Abstract
OBJECTIVE:
Post-traumatic stress disorder (PTSD) is common in Veterans. Symptoms can perpetuate into late life, negatively impacting physical and mental health. Exercise and social support are beneficial in treating anxiety disorders such as PTSD in the general population, although less is known about the impact on Veterans who have lived with PTSD for decades. This study assessed associations between social connectedness, physical function and self-reported change in PTSD symptoms among older Veterans specifically participating in Gerofit.
DESIGN:
Prospective clinical intervention.
SETTING:
Twelve sites of Veterans Affairs (VA) Gerofit exercise program across the United States.
PARTICIPANTS:
Three hundred and twenty one older Veteran Gerofit participants (mean age = 74) completed physical assessments and questionnaires regarding physical and emotional symptoms and their experience.
MEASUREMENTS:
Measures of physical function, including 30-second chair stands, 10-m and 6-min walk were assessed at baseline and 3 months; change in PTSD symptoms based on the Diagnostic Statistical Manual—5 (DSM-5) assessed by a self-report questionnaire; and social connection measured by the Relatedness Subscale of the Psychological Need Satisfaction in Exercise scale (PNSE) were evaluated after 3 months of participation in Gerofit.
RESULTS:
Ninety five (29.6%) Veterans reported PTSD. Significant improvement was noted in self-rated PTSD symptoms at 3 months (P < .05). Moderate correlation (r = .44) was found between social connectedness with other participants in Gerofit and PTSD symptom improvement for those Veterans who endorsed improvement (n = 59). All participants improved on measures of physical function. In Veterans who endorsed PTSD there were no significant associations between physical function improvement and PTSD symptoms.
CONCLUSION:
Veterans with PTSD that participated in Gerofit group exercise reported symptom improvement, and social connectedness was significantly associated with this improvement. In addition to physical health benefits, the social context of Gerofit may offer a potential resource for improving PTSD symptoms in older Veterans that warrants further study.
Keywords: PTSD, exercise, older adult, social support, Gerofit
Posttraumatic stress disorder (PTSD) was first recognized as a diagnosis in 1980 and is reported to have an estimated 30% lifetime prevalence in older Vietnam Veterans, the only group with a large enough cohort to determine prevalence.1 Veterans with PTSD are at greater risk of physical and mental health disorders including chronic pain, major depressive disorder, substance abuse, poorer cardiovascular and metabolic outcomes, and poorer adherence to positive health behaviors.2–6
Exercise intervention programs have shown promise as both primary and adjunctive interventions for many psychiatric conditions including depression and anxiety.7–10 Systematic review suggests that exercise decreases PTSD symptoms in younger Veterans, with strenuous exercise showing direct effects on avoidance/numbing and hyperarousal.11,12 There is a paucity of research on older Veterans, many of whom have lived with the burden of PSTD for over 30 years. Recently, a pilot study of exercise for older Veterans with PTSD demonstrated a 16% overall improvement in PTSD symptoms, with improvements found in several Diagnostic and Statistical Manual 5 (DSM 5) PTSD symptom clusters: 19% improvement in Negative Cognitions and Mood, and a 21% improvement in Re-experiencing from baseline to 3 months.13
The social aspect of exercise programs may also be a key element in improving mental health outcomes. Strong social connection is associated with better physical and mental health in older adults, and was the strongest predictor of positive mood in older adults participating in exercise programs in Australia.14,15 Specifically related to PTSD, a study of prolonged exposure treatment in middle aged Veterans found higher perceived social support was associated with reduced PTSD symptom severity.16
Gerofit is a supervised group exercise program that promotes health and wellness for older Veterans at 17 VA Healthcare sites around the United States. Gerofit participants have demonstrated significant gains in physical function that are maintained over 5-year follow-up, improvements in general well-being, and a 10-year 25% survival benefit.17 The current study evaluated older Veteran participant’s self-reported change in PTSD symptoms 3 months after enrollment in Gerofit. The goal was to determine if the Gerofit exercise program improved symptoms of PTSD, and if so, if physical gains or social engagement was associated with PTSD symptom improvement.
METHODS
The Gerofit Program
Gerofit is an exercise and health promotion program for Veterans ages 65 and above. Declared a VA Best Practice, it has been implemented in 17 medical centers.17 This analysis includes 321 participants across 12 sites who completed the self-reported change in PTSD symptoms survey at 3 months.
