Abstract
Individuals who abuse alcohol often show exaggerated attentional bias (AB) towards alcohol-related cues, which is thought to reflect reward conditioning processes. Rodent studies indicate that dopaminergic pathways play a key role in conditioned responses to reward- and alcohol-associated cues. However, investigation of the dopaminergic circuitry mediating this process in humans remains limited. We hypothesized that depletion of central dopamine levels in adult alcohol drinkers would attenuate AB and that these effects would be mediated by altered function in frontolimbic circuitry. Thirty-four male participants (22–38 years, including both social and heavy drinkers) underwent a two-session, placebo-controlled, double-blind dopamine precursor depletion procedure. At each visit, participants consumed either a balanced amino acid (control) beverage or an amino acid beverage lacking dopamine precursors (order counterbalanced), underwent resting-state fMRI, and completed behavioral testing on three AB tasks: an alcohol dot-probe task, an alcohol attentional blink task, and a task measuring AB to a reward-conditioned cue. Dopamine depletion significantly diminished AB in each behavioral task, with larger effects among subjects reporting higher levels of binge drinking. The depletion procedure significantly decreased resting-state functional connectivity among ventral tegmental area, striatum, amygdala, and prefrontal regions. Beverage-related AB decreases were mediated by decreases in functional connectivity between the fronto-insular cortex and striatum and, for alcohol AB only, between anterior cingulate cortex and amygdala. The results support a substantial role for dopamine in AB, and suggest specific dopamine-modulated functional connections between frontal, limbic, striatal, and brainstem regions mediate general reward AB versus alcohol AB.
Subject terms: Cognitive control, Brain, Human behaviour, Reward
Introduction
Attentional bias (AB) towards alcohol-related stimuli predicts alcohol craving [1], relapse risk [2–4], and future alcohol drinking [5]. Although the latter clinical predictive relationships are inconsistent [6], AB does appear to measure an underlying addiction state or trait. One such trait that is closely related to AB is a susceptibility to reward conditioning [7]. The development of AB to addiction-related cues is thought to reflect Pavlovian learning, such that drug reward-predicting cues eventually acquire the capacity to initiate drug seeking and use [8, 9]. Indeed, AB is greater among heavier drinkers [10]. AB to non-drug rewards is also heightened in the context of addiction, suggesting that substance misuse more generally associates with sensitivity to reward conditioning [11, 12]. However, whether alcohol-related AB relies on the same brain circuits as non-drug reward conditioning and AB is uncertain.
Human neuroimaging studies have begun to examine the neural correlates of alcohol AB. Testing individuals recovering from alcohol use disorder (AUD) on a dot-probe task, researchers identified positive correlations between alcohol AB and activations in the inferior frontal gyrus (IFG), anterior cingulate cortex (ACC), anterior insula, and striatum [13]. Individuals with AUD also displayed heightened nucleus accumbens (NAc) and medial prefrontal cortex activation during an implicit alcohol approach bias task [14]. Evidence from an alcohol word Stroop task indicates prefrontal hypoactivation associated with alcohol AB in AUD [15]. These prior studies highlight a role for frontal and limbic brain regions in AB to addiction-related cues. However, human fMRI studies of addiction AB have not yet identified the functional neurocircuitry mediating this behavior.
Given the limitations of current non-invasive human neuroimaging methods, rodent studies have been instrumental in probing the neural circuits of behavior. While AB is difficult to model in rodents, much is known about Pavlovian conditioned responses to reward-predictive cues. For example, mesolimbic dopamine projections from the ventral tegmental area (VTA) to the NAc play a critical role in both Pavlovian conditioning and the expression of conditioned responses [16, 17]. In addition, fast dopamine release events (dopamine transients) commence at the onset of a conditioned cue [18, 19]. Pavlovian conditioned responses to alcohol cues in rodents provide a model of alcohol AB that allows direct measurements and mechanistic manipulations of the neural circuitry underlying AB [20–22]. Taken together, preclinical evidence indicates a key role for dopaminergic pathways in mediating responses to alcohol-related cues [23–25]. Moreover, work in non-human primates highlights a role for the prefrontal cortex in reward signaling [26], and human fMRI studies show that prefrontal cortex drives phasic cue responses in the VTA [27, 28]. However, the dopaminergic circuitry mediating AB to alcohol cues in humans––and the extent to which this circuitry overlaps with the circuitry mediating conditioned responses to non-drug rewards––remains unclear.
The goal of the current study was to map the dopaminergic functional circuitry underlying alcohol AB in human subjects. To do so, we transiently reduced dopamine in human subjects by administering an amino acid beverage deficient in the dopamine precursors phenylalanine and tyrosine (P/T) [29, 30] prior to resting-state fMRI and testing on three AB tasks. In event-related fMRI procedures, dopamine depletion decreases reward-related brain activation [31–33] and reduces AB to smoking cues [34]. Thus, we hypothesized that acutely lowering dopamine via P/T depletion would reduce AB to both alcohol cues and non-drug, reward-conditioned cues and would do so in proportion to changes in the functional connectivity (FC) between prefrontal and subcortical brain regions. Furthermore, we predicted greater reductions in AB among subjects reporting heavier alcohol use. Because adolescent and recent alcohol use differentially impact the mesolimbic dopaminergic system [25, 35–38], we tested for both effects on AB. As behaviors modulated by PFC dopamine show ovarian cycle-dependent variance in females [39–46], here we tested adult males (n = 34) in two separate sessions: a P/T depletion session and a control session, in a double-blind, counter-balanced design.
Methods
Participants
Thirty-four healthy male participants (ages 22–38 years; mean = 26.3) were recruited from the University of North Carolina, Chapel Hill (UNC) campus and surrounding communities. Although our statistical tests utilized continuous measures of alcohol use, to ensure a broad distribution of alcohol use, we recruited participants into two groups that were guided by the National Institute on Alcohol Abuse and Alcoholism’s (NIAAA) definitions for moderate drinking and binge drinking [47]. The moderate, social drinking group (n = 15) self-reported <14 alcoholic drinks/week, <10 lifetime binge episodes, and no binge episodes in the past 12 months. The frequent binge drinking group (n = 15) self-reported ≥14 alcoholic drinks/week and ≥12 binge episodes (≥5 drinks/2 h) in the past 12 months. Participants had no current or past neurological or psychiatric diagnoses, no contraindications for MRI or the amino acid depletion manipulation. Additional exclusion criteria were current psychoactive drug use (including medications), history of treatment for a substance use disorder, or lifetime substance use disorder based on a structured clinical interview using DSM-IV criteria [48]. One participant reported light, non-dependent vaping. No participants reported any lifetime regular use of psychoactive medications (see Supplementary Materials). For individuals enrolled as heavy drinkers, current or past AUD was not exclusionary. All participants were native English speakers, right-handed, and had at least a high school education (or equivalent). Negative breathalyzer tests (FC-10, Lifeloc Inc., Wheat Ridge, CO) and urine drug screens for cocaine, THC, amphetamines, methamphetamine, and opiates (Biotechnostix, Inc., Markham, ON) were obtained at the beginning of each session; participants were instructed not to drink alcohol for 24 h before the session. Participants gave written, informed consent, as approved by the UNC Office of Human Research Ethics.
General procedure
We used a double-blinded, within-subjects, counter-balanced design consisting of two laboratory visits of ~8 h each; visits were separated by ≥72 h. The visits were identical and began with urine, alcohol, and health screening. Following screening, participants were given up to 30 min to consume the amino acid-containing beverage (see “Dopamine Depletion Procedure”). Following beverage consumption, participants completed questionnaires (see “Alcohol Use Inventories” and Supplementary Materials) and relaxed in the lab; 4–5 h after beverage consumption, they underwent a resting-state fMRI scan, then completed computerized behavioral tasks outside the scanner (see “Behavioral Tasks”). Participants were dismissed after being offered a high protein snack and were compensated for participation after completing the second visit.
Dopamine depletion procedure
The P/T depletion method has been safely used for many years, and its effects on brain dopamine levels are well established [49, 50]. As in our previous studies [29, 30], prior to each test session, subjects followed a low protein (<20 g) diet for 24 h and fasted from midnight until session onset (~8 A.M.). After participants provided a written account of their diet in the previous 24 h, they consumed either a control amino acid beverage or one deficient in the dopamine precursors, phenylalanine (P), and tyrosine (T) (see Supplementary Materials), to initiate the acute dopamine depletion process [51]. Under typical brain P/T concentrations, T is the preferred substrate for tyrosine hydroxylase, the rate-limiting enzyme in dopamine synthesis, but T-depletion without P-depletion is not sufficient to reduce brain dopamine [52]. Amino acid beverages lacking P and T decrease brain P/T concentrations [53–55] after 4–5 h [50]. Although brain norepinephrine synthesis is also reduced by P/T depletion [56] the dopamine system seems to be disproportionately affected [57], a distinct advantage of this method over administering the tyrosine hydroxylase inhibitor α-methyl-para-tyrosine (AMPT) [58], which also requires multiple doses and can cause motor and urinary side effects [59] and is generally used in an in-patient setting.
