–32 2 relied on control data that was over 10 years old,33, 34 3 lacked a comparison group,35, 36 and 2 failed to provide sufficient time between the climate change exposure and malnutrition outcome.27, 37 Figure 2 displays the characteristics and main findings of the final 22 studies.
Figure 2.
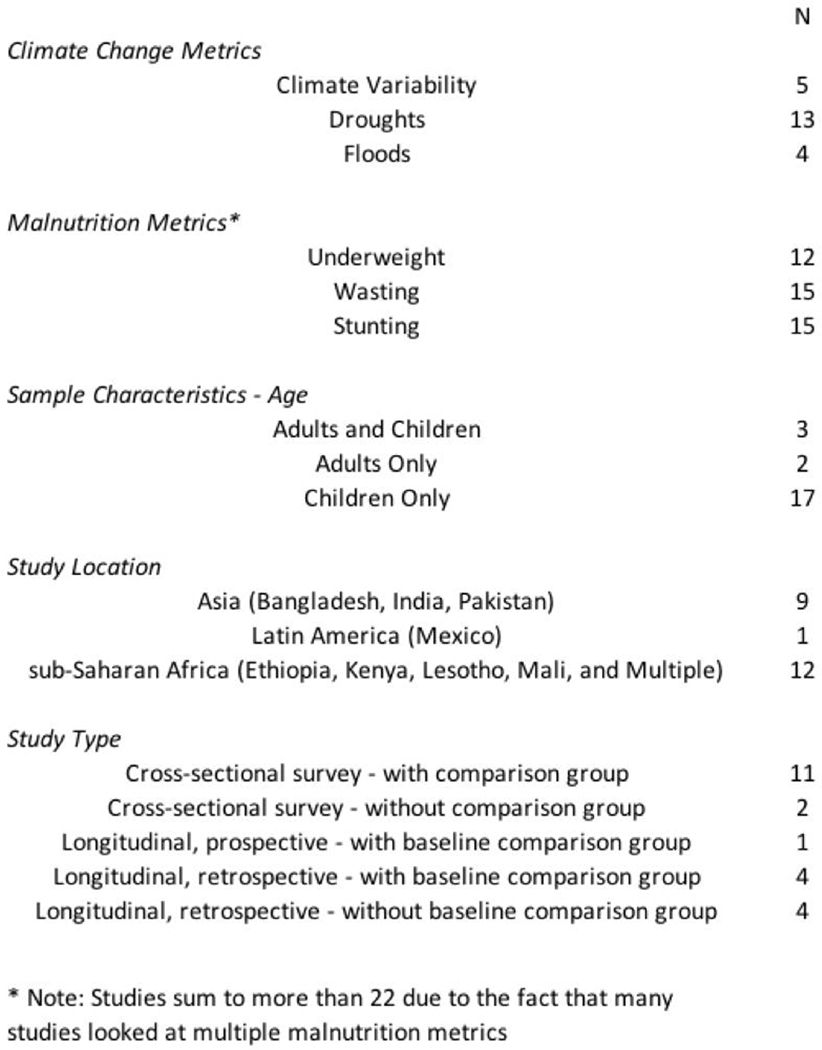
Study Types and Characteristics
Droughts
Figure 3 displays the characteristics and main findings of the 13 drought studies. Eight of these studies sampled children exclusively, 2 sampled adults exclusively, and 3 sampled both children and adults. Of the 10 studies that looked at drought and wasting, 6 found a significant positive association.
Figure 3.
Drought and Malnutrition
All of the drought studies focused primarily on rural locations with two including a combination of both rural and urban regions. Of these two, one found a higher level of childhood mortality and undernutrition in rural areas while the other found a higher prevalence of underweight among children living in semi-urban areas (i.e. near towns) in sub-Saharan Africa. It was hypothesized that the latter finding was due to preferential food aid distribution to more rural areas as well as an increased HIV prevalence in urban and semi-urban areas27, 39.
Nearly all of the drought studies also focused on populations in sub-Saharan Africa or India that relied heavily on subsistence agriculture for food and income29, 34, 40, 41. Of the seven studies that focused on sub-Saharan Africa, four examined the effects of a severe and prolonged period of drought between 2001-2004 that heavily impacted crop production and food availability in much of the continent. During this crisis, it is estimated that at least 15 million people in the six countries of southern Africa (Lesotho, Malawi, Mozambique, Swaziland, Zambia and Zimbabwe) became severely food insecure. Due in part to these food shortages, market failures and social and political upheavals also plagued many of these countries, further worsening the availability and efficacy of government-sponsored food aid programs38, 39, 42.
