Abstract
Introduction
cutaneous adenoid cystic carcinoma is a rare epithelial tumor with slow development, it is most often described in the scalp; palpebral involvement is very rare. And is accompanied by local aggressiveness and frequent recurrence. The aim of this work is to discuss the management and the interest of a close surveillance of adenoid cystic carcinoma.
Case presentation
The authors report a case of palpebral cystic adenoid carcinoma in a 65-year-old patient who underwent surgical excision followed by reconstruction of the loss of substance.
Discussion
Cutaneous cystic adenoid carcinoma of the eyelids remains a very rare entity that must be evoked in front of a nodular cutaneous palpebral tumor that progresses slowly. An early diagnosis and a complete excision guarantee a better prognosis.
Conclusion
Adenoid cystic carcinoma, because of its local aggressiveness and its capacity to recur despite satisfactory surgical removal, requires long-term surveillance. Its surgery may be responsible for functional and aesthetic sequelae.
Keywords: Adenoid cystic carcinoma, Eyelids, Perineural invasion, Surgery, Case report
Highlights
-
-
Cutaneous cystic adenoid carcinoma of the eyelids is a very rare entity that must be evoked in front of a nodular cutaneous tumor of the eyelids that progresses slowly.
-
-
It is characterized by a local aggressiveness with a high capacity of recurrence and the absence of a standardized protocol complicates its management.
-
-
The aim of this work is to discuss the management and the interest of a close surveillance of adenoid cystic carcinoma.
1. Introduction
Adenoid cystic carcinoma (ACC) is a malignant tumor that most commonly arises from the accessory salivary glands, less frequently from the lacrimal glands, breasts, cervix, and external auditory canal. Its cutaneous localization is rare and more described in middle-aged adults, on the head and neck [1]. The palpebral localization is even rarer and is accompanied by a high potential for local recurrence and metastasis, which are mostly regional [2], the differential diagnosis is clinically with chalazion, and histologically with basal cell carcinoma [3].
The treatment of choice for this entity is surgery with healthy excisional margins followed by prolonged surveillance. Chemotherapy and radiotherapy remain the recommended treatment options in cases where total excision is not possible [4].
We report the case of a surgically treated primary cystic adenoid carcinoma of the right lower eyelid. The aim of this work is to discuss the management and the interest of a close surveillance of adenoid cystic carcinoma.
This work has been reported in line with the SCARE 2020 criteria [5].
2. Case report
A 65-year-old patient with no particular history who consulted a private ophthalmologist for the management of a lower palpebral tumor that developed progressively over a period of 5 years. The patient complained of functional discomfort during palpebral opening and closing as well as aesthetic discomfort that motivated his consultation.
The patient was referred to our department of maxillofacial surgery at the university hospital for further treatment.
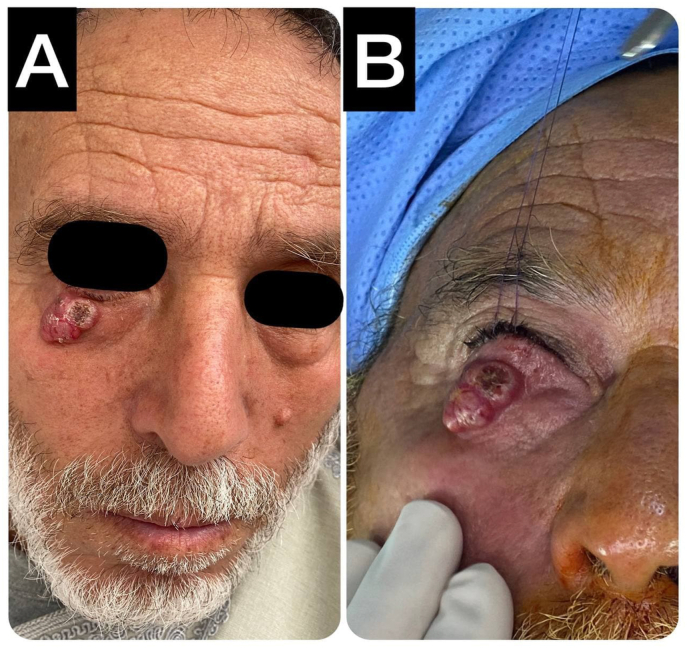
The clinical examination at the consultation showed a sessile lesion located on the lateral half of the right lower eyelid, respecting its free edge, purplish in color, measuring almost 15 mm in length, with a roughly polycyclic outline and a keratotic area, with some telangiectasias in places. The ganglionic areas were free (Fig. 1), ophthalmological examination of visual acuity, pupils, motility and intraocular pressures were normal.
Fig. 1.
Lower palpebral cystic adenoid carcinoma.