Alcohol use inventories
We quantified current alcohol use with the Alcohol Use Questionnaire [AUQ; 60] from which we calculated a “binge drinking score” [60]. This score was log transformed to provide a Gaussian distribution suitable for parametric statistics. The Carolina Alcohol Use Patterns Questionnaire (CAUPQ [61]) was used to estimate a total number of adolescent (0–21 years) binge episodes (see Supplementary Materials) and quarter-root transformed before statistical analysis.
Resting-state fMRI
We acquired resting-state fMRI data as 243 blood oxygenation level-dependent (BOLD) images on a Siemens 3 T Prisma scanner equipped with a 32-channel TEM send–receive radio frequency (RF) head coil (Siemens Healthineers, Erlangen, Germany), using a 1-shot gradient-echo EPI pulse sequence (TR = 2 s, TE = 25 ms, flip angle = 50°, 35 slices tilted at 30° from horizontal plane; FoV = 192 × 192 mm; voxel size = 3 × 3 × 4 mm with a 0.5 mm inter-slice gap). The fMRI acquisition was preceded by 11 s of dummy gradient RF pulses to achieve steady-state tissue magnetization. We also acquired a low-resolution T1-weighted co-planar image and a high-resolution magnetization-prepared rapid gradient-echo (MPRAGE) T1-weighted image (see Supplementary Materials). Participants were directed to stay awake, look at the fixation crosshair on a screen, and “let their minds wander” without focusing on particular thoughts.
Behavioral tasks
Dot-probe task
We assessed selective attention capture using a dot-probe task modified from our previous studies assessing AB toward smoking cues in cigarette smokers [62, 63] (See Supplementary Materials). Faster response times (RT) in trials in which the target was congruent with the alcohol image versus the neutral image indicates AB toward alcohol-related cues via selective attention capture.
Modified attentional blink task
To measure extended attention hold, participants completed a modified attentional blink task based on the emotional blink of attention paradigm [64–68] (See Supplementary Materials for details). Trials contained a rapid serial presentation of upright landscape or house images [69, 70], except for two images: the critical distractor (either neutral or alcohol-related images) and the target stimulus. Targets were house photos rotated 90° left or right and occurred 2 or 8 images after the distractors. Participants indicated the target orientation by button press. Reduced lag 2 accuracy relative to lag 8 accuracy indicates a greater attentional blink, and a greater blink following an alcohol distractor relative to neutral distractor is interpreted as greater AB to alcohol cues.
Reward task
We assessed reward conditioning sensitivity using a value-driven attention capture task identical to one described elsewhere [11] (Supplementary Materials). Briefly, participants were first trained to implicitly associate the colors red and green with a high or low reward (counterbalanced across subjects). In a separate test of reward conditioning, participants were instructed to ignore colors. However, 50% of trials included non-target red or green stimuli, representing conditioned distractors. Prolonged RTs in trials containing a distractor stimulus previously associated with reward indicates AB to reward-conditioned cues.
Behavioral analyses
We assessed whether measures of current or adolescent binge drinking moderated effects of dopamine depletion on AB using repeated-measures linear mixed models with PROC MIXED in SAS 9.4. We opted to use linear mixed models (LMM) rather than repeated-measures (RM) analysis of variance (ANOVA) here, as linear mixed models are better suited to handle missing data, among other advantages over RM-ANOVA [71]. All models included beverage order, as well as both current binge score and adolescent binge drinking as independent variables. Based on the hypothesis that heavier drinking would be associated with greater effects of dopamine depletion on AB, we specifically tested for interacting effects of beverage type and task parameters with binge drinking (independently for both current and adolescent) on performance in each task.
For the dot-probe task, the dependent measure was RT from correct trials. AB is measured by effects of cue type (neutral or alcohol). We excluded trials in which the RT was >2 standard deviations above the individual’s mean RT for that trial type or <200 ms. One participant was missing data from one session. In the LMM for this task we tested for significant interacting effects of both beverage type × cue type × current binge drinking, and beverage type × cue type × adolescent binge drinking.
For the attentional blink task, the dependent measure was the accuracy of target responses. AB is measured by the interaction of the lag (2 or 8) and distractor type (neutral or alcohol). Trials in which the RT was <200 ms were excluded. One participant was missing data from both sessions. In the LMM for this task we tested for significant interacting effects of both beverage type × cue type × lag × current binge drinking, and beverage type × cue type × lag × adolescent binge drinking.
For the reward task, the dependent measure was RT from correct responses during the test phase. To measure AB, a linear variable modeling the distractor trial type (high = 2, low = 1, no reward = 0) was created [72]. We excluded trials in which the RT was >3 standard deviations above the individual’s mean RT for that trial type or <200 ms. Thirteen participants only completed the task during their first session. In the LMM for this task we tested for significant interacting effects of both beverage type × distractor type × current binge drinking, and beverage type × distractor type × adolescent binge drinking.
We examined the behavioral evidence for overlapping mechanisms of alcohol and non-drug reward AB by conducting pairwise Spearman’s partial correlations among the three AB tasks, covarying for beverage effects. AB values were residual values from the linear regression analysis with the beverage effect added back; because this calculation provides a separate adjusted value for each trial type, a mean value was calculated to get a single AB score for each session.
Neuroimaging analyses
FMRI preprocessing included the following steps using Analysis of Functional Neuroimages (AFNI [73], version 19.3.07): slice time correction; realignment; co-registration to the low-resolution T1 image; MPRAGE segmentation; regression of nuisance time series corresponding to white matter, cerebrospinal fluid, and subject-specific realignment parameters; and normalization to a standard template in Montreal Neurological Institute (MNI) space. Images were resampled back into the original 2 mm3 voxel resolution and spatially smoothed with a 5 mm Gaussian kernel. A temporal filter of 0.008–0.1 Hz was applied. Data were “scrubbed” using a framewise displacement threshold of >0.3 mm, resulting in the removal of the flagged time point along with one preceding and two following [74]. Furthermore, two participants exhibiting an average framewise displacement of >0.2 mm for at least one session were omitted from FC analyses due to the likelihood of persistent motion artifacts [75].
Regions-of-interest analysis
An a priori-selected neural circuit of dopaminergic pathways predicted to underlie alcohol AB included the VTA, striatum, amygdala, and prefrontal cortical regions that are anatomically connected to the VTA and involved in motivated behaviors [76–81]. Mean time series were extracted from a priori regions of interests (ROI) selected from published research findings (Table 1). For each beverage condition, Pearson correlation values of the 11 ROI time series were calculated and Fisher-Z transformed. FC values were assessed for main effect of P/T depletion via general linear model covarying for beverage order, FC on placebo to account for individual differences in baseline FC/dopamine levels [29], and global FC of each of the two ROIs to account for motion induced FC effects [82]. Results were corrected for multiple comparisons using a false discovery rate correction (FDR, q = 0.05).
Table 1.
Regions of interest for functional connectivity analysis.
| Region of interest | MNI coordinates | Sources |
|---|---|---|
| Ventral tegmental area (VTA) | Probabilistic atlas | [120] |
| Dorsolateral prefrontal cortex (dlPFC) |
Left: −48, 18, 44 Right: 48, 18, 44 |
[121] |
| Anterior cingulate cortex (ACC) | −8,24,34 | [121] |
| Fronto-insular cortex (FIC) |
Left: −38, 24, −8 Right: 34, 24, −8 |
[121] |
| Inferior frontal gyrus pars opercularis (IFGop) | Structural atlas | Harvard–Oxford cortical and subcortical atlases [122] |
| Medial orbitofrontal cortex (medOFC) |
Left: −6, 37, −12 Right: 6, 37, −12 |
[123] |
| Amygdala (Amy) |
Left: −20, 6, 10 Right: 20, 6, −12 |
[123] |
| Lateral orbitofrontal cortex (latOFC) |
Left: −27, 39, −6 Right: 27, 39, −6 |
[123] |
| Limbic striatum (striatum L) | Probabilistic atlas | [124] |
| Executive striatum (striatum E) | Probabilistic atlas | [124] |
| Sensorimotor striatum (striatum S) | Probabilistic atlas | [124] |
Whole-brain VTA seed-based analysis
Because a priori ROI selection may miss potentially significant FC changes among regions not included in the analysis, we also conducted an exploratory seed-based FC analysis to examine whole-brain changes in VTA FC in a voxel-wise manner. Main effects of P/T depletion were tested via general linear model covarying for beverage order, FC on placebo [29], and global VTA FC [82]. Results were FDR corrected for multiple comparisons (q = 0.05).