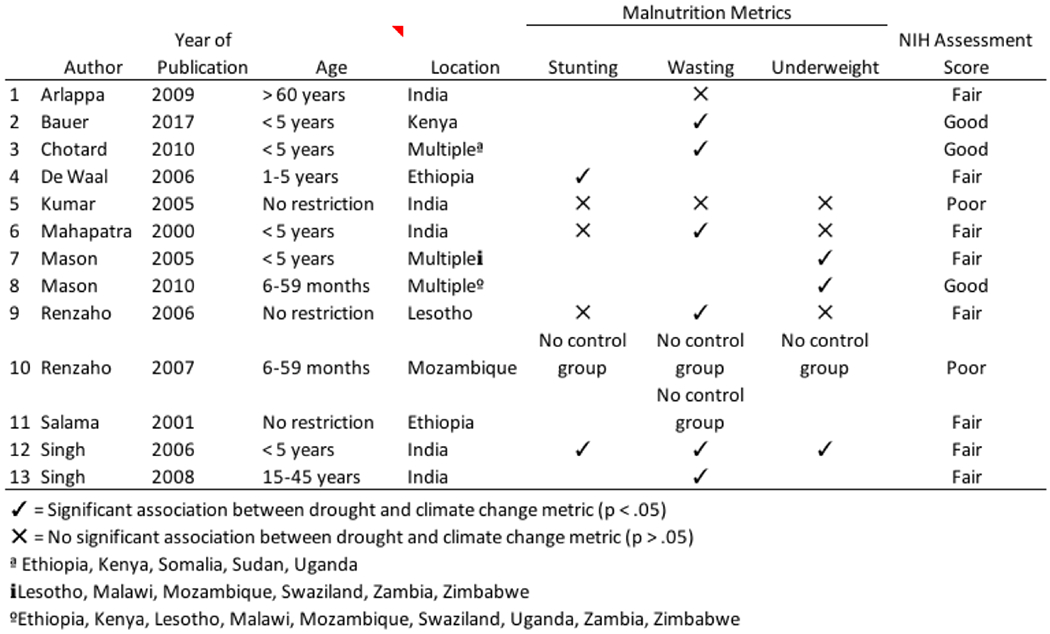
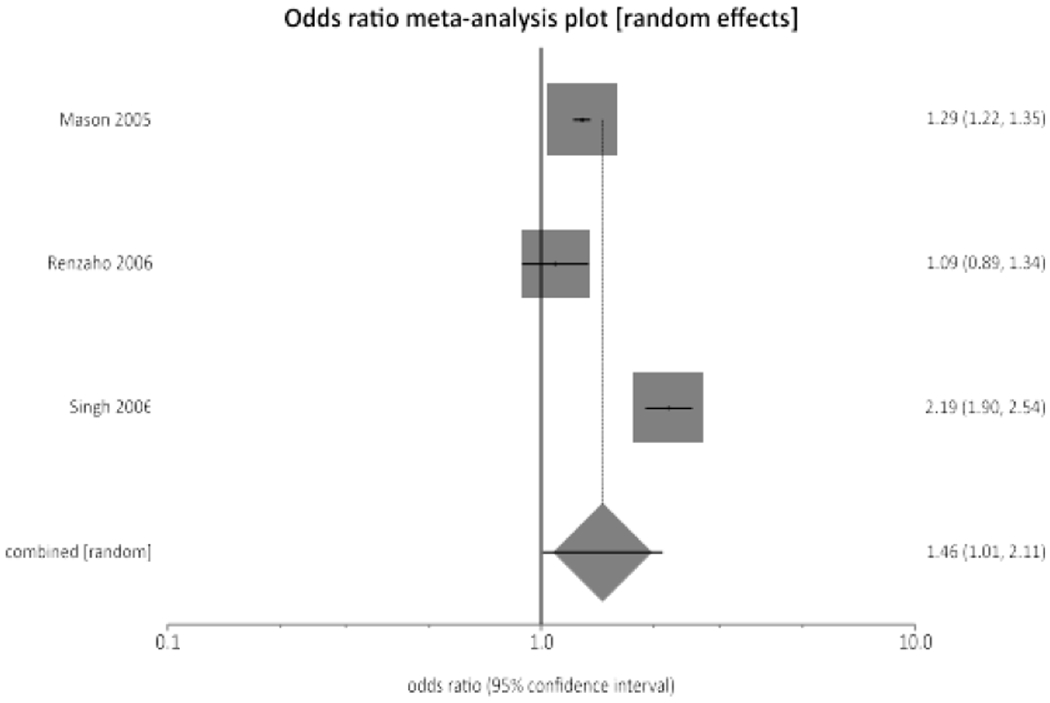
A meta-analysis of the 5 cross-sectional studies with available data that looked at the effects of drought on wasting found a pooled odds ratio of 1.21 (95% CI = 0.79-1.84). Of these studies, 2 looked exclusively at adults and defined wasting as a BMI < 18.5 kg/m2, 1 looked exclusively at children and defined wasting as weight-for-height z-scores 2SD below the WHO median, and 3 looked at both children and adults and relied upon both metrics.
The lack of statistical significance in the initial meta-analysis was driven, in part, to data from Kumar (2005), which found that wasting was actually less prevalent among both children and adults during drought conditions than non-drought conditions. This counterintuitive finding may have been attributed to the presence of food aid in the region during the drought, which also resulted in the study receiving a “Poor” rating. Removing this study from the meta-analysis resulted in an odds ratio of 1.46 (95% CI = 1.05-2.04). Figure 4 shows a forest plot of the four studies.
Figure 4.
Pooled odds ratios from the four studies with control data that looked at drought and wasting prevalence.
Of the 7 studies that looked at drought and underweight, 3 found a significant, positive association. All 7 studies looked at underweight prevalence exclusively in children and defined underweight as weight-for-age z-scores 2 SDs below the WHO median. Of the 3 studies that did find a significant association, 2 looked at the prevalence of underweight in a number of countries in sub-Saharan Africa before and after a drought crisis from 2001-2003.43, 44 During the initial drought period, the prevalence of underweight increased 5-7 percentage points per year, while in the three years following the drought, the prevalence decreased 0.1-0.9 percentage points per year until reaching pre-drought levels. A meta-analysis combining the 4 studies with control group data found a pooled odds ratio of 1.31 (95% CI = 1.25-1.38). Removing the Kumar study, which was confounded by food aid, resulted in an odds ratio of 1.46 (95% CI = 1.01-2.11). Figure 5 shows a forest plot combining the 3 studies.
Figure 5.
Pooled odds ratios from the four studies with control data that looked at drought and underweight prevalence.