A facial CT scan was performed, which did not reveal any bone lysis or intra-orbital extension.
The histological examination of the biopsy performed on the same day of her consultation showed a tumor proliferation of cribriform architecture with small rounded and regular cavities containing mucoid cylinders with monomorphic rounded and basophilic nuclei suggestive of a cystic adenoid carcinoma.
The primary character of the tumor was retained in the absence of any other suspicious lesion (facial and cervico-thoracic CT).
The patient's case was discussed during a multidisciplinary staff with ophthalmologists and resuscitators, the decision of surgical removal under general anaesthesia was recommended, the patient expressed his concern about the aesthetic result in post-op when he was told of the decision.
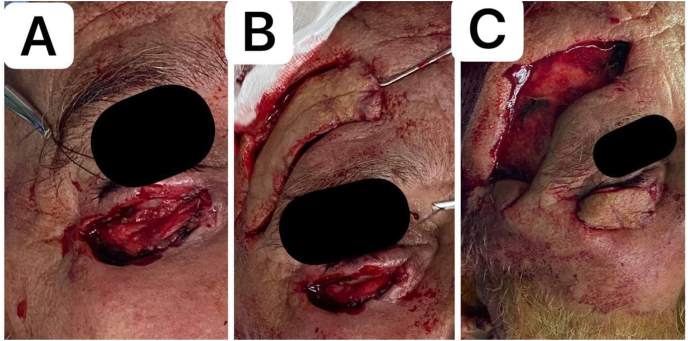
5 days later, the patient was operated on by the head of the department (15 years of experience) where he benefited from a tumor removal with 5 mm margins respecting the free edge, this resulted in a 25 mm loss of palpebral substance which was reconstructed by a supra-brow locoregional flap (Fig. 2).
Fig. 2.
The steps of reconstruction of the loss of substance.
The patient was seen at D1 or D2 (Fig. 3) and then every other day until 2 weeks, the wound was clean, no ectropion, the removal of thread at D6, the flap was warm and there were no signs of suffering, the patient was very satisfied with the result and in good mood.
Fig. 3.
Postoperative aspect after tumor removal and reconstruction of the substance loss by a supra-brow flap.
Long-term continuous monitoring of the patient is envisaged.
3. Discussion
Adenoid cystic carcinoma (ACC) is a rare malignant epithelial tumor representing 1–2% of all head and neck tumors and 10–15% of malignant salivary gland tumors [2]. The cutaneous involvement of this tumor is extremely rare and is most often described at the level of the scalp. Palpebral localization remains exceptional; at this level, it develops from the Moll's glands, the palpebral lobe of the lacrimal gland, the accessory lacrimal glands of the conjunctiva, or from an ectopic lacrimal glandular tissue [6].
The cutaneous involvement can be either primary (the case of our patient) or secondary by direct infiltration or following a peri-nervous extension or a cutaneous metastasis of a CAK [7].
The clinician must know how to eliminate a primary salivary KAC, hence the interest in performing a cervico-facial CT scan. The search for other locations justifies the performance of a thoraco-abdominal CT scan [8,9].
These tumors are clinically manifested by a firm nodular lesion without pain associated with loss or distortion of the cilia in middle-aged patients [10]. It may resemble basal cell carcinoma, palpebral sebaceous carcinoma or even a Chalazion-like lesion [6,11,12]. The majority of the cases of cutaneous CAK described in the literature were treated as Chalazion, the diagnosis was rectified by histological study of the specimen after excision or following lesion recurrences [11].
Its histological appearance is similar to that of other localizations [13]. It is composed of basophilic cells of cribriform, tubular or solid architecture occupying the mid to reticular dermis without any connection with the epidermis or hair follicles, the characteristic cystic spaces are filled by a hyaline substance discreetly eosinophilic, or by basophilic mucin.
The main differential diagnosis of cutaneous CAK is basal cell carcinoma [6,7,9,12]. Immunohistochemistry techniques allow to refine the diagnosis [13].
Peri-nervous invasion is found in more than 50% of primary ccam, it is the most frequent mode of dissemination and increases the rate of local recurrence after excision [9], hence the interest of the histological study of the excisional specimen in order to demonstrate a possible peri-nervous invasion [2].
Regional lymph node involvement is described but is not very frequent and distant metastases are very rare and occur late, mainly in the lung [9,11].
The treatment of choice for palpebral CAKc is carcinological surgical excision, some authors justify the use of micrographic surgery according to Mohs for the detection of peri-nerve invasion and therefore the reduction of the recurrence rate but there are no comparative studies of recurrence rates in patients treated by this method and those treated by the standard excision method [9,14].
Adjuvant radiotherapy reduces the risk of local recurrence and is indicated especially in the presence of peri-nerve invasion; chemotherapy can be administered in metastatic cases [1,7,14,15].