Exclusion criteria include those unable to perform ADLs; cognitive impairment leading to inability to function independently without assistance; unstable angina pectoris; proliferative diabetic retinopathy; oxygen dependence; no transportation to Gerofit; incontinence; open wounds; volatile behavior or inability to be effective in a group setting; active substance abuse and homelessness..17 Veterans are referred to Gerofit by their primary care providers who need to approve physical activity. At baseline, all Gerofit Veterans undergo a physical function assessment including gait speed (10-m walk); lower extremity strength (30-s chair stands); and cardiovascular endurance (6-min walk). Based on the baseline assessment, Veterans are given an individualized exercise prescription which may include resistance, aerobic, and balance and flexibility exercises. The exercises are progressed over time based on subsequent assessments. They are encouraged to attend Gerofit at least twice weekly. For aerobic exercises, the goal is moderate intensity (4–6 on the Borg Perceived Exertion Scale) and for resistance exercises, the goal is vigorous intensity (7–8 on the Borg Perceived Exertion Scale). Additional questionnaire data are collected at all subsequent assessment timepoints, including questions about change in PTSD symptoms (the focus of this report). All data were collected for clinical purposes and the Durham Institutional Review Board provided a waiver to allow the data to be combined across Gerofit sites.
Assessment of Change in PTSD Symptoms
A self-report PTSD survey to assess for change in PTSD symptoms was developed for this study (added in January 2018) and first given at the 3-month assessment timepoint if Veterans indicated that they had PTSD (Figure 1). This survey was based on the four PTSD symptom clusters in DSM-V18 and asked about the effect of Gerofit on: overall symptoms; disturbing memories/dreams and strong physical/psychological reactions to reminders of the stressful experience; avoiding thoughts or feelings or external clues that reminded them of the stressful experience; strong negative feelings, feeling distant or cut off from people or having trouble experiencing positive feelings; or being irritable, “super-alert” or watchful, having difficulty with concentration or sleep. Veterans responded with a 5-point Likert scale, ranging from worsening of symptoms to no change in symptoms to improvement of symptoms.
Figure 1.
Self-report scale of PTSD symptoms.
Assessment of Social Connection
The 6-item Relatedness Subscale from the Psychological Need Satisfaction in Exercise scale (PNSE) (Wilson, 2006) assessed the perception of social connection between Veterans who were exercising together.19 Examples of questions asked in the scale included: if Veterans felt attached to exercise companions because of acceptance; do they feel they share a common bond with people who are important to them; do they feel a sense of camaraderie; do they feel connected; and do they get along well with other people while exercising. Veterans responded from 1—definitely false to 6—definitely true with higher overall number indicating higher perception of social connectedness. A total score was obtained by summing across all items- this was used in all analyses.
Statistical Plan
Analyses were conducted in SPSSv25. Independent t-tests and chi square were used to compare PTSD+ and PTSD− groups on demographics. In those with PTSD, the mean response to PTSD symptom change was calculated for each symptom separately. One-sample t-tests were used to determine if the average change in symptoms was significantly greater than no change (rating of “3”) and multivariate analysis of variance (MANOVA) with all symptoms as the dependent variables was used to determine if there was a differential response based on symptom type. Independent samples t-tests were used to compare the PTSD+ and PTSD− groups on social connection. Mixed effects ANOVA was used to assess differences in change in physical function over time (baseline, 3 months) based on self-reported PTSD diagnosis. Pearson correlation was used to assess associations between symptom change, social connectedness, and physical fitness gains in those with PTSD. Not all participants had data for all variables. If a participant had missing data for a given analysis, they were excluded. Sample sizes are specified for each analysis.
RESULTS
Sample Characteristics
Comparisons were made between those with and without PTSD at baseline (Table 1). Two hundred and sixty six Veterans self-reported no PTSD and 95 self-reported having PTSD. There were no differences in demographic characteristics between groups except for age, those with PTSD were 4 years younger (P < .001).
Table 1.
Participant Demographics and PTSD Rates
| Total n = 321 | No PTSD n = 226 | PTSD n = 95 | P-value | |
|---|---|---|---|---|
| Age | 73.92 ± 6.76 | 75.09 ± 7.31 | 71.14 ± 4.09 | t = 4.94, P < .001a |
| Sex | χ2 = 0.01, n.s. | |||
| Male | 300 | 211 | 89 | |
| Female | 21 | 15 | 6 | |
| Race: | χ2 = 4.52, n.s. | |||
| Caucasian | 190 (59.2%) | 136 (60.2%) | 54 (56.8%) | |
| African American | 101 (31.5%) | 67 (29.6%) | 34 (35.8%) | |
| Asian | 9 (2.8%) | 5 (2.2%) | 4 (4.2%) | |
| Pacific Islander | 17 (5.3%) | 15 (6.6%) | 2 (2.1%) | |
| Missing | 4 (1.2%) | 3 (1.3%) | 1 (1.1%) | |
| BMI | 30.43 ± 5.36 | 30.12 ± 5.28 | 31.18 ± 5.49 | t = 1.62, n.s. |
Significant at .001 level for age (PTSD sample younger).