Stunting was included in 6 studies where drought was the climate change proxy. In all 6 studies, stunting was measured exclusively in children and was defined as height-for-age z-scores 2 SDs below the WHO median. Of these studies, 2 found a significant association while 4 did not. In Singh et al (2006), the prevalence of severe childhood stunting following a 2003 drought in India was 10%, significantly more than that found by the National Institute of Nutrition during a previous non-drought period (1.6%). In addition, in De Waal et al (2006), the prevalence of stunting among children aged 1-5 years old in drought-affected areas of Ethiopia was 57%. A meta-analysis was not conducted on stunting due to a lack of available control data.
Floods
Figure 6 displays the characteristics and main findings of the 4 flood studies, all of which looked exclusively at children. All 4 studies looked at the effects of flooding on stunting, with three also looking at wasting and underweight prevalence. A meta-analysis was not performed looking at floods and malnutrition due to a lack of available control data.
Figure 6.
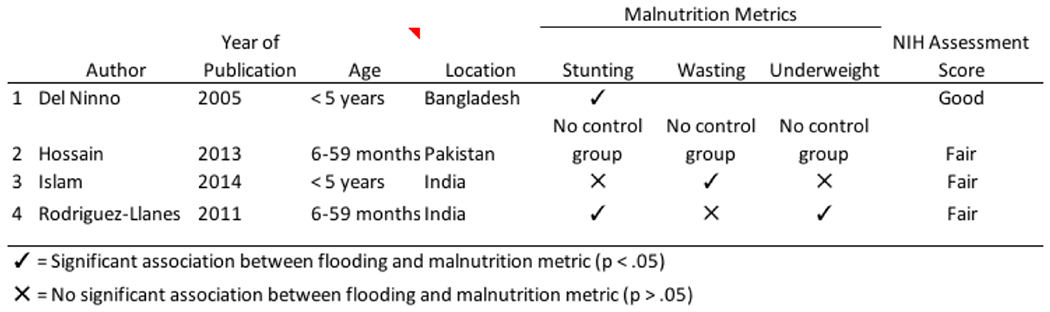
Floods and Malnutrition
All four of the flood studies looked at countries in South Asia, including India, Pakistan, and Bangladesh. This region is particularly vulnerable to flooding due to a number of high-density population centers located in low-lying coastal areas around the Bay of Bengal45. According to a 2019 study in the journal Nature Communications, 75% of the 300 million people worldwide who currently reside in areas at risk of flooding due to climate change live in China, Bangladesh, India, Vietnam, Indonesia, or Thailand46.
All four of the studies that looked at the effects of flooding on malnutrition also focused on rural, agrarian societies where food access and livelihoods are directly linked to crop production. In Bangladesh, for example, domestically produced rice and wheat accounts for about 80% of the average person’s daily caloric intake47. The largest of the four flood studies found that decreases in rice production were partially responsible for increased levels of stunting among 4,433 Bangladeshi children following a devastating flood in the summer of 1998 that covered over two-thirds of the country. In the study, children living in flood-exposed regions of Bangladesh were significantly more likely to be stunted by one-half of one standard deviation compared to flood-unexposed children. For a 3-year-old child, this corresponded to a difference of more than 5 centimeters48.
Of the 3 studies that looked at flooding and underweight, two found that children living in flood-affected communities were more likely to be underweight than those living in non-flooded communities. In Rodriguez Llanes et al (2011), flood-exposed children in rural India were 86% more likely to be stunted than flood-unexposed children, and the difference was statistically significant (Adjusted prevalence ratio 1.86; 95% CI = 1.04-3.30).37 In Hossain et al (2013), the prevalence of underweight among children in severely flood-affected regions of Pakistan (46-48%) was also higher than in moderately affected regions (39%-40%), though no significance values were reported.35
Wasting was also evaluated in 3 of the flood studies, 1 of which found a significant association.35, 37, 49 In Islam et al (2014), the prevalence of underweight was found to be 21.6% in the flood-affected areas of Assam, India, compared to 13.7% in non-flooded areas. In the other 2 studies, wasting was still more prevalent in the flooded regions, but the differences were not statistically significant.35, 37
Climate Variability
The main results and characteristics of the 5 climate variability studies are summarized in Figure 7. A meta-analysis was not performed on these studies due to a lack of available control data and a heterogeneity of metrics.
Figure 7.
