Abstract
Policy Points.
Telehealth has many potential advantages during an infectious disease outbreak such as the COVID‐19 pandemic, and the COVID‐19 pandemic has accelerated the shift to telehealth as a prominent care delivery mode.
Not all health care providers and patients are equally ready to take part in the telehealth revolution, which raises concerns for health equity during and after the COVID‐19 pandemic.
Without proactive efforts to address both patient‐ and provider‐related digital barriers associated with socioeconomic status, the wide‐scale implementation of telehealth amid COVID‐19 may reinforce disparities in health access in already marginalized and underserved communities.
To ensure greater telehealth equity, policy changes should address barriers faced overwhelmingly by marginalized patient populations and those who serve them.
Context
The COVID‐19 pandemic has catalyzed fundamental shifts across the US health care delivery system, including a rapid transition to telehealth. Telehealth has many potential advantages, including maintaining critical access to care while keeping both patients and providers safe from unnecessary exposure to the coronavirus. However, not all health care providers and patients are equally ready to take part in this digital revolution, which raises concerns for health equity during and after the COVID‐19 pandemic.
Methods
The study analyzed data about small primary care practices’ telehealth use and barriers to telehealth use collected from rapid‐response surveys administered by the New York City Department of Health and Mental Hygiene's Bureau of Equitable Health Systems and New York University from mid‐April through mid‐June 2020 as part of the city's efforts to understand how primary care practices were responding to the COVID‐19 pandemic following New York State's stay‐at‐home order on March 22. We focused on small primary care practices because they represent 40% of primary care providers and are disproportionately located in low‐income, minority or immigrant areas that were more severely impacted by COVID‐19. To examine whether telehealth use and barriers differed based on the socioeconomic characteristics of the communities served by these practices, we used the Centers for Disease Control and Prevention Social Vulnerability Index (SVI) to stratify respondents as being in high‐SVI or low‐SVI areas. We then characterized respondents’ telehealth use and barriers to adoption by using means and proportions with 95% confidence intervals. In addition to a primary analysis using pooled data across the five waves of the survey, we performed sensitivity analyses using data from respondents who only took one survey, first wave only, and the last two waves only.
Findings
While all providers rapidly shifted to telehealth, there were differences based on community characteristics in both the primary mode of telehealth used and the types of barriers experienced by providers. Providers in high‐SVI areas were almost twice as likely as providers in low‐SVI areas to use telephones as their primary telehealth modality (41.7% vs 23.8%; P <.001). The opposite was true for video, which was used as the primary telehealth modality by 18.7% of providers in high‐SVI areas and 33.7% of providers in low‐SVI areas (P <0.001). Providers in high‐SVI areas also faced more patient‐related barriers and fewer provider‐related barriers than those in low‐SVI areas.
Conclusions
Between April and June 2020, telehealth became a prominent mode of primary care delivery in New York City. However, the transition to telehealth did not unfold in the same manner across communities. To ensure greater telehealth equity, policy changes should address barriers faced overwhelmingly by marginalized patient populations and those who serve them.
Keywords: Telehealth, telemedicine, health equity
The covid‐19 pandemic has catalyzed fundamental shifts across the US health care delivery system, including a rapid transition to telehealth. Defined as “the use of electronic information and telecommunications technologies to support and promote long‐distance clinical health care, patient and professional health‐related education, public health and health administration,” 1 telehealth is an umbrella term that encompasses a wide range of tools and technologies to facilitate the delivery of care at a distance. Although telehealth has existed for several decades, its uptake had been slow prior to the pandemic, especially among small primary care providers. 2 During the pandemic, the need to avoid in‐person contact accelerated the movement to telehealth, reshaping how and where care is delivered. In March 2020, telehealth claims in the United States were 4,347% higher than in March 2019. 3 Nearly half of all Medicare primary care visits were provided via telehealth in April 2020, representing a 350% increase in visits from pre‐pandemic levels. 4 In total, more than 9 million Medicare beneficiaries received a telehealth service from mid‐March to mid‐June 2020. 5 These striking figures suggest that telehealth may now be a prominent fixture in the US health care landscape that will continue to shape health care delivery and access for the foreseeable future.
Telehealth has many potential advantages during an infectious disease outbreak such as the COVID‐19 pandemic. 6 Telehealth modalities that allow patients to connect with providers remotely, such as telephone, videoconferencing, and patient portals, are particularly beneficial. For patients with suspected COVID‐19, phone or video visits can be used to triage, screen, and monitor their health without the need to physically interact with providers. For the general population, telehealth visits can help maintain continuity of care by preserving the patient‐provider relationship when in‐person visits may not be feasible. Meanwhile, patient portals can reduce administrative burden by allowing patients and providers to schedule appointments, communicate through direct messaging, and complete virtual prescription refills on their own time. Such telehealth capabilities sustain critical access to care while keeping both patients and providers safe from unnecessary exposure to the novel coronavirus—a feature that may be especially beneficial for historically underserved, low‐income communities, which have been disproportionally affected by COVID‐19.
Although the potential benefits of telehealth are clear, much less is known about potential disparities arising from its rapid expansion during a public health emergency when in‐person contact is discouraged. These disparities arise from two forms of digital divide: one among health care providers, and the other among patients.