Perceived PTSD Symptom Change
Figure 2 shows reported change in PTSD symptoms overall as well as specific symptoms at 3 months. Individuals with PTSD reported significant overall symptom improvement following 3 months of Gerofit participation (n = 84, t(83) = 10.4, P < .001). This was true for all symptoms (intrusion: n = 83, t(82) = 8.2, P < .001; avoidance n = 82, t(81) = 8.4, P < .001; negative cognitions/mood n = 83, t(82) = 10.2, P < .001, hyperarousal n = 86, t(85) = 7.6, P < .001). Results of MANOVA showed an overall effect of symptom type (n = 79, Greenhouse–Geisser corrected, F(2.88, 244.47 = 2.80, P = .043), characterized by less improvement in hyperarousal relative to avoidance (P = .004) and negative cognitions/mood (P < .05) symptoms. Please see Figure 2.
Figure 2.
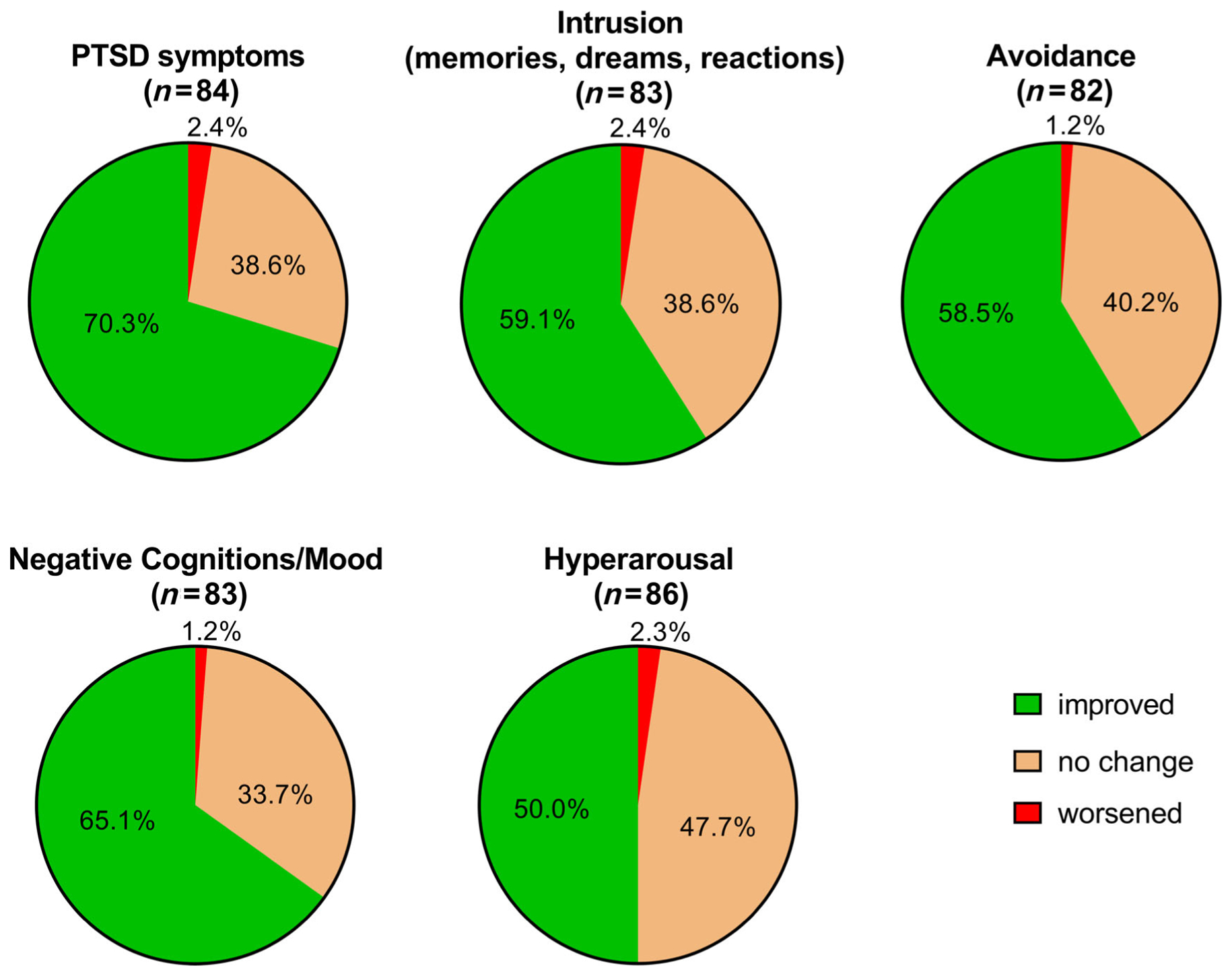
Significant self-rated improvement in overall and specific PTSD symptoms at 3 Months.