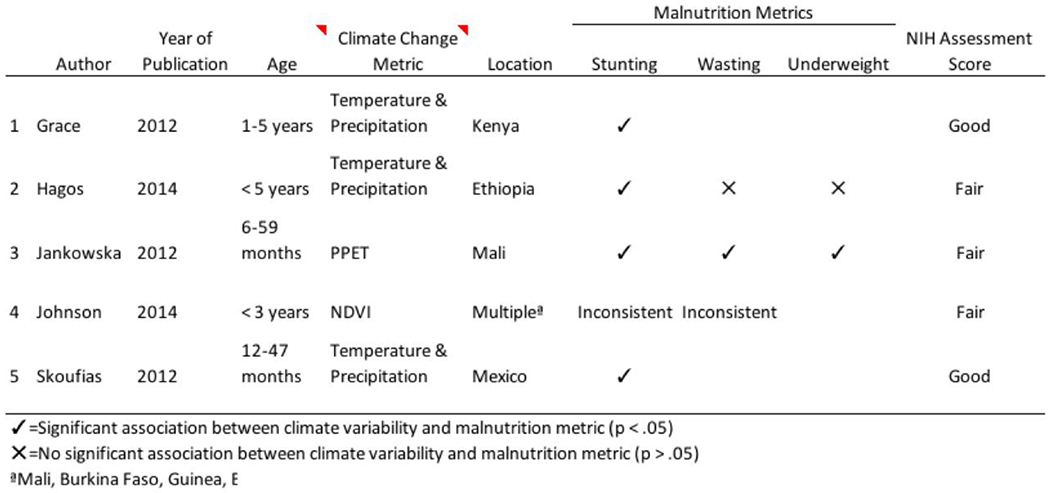
Climate Variability and Malnutrition
All 5 of the studies that looked at climate variability and stunting found a significant association. However, the direction of this relationship was inconsistent across studies. Two of the 5 studies found that increases in precipitation and decreases in temperature were significantly correlated with stunting,50, 51 while two found that decreases in precipitation were significantly correlated with stunting.52, 53
Skoufias et al (2012), for example, calculated weather “shocks” in Mexico based on the degree of deviation from the 1951-1985 average temperature and rainfall levels in the region. Positive or negative rainfall shocks were defined by indicator variables identifying those years when the rainfall was, respectively, plus or minus one standard deviation from the region’s long-term mean. Similarly, positive or negative temperature shocks were applied to those years when the average annual temperature was plus or minus one standard from the long-term mean. The authors found that positive rainfall shocks were significantly associated with stunting. More specifically, children who experienced more rainfall had, on average, height-for-age z-scores that were 0.32-0.87 lower than children who experienced an average amount of rain during the rainy season. In this case, malaria was proposed as a mediating factor.
Of the 3 studies that looked at climate variability and wasting, 2 found a significant positive association. In Jankowska et al (2012), for example, the authors used a composite metric based on temperature and rainfall patterns (PPET) to identify regions of Mali as arid (PPET < −100) or semi-arid (PPET > −100). Increases in this composite metric were used as a proxy by the study authors for increased temperature and precipitation. The researchers found that both stunting and underweight prevalence were significantly greater in arid regions than semi-arid regions. Decreased crop yields in the arid regions were proposed as a likely mediating factor.
Factors Related to Malnutrition
In an effort to better understand the mechanisms linking climate change proxies and malnutrition, a number of potential mediating and moderating variables were identified among the 22 studies. Figure 8 shows a visual representation of the direction and strength of these mediating and moderating variables on malnutrition.
Figure 8.
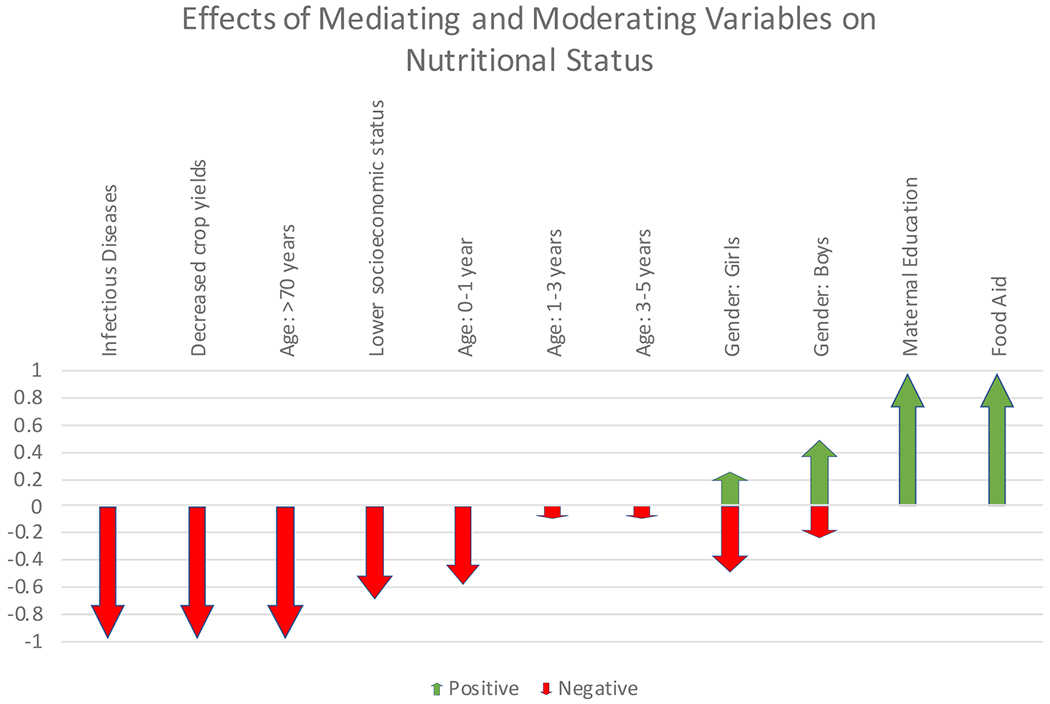
Factors Mediating/Moderating Effects of Climate Change on Malnutrition
Mediating Variables
Infectious Disease Co-Morbidities: Infectious disease co-morbidities were identified as potential mediating factors in 6 of the studies.36, 43, 44, 50, 51, 54 Of these, 3 focused on malaria, 2 on HIV/AIDS, and 1 on measles. In the malaria studies, increases in precipitation were thought to also increase the range of the Anopheles mosquito, thereby increasing the spread of malaria and the development of anemia. Particularly in children, malarial anemia can result in delayed growth and have long-term effects on neurological development.55 The 2 studies that focused on HIV/AIDS found that regions with a higher HIV/AIDS prevalence—which were often in or near urban areas—were also more vulnerable to the effects of drought on malnutrition.