Historically, health care providers have often experienced a variety of barriers to telehealth implementation, including low reimbursement rates, cost, lack of investment in telecommunications infrastructure, issues with interoperability, the need to redesign workflows to accommodate telehealth, and challenges around time management. 7 , 8 , 9 , 10 Studies of telehealth implementation have also reported technical problems, especially for video visits 11 , 12 , 13 and patient portals. 10 Earlier research on telehealth adoption found that that while telephone services were widely available, video visits and patient portals were not broadly integrated into existing clinical care. 14 , 15 , 16 This was especially the case for small primary care practices, which had been among the slowest to use telehealth in routine practice before the pandemic. 2 , 17
Further, the changes required to implement new telehealth initiatives in response to COVID‐19 increased operating costs in a way that was particularly onerous for small primary care practices. 18 Unlike larger groups that can benefit from economies of scale by distributing the costs of practice transformation across clinicians, small practices have limited capacity to absorb the infrastructure, workflow, logistics, and training‐related costs associated with adopting new modes of care delivery. 18 Because small practices have typically lacked the technological infrastructure, financial and personnel resources, or prior experience to implement the full range of telehealth capabilities, they have faced a digital divide separating them from larger, well‐established health systems with a developed capacity and tools to deliver care remotely through multiple modalities. 8 As a result, the actual uptake and integration of telehealth into mainstream medical practice, and especially small primary care practices, was fragmented and slow before the pandemic, and many pilot programs had not advanced into sustained services. 6
For patients, the digital divide can manifest as limited digital access or limited digital literacy. Like other health disparities, these barriers are borne disproportionately by socioeconomically and medically disadvantaged patient populations. More than a third of US households headed by a person age 65 years or older do not have access to a computer, and more than half do not have a smartphone. 19 Children in low‐income households are substantially less likely to have access to a computer compared to wealthier classmates, as are Black or Hispanic children compared to white peers. 20 Studies have found that older adults, low‐income patients, less‐educated patients, and those with chronic conditions are less likely to use video‐enabled telehealth, even when given the option. 21 , 22 Prior to the COVID‐19 pandemic, patients with poorer self‐reported health, older age, and lower income were also less likely to express an interest in communicating about their care using patient portals. 23
Taken together, these findings suggest that not all health care providers and patients are equally ready to take part in the digital revolution, which raises important questions about potential disparities in health care access during and after the COVID‐19 pandemic. Early in the pandemic, policymakers and insurers introduced several measures to broaden access to telehealth during public health emergency, including relaxing privacy regulations, increasing reimbursement, and expanding coverage for services. 24 These efforts rapidly expanded and encouraged telehealth capabilities, including among small practices that previously had little or no experience delivering care virtually. Little is known about potential disparities arising from this rapid expansion, as most published studies examining disparities in access to and use of telehealth services were conducted prior to the onset of COVID‐19 and corresponding changes to policy. Furthermore, while remote visits have long been used in rural and specialty consultation settings and large health systems, evidence on telehealth visits used in small primary care setting before the pandemic was limited. 25 , 26 Therefore, there is a need to evaluate differences in telehealth adoption and barriers faced by small primary care providers and the communities they serve in the context of COVID‐19.
The aims of this study are to examine differences in telehealth use and barriers to adoption among primary care practices and how those differences are influenced by the socioeconomic characteristics of their communities. This study focuses on small primary care practices, which play an important role in the US health care delivery system. Nationally, these practices have the highest percentage of physicians providing care in Spanish and other non‐English languages among primary care practices and represent a key point of access for underserved communities. 27 In New York City, small primary care practices represent 40% of primary care providers 18 and are disproportionately located in low‐income, minority or immigrant areas that were more severely impacted by COVID‐19. 27 , 28 Examining the response of small primary care practices in New York City, the early epicenter of the US pandemic, can provide a preliminary understanding of health disparities related to the accelerated shift to telehealth, and inform policies regarding the use and reimbursement of telehealth services during the COVID‐19 pandemic and beyond.
Data and Measures
Data Collection
This study uses data from five waves of rapid‐response surveys administered by the New York City Department of Health and Mental Hygiene's Bureau of Equitable Health Systems (BEHS) and New York University (NYU) as part of the city's efforts to understand how primary care practices were responding to the COVID‐19 pandemic following New York State's stay‐at‐home order on March 22, 2020. BEHS operates a federally and state‐funded program designed to help small primary care providers adopt and implement health information systems, quality improvement, and practice transformation initiatives in New York City.
Survey questions were developed jointly by representatives at BEHS and researchers at NYU and included both closed‐ and open‐text questions regarding COVID‐related stressors, closures, support needs, and telehealth adoption. Data collection and analysis were participatory and iterative: following each wave of data collection, BEHS representatives and NYU researchers discussed findings and updated the survey instrument in response to findings and changes at the national or state level related to the pandemic. The primary purposes of the data collected were to support BEHS's efforts to understand the needs of primary care practices during the pandemic and to identify topics for a weekly public health emergency webinar series that offered practices information on a range of COVID‐19‐related issues, including telehealth. Survey instruments are available at https://nyu.app.box.com/s/jnycpaw8nr1tmattg522sd2mjoa52t3l.
The first survey wave was launched on April 10, 2020, and new waves were administered every other week until June 18, 2020, for a total of five waves of data collection. At the beginning of each wave, a BEHS representative sent an invitation to an internal LISTSERV of 5,418 primary care providers to participate in the survey via email. After excluding providers who expressed their unwillingness to participate in the survey, an average of 5,372 providers were contacted across the five waves. Wave I had 491 responses, wave II had 199, wave III had 123, wave IV had 154, and wave V had 133. Of the 1,100 total responses, 58 within‐wave duplicate responses and 124 responses missing zip codes were removed, resulting in 918 total pooled responses and 493 responses from those who took only one survey.
Measures
Telehealth Use and Modality
The survey asked providers about their use of three commonly used telehealth modalities: video, telephone, and patient portal. Providers were asked to select the proportion of care delivered by each modality in quartiles (0%, 1%‐25%, 26%‐50%, 51%‐75%, 76%‐100%). The survey also asked about the delivery of in‐person or home‐based care. Respondents who indicated that they were providing 51% or more of their care with any one or a combination of the three telehealth modalities were defined as providing a majority of their services through telehealth.
Telehealth Barriers
Providers were asked to select from a list of six practice‐related and five patient‐related barriers to telehealth use. Practice‐related barriers were provider discomfort, staff discomfort, concerns about the quality of care, being unable to deliver care remotely, insufficient reimbursement, and uncertainty around reimbursements. Patient‐related barriers were patient discomfort, language barriers, lack of access to the internet or appropriate devices, low use or uptake of telehealth, and patients not being forthcoming. Items about staff discomfort and patients not being forthcoming were removed in wave III following discussions with BEHS because of their low recurrence among respondents and in an effort to keep the survey short. Questions about the certainty and level of reimbursement were added in wave II after examining open‐text responses. All other items were included across all five waves.