Social Connectedness
Social connectedness outcomes at the 3-month timepoint was available from 215 Veterans without PTSD and 92 Veterans with PTSD. The majority of participants (those with and without PTSD) felt they got along well with the other Gerofit participants and endorsed a positive connection, bond, attachment, and sense of camaraderie with their exercise companions. There was no significant difference between PTSD and no PTSD groups on the PNSE perceptions scale total score (t(305) = 1.37, n.s.).
We explored if connectedness was associated with PTSD symptom improvement in the PTSD group. Among the 25 Veterans who did not report symptom improvement there were no significant associations between perceived PTSD symptom changes and PNSE score. Of the 59 Veterans reporting improvement in overall PTSD symptoms; there was a significant association between PNSE score and symptom change, suggesting greater improvement in those who felt more connected to their peers (r = .44, P = .001). This was also observed for intrusion (r = .34, P = .01), avoidance (r = .30, P = .02), negative cognitions/mood (r = .29, P = .03), and hyperarousal (r = .40, P = .002).
Physical Function
Not all participants received both baseline and 3 month assessments; sample sizes are specified for each analysis. For the 10-m walk (n = 208: no PTSD = 147, PTSD = 61, there was no interaction between time and PTSD (n.s), nor overall effect of PTSD on change on 10-m walk time (n.s.). All participants improved over time (F(1,207 = 26.94, P < .001). For the 30-s chair stands (n = 204, no PTSD = 144, PTSD = 60) there was an interaction between time and PTSD (F(1,202 = 4.67, P = .032) and no overall effect of PTSD. There were no differences between groups at baseline or 3 months, but the slope of change was greater in the PTSD group (change score no PTSD = 1.5 ± 3.2; PTSD = 2.7 ± 4.0, t = 2.1, P = .03). All participants showed improvement (F(1,203 = 56.07, P < .001). Finally, for the 6-min walk (n = 208, no PTSD = 146, PTSD = 62) the PTSD by time interaction was not significant (F(1,206) = 3.31, P = .07) and there was no effect of PTSD. All participants improved (F(1,207 = 59.15, P < .001). There were no significant associations between change in 6 min walk distance and PTSD symptom improvement.
DISCUSSION
This preliminary uncontrolled study of the Gerofit exercise program found that older Veteran participants reported significant improvement in their overall PTSD symptoms as well as each of the four PTSD symptom clusters (intrusion, avoidance, negative cognitions/mood, hyperarousal) after 3 months. Of note, smaller improvement was found in hyperarousal relative to avoidance and negative cognitions/mood. Overall PTSD symptom improvement (a bit or a lot) was endorsed by 70% of participants at 3 months. This is consistent with a recent pilot study of 36 older Veterans that found clinically significant improvement in PTSD symptoms of negative cognitions and mood and re-experiencing (intrusion) after 3 months of exercise.16 Studies have also found exercise interventions decrease PTSD symptoms in younger Veterans, with strenuous exercise showing direct effects on avoidance/numbing and hyperarousal.14,15
Social connectedness was rated as high by all Gerofit participants, with the majority endorsing positive social support and relatedness with their exercise companions. In those Veterans with PTSD that reported symptom improvement, positive feelings of social connection were significantly related, accounting for approximately 20% of the gain. Gerofit is comprised of both an exercise component and a social support type club. Participants earn matching Gerofit t-shirts, and members socialize and support each other in their fitness and health goals. Social support is highly valued by participants and the social bond is clearly an important aspect of the Gerofit program. The dimension of social connection is an integral part of the care that goes beyond just the physical exercise benefit. In addition to physical health benefits, the social context of Gerofit may offer a potential resource for improving PTSD symptoms. Novel approaches to improve PTSD symptoms are critical for older Veterans who may be unwilling to participate in psychotherapy or as an adjunctive treatment to maximize symptom improvement.