Crop yields: Crop yields were identified as a potential mediating factor in 3 studies.29, 51, 52 All 3 found that decreases in crop yields were associated with increases in child malnutrition. In Hagos et al (2014), for example, the authors found that livelihood zones with a higher per capita crop availability had a relatively lower prevalence of wasting. Similarly, in Grace et al (2012), children living in a mixed farming zone in Kenya had significantly lower height-for-age scores than those living in the higher producing Central zone.
Moderating Variables
Age: Age was identified as a factor related to malnutrition outcomes in nearly half of the studies.30, 35, 37, 50, 54, 56 For those studies that included children, most found that children between the ages of 1 and 2 years were most vulnerable to the effects of climate change on malnutrition.48, 56 However, Rodriguez-Llanes et al (2011) found that children in the 26- to 36-month age group (2-3 years) were more vulnerable to floods than either their younger or older counterparts (difference in Z score = −1.1; p < 0.001). Among adults, Arlappa et al (2009) found that older adults (> 70 years old) were more vulnerable to wasting during a severe drought than younger adults (60-69 years old).
Socioeconomic status: Seven studies looked at socioeconomic status as a variable related to climate change proxies and malnutrition.27, 29, 30, 44, 51, 52, 54 Of these, 5 found that the poorest members of the population were the most vulnerable to the effects of climate change on malnutrition.
Food Aid: Six studies mentioned government or international food aid as a factor moderating the effects of climate change proxies on malnutrition.27–30, 48, 50 This factor limited the internal validity of many of the included studies. In Arlappa (2009) and Kumar (2005), for example, the authors suggest that Indian government interventions such as the Food for Work Program and Targeted Public Distribution System may have buffered the effects of drought on wasting in children and adults.
Gender: Gender was identified as a relevant factor in 4 of the studies.29, 34, 50, 56 Of these, 2 suggested that girls were more vulnerable than boys to malnutrition in the setting of droughts and 1 suggested that boys were more vulnerable than girls to the effects of increased precipitation on malnutrition. The fourth study looked exclusively at adults and found that adult men were more susceptible to wasting than adult women during drought conditions (p < 0.01).
Mother’s education level: Maternal education was identified as a related factor in 4 studies, all of which looked at climate variability.50, 52–54 All 4 of these studies found that higher levels of maternal education were protective against the development of malnutrition in children.
Discussion
To the best of our knowledge, this may be the first systematic review and meta-analysis to evaluate the effects of climate change proxies on malnutrition using current research with a focus on both children and adults. Of the 22 articles in this review, 17 found an important relationship between climate change proxies and at least one of the malnutrition metrics, indicating a strong positive relationship between climate change and malnutrition. Meta-analyses using a subset of drought studies also showed that drought conditions were significantly associated with both wasting and underweight prevalence.
While some studies found that climate change had an effect on all of the malnutrition metrics, most studies found that climate change proxies were associated with increases in some malnutrition metrics but not others. This is largely due to the fact that some metrics (e.g. stunting) are an indication of chronic malnutrition, while others (e.g. wasting) indicate acute malnutrition. Thus, which malnutrition metric was most affected depended heavily on the timing of the study, with wasting, underweight, and nutrient deficiencies being more prevalent in the weeks and months following an extreme weather event and stunting being more common years afterwards.
A thorough investigation of the mechanisms linking climate change to malnutrition lies outside the scope of this study. However, this review highlights a number of important mechanisms that could potentially mediate this relationship, including decreased crop production and an increased prevalence of infectious diseases such as HIV and malaria. In all 3 of the studies that tracked crop yields, malnutrition was greater in regions with lower crop productivity. In South Asia, for example, the destruction of rice fields during extreme flooding events was found to be a particularly strong factor linking climate change with malnutrition48. In sub-Saharan Africa, the decreased production of cereals, particularly maize, during periods of drought was also found to be a strong predictor of malnutrition38. These findings underscore the importance of implementing sustainable agriculture and water irrigation strategies as techniques for combating the negative effects of climate change on human nutrition.
With regard to infectious disease prevalence, the increased spread of vector-borne diseases such as malaria was also referenced across studies as a potential factor linking increased temperature and precipitation with malnutrition. Combatting these diseases by distributing insecticide-treated bed-nets and draining stagnant water to reduce mosquito breeding could therefore serve a powerful role in protecting vulnerable population from the negative health effects of climate change. Increased HIV transmission due to rural-to-urban migration was also noted to worsen nutritional outcomes during periods of drought in sub-Saharan Africa, suggesting that HIV infection could also amplify the effects of droughts on malnutrition39. Targeting migrant populations in urban nutritional assistance and HIV surveillance programs could therefore be an effective strategy to combat the effects of climate change on malnutrition in areas with a high HIV prevalence.
This review also highlighted a number of factors moderating the effects of climate and weather variability on malnutrition. Of these, age was found to be one of the most significant, with younger children and older adults being the most vulnerable to changes in weather and climate. Among children, those in the 1-2 year age group were found to be the most vulnerable to drought conditions -- likely due to changes in infancy feeding patterns during this period -- while adults over 70 years old were found to be more vulnerable than adults aged 60-69 years old. This is consistent with previous research suggesting that younger children and older adults are particularly vulnerable to the health effects of climate and weather variability in both developed and developing countries57, 58. Older adults are thought to be at higher risk of becoming malnourished due to a combination of physiological changes, restrictive financial and social status, and functional decline. Older adults are also often left alone at home while their children migrate to distant urban areas seeking seasonal work during and after extreme weather events30.