Vulnerability
To examine whether respondents differed based on the socioeconomic characteristics of their communities, we linked the data set to the Centers for Disease Control and Prevention (CDC) Social Vulnerability Index (SVI). Social vulnerability is defined in terms of the characteristics of a person or group that affect “their capacity to anticipate, cope with, resist, and recover from the impact” of a discrete and identifiable disaster in nature or society. 29 The CDC developed the SVI to identify and map at‐risk communities that will most likely need support before, during, and after “natural or human caused disasters or disease outbreaks.” 30 The index uses 15 US variables from the American Community Survey, including poverty, unemployment, income, education, percent elderly, percent under 17, civilian with a disability, single‐parent households, minority status, language, lack of vehicle access, crowding, group quarters, multi‐unit structures, and mobile homes. 31 , 32 The composite SVI score is continuous, ranging from 0 to 1, with 1 indicating communities at highest risk and in need of greatest support. We categorized clinics as being in “high” risk areas if they were in an area that scored 0.75 or higher in the index, and “low” risk otherwise. Because the SVI score is coded at the census‐tract level and the survey collected zip code–level information, we used the US Department of Housing and Urban Development's zip code‐to‐census tract crosswalk to assign a primary census tract to each provider zip code. Less than half of the clinics (n = 408; 44.4%) in the sample were categorized as practicing in high‐SVI areas, and the remaining practices were in low‐SVI areas (n = 510; 55.6%).
Practice Characteristics
Three measures of practice characteristics were included in the survey: the size of practice (total number of providers), clinic ownership (privately owned, part of a health system, or part of a physician organization), and respondent role (clinician or administrator).
Analytic Approach
We characterized telehealth use and barriers to adoption by using means and proportions with 95% confidence intervals. We tracked telehealth use over time by plotting the percentage of respondents who indicated that they provided the majority of health care using a combination of the three telehealth platforms (video, telephone, and patient portal) as well as each of the telehealth platforms individually across the five survey waves. We used χ2 tests to compare responses between practices in high‐ and low‐SVI areas. Significance was set at 2‐sided P = .05. To examine the primary modality of telehealth delivery and telehealth barriers, we pooled data across the five waves. For sensitivity analysis, we repeated the findings using data from respondents who only took one survey, first wave only, and the last two waves only. We excluded survey responses with missing data for a given variable. Data analysis was conducted using Stata SE 16.1.
Findings
Practice Characteristics
BEHS operates a federally and state‐funded program designed to help small primary care providers adopt and implement technology, so small practices were overrepresented in the survey. Most respondents (70.7%) worked in small practices with fewer than four full‐time providers. In comparison, an internal analysis by the city health department suggests 40% of New York City primary care providers work in practices of a similar size. 18
The size and ownership type of the practices included in the surveys were fairly consistent across waves. Most respondents were from practices with one to three providers (ranging from 61% in wave I to 82% in wave IV), and most were from privately owned practices (ranging from 74% in wave IV to 92% in wave III). Most respondents were clinicians (ranging from 78% in wave III to 88% in wave IV) rather than administrators. Appendix Table A provides more details on respondent characteristics by wave.
Use of Telehealth Over Time
Table 1 and Figure 1 show the levels of telehealth services provided as reported by respondents in survey waves I through V. In wave I, fielded April 10‐23, 2020, during the peak of the pandemic in New York City, 33 71.3% percent of providers reported they were delivering most of their care through telehealth, the highest level of telehealth use reported during data collection. Telephone was the most used modality, with 40.6% of respondents reporting that more than half of the health services they provided were via telephone. In the same wave, one‐third (33.3%) of providers indicated they delivered most patient care via video, and 10.5% used a patient portal for most services. The overall use of telehealth for service delivery declined over time, dropping to 40.3% of providers by wave V. Reported use of all three types of telehealth services among the providers decreased across the waves, with the biggest drop occurring in telephone visits. This decrease corresponded with an increase in in‐person visits over time as the city slowly began reopening as COVID‐19 infection rates decreased.
Table 1.
Percentage of Providers Who Indicated Delivering Most (>50%) Patient Care Using a Specific Mode of Care a
| Care Modality | Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 |
|---|---|---|---|---|---|
| Video | 33.3% | 24.6% | 23.5% | 25.0% | 16.1% |
| Telephone | 40.6% | 35.6% | 27.6% | 18.8% | 13.9% |
| Patient portal | 10.5% | 9.0% | 3.2% | 3.2% | 2.7% |
| In person | 9.0% | 12.3% | 10.3% | 22.0% | 26.9% |
Providers were asked to select the proportion of care delivered by each modality in quartiles (0%, 1%‐25%, 26%‐50%, 51%‐75%, 76%‐100%). Percentages per wave do not add up to 100% because some providers did not rely on one dominant modality but instead delivered care using a proportionate mix of modalities.
Figure 1.
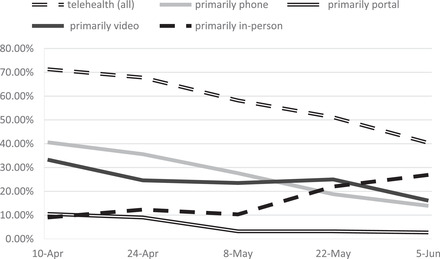
Primary mode of care delivery over timea
aCurves represent the percentage of providers who indicated delivering most (>50%) patient care using a specific mode of care (video, phone, portal, in person). Providers were asked to select the proportion of care delivered by each modality in quartiles (0%, 1%‐25%, 26%‐50%, 51%‐75%, 76%‐100%). Respondents who indicated that they provided 51% or more of care with any one or a combination of the three telehealth modalities were defined as providing most of their services through telehealth (all). Percentages per wave do not add up to 100% because some providers did not rely on one dominant modality but instead delivered care using a proportionate mix of modalities.
Primary Mode of Telehealth Delivery and Social Vulnerability
The level of overall telehealth service provision did not differ significantly by social vulnerability of the community. Across the five survey waves, 62.2% of providers indicated that most of their services were provided through telehealth, including 64.7% of providers in high‐SVI areas and 60.2% of providers in low‐SVI areas. However, significant differences emerged when we examined each telehealth modality by social vulnerability (see Figure 2). In high‐SVI areas, 41.7% of providers delivered most patient care through telephone services, as compared with 23.8% of providers in low‐SVI areas (P <.001). The opposite was true for telehealth through video: 18.7% of providers in high‐SVI areas used it for most patient care vs 33.7% of providers in low‐SVI areas (P <.001). There was no significant difference between providers in high‐SVI and low‐SVI areas for telehealth through patient portal (5.8% vs 8.5%). Similar relationships were found in sensitivity analysis using data from respondents who only took one survey, participated in wave I only, or participated in the last two waves.
Figure 2.