Mediation Analyses
Mediation analyses using the Multilevel Mediation and Moderation (M3) Matlab Toolbox [83] identified functional connections that mediated the effects of P/T depletion on AB for each of the AB tasks. We limited mediation testing to those ROI–ROI connections for which the depletion effects survived a threshold of p < 0.05, uncorrected, since these connections were most likely to contribute to significant indirect effects. FC values (i.e., the mediators) in these analyses were residual values from the linear model described above (“Regions-of-Interest Analysis”). Likewise, AB values (i.e., the outcome variables) were also adjusted values identical to those used in the task behavioral correlation analysis (see “Behavioral Analyses”). Significance testing was performed with 100,000 bootstrap iterations and a 95% CI, one-tailed distribution. Due to multiple tests performed across 10 ROI–ROI connections and three tasks, results were FDR-corrected (q = 0.05). Only participants with complete FC and AB data for the given task were included for each analysis.
Results
Demographic and psychometric data
Drinking groups were similar in age, years of education, and familial alcoholism (Supplementary Table 2). Individuals recruited to the heavy drinking group reported higher rates of current and adolescent binge drinking, although these measures were only modestly correlated across groups (ρ = 0.36, p = 0.037)
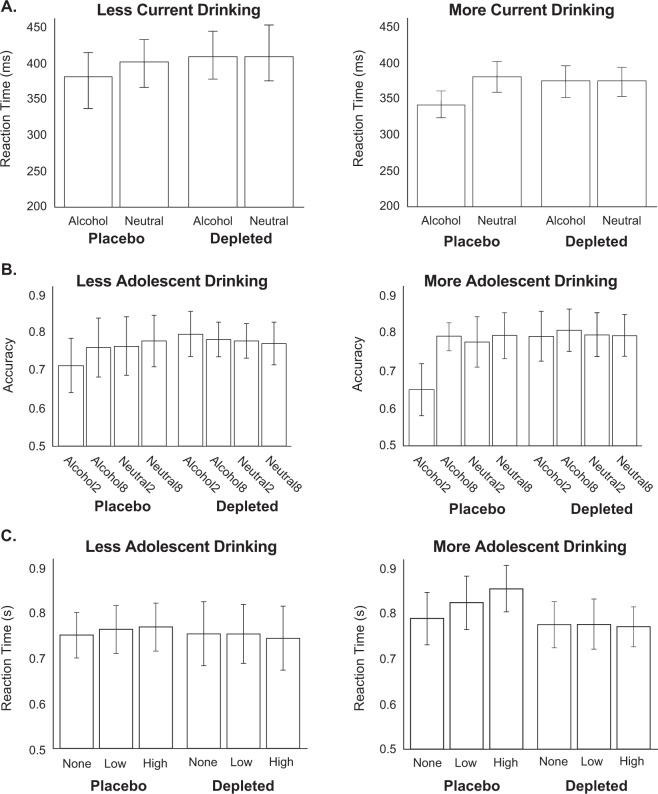
Effects of P/T depletion on AB measures
As detailed below, linear mixed models (LMMs) of performance in each behavioral task indicated that P/T depletion diminished AB to a greater extent among subjects reporting higher levels of binge drinking. For the dot-probe task, the LMM found significant interacting effects of beverage type, cue type, and current binge drinking on RT (t(30) = −2.28, p = 0.030; Fig. 1a); however, adolescent binge drinking did not significantly interact with beverage type and cue type (t(30) = 1.57, p = 0.12). In other words, current binge drinking significantly moderated the change in AB after P/T depletion. Specifically, the difference in RT between alcohol and neutral cues on placebo was greater for those reporting greater current binge drinking, but this AB effect was diminished by P/T depletion.
Fig. 1. Dopamine depletion attenuates attentional bias, dependent on binge drinking severity.
A For the dot-probe task, a linear mixed model indicated a significant beverage type × cue type × current binge drinking interaction effect on RT. B For the attentional blink task, a linear mixed model indicated a significant beverage type × cue type × lag × adolescent binge drinking interaction effect on accuracy. C For the reward task, a linear mixed model indicated a significant beverage type × distractor type × adolescent binge drinking interaction effect on RT. Least squares means are presented. For display purposes, binge drinking was binarized: “More Current Binge Drinking” corresponds to an Alcohol Use Questionnaire binge score of >10, whereas “More Adolescent Binge Drinking” corresponds with >9 estimated binge episodes by the age of 21.
For the attentional blink task, the LMM found significant interacting effects of beverage type, cue type, lag, and adolescent binge drinking on accuracy, indicating that adolescent binge drinking significantly moderated the change in AB after P/T depletion (t(30) = −2.52, p = 0.017; Fig. 1b). Specifically, adolescent binge drinking was associated with lower alcohol lag 2 accuracy, and this AB effect was rescued by P/T depletion. The LMM did not find a statistically significant interaction of current binge drinking with beverage type, cue type, and lag (t(30) = 1.35, p = 0.19).
For the reward task, the LMM found significant interacting effects of beverage type, distractor type, and adolescent binge drinking on RT, again finding that adolescent binge drinking significantly moderated the change in AB after P/T depletion (t(30) = 3.93, p < 0.001; Fig. 1c). The significant interaction reflected a larger non-drug reward AB on placebo among those reporting more frequent adolescent binge drinking, which was diminished following P/T depletion. Again, the corollary interaction term that instead included current binge drinking was not statistically significant (t(30) = −0.48, p = 0.63).
Covarying for P/T depletion effects, AB toward alcohol cues in the dot-probe task positively correlated with AB toward to alcohol cues in the blink task (ρ(58) = 0.34, p = 0.008) and with AB toward conditioned non-drug cues in the reward task (ρ(49) = 0.32, p = 0.023). Alcohol AB in the blink task also correlated with AB on the reward task (ρ(47) = 0.41, p = 0.003).
P/T depletion effects on frontolimbic FC
Using an ROI-to-ROI approach, we assessed beverage-related changes in pairwise FC (Fig. 2). Ten connections showed altered FC (p < 0.05; these 10 were included in mediation analyses), six of which survived an FDR correction. Nine of these connections demonstrated reduced FC with P/T depletion, whereas only one connection demonstrated greater FC.
Fig. 2. Region-of-interest analysis results.
Functional connectivity estimates (Fisher Z-transformed Pearson correlations) are displayed for the depleted (top) and control (middle) beverages and t-statistics are displayed for the contrast of depleted minus control (bottom). Bold text indicated p < 0.05uncorrected, whereas outlined cells indicate connections surviving an FDR correction. VTA ventral tegmental area, dlPFC dorsolateral prefrontal cortex, ACC anterior cingulate cortex, FIC fronto–insular cortex, IFGop inferior frontal gyrus pars opercularis, medOFC medial orbitofrontal cortex, latOFC lateral orbitofrontal cortex, Amy amygdala, striatum L limbic subdivision of the striatum, striatum E executive subdivision of the striatum, striatum S sensorimotor subdivision of the striatum.
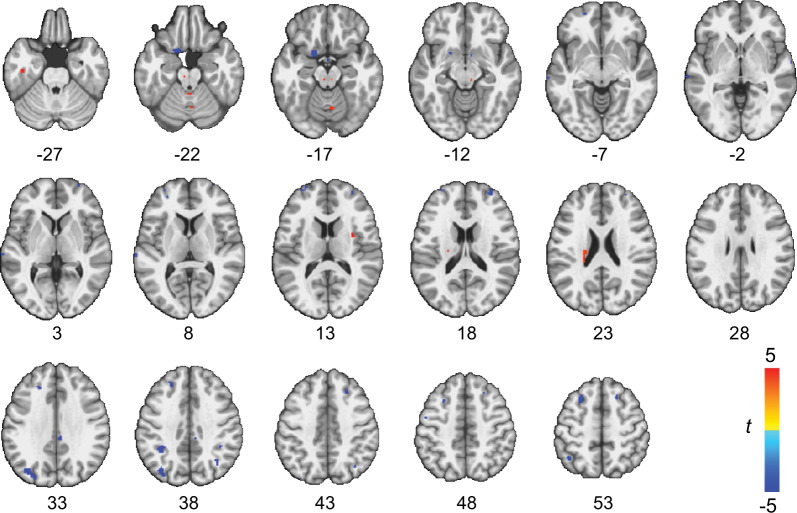
Dopamine depletion effects on VTA FC
As the VTA is a major nucleus of dopamine cell bodies, we explicitly assessed changes in connectivity with the VTA induced by depletion of dopamine precursors. In testing for voxels demonstrating significant changes in FC with the VTA following P/T depletion, we found decreased FC between the VTA and the OFC, NAc, intra-parietal sulcus and the superior frontal sulcus (Fig. 3; Supplementary Table 3), whereas increased FC was detected with the brainstem, temporal lobe, caudate tail, and cerebellum.