Gender was also found to be a relevant moderating factor in four studies. Two studies found that girls were more vulnerable than boys to the effects of climate change on malnutrition while one found that boys were more vulnerable than girls. These findings are a consistent with previous research highlighting the increased vulnerability of girls to extreme weather events due to a variety of social factors, including the preferential allocation of food to boys in some cultures59, 60. Among adults, one study found that men aged 15-45 years were more likely to experience wasting than women during droughts, which was thought to be due to increased seasonal migration among men searching for work and food34.
Two topic areas that were underrepresented in this study include the impact of floods on malnutrition and the impact of climate change proxies on adult, rather than child, malnutrition. With regard to flooding, only 4 of the 22 studies in this review looked at the impact of floods on malnutrition, and all 4 were based in South Asia. More research from a more diverse range of countries and continents is urgently needed to help fill in this gap in the literature, particularly due to the topic’s increasing relevance and importance in the coming years. The topic of adult malnutrition was also heavily underrepresented in our review of the literature. Of the 22 studies in the review, only 2 looked exclusively at malnutrition in adults30, 34 while 3 looked at malnutrition in both children and adults.28, 29, 36
Our study has a number of limitations. First, available data regarding control groups was limited, particularly in those studies that focused on droughts and floods. This is an unfortunate consequence of conducting research in this field, as unpredictable weather events make it difficult, if not impossible, to prospectively identify control groups. Our review may have also been influenced by publication bias since those studies that found no significance may have been less likely to be published. In the future, utilization of the snowball method could better assist in the identification of studies that did not reach statistical significance. A funnel plot could also be used to help identify publication bias but was not possible for this review due to inconsistent effects measures across studies. With regard to our inclusion and exclusion criteria, studies that looked at extreme weather events such as hurricanes and typhoons were excluded, even though many were likely accompanied by flooding, which was included. This decision was made in order to provide consistency with regard to our exposure metrics and to eliminate other confounders that may accompany such events, such as wind damage. This review also looked almost exclusively at malnutrition in low- and middle-income countries, where people are highly reliant on subsistence agriculture for income and food. While we did not intend for this to happen, one of our selection criterion (that studies include quantitative metrics for malnutrition) excluded the relatively few studies that looked at malnutrition and climate change proxies in high-income nations. Consequently, the results of this review may not be generalizable to more industrialized nations where populations are less reliant on subsistence agriculture. Finally, our review treated both flooding and droughts as dichotomous variables—either a community was affected or it was not—even though the severity of these events likely differed across studies and even within the samples of each study.
Conclusion
The World Health Organization (WHO) projects that malnutrition will be the greatest contributor to morbidity and mortality as a result of climate change.62 We present a systematic review and meta-analysis of the literature linking climate change proxies with malnutrition in both children and adults. We found that 17 out of 22 studies reported a significant relationship between climate change proxies and at least one malnutrition metric. In addition, meta-analyses using a subset of drought studies showed that drought conditions increased the odds of wasting and underweight by nearly 50%. Due to the long-term consequences of malnutrition on individuals and society, adoption of adaptation strategies such as teaching sustainable agriculture practices and increasing educational opportunities for women should therefore attain a high place on global public policy agendas in the coming years.
References
- 1.Hirabayashi Y, Mahendran R, Koirala S, et al. Global flood risk under climate change. Nature Climate Change. 2013;3(9):816. [Google Scholar]
- 2.Trenberth KE. Changes in precipitation with climate change. Climate Research. 2011;47(1/2):123–138. [Google Scholar]
- 3.Lobell DB, Schlenker W, Costa-Roberts J. Climate trends and global crop production since 1980. Science. 2011;333(6042):616–620. [DOI] [PubMed] [Google Scholar]
- 4.Ray DK, Gerber JS, MacDonald GK, West PC. Climate variation explains a third of global crop yield variability. Article. Nature Communications January 2015;6:9. 5989. doi: 10.1038/ncomms6989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kjellstrom T Climate change, direct heat exposure, health and well-being in low and middle-income countries. Global Health Action. 2009;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luber G, McGeehin M. Climate change and extreme heat events. American journal of preventive medicine. 2008;35(5):429–435. [DOI] [PubMed] [Google Scholar]
- 7.Hanjra MA, Qureshi ME. Global water crisis and future food security in an era of climate change. Food Policy. 2010;35(5):365–377. [Google Scholar]