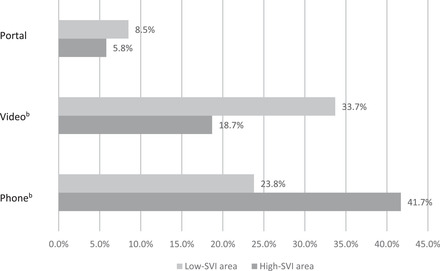
Primary mode of telehealth delivery by community characteristicsa
aBivariate analysis of the relationship between practice location's Social Vulnerability Index (SVI; high vs low) and the primary mode of telehealth used to deliver care across waves. Percentages do not add up to 100% because some providers did not rely on one dominant modality but instead delivered care using a proportionate mix of modalities.
b P <.001.
Practice–Related Barriers to Telehealth Adoption
Overall, out of the 11 barriers included in the surveys, providers in high‐SVI areas reported a slightly higher number of telehealth barriers than those in low‐SVI areas (2.94 vs 2.67; P <.05). However, more striking differences emerged when we stratified the barriers to telehealth adoption as either practice‐related or patient‐related. Providers in high‐SVI areas reported fewer provider‐related barriers than counterparts in low‐SVI areas (1.273 vs 1.457; P <.05). These differences were driven largely by a marked gap in the perception that the quality of care through telehealth is inferior to in‐person care: Whereas 58% of providers in low‐SVI areas reported this concern about quality, 46% of providers in high‐SVI areas identified this issue as a barrier to telehealth adoption. Providers in low‐SVI areas were also more likely than counterparts in high‐SVI areas to perceive the appropriateness of care being delivered by phone or video as an issue (31.4% vs 26.0%), though the difference was not statistically significant (see Figure 3).
Figure 3.
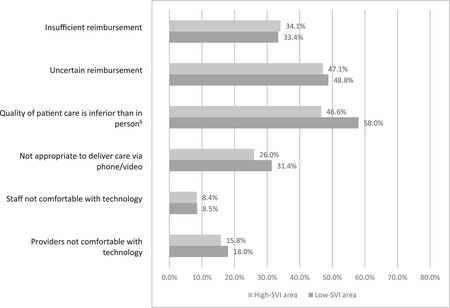
Practice‐related telehealth barriersa
aBivariate analysis of the relationship between practice location's Social Vulnerability Index (SVI; high vs low) and practice‐related telehealth barriers across waves. Providers were asked to select key barriers to using telehealth.
b P <.001.
Concerns around reimbursements were highly relevant to providers in both high‐ and low‐SVI areas: About half of respondents (48.8% in low‐SVI areas vs 47.1% in high‐SVI areas) reported that uncertain reimbursements were a barrier to telehealth implementation. About a third of respondents (33.4% in low‐SVI areas vs 34.1% for high‐SVI areas) identified insufficient reimbursements to be a barrier. These results suggest that across the board, the uncertainties about reimbursements were a bigger concern than low reimbursements.
Finally, compared to other provider‐related barriers, staff or provider discomfort with technology did not appear to be a salient issue for providers in low‐ or high‐SVI areas.
Patient‐Related Barriers to Telehealth Adoption
Providers in high‐SVI areas were significantly more likely to experience all five of the patient‐related telehealth barriers included in the surveys (see Figure 4). The biggest difference between high‐ and low‐SVI areas was patient access to reliable internet or an appropriate device: 70.4% of providers in high‐SVI areas indicated this was a barrier, compared to 52.5% of providers in low‐SVI areas (P <.001). Other barriers reported more by providers in high‐SVI areas than those in low‐SVI areas were low uptake or use of the patient portal (37.9% vs 25.5%; P <.001), and patients not feeling comfortable with technology (52.7% vs 45.1%; P <.05). Providers in high‐SVI areas were also twice as likely to report language barriers as a concern (15.2% vs 7.3%; P <.001).
Figure 4.

Patient‐related telehealth barriersa
aBivariate analysis of the relationship between practice location's Social Vulnerability Index (SVI; high vs low) and patient‐related telehealth barriers across waves. Providers were asked to select key barriers to using telehealth.
b P <.05.
c P <.01.
d P <.001.
In total, providers in high‐SVI areas reported a significantly higher number of patient‐related barriers than counterparts in low‐SVI areas (1.67 vs 1.22; P <.001). Sensitivity analysis resulted in similar findings.
Discussion
A burgeoning body of evidence suggests that virtual visits between clinicians and patients are technically possible and increasingly acceptable as an alternative to in‐person visits. 12 , 34 Previous research indicates that compared to face‐to‐face visits, telephone visits reduce practice workload 35 and result in similar patient satisfaction and safety outcomes, 36 whereas the use of videoconferencing has a positive impact on both patient 38 , 39 and provider 40 satisfaction and enhances communication 38 and engagement between health care providers and patients. 12 Two benefits of particular importance for both video and telephone visits are reduced wait times and reduced costs related to travel. 12 , 38 , 39
However, when it comes to equity in access, telehealth presents a double‐edged sword. On the one hand, telehealth visits can increase access to both primary and specialty care by removing barriers such as distance or transportation costs. 38 , 41 On the other hand, socioeconomically and medically vulnerable populations that could stand to benefit most from telehealth may be the least ready to use it, which raises questions around potential disparities in access to care arising from the widespread use of telehealth. 21 , 22 In a systematic review of the use of patient portals, Mold and colleagues found that while telehealth tools may improve aspects of care delivery, concerns around disparities in access remained a key concern. 10 Similarly, in a systematic review of the use of video consultations in primary care, Thiyagarajan and colleagues concluded that while convenience and access are key benefits for patients, “these benefits may not be afforded to all patients” because of disparities in use. 39 Findings from our study contribute to this growing literature examining the role of telehealth and virtual visits on health access and equity.
This study investigated the use of telehealth among primary care practices during the COVID‐19 pandemic and its potential implications for health access and equity. We found that overall, telehealth (video, phone, and portal) was used at high rates among primary care practices in New York City from April 10 to June 18, 2020. At the peak of the pandemic during that period, almost three‐quarters of the primary care practices participating in our surveys were providing most of their services through phone, video, and portal modalities. Although reliance on telehealth dropped as in‐person visits increased over time, the high rates of telehealth use in New York City were consistent with the growth trends for telehealth at the state, regional, and national levels, indicating a rapid transition to telehealth during the initial months of the COVID‐19 pandemic. 3
A more nuanced analysis including community‐level socioeconomic characteristics reveals a digital divide between practices located in areas ranking high on the SVI compared to those practicing in low‐SVI areas. Two findings are salient. First, providers in high‐SVI areas were nearly twice as likely than counterparts in low‐SVI communities to rely on telephone as their primary mode of telehealth delivery and only half as likely to rely on video‐based telehealth services. These results suggest that the transition to telehealth did not unfold in the same manner across communities.