Fig. 3. Voxel-wise results of dopamine depletion effects on functional connectivity of the ventral tegmental area (VTA).
Warm colors indicate increased connectivity following dopamine depletion, whereas cool colors indicate decreased connectivity following dopamine depletion. Significant voxels after false discovery rate (FDR) correction are displayed.
Mediation Analyses
Several ROI–ROI connections mediated the effects of P/T depletion on AB. For the blink task, P/T-depletion effects on AB were mediated by FC changes between both fronto–insular cortex (FIC)–limbic striatum and ACC–amygdala (Fig. 4a). Although these same two connections also demonstrated mediating effects of P/T depletion on dot-probe AB (puncorrected < 0.05), the effects did not survive an FDR correction. Similar to the alcohol AB tasks, depletion effects on reward task AB were mediated by FIC–limbic striatum FC changes; reward task AB was additionally mediated by FC changes between the FIC and both executive and sensorimotor subdivisions of the striatum (Fig. 4b).
Fig. 4. Mediation analysis results.
Functional connectivity mediation of dopamine depletion effects on (A) attentional bias on the blink task and (B) attentional bias on the reward task. Significant indirect effects indicate the functional connection significantly mediated the effect of beverage type on attentional bias. c is the direct effect without the mediator, and c′ is the effect after entering the mediator.
Discussion
Here we quantified AB toward alcohol and non-drug, reward-conditioned cues and their neural underpinnings after acute dopamine precursor depletion across a broad spectrum of alcohol users. P/T depletion significantly reduced AB across three different tasks, particularly in individuals who reported heavier drinking. P/T depletion altered FC between prefrontal and subcortical brain regions involved in reward processing and motivation, and these alterations predicted changes in AB.
AB behavior following dopamine depletion
P/T depletion reduced AB to both alcohol and non-drug, reward-conditioned cues in this study. This reduction is consistent with the one prior study that tested the effects of P/T depletion on smoking AB [34]. Animal studies demonstrate that mesolimbic dopamine projections from the VTA to the NAc play a critical role in both Pavlovian conditioning and expression of conditioned responses, which are often conceptualized as a preclinical model of AB [16, 17]. Human neuroimaging work also indicates a role of dopamine release, specifically within the anterior caudate, in generalized reward conditioning [84]. In addition to conditioned responding, the AB tasks employed in the current study also require attentional processes such as alerting, and orientating to stimuli, and executive control function processes relying on dopamine [85]. Thus, the observed AB changes following P/T depletion reflect not only changes to dopamine transients [57] in response to conditioned cues [18, 19], but also changes to catecholamine systems involved in attention and cognitive control. While data suggest that P/T depletion affects dopamine more than norepinephrine [50, 58, 86, 87], changes to norepinephrine systems could contribute to the effects reported here.
The effects of P/T depletion on AB in this sample of light/moderate to heavy drinkers depended on binge drinking levels. Specifically, greater binge patterns of drinking during adolescence enhanced AB effects in the reward task and the blink task, whereas current binge drinking more strongly predicted AB effects in the dot-probe task. These findings were consistent with the enhanced AB present among heavier versus lighter drinkers [10], an association attenuated here by P/T depletion. Exposure to alcohol during adolescence is associated with persistent changes in brain function [88, 89]. Preclinical models of adolescent binge drinking demonstrate deleterious effects of alcohol exposure on neurogenesis [90] as well as on prefrontal function, leading to persistent changes in adult cognition [91–93]. Significant changes to reward neurocircuitry also occur during this period [94, 95]. Our findings of adolescent alcohol exposure moderating P/T depletion-related changes in AB, even when controlling for current drinking, is consistent with the harmful consequences of alcohol on the developing brain. However, it is also possible that effects of adolescent binge drinking on AB reflect premorbid cognitive differences between those who initiated alcohol use in adolescence and those who did not; notably, impulsive behavior in childhood predicts adolescent misuse of alcohol and other substances [96, 97], and impulsivity further predicts AB [72]. We also found that current binge drinking levels predicted AB on the dot-probe task, covarying for adolescent alcohol binges. In adult rodents, binge-like drinking exposure leads to deficits [98] in prefrontal functions including reversal learning [99, 100]. Taken together, these findings emphasize the importance of both past and current binge drinking on AB and provide insight into developmental and acute impacts of alcohol on the dopamine system.
Beverage effects on FC
Although two previous studies reported changes in intrinsic FC associated with dopamine precursor depletion [101, 102], this is the first to link such changes to attentional control, as well as the first to show moderating effects of binge drinking history. This procedure mostly reduced FC between prefrontal (i.e., FIC, MFG) and subcortical (i.e., striatum, amygdala, VTA) brain regions. An increase in FC between ACC and FIC, two core regions of the “salience network” [103], was a notable exception. A seed-based approach enabled a whole-brain examination of VTA FC changes that was not restricted to a priori ROIs. This analysis revealed diminished VTA FC with both reward-related regions (e.g., OFC and NAc) as well as regions involved in visual attention (e.g., intra-parietal sulcus). These findings support the recent suggestion that dopamine may stabilize signaling within networks engaged when orienting attention towards behaviorally relevant stimuli [101].
FC mediation of AB
The consistent mediation of AB by FIC–limbic striatum across all three tasks (although not significant after FDR correction for the dot-probe task) indicates a general mechanism of processing reward-predicting cues, which may represent a trait marker of susceptibility to reward conditioning. The limbic striatum ROI is primarily centered in the NAc. Indeed, preclinical work emphasizes the role of NAc in stimulus-reward learning [17, 104], which extends to drug-related cues [22, 105–107]. This coherent FC relationship across AB tasks is also consistent with the significant correlations between behavioral measures of AB. Conversely, ACC–amygdala FC only mediated alcohol-related AB. Interactions between these two brain regions modulate responses to emotional stimuli [108–110] and may also underlie motivation for rewards [111]. The unique association of this connection with alcohol AB, but not generalized reward AB, suggests that alcohol cues become imbued with distinct emotional and motivational qualities beyond their ability to predict reward.
It is noteworthy that the ACC and FIC––the prefrontal brain regions for which increased FC following P/T depletion mediated AB in this study––are major hubs of the salience network that is involved in conditioning and assigning incentive salience to drugs and drug-related cues [112]. The FIC specifically facilitates access to attention and working memory resources when a salient event is detected and regulates reactivity to salient stimuli [113, 114]. Our findings support prior work indicating the importance of dopaminergic signaling in salience network FC [101, 115], and supporting a potentially key role for this functional network in AB [116].
Strengths and limitations
The within-subjects, repeated-measures study design afforded power to detect significant effects of dopamine depletion despite an otherwise modest sample size (34 individuals). A study limitation is that, although our results indicated P/T depletion effects on the brain and behavior, we did not directly measure dopamine or dopamine metabolite levels. Individual differences, such as baseline dopamine levels, sex, state factors, and genetic factors may play a role in the depletion effects as seen in previous studies [29, 117]. Our conclusions would have been strengthened by including plasma measurements of amino acids to confirm the effectiveness of the P/T depletion procedure. In addition, this study only included males due to sex differences in the dopamine system [118, 119]. Finally, preclinical studies demonstrate phasic dopamine release in response to conditioned reinforcers [23, 36], and P/T depletion suppresses spontaneous dopamine transients in the NAc of rats at rest [57]. However, in this study, the behavioral tasks were performed after the resting-state scan; future work pairing event-related fMRI AB tasks with the P/T depletion procedure may provide additional insight into the dopamine response to alcohol or non-drug reward cues.