- 8.Brown O, Crawford A. Rising temperatures, rising tensions: climate change and the risk of violent conflict in the Middle East. 2009; [Google Scholar]
- 9.Zell R Global climate change and the emergence/re-emergence of infectious diseases. Int J Med Microbiol. April 2004;293 Suppl 37:16–26. [DOI] [PubMed] [Google Scholar]
- 10.Rosenthal J Climate change and the geographic distribution of infectious diseases. Ecohealth. December 2009;6(4):489–95. doi: 10.1007/s10393-010-0314-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Reilly CM, Alin SR, Plisnier PD, Cohen AS, McKee BA. Climate change decreases aquatic ecosystem productivity of Lake Tanganyika, Africa. Nature. 2003:766–8. vol. 6950. [DOI] [PubMed] [Google Scholar]
- 12.Hoegh-Guldberg O, Bruno JF. The impact of climate change on the world’s marine ecosystems. Science. 2010;328(5985):1523–1528. [DOI] [PubMed] [Google Scholar]
- 13.Kim KH, Kabir E, Ara Jahan S. A review of the consequences of global climate change on human health. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2014;32(3):299–318. doi: 10.1080/10590501.2014.941279 [DOI] [PubMed] [Google Scholar]
- 14.Ebi KL. Adaptation costs for climate change-related cases of diarrhoeal disease, malnutrition, and malaria in 2030. Global Health. 2008;4:9. doi: 10.1186/1744-8603-4-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. The lancet. 2008;371(9609):340–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martorell R The nature of child malnutrition and its long-term implications. Food and nutrition Bulletin. 1999;20(3):288–292. [Google Scholar]
- 17.Pachauri RK, Reisinger A. IPCC fourth assessment report. IPCC, Geneva. 2007:2007. [Google Scholar]
- 18.Change IPOC. IPCC. Climate change. 2014; [Google Scholar]
- 19.McMichael AJ, Kovats RS. Climate change and climate variability: adaptations to reduce adverse health impacts. Environmental Monitoring and Assessment. 2000;61(1):49–64. [Google Scholar]
- 20.Ziervogel G, Nyong A, Osman B, Conde C, Cortés S, Downing T. Climate variability and change: implications for household food security. Assessment of Impacts and Adaptations to Climate Change (AIACC): Washington, DC, USA. 2006; [Google Scholar]
- 21.Zhang T, Huang Y. Impacts of climate change and inter-annual variability on cereal crops in China from 1980 to 2008. Journal of the Science of Food and Agriculture. 2012;92(8):1643–1652. doi: 10.1002/jsfa.5523 [DOI] [PubMed] [Google Scholar]
- 22.Smit B, Burton I, Klein RJ, Wandel J. An anatomy of adaptation to climate change and variability. Climatic change. 2000;45(1):223–251. [Google Scholar]
- 23.Phalkey RK, Aranda-Jan C, Marx S, Hofle B, Sauerborn R. Systematic review of current efforts to quantify the impacts of climate change on undernutrition. Proc Natl Acad Sci U S A. August 18 2015;112(33):E4522–9. doi: 10.1073/pnas.1409769112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Change IPoC. Climate Change 2014–Impacts, Adaptation and Vulnerability: Regional Aspects. Cambridge University Press; 2014. [Google Scholar]
- 25.Dai A. Increasing drought under global warming in observations and models. Nature Climate Change. 2013;3(1):52. [Google Scholar]
- 26.Sanderson S, Tatt ID, Higgins JP. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. International journal of epidemiology. 2007;36(3):666–676. [DOI] [PubMed] [Google Scholar]
- 27.De Waal A, Taffesse AS, Carruth L. Child survival during the 2002-2003 drought in Ethiopia. Glob Public Health. 2006;1(2):125–32. doi: 10.1080/17441690600661168 [DOI] [PubMed] [Google Scholar]
- 28.Renzaho A. Mortality malnutrition and the humanitarian response to the food crises in Lesotho. Australasian Journal of Paramedicine. 2015;4(4) [Google Scholar]
- 29.Kumar S, Bhawani L. Managing child malnutrition in a drought affected district of Rajasthan--a case study. Indian J Public Health. October-December 2005;49(4):198–206. [PubMed] [Google Scholar]
- 30.Arlappa N, Venkaiah K, Rao KM, et al. Prevalence of chronic energy deficiency in rural-dwelling older Indian adults during a period of severe drought. J Nutr Elder. July 2009;28(3):301–12. doi: 10.1080/01639360903140338 [DOI] [PubMed] [Google Scholar]
- 31.Renzaho AMN Mortality Rates, Prevalence of Malnutrition, and Prevalence of Lost Pregnancies among the Drought-Ravaged Population of Tete Province, Mozambique. Prehospital and Disaster Medicine. 2007;22(1):26–34. doi: 10.1017/S1049023X00004301 [DOI] [PubMed] [Google Scholar]
- 32.Bauer JM, Mburu S. Effects of drought on child health in Marsabit District, Northern Kenya. Economics & Human Biology. 2017/February/01/ 2017;24(Supplement C):74–79. doi: 10.1016/j.ehb.2016.10.010 [DOI] [PubMed] [Google Scholar]
- 33.Singh MB, Fotedar R, Lakshminarayana J, Anand PK. Studies on the nutritional status of children aged 0-5 years in a drought-affected desert area of western Rajasthan, India. Public Health Nutr. December 2006;9(8):961–7. [DOI] [PubMed] [Google Scholar]
- 34.Singh MB, Lakshminarayana J, Fotedar R. Chronic energy deficiency and its association with dietary factors in adults of drought affected desert areas of Western Rajasthan, India. Asia Pac J Clin Nutr. 2008;17(4):580–5. [PubMed] [Google Scholar]
- 35.Hossain S, Talat M, Boyd E, et al. Evaluation of Nutrition Surveys in Flood-affected Areas of Pakistan: Seeing the Unseen! IDS Bulletin. 2013;44(3):10–20. [Google Scholar]
- 36.Salama P, Assefa F, Talley L, Spiegel P, van Der Veen A, Gotway CA. Malnutrition, measles, mortality, and the humanitarian response during a famine in Ehiopia. Jama. August 1 2001;286(5):563–71. [DOI] [PubMed] [Google Scholar]