Prior work has demonstrated improvement in physical function following Gerofit participation.17 We again found that measures of physical function (gait speed, lower extremity strength and cardiovascular endurance) improved significantly for all participants over 3 months, independent of self-reported PTSD symptoms. Lower extremity strength showed greater improvement in the PTSD group, with the PTSD group starting at lower strength suggesting a potential negative effect of PTSD on physical health. Interestingly, in contrast to social connectedness, there were no significant associations between change in physical function measures and PTSD symptom improvement.
There are several limitations to this study. The scale we used to assess PTSD symptoms was based on the DSM 5 but has not been validated. Determination of PTSD was made via self-report of Veterans who had been told they had PTSD rather than asking if they had experienced a trauma or administration of a formal diagnostic interview. The self-report aspect of PTSD symptom change is likely highly meaningful as patient’s personal experience of symptoms is clearly relevant. However future studies will benefit from having formal diagnostic criteria utilized, with specific PTSD symptoms and their level of clinical significance monitored over time through validated instruments. Data was not available to determine if Veterans were receiving concurrent mental health services, including PTSD treatment or psychotropic medications during this study which may have impacted the findings. Finally, as an older Veteran cohort, the vast majority of participants were male thus it is not clear if these findings are generalizable to both sexes.
Future studies will benefit from assessing the role that both exercise/increased fitness and socialization play in improving PTSD in older Veterans to optimize gains. Specifically, effects of exercise and social connection on the four PTSD symptom “clusters” (intrusion, avoidance, negative cognitions/mood and hyperarousal) will be of interest.18 Some participants do not connect and maintain participation in Gerofit and further assessing elements involved in these “drop-outs”, particularly mental health aspects, will also improve care and approaches to optimizing benefits for older Veterans with PTSD. In addition, a control group who is not receiving the Gerofit intervention will be beneficial for comparison. Gerofit may be particularly helpful for older Veterans with PTSD, and these preliminary results suggest that the social support offered may be a key factor. Further study is recommended.
CONCLUSIONS
In this preliminary, non-controlled study, older Veterans participating in the Gerofit exercise program for 3 months self-reported overall PTSD symptom improvement as well as improvement in each of the four PTSD symptom clusters (intrusion, avoidance, negative cognitions/mood, hyperarousal). In those with PTSD that reported symptom improvement, increased social support/connectedness accounted for about 20% of the improvement. Gerofit offers the health advantage of exercise within a social and supportive context and may provide an effective primary or adjunctive intervention for PTSD symptoms in older Veterans.
ACKNOWLEDGMENTS
We are grateful for the VA Offices of Geriatrics and Extended Care and Rural Health for their support, for the VA Greater Los Angeles Healthcare System GRECC and our partner Gerofit programs including the Finger Lakes Health Care System, Canandaigua/Rochester, NY; Baltimore VA Medical Center GRECC and University of Maryland Older Americans Independence Center; VA Cincinnati Medical Center; VA Ann Arbor Health Care System GRECC; VA Pacific Islands Health Care System; VA Puget Sound Health Care System GEC/GRECC; VA Pittsburgh Healthcare System; VA Eastern Colorado Health Care System GRECC; New England GRECC, VA Boston Healthcare System; Miami VA Healthcare System GRECC; GRECC VA Health Care System Durham, Center for the Study of Aging/Claude D. Pepper Older Americans Independence Center. The views expressed in this paper are not the views of the VHA.
Financial Disclosure:
Gerofit dissemination has been funded by the Veterans Health Affairs Office of Geriatrics and Extended Care Non-Institutional Long Term Care Funding and Mentored Partnership program and the VHA Office of Rural Health. The West Los Angeles Gerofit program has been locally supported by the Greater Los Angeles VA Geriatric, Research, Education and Clinical Program. Dr Katzel, MD, PhD is supported by the Baltimore GRECC and University of Maryland Older Americans Independence Center (P30 AG028747) and Dr. Hall by Funding: RR&D Service (RX003120, Hall, PI).
Sponsor’s Role:
The sponsor had no role in the study design; the collection, analysis, and interpretation of the data; the writing of the report; and the decision to submit the article for publication.