Conclusions
Our findings are the first to identify the dopamine-related functional connections underlying alcohol-related AB in humans. The results point to a significant role of dopamine for both alcohol and non-drug reward AB and indicate that specific dopamine-dependent functional connections between frontal, limbic, striatal, and brainstem regions mediate these behaviors.
Funding and disclosure
This work was funded by NIH award grant number P60AA011605 to CAB and DLR, NIH grant numbers T32DA007244 and F31AA023720 to MLF, and NIH grant numbers T32AA007573 and K01AA026334 to AE. The authors declare no competing financial interests.
Supplementary information
Acknowledgements
We thank M. Powell, A. Sapp, L. Harvey, A. Paulson, and C. Fare for assistance with data collection, and T. McKim, J. Hopfinger, M. Sheridan, and T. Thiele for valuable comments and discussion.
Author contributions
These authors contributed equally: Monica L. Faulkner, Amanda Elton. CAB, DLR and MLF designed the research. MLF performed the research. MLF and AE analyzed the data. All authors made a substantial contribution to interpretation of the data and drafting of the manuscript.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Amanda Elton, Monica L. Faulkner
Supplementary information
The online version contains supplementary material available at 10.1038/s41386-021-00993-9.
References
- 1.Field M, Mogg K, Bradley BP. Craving and cognitive biases for alcohol cues in social drinkers. Alcohol Alcohol. 2005;40:504–10. doi: 10.1093/alcalc/agh213. [DOI] [PubMed] [Google Scholar]
- 2.Cox WM, Hogan LM, Kristian MR, Race JH. Alcohol attentional bias as a predictor of alcohol abusers’ treatment outcome. Drug alcohol Depend. 2002;68:237–43. doi: 10.1016/s0376-8716(02)00219-3. [DOI] [PubMed] [Google Scholar]
- 3.Waters AJ, Shiffman S, Sayette MA, Paty JA, Gwaltney CJ, Balabanis MH. Attentional bias predicts outcome in smoking cessation. Health Psychol. 2003;22:378–87. doi: 10.1037/0278-6133.22.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marissen MA, Franken IH, Waters AJ, Blanken P, van den Brink W, Hendriks VM. Attentional bias predicts heroin relapse following treatment. Addiction (Abingdon, Engl) 2006;101:1306–12. doi: 10.1111/j.1360-0443.2006.01498.x. [DOI] [PubMed] [Google Scholar]
- 5.Field M, Eastwood B. Experimental manipulation of attentional bias increases the motivation to drink alcohol. Psychopharmacology. 2005;183:350–7. doi: 10.1007/s00213-005-0202-5. [DOI] [PubMed] [Google Scholar]
- 6.Field M, Marhe R, Franken IH. The clinical relevance of attentional bias in substance use disorders. CNS Spectr. 2014;19:225–30. doi: 10.1017/S1092852913000321. [DOI] [PubMed] [Google Scholar]
- 7.Anderson BA. What is abnormal about addiction-related attentional biases? Drug alcohol Depend. 2016;167:8–14. doi: 10.1016/j.drugalcdep.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychological Rev. 1990;97:147–68. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- 9.Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Brain Res Rev. 1993;18:247–91. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- 10.Jones BT, Bruce G, Livingstone S, Reed E. Alcohol-related attentional bias in problem drinkers with the flicker change blindness paradigm. Psychol Addict Behav. 2006;20:171–7. doi: 10.1037/0893-164X.20.2.171. [DOI] [PubMed] [Google Scholar]
- 11.Anderson BA, Faulkner ML, Rilee JJ, Yantis S, Marvel CL. Attentional bias for nondrug reward is magnified in addiction. Exp Clin Psychopharmacol. 2013;21:499–506. doi: 10.1037/a0034575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bjork JM, Smith AR, Chen G, Hommer DW. Mesolimbic recruitment by nondrug rewards in detoxified alcoholics: effort anticipation, reward anticipation and reward delivery. Hum Brain Mapp. 2012;33:2174–88. doi: 10.1002/hbm.21351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vollstädt-Klein S, Loeber S, Richter A, Kirsch M, Bach P, von der Goltz C, et al. Validating incentive salience with functional magnetic resonance imaging: association between mesolimbic cue reactivity and attentional bias in alcohol-dependent patients. Addict Biol. 2012;17:807–16. doi: 10.1111/j.1369-1600.2011.00352.x. [DOI] [PubMed] [Google Scholar]
- 14.Wiers CE, Stelzel C, Park SQ, Gawron CK, Ludwig VU, Gutwinski S, et al. Neural correlates of alcohol-approach bias in alcohol addiction: the spirit is willing but the flesh is weak for spirits. Neuropsychopharmacology. 2014;39:688–97. doi: 10.1038/npp.2013.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muller-Oehring EM, Le Berre AP, Serventi M, Kalon E, Haas AL, Padula CB, et al. Brain activation to cannabis- and alcohol-related words in alcohol use disorder. Psychiatry Res Neuroimaging. 2019;294:111005. doi: 10.1016/j.pscychresns.2019.111005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Ciano P, Cardinal RN, Cowell RA, Little SJ, Everitt BJ. Differential involvement of NMDA, AMPA/kainate, and dopamine receptors in the nucleus accumbens core in the acquisition and performance of pavlovian approach behavior. J Neurosci. 2001;21:9471–7. doi: 10.1523/JNEUROSCI.21-23-09471.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parkinson JA, Dalley JW, Cardinal RN, Bamford A, Fehnert B, Lachenal G, et al. Nucleus accumbens dopamine depletion impairs both acquisition and performance of appetitive Pavlovian approach behaviour: implications for mesoaccumbens dopamine function. Behavioural Brain Res. 2002;137:149–63. doi: 10.1016/s0166-4328(02)00291-7. [DOI] [PubMed] [Google Scholar]
- 18.Day JJ, Roitman MF, Wightman RM, Carelli RM. Associative learning mediates dynamic shifts in dopamine signaling in the nucleus accumbens. Nat Neurosci. 2007;10:1020–8. doi: 10.1038/nn1923. [DOI] [PubMed] [Google Scholar]
- 19.Flagel SB, Clark JJ, Robinson TE, Mayo L, Czuj A, Willuhn I, et al. A selective role for dopamine in stimulus-reward learning. Nature. 2011;469:53–7. doi: 10.1038/nature09588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Millan EZ, Kim HA, Janak PH. Optogenetic activation of amygdala projections to nucleus accumbens can arrest conditioned and unconditioned alcohol consummatory behavior. Neuroscience. 2017;360:106–17. doi: 10.1016/j.neuroscience.2017.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chaudhri N, Woods CA, Sahuque LL, Gill TM, Janak PH. Unilateral inactivation of the basolateral amygdala attenuates context-induced renewal of Pavlovian-conditioned alcohol-seeking. Eur J Neurosci. 2013;38:2751–61. doi: 10.1111/ejn.12278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Corbit LH, Fischbach SC, Janak PH. Nucleus accumbens core and shell are differentially involved in general and outcome-specific forms of Pavlovian-instrumental transfer with alcohol and sucrose rewards. Eur J Neurosci. 2016;43:1229–36. doi: 10.1111/ejn.13235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shnitko TA, Robinson DL. Regional variation in phasic dopamine release during alcohol and sucrose self-administration in rats. ACS Chem Neurosci. 2015;6:147–54. doi: 10.1021/cn500251j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sparks LM, Sciascia JM, Ayorech Z, Chaudhri N. Vendor differences in alcohol consumption and the contribution of dopamine receptors to Pavlovian-conditioned alcohol-seeking in Long-Evans rats. Psychopharmacol (Berl) 2014;231:753–64. [Google Scholar]