Our findings align with recent experiences reported by large safety net providers during the COVID‐19 pandemic. For example, Cambridge Health Alliance, a large public health care system in Massachusetts, reported that only 1% of primary care telehealth visits took place via video in the first week of June 2020. 41 Similarly, NYC Health + Hospitals, the largest safety net hospital system in the United States, reported that telephone visits were the most scalable modality because of their ease of use for both patients and providers and that video visits were more challenging and often required in‐person or virtual navigators to facilitate. 42
Second, although respondents from practices in high‐SVI areas reported more telehealth barriers overall, they experienced fewer practice‐related barriers to telehealth use and were equally likely to be comfortable with technology as providers in low‐SVI communities. In fact, respondents representing practices in high‐SVI areas were less likely to perceive quality of care or appropriateness of care as a point of concern, suggesting that providers in high‐SVI communities were equally, if not more, willing to pivot to telehealth. Yet, these providers were significantly more likely to report a multitude of patient‐related barriers, including patient discomfort with technology and language barriers. Helping patients overcome these barriers and adjust to new telehealth tools requires a substantial investment of effort and time, 40 and our findings suggest this burden was borne unequally by providers serving patients in high‐SVI areas.
The findings about patient‐ and practice‐related barriers to telehealth use are closely intertwined. Practices located in high‐SVI areas are more likely to serve populations with low socioeconomic status, older patients, and populations with low English‐language proficiency. 29 These findings align with previous research that suggests low‐income patients, 43 , 44 , 45 older patients, 46 , 47 , 48 or those with less education, 49 , 50 may be even less comfortable with, or unable to access, telehealth platforms with a visual interface. For example, video visits require access to high‐speed internet as well as a tablet, personal computer, or smartphone—all of which may be out of reach for economically marginalized patients. As one primary care provider noted in an open‐ended response to the survey, “For most elderly and low‐income patients, they can only afford telephonic service, without video. To require video is to deny them telehealth access.”
At the same time, providers who work in socially vulnerable areas typically face severe economic constraints and often operate with very narrow operating margins. 51 With fewer resources available to shore up the technological infrastructure required for more advanced telehealth technologies, these providers may have no choice but to rely on the telephone to continue providing care for their patients while maintaining social distancing.
In 2020, primary care practices faced a projected $15 billion revenue loss due to COVID‐19, 52 with some practices closing permanently as a result. Telehealth is an important tool that could help mitigate some of these losses and ensure access to care during the COVID‐19 pandemic and beyond. Yet, findings from our study imply that telehealth, like many other services in health care, is not distributed equally. Neighborhoods with historical divestment that makes the population more susceptible to disasters and communicable diseases also face a digital divide that shapes their ability to take full advantage of telehealth capabilities. It is therefore essential that policymakers ensure that the leap toward telehealth occurs with greater equity by taking into consideration the barriers faced overwhelmingly by vulnerable patient populations and those who serve them.
In 2020, the US Department of Health and Human Services (HHS) 53 and the Centers for Medicare and Medicaid Services (CMS) 54 enacted sweeping changes to telehealth policies in response to COVID‐19. These measures included lifting geographic and originating‐site restrictions so patients and providers can use telehealth from any location, allowing the use of technologies that do not comply with Health Insurance Portability and Accountability Act requirements, expanding the types of covered services that can be provided remotely, and enhancing reimbursement of phone‐only telehealth to match reimbursement for video and in‐person visits. These waivers and reimbursements provided a source of much needed revenue for providers across the country 55 while increasing access to care for patients during the pandemic. However, these waivers were set to expire at the end of the public health emergency declaration, which means long‐term support for and sustainability of telehealth use is uncertain.
Policy Implications
Our findings support three policy recommendations. First, CMS and state Medicaid programs should extend temporary waivers for telehealth beyond the end of the public health emergency declaration. Our study finds that reimbursement for telehealth is a salient topic for all primary care providers, and uncertainties surrounding reimbursements are a bigger barrier to telehealth than insufficient reimbursements. As one respondent said, “Primary care is extremely challenging with the constant change in protocols, the uncertainty, and enormously confusing insurance schemes.” The lack of clarity about the reversion to pre‐pandemic reimbursement levels can create a kind of limbo for providers and may deter many from investing in resources to buttress their current telehealth capabilities.
Second, insurers should consider reimbursing telephonic visits on par with video visits. Although research comparing telehealth modalities are rare, one study suggests that telephone and video encounters are similar in terms of consultation length, content, and quality. 56 Other studies find that videoconferencing may be superior to telephonic care because the clinician's ability to visibly see patients can provide useful clinical context or help build rapport and reassurance, improving patient‐provider communication. 12 , 56 , 57 , 58 However, technical problems and disparities in use are also more common with videoconferencing than with phone encounters. 11 , 12 , 56 In a study comparing face‐to‐face, video, and telephonic primary care visits in the United Kingdom, Hammersley and colleagues found that older patients and individuals with lower digital literacy were less likely to use videoconferencing. 56 Similarly, in a randomized controlled pilot trial of a smoking cessation intervention among women living with HIV, 11 a video call intervention was almost 30% less feasible than a voice call intervention because women who were older or earned less income did not have access to video call equipment. Moreover, one recent study examining patient choice between an office, video, or telephone visit found that many patients preferred to use phone‐ rather than video‐enabled care, 25 suggesting that both modalities play roles in health care access.