Footnotes
Conflict of Interest: The authors have no conflicts of interest for this article.
REFERENCES
- 1.Kulka RA, Schlenger WA, Fairbanks JA, et al. Trauma and the Vietnam War Generation: Report of Findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel; 1990. [Google Scholar]
- 2.Harada N, Wilkins SS, Schneider B, et al. The influence of depression and PTSD on exercise adherence in older Veterans. Mil Behav Health. 2018;1: 146–151. [Google Scholar]
- 3.Dedert EA, Calhoun PS, Watkins LL, Sherwood A, Beckham JC. Post-traaumatic stress disorder, cardiovascular and metabolic disease: a review of the evidence. Ann Behav Med. 2010;39(1):61–78. 10.1007/s12160-010-9165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farr OM, Sloan DM, Keane TM, Mantzoros CS. Stress and PTSD-associated obesity and metabolic dysfunction: a growing problem requiring further research and novel treatments. Metabolism. 2014;63:1463–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reisman M PTSD treatment for Veterans: What’s working, what’s new, and what’s next. Pharm Therapeut. 2016;41(10):623–627. 632–634. [PMC free article] [PubMed] [Google Scholar]
- 6.Durai C, Chopra MP, Coakley E, et al. Exposure to trauma and post-traumatic stress disorder symptoms in older Veterans attending primary care: comorbid conditions and self-rated health status. J Am Geriatr Soc. 2011; 59(6):1087–1092. [DOI] [PubMed] [Google Scholar]
- 7.Honey Ekkekakis P., I shrunk the pooled SDM! Guide to critical appraisal of systematic reviews and meta-analyses using the Cochran review on exercise for depression as an example. Mental Health Phys Act. 2015;8:21–36. [Google Scholar]
- 8.Stubbs B, Vancampfort D, Rosenbaum S, et al. An examination of the anxiolytic effects of anxiety for people with anxiety and stress disorders: a meta-analysis. Psychiatry Res. 2017;249:102–108. [DOI] [PubMed] [Google Scholar]
- 9.Jayakody K, Gunadasa S, Hosker C. Exercise for anxiety disorders: systematic review. Br J Sports Med. 2014;48(3):187–196. [DOI] [PubMed] [Google Scholar]
- 10.Rosenbaum S, Tiedmann A, Sherrington C, Curtis J, Ward PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry. 2014;75:964–974. [DOI] [PubMed] [Google Scholar]
- 11.Whitworth JW, Exercise CJT. Post-traumatic stress disorder in military Veterans: a systematic review. Mil Med. 2016;9:953–960. [DOI] [PubMed] [Google Scholar]
- 12.Whitworth JW, Craft LL, Dunsiger SI, Ciccolo JT. Direct and indirect effects of exercise on postrumatic stress disorder symptoms: a longitudinal study. Gen Hosp Psychiatry. 2017;49:56–62. [DOI] [PubMed] [Google Scholar]
- 13.Hall KS, Morey MC, Bosworth HB, et al. Pilot randomized controlled trial of exercise training for older Veterans with PTSD. J Behav Med. 2019;43: 648–659. 10.1007/s10865-019-00073-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hornby-Turner YC, Peel NM, Hubbard RE. Health assets in older age: a systematic review. BMJ Open. 2017;7(5):e013226. 10.1136/bmjopen-2016-013226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller KJ, Mesagno C, McLaren S, Grace F, Yates M, Gomez R. Exercise, mood, self-efficacy, and social support as predictors of depressive symptoms in older adults: direct and interaction effects. Front Psychol. 2019;10:2145. 10.3389/fpsyg.2019.02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Price M, Lancaster CL, Gros DF, Legrand AC, van Stolk-Cooke K, Acierno R. An examination of social support and PTSD treatment response during prolonged exposure. Psychiatry. 2018;81(3):258–270. 10.1080/00332747.2017.1402569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morey MC, Lee CC, Castle S, et al. Models of geriatric care, quality improvement, and program dissemination should structured exercise be promoted as a model of care? Dissemination of the Department of Veterans Affairs Gerofit Program. J Am Geriatr Soc. 2018;66(5):1009–1016. 10.1111/jgs.15276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, D.C.: American Psychiatric Association; 2013. [Google Scholar]
- 19.Wilson PM, Rogers WT, Rodgers WM, Wild CT. The psychological need satisfaction in exercise scale. J Sport Exerc Psychol. 2006;28:231–251. [Google Scholar]