- 25.Fiorenza AM, Shnitko TA, Sullivan KM, Vemuru SR, Gomez AA, Esaki JY, et al. Ethanol exposure history and alcoholic reward differentially alter dopamine release in the nucleus accumbens to a reward-predictive cue. Alcohol Clin Exp Res. 2018;42:1051–61. doi: 10.1111/acer.13636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wallis JD, Kennerley SW. Heterogeneous reward signals in prefrontal cortex. Curr Opin Neurobiol. 2010;20:191–98. doi: 10.1016/j.conb.2010.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ballard IC, Murty VP, Carter RM, MacInnes JJ, Huettel SA, Adcock RA. Dorsolateral prefrontal cortex drives mesolimbic dopaminergic regions to initiate motivated behavior. J Neurosci: Off J Soc Neurosci. 2011;31:10340–6. doi: 10.1523/JNEUROSCI.0895-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murty VP, Ballard IC, Adcock RA. Hippocampus and prefrontal cortex predict distinct timescales of activation in the human ventral tegmental area. Cereb Cortex. 2017;27:1660–69. doi: 10.1093/cercor/bhw005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kelm MK, Boettiger CA. Effects of acute dopamine precusor depletion on immediate reward selection bias and working memory depend on catechol-O-methyltransferase genotype. J Cogn Neurosci. 2013;25:2061–71. doi: 10.1162/jocn_a_00464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelm MK, Boettiger CA. Age moderates the effect of acute dopamine depletion on passive avoidance learning. Pharmacol Biochem Behav. 2015;131:57–63. doi: 10.1016/j.pbb.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nagano-Saito A, Cisek P, Perna AS, Shirdel FZ, Benkelfat C, Leyton M, et al. From anticipation to action, the role of dopamine in perceptual decision making: an fMRI-tyrosine depletion study. J Neurophysiol. 2012;108:501–12. doi: 10.1152/jn.00592.2011. [DOI] [PubMed] [Google Scholar]
- 32.da Silva Alves F, Schmitz N, Figee M, Abeling N, Hasler G, van der Meer J, et al. Dopaminergic modulation of the human reward system: a placebo-controlled dopamine depletion fMRI study. J Psychopharmacol. 2011;25:538–49. doi: 10.1177/0269881110367731. [DOI] [PubMed] [Google Scholar]
- 33.Bjork JM, Grant SJ, Chen G, Hommer DW. Dietary tyrosine/phenylalanine depletion effects on behavioral and brain signatures of human motivational processing. Neuropsychopharmacology. 2014;39:595–604. doi: 10.1038/npp.2013.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hitsman B, MacKillop J, Lingford-Hughes A, Williams TM, Ahmad F, Adams S, et al. Effects of acute tyrosine/phenylalanine depletion on the selective processing of smoking-related cues and the relative value of cigarettes in smokers. Psychopharmacology. 2008;196:611–21. doi: 10.1007/s00213-007-0995-5. [DOI] [PubMed] [Google Scholar]
- 35.Pascual M, Boix J, Felipo V, Guerri C. Repeated alcohol administration during adolescence causes changes in the mesolimbic dopaminergic and glutamatergic systems and promotes alcohol intake in the adult rat. J neurochemistry. 2009;108:920–31. doi: 10.1111/j.1471-4159.2008.05835.x. [DOI] [PubMed] [Google Scholar]
- 36.Spoelder M, Tsutsui KT, Lesscher HM, Vanderschuren LJ, Clark JJ. Adolescent alcohol exposure amplifies the incentive value of reward-predictive cues through potentiation of phasic dopamine signaling. Neuropsychopharmacology. 2015;40:2873–85. doi: 10.1038/npp.2015.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thielen RJ, Engleman EA, Rodd ZA, Murphy JM, Lumeng L, Li T-K, et al. Ethanol drinking and deprivation alter dopaminergic and serotonergic function in the nucleus accumbens of alcohol-preferring rats. J Pharmacol Exp Therapeutics. 2004;309:216–25. doi: 10.1124/jpet.103.059790. [DOI] [PubMed] [Google Scholar]
- 38.Wai JM, Grassetti A, Slifstein M, Matuskey D, Nabulsi N, Ropchan J, et al. Binge alcohol use is not associated with alterations in striatal dopamine receptor binding or dopamine release. Drug alcohol Depend. 2019;205:107627. doi: 10.1016/j.drugalcdep.2019.107627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kritzer MF, Kohama SG. Ovarian hormones influence the morphology, distribution, and density of tyrosine hydroxylase immunoreactive axons in the dorsolateral prefrontal cortex of adult rhesus monkeys. J Comp Neurol. 1998;395:1–17. [PubMed] [Google Scholar]
- 40.Becker JB. Gender differences in dopaminergic function in striatum and nucleus accumbens. Pharmacol Biochem Behav. 1999;64:803–12. doi: 10.1016/s0091-3057(99)00168-9. [DOI] [PubMed] [Google Scholar]
- 41.Rosenberg L, Park S. Verbal and spatial functions across the menstrual cycle in healthy young women. Psychoneuroendocrinology. 2002;27:835–41. doi: 10.1016/s0306-4530(01)00083-x. [DOI] [PubMed] [Google Scholar]
- 42.Shansky RM, Glavis-Bloom C, Lerman D, McRae P, Benson C, Miller K, et al. Estrogen mediates sex differences in stress-induced prefrontal cortex dysfunction. Mol Psychiatry. 2004;9:531–8. doi: 10.1038/sj.mp.4001435. [DOI] [PubMed] [Google Scholar]
- 43.Joffe H, Hall JE, Gruber S, Sarmiento IA, Cohen LS, Yurgelun-Todd D, et al. Estrogen therapy selectively enhances prefrontal cognitive processes: a randomized, double-blind, placebo-controlled study with functional magnetic resonance imaging in perimenopausal and recently postmenopausal women. Menopause. 2006;13:411–22. doi: 10.1097/01.gme.0000189618.48774.7b. [DOI] [PubMed] [Google Scholar]
- 44.Gasbarri A, Pompili A, d’Onofrio A, Cifariello A, Tavares MC, Tomaz C. Working memory for emotional facial expressions: role of the estrogen in young women. Psychoneuroendocrinology. 2008;33:964–72. doi: 10.1016/j.psyneuen.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 45.Jacobs E, D’Esposito M. Estrogen shapes dopamine-dependent cognitive processes: implications for women’s health. J Neurosci. 2011;31:5286–93. doi: 10.1523/JNEUROSCI.6394-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smith CT, Sierra Y, Oppler SH, Boettiger CA. Ovarian Cycle Effects on Immediate Reward Selection Bias in Humans: A Role for Estradiol. J Neurosci. 2014;34:5468–76. doi: 10.1523/JNEUROSCI.0014-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.US Department of Health and Human Services. National Institute on Alcohol Abuse and Alcoholism NIAAA Council approves definition of binge drinking. InNIAAA Newsletter; US Department of Health and Human Services: Washington, DC, USA, 2004.