Despite its low metastatic potential, patients with cACC should be followed up for a long time because of its aggressive local potential and frequent recurrences that can occur late, up to 35 years after surgery [[9 ], [10], [11],16].
4. Conclusion
Cutaneous cystic adenoid carcinoma of the eyelids remains a very rare entity that must be evoked in front of a nodular cutaneous tumor of the eyelids that progresses slowly. It is characterized by a local aggressiveness and its capacity of recurrence in spite of a satisfactory surgical excision. Early diagnosis and complete excision are associated with a better prognosis. Nevertheless, long-term monitoring is necessary.
Sources of funding
The authors declared that this study has received no financial support.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Iro SALISSOU: Corresponding author writing the paper.
Raiteb MOHAMED: writing the paper.
MAADANE Amina: writing the paper.
ELMRINI SANAA: writing the paper.
Faiçal Slimani: Correction of the paper.
Trial registry number
-
1.
Name of the registry: researchregistry
-
2.
Unique Identifying number or registration ID:
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
The Guarantor is the one or more people who accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Declaration of competing interest
Authors of this article have no conflict or competing interests. All of the authors approved the final version of the manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102467.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Ramakrishnan R. vol. 37. 2013. pp. 1603–1611. (Primary Cutaneous Adenoid Cystic Carcinoma A Clinicopathologic and Immunohistochemical Study of 27 Cases). 10. [DOI] [PubMed] [Google Scholar]
- 2.Report C. vol. 29. 2013. pp. 143–146. (Multidisciplinary Management of Primary Adenoid Cystic Carcinoma of the Eyelid with Perineural Invasion). 6. [DOI] [PubMed] [Google Scholar]
- 3.Cecinio C. Ronquillo et Al reportAdenoid Cystic Carcinoma of the Eyelid Can Locally Recur and Mimic Basal Cell Carcinoma: Case Report and Review of the Literature . [DOI] [PubMed]
- 4.Feasel A.M., Brown T.J., Bogle M.A., Tschen J.A., Nelson B.R. Perineural invasion of cutaneous malignancies. Dermatol. Surg. 2001;27(6):531–542. doi: 10.1046/j.1524-4725.2001.00330.x. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Marback E.F., Costa A.L., Nossa L.M.B., Marback R.L. vol. 1. C; 2003. pp. 118–125. (Eyelid Skin Adenoid Cystic). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng C.H., Liao Y.L., Hong H.S. Cutaneous metastasis from adenoid cystic carcinoma of the parotid gland. Dermatol. Surg. 2003;1:775–779. doi: 10.1046/j.1524-4725.2003.29196.x. [DOI] [PubMed] [Google Scholar]
- 8.Barnes J., Garcia C. vol. 81. March; 2008. pp. 243–246. (“Primary Cutaneous Adenoid Cystic Carcinoma : A Case Report and Review of the Literature). [PubMed] [Google Scholar]
- 9.Tumor C., Micrographic M. 2009. Adenoid Cystic Carcinoma of the Eyelid : A Rare; pp. 997–1000. [DOI] [PubMed] [Google Scholar]
- 10.Cavazza S., Luca G., Laura L., Collina G. 2012. Primary Cutaneous Adenoid Cystic Carcinoma of the Upper Lid : a Case Report and Literature Review; pp. 31–35. [DOI] [PubMed] [Google Scholar]
- 11.Report C. vol. 78. 2015. pp. 323–325. (Primary Cutaneous Adenoid Cystic Carcinoma of the Eyelid and Literature Review). 5. [DOI] [PubMed] [Google Scholar]
- 12.Ellis N., Mamalis N. vol. 36. 2020. pp. 113–116. (Adenoid Cystic Carcinoma of the Eyelid Can Locally Recur and Mimic Basal Cell Carcinoma: Case Report and Review of the Literature). 5. [DOI] [PubMed] [Google Scholar]
- 13.Alkan B.I., Bozdogan O., Karadeniz M., Bozdoğan N. vol. 2017. 2017. (Case Report Two Different Cell Populations Is an Important Clue for Diagnosis of Primary Cutaneous Adenoid Cystic Carcinoma : Immunohistochemical Study). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang S., Ahn S., Choi J., Sung K. 1999. Primary Adenoid Cystic Carcinoma of Skin with Lung Metastasis; pp. 640–642. [DOI] [PubMed] [Google Scholar]
- 15.Naylor E., Sarkar P., Perlis C.S., Giri D. 2008. Primary Cutaneous Adenoid Cystic Carcinoma; pp. 636–641. [DOI] [PubMed] [Google Scholar]
- 16.Report C. Vol. 28. 2012. pp. 2011–2012. (Primary Adenoid Cystic Carcinoma). 2. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.