Although CMS increased Medicare reimbursements for both telephone and video visits to match payments for in‐person visits, many Medicaid programs, fully insured plans, and self‐insured plans did not follow suit. 59 The failure to provide payment parity for both telehealth modalities may disincentivize providers from offering telephonic services and could potentially reduce access to and usage of care for patients who do not have video‐enabled devices or sufficient technological literacy. As one respondent in our surveys noted, a key barrier to adopting telehealth was “insurance companies not reimbursing telephone visits at a rate that supports the level of work done on a telephone visit.” Prior to the COVID‐19 pandemic, few states permitted audio‐only care to qualify as a reimbursable telehealth service. 60 Some states, including New York, expanded Medicaid reimbursement criteria for telehealth to include some, though not all, telephonic evaluations during the state of emergency due to COVID‐19. 61 The expanded coverage of telephonic services in the New York State Medicaid program may partly explain the heavy reliance on telephone services among high‐SVI areas found in our study. However, like other provisions enacted during the emergency declaration, telephonic service coverage and reimbursements may revert to pre‐pandemic levels when the emergency ends. Without continued equitable payment support and given their higher reliance on telephone‐enabled care, providers serving the high‐SVI communities will likely be most susceptible to closures, which may further exacerbate health care inequities. Equitable reimbursements for both telephone and video telehealth modalities would provide much‐needed flexibility for patients and providers as they navigate the many uncertainties of a post‐pandemic future.
Third, policymakers should consider developing targeted payment mechanisms to reimburse providers for helping patients adapt to video‐enabled telehealth. Part of the solution involves expanding broadband access to the approximately 24 million people in the United States who live in “digital deserts,” 62 and subsidizing access to the internet as well as devices, such as mobile phones, laptops, and tablets. However, successful use of video‐enabled health requires more than stable internet connectivity and appropriate hardware. In our surveys, more than half of the providers in high‐SVI areas reported patient discomfort with technology as a significant barrier to telehealth use. Onboarding patients to telehealth platforms for the first time is a challenging and time‐consuming endeavor, 42 which may require in‐person or virtual navigators to facilitate. As one respondent noted, “I am more stressed out doing telehealth, as we spend time to fix internet, video, and voice. There are calling issues, so it's more time consuming.” A separate billing code for telehealth training and management can help reduce the administrative burden on health care providers and further expand video‐enabled telehealth use among patients unfamiliar with the technology.
Limitations
Our study is subject to several limitations. First, this study uses a convenience sample of primary care practices included in the BEHS LISTSERV. Given the primary mission of BEHS to assist small, independent primary care practices to adopt new technologies, the data may overrepresent smaller practices who need such help. For example, 70.7% of our survey respondents worked in small practices with fewer than five full time providers. In comparison, 40% of primary care physicians in New York City are estimated to work in small practices. 18 This, combined with the low survey response rates during the pandemic, implies that the data may not be representative of the entire population of primary care providers in the city. However, this concern is tempered by the focus of our paper on comparing telehealth access and use between providers in high‐ and low‐SVI areas rather than describing the experience of all primary care practices in general.
Second, though the SVI considers multiple socioeconomic factors, classifying communities based on a single index creates a blunt measure of vulnerability. Third, by pooling data across waves, the analytic sample may also overrepresent respondents who completed the survey multiple times across waves. We addressed some of these limitations by running sensitivity analyses on the respondents who only took one survey, those who participated in the first wave only, as well as respondents in the final two waves, and these analyses resulted in similar findings.
Fourth, the survey was administered during the peak of the COVID‐19 pandemic in the city and was kept short (under 5 minutes) to reduce the burden on providers. As a result, the survey failed to include many relevant variables, including demographic information about the providers and patients, prior use of telehealth by modality, and the total number of patients served. Including this information could have strengthened the analysis.
Finally, we asked providers to report their perceptions of patient barriers such as access to internet and did not measure these barriers directly. This approach limited our ability to assess barriers from the patient's perspective.
Despite the limitations, our study adds to the growing evidence base surrounding the potential disparities arising from the use of telehealth and virtual visits. Although telehealth existed prior to the COVID‐19 pandemic, regulatory barriers and low reimbursement rates restricted its widespread use, particularly among small primary care practices. As a result, research on telehealth use in community‐based primary care settings was limited. 25 , 26 To our knowledge, no prior research has been conducted to compare the use of phone and video visits among community‐based primary care practices based on the characteristics of their communities. Furthermore, our study is the first to apply the SVI, a standardized measure created to track community need specifically during public health emergencies, such as the COVID‐19 pandemic, to examine differential adoption and barriers to telehealth use among small primary care providers. As primary care providers continue to gain experience with telehealth, ongoing research will be needed to examine the factors that may affect adoption by both patients and providers as well as quality and clinical outcomes associated with telehealth visits and implementation.
Conclusion
The rapid changes in regulation around telehealth coupled with increases in reimbursements accelerated the shift to telehealth as a prominent mode of care delivery. Telehealth holds great potential to improve both the convenience and experience of care by letting patients connect with providers from the comforts of home. It can also help maintain continuity of care by helping preserve the patient‐provider relationship when in‐person visits may not be feasible. These features may be especially beneficial for historically underserved, low‐income communities disproportionally affected by COVID‐19. As a result, some researchers and policymakers have heralded telehealth as a “virtually perfect” solution to the current pandemic. 63 However, not all patients and providers may be equally ready to fully participate in the telehealth revolution. Without proactive efforts to address both patient‐ and provider‐related digital barriers, the widescale implementation of telehealth during the COVID‐19 pandemic may reinforce disparities in health access in communities that stand to benefit most from its use.
Funding/Support: None.
Conflict of Interest Disclosures: All authors have completed the ICMJE form for potential conflicts of interest. No conflicts were reported.
Acknowledgements: We acknowledge the help of our partners at the Bureau of Equitable Health Systems in the New York City Department of Health and Mental Hygiene, including Hang Pham‐Singer, Winfred Wu, Caroline Peterson, Lily Glenn, Matthew Krco, Samantha De Leon, and Sonali Das. These individuals helped with survey design, data collection, and manuscript editing.