- 48.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 49.Moja EA, Lucini V, Benedetti F, Lucca A. Decrease in plasma phenylalanine and tyrosine after phenylalanine-tyrosine free amino acid solutions in man. Life Sci. 1996;58:2389–95. doi: 10.1016/0024-3205(96)00242-1. [DOI] [PubMed] [Google Scholar]
- 50.Sheehan B, Tharyan P, McTavish S, Campling G, Cowen P. Use of a dietary manipulation to deplete plasma tyrosine and phenylalanine in healthy subjects. J Psychopharm. 1996;10:231–34. doi: 10.1177/026988119601000309. [DOI] [PubMed] [Google Scholar]
- 51.Karobath M, Baldessarini RJ. Formation of catechol compounds from phenylalanine and tyrosine with isolated nerve endings. Nat: N. Biol. 1972;236:206–8. doi: 10.1038/newbio236206a0. [DOI] [PubMed] [Google Scholar]
- 52.Fernstrom JD, Fernstrom MH. Tyrosine, phenylalanine, and catecholamine synthesis and function in the brain. J Nutr. 2007;137:1539S–47S. doi: 10.1093/jn/137.6.1539S. [DOI] [PubMed] [Google Scholar]
- 53.Booij L, Van der Does AJ, Riedel WJ. Monoamine depletion in psychiatric and healthy populations: review. Mol Psychiatry. 2003;8:951–73. doi: 10.1038/sj.mp.4001423. [DOI] [PubMed] [Google Scholar]
- 54.Leyton M, Dagher A, Boileau I, Casey K, Baker GB, Diksic M, et al. Decreasing amphetamine-induced dopamine release by acute phenylalanine/tyrosine depletion: A PET/[11C]raclopride study in healthy men. Neuropsychopharmacology. 2004;29:427–32. doi: 10.1038/sj.npp.1300328. [DOI] [PubMed] [Google Scholar]
- 55.Montgomery AJ, McTavish SF, Cowen PJ, Grasby PM. Reduction of brain dopamine concentration with dietary tyrosine plus phenylalanine depletion: an [11C]raclopride PET study. Am J psychiatry. 2003;160:1887–9. doi: 10.1176/appi.ajp.160.10.1887. [DOI] [PubMed] [Google Scholar]
- 56.Palmour RM, Ervin FR, Baker GB, Young SN. An amino acid mixture deficient in phenylalanine and tyrosine reduces cerebrospinal fluid catecholamine metabolites and alcohol consumption in vervet monkeys. Psychopharmacology. 1998;136:1–7. doi: 10.1007/s002130050532. [DOI] [PubMed] [Google Scholar]
- 57.Shnitko TA, Taylor SC, Stringfield SJ, Zandy SL, Cofresi RU, Doherty JM, et al. Acute phenylalanine/tyrosine depletion of phasic dopamine in the rat brain. Psychopharmacology. 2016;233:2045–54. doi: 10.1007/s00213-016-4259-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McTavish SF, Callado L, Cowen PJ, Sharp T. Comparison of the effects of alpha-methyl-p-tyrosine and a tyrosine-free amino acid load on extracellular noradrenaline in the rat hippocampus in vivo. J Psychopharmacol (Oxf, Engl) 1999;13:379–84. doi: 10.1177/026988119901300408. [DOI] [PubMed] [Google Scholar]
- 59.Bloemen OJ, De Koning M, Boot E, Booij J, van Amelsvoort T. Challenge and therapeutic studies using alpha-methyl-para-tyrosine (AMPT) in neuropsychiatric disorders: a review. Cent Nerv Syst Agents Medicinal Chem. 2008;8:249–56. [Google Scholar]
- 60.Townshend JM, Duka T. Patterns of alcohol drinking in a population of young social drinkers: a comparison of questionnaire and diary measures. Alcohol Alcohol (Oxf, Oxfs) 2002;37:187–92. doi: 10.1093/alcalc/37.2.187. [DOI] [PubMed] [Google Scholar]
- 61.Elton A, Dove S, Spencer CN, Robinson DL, Boettiger CA. Naltrexone Acutely Enhances Connectivity Between the Ventromedial Prefrontal Cortex and a Left Frontoparietal Network. Alcohol, Clin Exp Res. 2019;43:965–78. doi: 10.1111/acer.13999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chanon VW, Sours CR, Boettiger CA. Attentional bias toward cigarette cues in active smokers. Psychopharmacology. 2010;212:309–20. doi: 10.1007/s00213-010-1953-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Elton A, Chanon VW, Boettiger CA. Multivariate pattern analysis of the neural correlates of smoking cue attentional bias. Pharmacol Biochem Behav. 2019;180:1–10. doi: 10.1016/j.pbb.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Most SB, Laurenceau JP, Graber E, Belcher A, Smith CV. Blind jealousy? romantic insecurity increases emotion-induced failures of visual perception. Emotion. 2010;10:250–56. doi: 10.1037/a0019007. [DOI] [PubMed] [Google Scholar]
- 65.Most SB, Smith SD, Cooter AB, Levy BN, Zald DH. The naked truth: positive, arousing distractors impair rapid target perception. Cognition Emot. 2007;21:964–81. [Google Scholar]
- 66.Most SB, Chun MM, Widders DM, Zald DH. Attentional rubbernecking: Cognitive control and personality in emotion-induced blindness. Psychonomic Bull & Rev. 2005;12:654–61. doi: 10.3758/bf03196754. [DOI] [PubMed] [Google Scholar]
- 67.Kennedy BL, Most SB. Perceptual, not memorial, disruption underlies emotion-induced blindness. Emotion. 2012;12:199–202. doi: 10.1037/a0026380. [DOI] [PubMed] [Google Scholar]
- 68.Most SB. Setting sights higher: category-level attentional set modulates sustained inattentional blindness. Psychological Research. 2013;77:139–46. doi: 10.1007/s00426-011-0379-7. [DOI] [PubMed] [Google Scholar]
- 69.Wais PE, Rubens MT, Boccanfuso J, Gazzaley A. Neural mechanisms underlying the impact of visual distraction on retrieval of long-term memory. J Neurosci. 2010;30:8541–50. doi: 10.1523/JNEUROSCI.1478-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Anderson AK, Wais PE, Gabrieli JD. Emotion enhances remembrance of neutral events past. Proc Natl Acad Sci USA. 2006;103:1599–604. doi: 10.1073/pnas.0506308103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Smith PF. A note on the advantages of using linear mixed model analysis with maximal likelihood estimation over repeated measures ANOVAs in psychopharmacology: comment on Clark et al. (2012) J Psychopharmacol. 2012;26:1605–07. doi: 10.1177/0269881112463471. [DOI] [PubMed] [Google Scholar]
- 72.Anderson BA, Laurent PA, Yantis S. Value-driven attentional capture. Proc Natl Acad Sci USA. 2011;108:10367–71. doi: 10.1073/pnas.1104047108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Computers Biomed Res. 1996;29:162–73. doi: 10.1006/cbmr.1996.0014. [DOI] [PubMed] [Google Scholar]
- 74.Power JD, Barnes KA, Snyder AZ, Schlaggar BL, Petersen SE. Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. NeuroImage. 2012;59:2142–54. doi: 10.1016/j.neuroimage.2011.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Power JD, Mitra A, Laumann TO, Snyder AZ, Schlaggar BL, Petersen SE. Methods to detect, characterize, and remove motion artifact in resting state fMRI. NeuroImage. 2014;84:320–41. doi: 10.1016/j.neuroimage.2013.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Brain Res Rev. 1998;28:309–69. doi: 10.1016/s0165-0173(98)00019-8. [DOI] [PubMed] [Google Scholar]
- 77.Wise RA. Dopamine, learning and motivation. Nat Rev Neurosci. 2004;5:483–94. doi: 10.1038/nrn1406. [DOI] [PubMed] [Google Scholar]
- 78.Goto Y, Grace AA. Dopamine-dependent interactions between limbic and prefrontal cortical plasticity in the nucleus accumbens: disruption by cocaine sensitization. Neuron. 2005;47:255–66. doi: 10.1016/j.neuron.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 79.Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Annu Rev Neurosci. 2001;24:167–202. doi: 10.1146/annurev.neuro.24.1.167. [DOI] [PubMed] [Google Scholar]
- 80.Watanabe M, Sakagami M. Integration of cognitive and motivational context information in the primate prefrontal cortex. Cereb cortex. 2007;17:i101–9. doi: 10.1093/cercor/bhm067. [DOI] [PubMed] [Google Scholar]
- 81.Schultz W. Predictive reward signal of dopamine neurons. J Neurophysiol. 1998;80:1–27. doi: 10.1152/jn.1998.80.1.1. [DOI] [PubMed] [Google Scholar]
- 82.Yan C-G, Craddock RC, Zuo X-N, Zang Y-F, Milham MP. Standardizing the intrinsic brain: towards robust measurement of inter-individual variation in 1000 functional connectomes. Neuroimage. 2013;80:246–62. doi: 10.1016/j.neuroimage.2013.04.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wager TD, Davidson ML, Hughes BL, Lindquist MA, Ochsner KN. Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron. 2008;59:1037–50. doi: 10.1016/j.neuron.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Anderson BA, Kuwabara H, Wong DF, Roberts J, Rahmim A, Brašić JR, et al. Linking dopaminergic reward signals to the development of attentional bias: a positron emission tomographic study. Neuroimage. 2017;157:27–33. doi: 10.1016/j.neuroimage.2017.05.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Geva R, Zivan M, Warsha A, Olchik D. Alerting, orienting or executive attention networks: differential patters of pupil dilations. Front Behav Neurosci. 2013;7:145. doi: 10.3389/fnbeh.2013.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.McTavish SF, Cowen PJ, Sharp T. Effect of a tyrosine-free amino acid mixture on regional brain catecholamine synthesis and release. Psychopharmacology. 1999;141:182–8. doi: 10.1007/s002130050823. [DOI] [PubMed] [Google Scholar]
- 87.Harmer CJ, McTavish SF, Clark L, Goodwin GM, Cowen PJ. Tyrosine depletion attenuates dopamine function in healthy volunteers. Psychopharmacology. 2001;154:105–11. doi: 10.1007/s002130000613. [DOI] [PubMed] [Google Scholar]