- 37.Rodriguez-Llanes JM, Ranjan-Dash S, Degomme O, Mukhopadhyay A, Guha-Sapir D. Child malnutrition and recurrent flooding in rural eastern India: a community-based survey. BMJ Open. January 1 2011;1(2):e000109. doi: 10.1136/bmjopen-2011-000109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Renzaho AM. Mortality rates, prevalence of malnutrition, and prevalence of lost pregnancies among the drought-ravaged population of Tete Province, Mozambique. Prehosp Disaster Med. January-February 2007;22(1):26–34. [DOI] [PubMed] [Google Scholar]
- 39.Mason JB, Bailes A, Mason KE, et al. AIDS, drought, and child malnutrition in southern Africa. Public Health Nutrition. 2005;8(6):551–563. doi: 10.1079/PHN2005726 [DOI] [PubMed] [Google Scholar]
- 40.Singh MB, Lakshminarayana J, Fotedar R, Anand PK. Childhood illnesses and malnutrition in under five children in drought affected desert area of western Rajasthan, India. J Commun Dis. March 2006;38(1):88–96. [PubMed] [Google Scholar]
- 41.Mahapatra A, Geddam JJ, Marai N, et al. Nutritional status of preschool children in the drought affected Kalahandi district of Orissa. Indian J Med Res. March 2000;111:90–4. [PubMed] [Google Scholar]
- 42.Mason JB, Chotard S, Bailes A, Mebrahtu S, Hailey P. Impact of drought and HIV on child nutrition in Eastern and Southern Africa. Food and nutrition bulletin. 2010;31(3 Suppl):S209–218. [DOI] [PubMed] [Google Scholar]
- 43.Mason JB, Bailes A, Mason KE, et al. AIDS, drought, and child malnutrition in southern Africa. Public Health Nutr. 2005:551–63. vol. 6. [DOI] [PubMed] [Google Scholar]
- 44.Mason JB, Chotard S, Bailes A, Mebrahtu S, Hailey P. Impact of drought and HIV on child nutrition in Eastern and Southern Africa. Food Nutr Bull. September 2010;31(3 Suppl):S209–18. [DOI] [PubMed] [Google Scholar]
- 45.Kirezci E, Young IR, Ranasinghe R, et al. Projections of global-scale extreme sea levels and resulting episodic coastal flooding over the 21st Century. Scientific reports. 2020;10(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kulp SA, Strauss BH. New elevation data triple estimates of global vulnerability to sea-level rise and coastal flooding. Nature communications. 2019;10(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.del Ninno C, Dorosh P, Smith L, Roy D. The 1998 Floods in Bangladesh Disaster Impacts, Household Coping Strategies, and Response. Research Report of the International Food Policy Research Institute. January/01 2001:1–114. [Google Scholar]
- 48.del Ninno C, Lundberg M. Treading water. The long-term impact of the 1998 flood on nutrition in Bangladesh. Econ Hum Biol. March 2005;3(1):67–96. doi: 10.1016/j.ehb.2004.12.002 [DOI] [PubMed] [Google Scholar]
- 49.Islam S, Mahanta TG, Sarma R, Hiranya S. Nutritional status of under 5 children belonging to tribal population living in riverine (Char) areas of Dibrugarh district, Assam. Indian journal of community medicine: official publication of Indian Association of Preventive & Social Medicine. 2014;39(3):169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Skoufias E, Vinha K. Climate variability and child height in rural Mexico. Econ Hum Biol. January 2012;10(1):54–73. doi: 10.1016/j.ehb.2011.06.001 [DOI] [PubMed] [Google Scholar]
- 51.Hagos S, Lunde T, Mariam DH, Woldehanna T, Lindtjorn B. Climate change, crop production and child under nutrition in Ethiopia; a longitudinal panel study. Article. Bmc Public Health. August 2014;14:9. 884. doi: 10.1186/1471-2458-14-884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grace K, Davenport F, Funk C, Lerner AM. Child malnutrition and climate in Sub-Saharan Africa: An analysis of recent trends in Kenya. Applied Geography. 2012;35(1-2):405–413. doi: 10.1016/j.apgeog.2012.06.017 [DOI] [Google Scholar]
- 53.Jankowska MM, Lopez-Carr D, Funk C, Husak GJ, Chafe ZA. Climate change and human health: Spatial modeling of water availability, malnutrition, and livelihoods in Mali, Africa. Applied Geography. 2012;33(1):4–15. doi: 10.1016/j.apgeog.2011.08.009 [DOI] [Google Scholar]
- 54.Johnson K, Brown ME. Environmental risk factors and child nutritional status and survival in a context of climate variability and change. Article. Applied Geography. October 2014;54:209–221. doi: 10.1016/j.apgeog.2014.08.007 [DOI] [Google Scholar]
- 55.Soliman AT, De Sanctis V, Kalra S. Anemia and growth. Indian Journal of Endocrinology and Metabolism. 2014;18(Suppl 1):S1–S5. doi: 10.4103/2230-8210.145038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Singh MB, Fotedar R, Lakshminarayana J, Anand PK. Studies on the nutritional status of children aged 0-5 years in a drought-affected desert area of western Rajasthan, India. Public Health Nutrition. 2006;9(8):961–967. doi: 10.1017/PHN2006993 [DOI] [PubMed] [Google Scholar]
- 57.Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. Journal of Occupational and Environmental Medicine. 2009;51(1):33–37. [DOI] [PubMed] [Google Scholar]
- 58.McCarthy JJ. Climate change 2001: impacts, adaptation, and vulnerability: contribution of Working Group II to the third assessment report of the Intergovernmental Panel on Climate Change. Cambridge University Press; 2001. [Google Scholar]
- 59.Kuku O, Gundersen C, Garasky S. Differences in food insecurity between adults and children in Zimbabwe. Food Policy. 2011;36(2):311–317. [Google Scholar]
- 60.Hadley C, Lindstrom D, Tessema F, Belachew T. Gender bias in the food insecurity experience of Ethiopian adolescents. Social science & medicine. 2008;66(2):427–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fernandez A, Black J, Jones M, et al. Flooding and mental health: a systematic mapping review. PLoS One. 2015;10(4):e0119929. doi: 10.1371/journal.pone.0119929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Organization WH Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s. World Health Organization; 2014. [Google Scholar]