Table A. Respondent Characteristics
| Pooled Sample (N = 918) | Single Respondents (n = 493) | Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | |
|---|---|---|---|---|---|---|---|
| Practice Size | |||||||
| 1‐3 providers | 612 (66.89%) | 339 (69.04%) | 247 (60.84%) | 128 (73.56%) | 79 (82.29%) | 81 (62.31%) | 77 (70.64%) |
| 4‐9 providers | 164 (17.92%) | 86 (17.52%) | 77 (18.97%) | 30 (17.24%) | 14 (14.58%) | 28 (21.54%) | 15 (13.76%) |
| ≥10 providers | 139 (15.19%) | 66 (13.44%) | 82 (20.20%) | 16 (9.20%) | 3 (3.13%) | 21 (16.15%) | 17 (15.60%) |
| Clinic Ownership | |||||||
| Privately owned | 721 (81.84%) | 396 (83.54%) | 307 (79.53%) | 153 (88.44%) | 85 (92.39%) | 92 (74.19%) | 84 (79.25%) |
| Part of health system | 160 (18.16%) | 78 (16.46%) | 79 (20.47%) | 20 (11.56%) | 7 (7.61%) | 32 (25.81%) | 22 (20.75%) |
| Respondent Type | |||||||
| Clinician | 761 (82.99%) | 399 (81.10%) | 329 (81.03%) | 148 (84.09%) | 75 (78.13%) | 114 (87.69%) | 95 (87.16%) |
| Administrator | 156 (17.01%) | 93 (18.90%) | 77 (18.97%) | 28 (15.91%) | 21 (21.88%) | 16 (12.31%) | 14 (12.84%) |
Totals for each subparts of columns 1 and 2 do not equal to N and n because we are not reporting non‐respondents.
References
- 1. Health Resources and Services Administration . Telehealth Programs 2019. https://www.hrsa.gov/rural-health/telehealth. Updated August 2019. Accessed April 20, 2021.
- 2. Kane CK, Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Affairs. 2018;37(12):1923‐1930. [DOI] [PubMed] [Google Scholar]
- 3. Gelburd R. Examining the state of telehealth during the COVID‐19 pandemic. United Hospital Fund. https://uhfnyc.org/publications/publication/telehealth-during-covid-19. Published June 29, 2020. Accessed April 20, 2021.
- 4. Verma S. Early impact of CMS expansion of Medicare telehealth during COVID‐19. Health Affairs Blog. July 15, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/. Accessed April 7, 2021.
- 5. Verma S. Early impact of CMS expansion of Medicare telehealth during COVID‐19. Health Affairs Blog. July 15, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full. Accessed April 20, 2021.
- 6. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID‐19). J Telemed Telecare. 2020;26(5):309‐313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Weigel G, Ramaswamy A, Sobel L, Salganicoff A, Cubanski J, Freed M. Opportunities and barriers for telemedicine in the US during the COVID‐19 emergency and beyond. Kaiser Family Foundation: Women's Health Policy. https://www.kff.org/womens-health-policy/issue-brief/opportunities-and-barriers-for-telemedicine-in-the-u-s-during-the-covid-19-emergency-and-beyond. Published May 11, 2020. Accessed April 20, 2021.
- 9. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID‐19). J Telemed Telecare. 2020;26(5):309‐313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mold F, Hendy J, Lai Y‐L, de Lusignan S. Electronic consultation in primary care between providers and patients: systematic review. JMIR medical informatics. 2019;7(4):e13042. 10.2196/13042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim SS, Darwish S, Lee SA, Sprague C, DeMarco RF. A randomized controlled pilot trial of a smoking cessation intervention for US women living with HIV: telephone‐based video call vs voice call. Int J Womens Health. 2018;10:545‐555. 10.2147/IJWH.S172669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Donaghy E, Atherton H, Hammersley V, et al. Acceptability, benefits, and challenges of video consulting: a qualitative study in primary care. Br J Gen Pract. 2019;69(686):e586‐e594. 10.3399/bjgp19X704141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hammersley V, Donaghy E, Parker R, et al. Comparing the content and quality of video, telephone, and face‐to‐face consultations: a non‐randomised, quasi‐experimental, exploratory study in UK primary care. Br J Gen Pract. 2019;69(686):e595‐e604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hanna L, May C, Fairhurst K. Non‐face‐to‐face consultations and communications in primary care: the role and perspective of general practice managers in Scotland. Inform Prim Care. 2011;19(1):17‐24. https://doi.org/10.14236/jhi.v19i1.789 [DOI] [PubMed] [Google Scholar]
- 15. Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377(16):1585‐1592. 10.1056/NEJMsr1503323 [DOI] [PubMed] [Google Scholar]
- 16. Harvey JB, Valenta S, Simpson K, Lyles M, McElligott J. Utilization of outpatient telehealth services in parity and nonparity states 2010–2015. Telemed J E Health. 2019;25(2):132‐136. 10.1089/tmj.2017.0265 [DOI] [PubMed] [Google Scholar]
- 17. Petterson S, McNellis R, Klink K, Meyers D, Bazemore A. The state of primary care in the United States: a chartbook of facts and statistics. Robert Graham Center. https://www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/PrimaryCareChartbook.pdf. Published January 2018. Accessed April 20, 2021.
- 18. NYC Population Health Improvement Project , United Hospital Fund. The PHIP Small Practice Project: final report. https://www1.nyc.gov/assets/doh/downloads/pdf/public/phip-report2018.pdf. Published June 2018. Accessed April 20, 2021.
- 19. Ryan CL, Lewis JM. Computer and internet use in the United States: 2015. US Census Bureau report no. ACS‐37. https://www.census.gov/library/publications/2017/acs/acs-37.html. Published September 11, 2017. Accessed April 20, 2021.
- 20. Trends Child. Home computer access and internet use. https://www.childtrends.org/indicators/home-computer-access. Published 2018. Accessed April 20, 2021.
- 21. Reiners F, Sturm J, Bouw LJW, Wouters EJM. Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int J Environ Res Public Health. 2019;16(4):645. https://doi.org/10.3390/ijerph16040645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375(2):154‐161. [DOI] [PubMed] [Google Scholar]
- 23. Denberg TD, Ross SE, Steiner JF. Patient acceptance of a novel preventive care delivery system. Prevent Med. 2007;44(6):543‐546. [DOI] [PubMed] [Google Scholar]
- 24. Centers for Medicare and Medicaid Services . Medicare telemedicine health care provider fact sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Published March 17, 2020. Accessed February 23, 2021.