- 88.Cservenka A, Jones SA, Nagel BJ. Reduced cerebellar brain activity during reward processing in adolescent binge drinkers. Dev Cogn Neurosci. 2015;16:110–20. doi: 10.1016/j.dcn.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liu W, Crews FT. Adolescent intermittent ethanol exposure enhances ethanol activation of the nucleus accumbens while blunting the prefrontal cortex responses in adult rat. Neuroscience. 2015;293:92–108. doi: 10.1016/j.neuroscience.2015.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Vetreno RP, Crews FT. Binge ethanol exposure during adolescence leads to a persistent loss of neurogenesis in the dorsal and ventral hippocampus that is associated with impaired adult cognitive functioning. Front Neurosci. 2015;9:35. doi: 10.3389/fnins.2015.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Crews F, He J, Hodge C. Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86:189–99. doi: 10.1016/j.pbb.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gass JT, Glen WB, Jr., McGonigal JT, Trantham-Davidson H, Lopez MF, Randall PK, et al. Adolescent alcohol exposure reduces behavioral flexibility, promotes disinhibition, and increases resistance to extinction of ethanol self-administration in adulthood. Neuropsychopharmacology. 2014;39:2570–83. doi: 10.1038/npp.2014.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sey NYA, Gomez AA, Madayag AC, Boettiger CA, Robinson DL. Adolescent intermittent ethanol impairs behavioral flexibility in a rat foraging task in adulthood. Behavioural brain Res. 2019;373:112085. doi: 10.1016/j.bbr.2019.112085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wahlstrom D, Collins P, White T, Luciana M. Developmental changes in dopamine neurotransmission in adolescence: behavioral implications and issues in assessment. Brain Cogn. 2010;72:146–59. doi: 10.1016/j.bandc.2009.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Luciana M. Adolescent brain development in normality and psychopathology. Dev Psychopathol. 2013;25:1325–45. doi: 10.1017/S0954579413000643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nigg JT, Wong MM, Martel MM, Jester JM, Puttler LI, Glass JM, et al. Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. J Am Acad Child Adolesc Psychiatry. 2006;45:468–75. doi: 10.1097/01.chi.0000199028.76452.a9. [DOI] [PubMed] [Google Scholar]
- 97.Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, et al. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. Am J Psychiatry. 2003;160:1078–85. doi: 10.1176/appi.ajp.160.6.1078. [DOI] [PubMed] [Google Scholar]
- 98.Fernandez GM, Lew BJ, Vedder LC, Savage LM. Chronic intermittent ethanol exposure leads to alterations in brain-derived neurotrophic factor within the frontal cortex and impaired behavioral flexibility in both adolescent and adult rats. Neuroscience. 2017;348:324–34. doi: 10.1016/j.neuroscience.2017.02.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Badanich KA, Becker HC, Woodward JJ. Effects of chronic intermittent ethanol exposure on orbitofrontal and medial prefrontal cortex-dependent behaviors in mice. Behavioral Neurosci. 2011;125:879. doi: 10.1037/a0025922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nimitvilai S, Lopez MF, Mulholland PJ, Woodward JJ. Chronic intermittent ethanol exposure enhances the excitability and synaptic plasticity of lateral orbitofrontal cortex neurons and induces a tolerance to the acute inhibitory actions of ethanol. Neuropsychopharmacology. 2016;41:1112–27. doi: 10.1038/npp.2015.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shafiei G, Zeighami Y, Clark CA, Coull JT, Nagano-Saito A, Leyton M, et al. Dopamine signaling modulates the stability and integration of intrinsic brain networks. Cereb Cortex. 2019;29:397–409. doi: 10.1093/cercor/bhy264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Carbonell F, Nagano-Saito A, Leyton M, Cisek P, Benkelfat C, He Y, et al. Dopamine precursor depletion impairs structure and efficiency of resting state brain functional networks. Neuropharmacology. 2014;84:90–100. doi: 10.1016/j.neuropharm.2013.12.021. [DOI] [PubMed] [Google Scholar]
- 103.Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–56. doi: 10.1523/JNEUROSCI.5587-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Saunders BT, Robinson TE. The role of dopamine in the accumbens core in the expression of Pavlovian-conditioned responses. Eur J Neurosci. 2012;36:2521–32. doi: 10.1111/j.1460-9568.2012.08217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Grusser SM, Wrase J, Klein S, Hermann D, Smolka MN, Ruf M, et al. Cue-induced activation of the striatum and medial prefrontal cortex is associated with subsequent relapse in abstinent alcoholics. Psychopharmacology. 2004;175:296–302. doi: 10.1007/s00213-004-1828-4. [DOI] [PubMed] [Google Scholar]
- 106.Volkow ND, Wang GJ, Telang F, Fowler JS, Logan J, Childress AR, et al. Cocaine cues and dopamine in dorsal striatum: mechanism of craving in cocaine addiction. J Neurosci. 2006;26:6583–8. doi: 10.1523/JNEUROSCI.1544-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Volkow ND, Morales M. The brain on drugs: from reward to addiction. Cell. 2015;162:712–25. doi: 10.1016/j.cell.2015.07.046. [DOI] [PubMed] [Google Scholar]
- 108.Etkin A, Schatzberg AF. Common abnormalities and disorder-specific compensation during implicit regulation of emotional processing in generalized anxiety and major depressive disorders. Am J Psychiatry. 2011;168:968–78. doi: 10.1176/appi.ajp.2011.10091290. [DOI] [PubMed] [Google Scholar]
- 109.Egner T, Etkin A, Gale S, Hirsch J. Dissociable neural systems resolve conflict from emotional versus nonemotional distracters. Cereb Cortex. 2008;18:1475–84. doi: 10.1093/cercor/bhm179. [DOI] [PubMed] [Google Scholar]
- 110.Kompus K, Hugdahl K, Ohman A, Marklund P, Nyberg L. Distinct control networks for cognition and emotion in the prefrontal cortex. Neurosci Lett. 2009;467:76–80. doi: 10.1016/j.neulet.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 111.Passamonti L, Rowe JB, Ewbank M, Hampshire A, Keane J, Calder AJ. Connectivity from the ventral anterior cingulate to the amygdala is modulated by appetitive motivation in response to facial signals of aggression. Neuroimage. 2008;43:562–70. doi: 10.1016/j.neuroimage.2008.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev. 2011;12:652–69. doi: 10.1038/nrn3119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506. doi: 10.1016/j.tics.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 114.Menon V, Uddin LQ. Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct. 2010;214:655–67. doi: 10.1007/s00429-010-0262-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Conio B, Martino M, Magioncalda P, Escelsior A, Inglese M, Amore M, et al. Opposite effects of dopamine and serotonin on resting-state networks: review and implications for psychiatric disorders. Mol Psychiatry. 2020;25:82–93. doi: 10.1038/s41380-019-0406-4. [DOI] [PubMed] [Google Scholar]
- 116.Hilland E, Landrø NI, Harmer CJ, Maglanoc LA, Jonassen R. Within-Network Connectivity in the Salience Network After Attention Bias Modification Training in Residual Depression: Report From a Preregistered Clinical Trial. Front Hum Neurosci. 2018;12:508. doi: 10.3389/fnhum.2018.00508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cools R, Frank MJ, Gibbs SE, Miyakawa A, Jagust W, D’Esposito M. Striatal dopamine predicts outcome-specific reversal learning and its sensitivity to dopaminergic drug administration. J Neurosci. 2009;29:1538–43. doi: 10.1523/JNEUROSCI.4467-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Robinson OJ, Standing HR, DeVito EE, Cools R, Sahakian BJ. Dopamine precursor depletion improves punishment prediction during reversal learning in healthy females but not males. Psychopharmacology. 2010;211:187–95. doi: 10.1007/s00213-010-1880-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Munro CA, McCaul ME, Wong DF, Oswald LM, Zhou Y, Brasic J, et al. Sex differences in striatal dopamine release in healthy adults. Biol Psychiatry. 2006;59:966–74. doi: 10.1016/j.biopsych.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 120.Murty VP, Shermohammed M, Smith DV, Carter RM, Huettel SA, Adcock RA. Resting state networks distinguish human ventral tegmental area from substantia nigra. NeuroImage. 2014;100:580–9. doi: 10.1016/j.neuroimage.2014.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Uddin LQ, Supekar KS, Ryali S, Menon V. Dynamic reconfiguration of structural and functional connectivity across core neurocognitive brain networks with development. J Neurosci. 2011;31:18578–89. doi: 10.1523/JNEUROSCI.4465-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Desikan RS, Segonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31:968–80. doi: 10.1016/j.neuroimage.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 123.Ma N, Liu Y, Li N, Wang C-X, Zhang H, Jiang X-F, et al. Addiction related alteration in resting-state brain connectivity. NeuroImage. 2010;49:738–44. doi: 10.1016/j.neuroimage.2009.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tziortzi AC, Haber SN, Searle GE, Tsoumpas C, Long CJ, Shotbolt P, et al. Connectivity-based functional analysis of dopamine release in the striatum using diffusion-weighted MRI and positron emission tomography. Cereb Cortex. 2014;24:1165–77. doi: 10.1093/cercor/bhs397. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.