- 25. Reed ME, Huang J, Graetz I, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. 2020;3(6):e205873. Published June 1, 2020. 10.1001/jamanetworkopen.2020.5873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Car J, Koh GC‐H, Foong PS, Wang CJ. Video consultations in primary and specialist care during the COVID‐19 pandemic and beyond. BMJ. 2020;371:m3945. 10.1136/bmj.m3945 [DOI] [PubMed] [Google Scholar]
- 27. Pathman DE, Konrad TR, Dann R, Koch G. Retention of primary care physicians in rural health professional shortage areas. Am J Public Health. 2004;94(10):1723‐1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Calderón‐Larrañaga A, Dekhtyar S, Vetrano DL, Bellander T, Fratiglioni L. COVID‐19: risk accumulation among biologically and socially vulnerable older populations. Ageing Res Rev. 2020;63:101149. 10.1016/j.arr.2020.101149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chen J, Wilkinson D, Richardson RB, Waruszynski B. Issues, considerations and recommendations on emergency preparedness for vulnerable population groups. Radiat Prot Dosimetry. 2009;134(3‐4):132‐135. 10.1093/rpd/ncp083 [DOI] [PubMed] [Google Scholar]
- 30. Centers for Disease Control and Prevention . Planning for an emergency: strategies for identifying and engaging at‐risk groups. a guidance document for emergency managers. https://www.cdc.gov/nceh/hsb/disaster/atriskguidance.pdf. Published 2015. Accessed April 20, 2021.
- 31. Flanagan BE, Hallisey EJ, Adams E, Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the Centers for Disease Control and Prevention's Social Vulnerability Index. J Environ Health. 2018;80(10):34‐36. [PMC free article] [PubMed] [Google Scholar]
- 32. Agency for Toxic Substances and Disease Registry . CDC Social Vulnerability Index 2018. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html. Updated September 12, 2018. Accessed April 20, 2021.
- 33. Thompson CN, Baumgartner J, Pichardo C, et al. COVID‐19 Outbreak — New York City, February 29–June 1, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1725‐1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Greenhalgh T, Vijayaraghavan S, Wherton J, et al. Virtual online consultations: advantages and limitations (VOCAL) study. BMJ Open. 2016;6(1):e009388. 10.1136/bmjopen-2015-009388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Downes MJ, Mervin MC, Byrnes JM, Scuffham PA. Telephone consultations for general practice: a systematic review. Syst Rev. 2017;6(1):128. 10.1186/s13643-017-0529-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McKinstry B, Hammersley V, Burton C, et al. The quality, safety and content of telephone and face‐to‐face consultations: a comparative study. Qual Saf Health Care. 2010;19(4):298‐303. 10.1136/qshc.2008.027763 [DOI] [PubMed] [Google Scholar]
- 37. Bleyel C, Hoffmann M, Wensing M, Hartmann M, Friederich H‐C, Haun MW. Patients’ perspective on mental health specialist video consultations in primary care: qualitative preimplementation study of anticipated benefits and barriers. J Med Internet Res. 2020;22(4):e17330. 10.2196/17330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Thiyagarajan A, Grant C, Griffiths F, Atherton H. Exploring patients’ and clinicians’ experiences of video consultations in primary care: a systematic scoping review. BJGP Open. 2020;4(1). 10.3399/bjgpopen20X101020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Viers BR, Lightner DJ, Rivera ME, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015. Oct;68(4):729‐35. [DOI] [PubMed] [Google Scholar]
- 41. Freyer JF. Forced by the pandemic, health care plunges into the digital age. Boston Globe. June 12, 2020. https://www.bostonglobe.com/2020/06/12/metro/forced-by-pandemic-health-care-plunges-into-digital-age. Accessed April 20, 2021. [Google Scholar]
- 42. Lau J, Knudsen J, Jackson H, et al. Staying connected in the COVID‐19 pandemic: telehealth at the largest safety‐net system in the United States. Health Affairs. Published June 11, 2020. 10.1377/hlthaff.2020.00903 [DOI] [PubMed] [Google Scholar]
- 43. Samiei V, Wan Puteh SE, Abdul Manaf MR, Abdul Latip K, Ismail A. Are Malaysian diabetic patients ready to use the new generation of health care service delivery? A telehealth interest assessment. Malays J Med Sci. 2016;23(2):44‐52. [PMC free article] [PubMed] [Google Scholar]
- 44. Whittemore R, Jaser SS, Faulkner MS, et al. Type 1 diabetes eHealth psychoeducation: youth recruitment, participation, and satisfaction. J Med Internet Res. 2013;15(1):e15. 10.2196/jmir.2170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Han JH, Sunderland N, Kendall E, Gudes O, Henniker G. Professional practice and innovation: chronic disease, geographic location and socioeconomic disadvantage as obstacles to equitable access to e‐health. Health Inf Manag. 2010;39(2):30‐36. 10.1177/183335831003900205 [DOI] [PubMed] [Google Scholar]
- 46. Duplaga M. A cross‐sectional study assessing determinants of the attitude to the introduction of eHealth services among patients suffering from chronic conditions. BMC Med Inform Decis Mak. 2015;15:33. 10.1186/s12911-015-0157-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kamis K, Janevic MR, Marinec N, Jantz R, Valverde H, Piette JD. A study of mobile phone use among patients with noncommunicable diseases in La Paz, Bolivia: implications for mHealth research and development. Global Health. 2015;11(1):30. 10.1186/s12992-015-0115-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Terschüren C, Mensing M, Mekel OC. Is telemonitoring an option against shortage of physicians in rural regions? Attitude towards telemedical devices in the North Rhine‐Westphalian health survey, Germany. BMC Health Serv Res. 2012;12(1):95. 10.1186/1472-6963-12-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hofstede J, de Bie J, Van Wijngaarden B, Heijmans M. Knowledge, use and attitude toward eHealth among patients with chronic lung diseases. Int J Med Inform. 2014;83(12):967‐974. 10.1016/j.ijmedinf.2014.08.011 [DOI] [PubMed] [Google Scholar]
- 50. LaMonica HM, English A, Hickie IB, et al. Examining internet and eHealth practices and preferences: survey study of Australian older adults with subjective memory complaints, mild cognitive impairment, or dementia. J Med Internet Res. 2017;19(10):e358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Shin P, Alvarez C, Sharac J, et al. A profile of community health center patients: implications for policy. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/a-profile-of-community-health-center-patients-implications-for-policy. Published December 23, 2013. Accessed April 20, 2021. [Google Scholar]
- 52. Basu S, Phillips RS, Phillips R, Peterson LE, Landon BE. Primary care practice finances in the United States amid the COVID‐19 pandemic. Health Affairs. 2020;39(9). 10.1377/hlthaff.2020.00794 [DOI] [PubMed] [Google Scholar]
- 53. Telehealth: Delivering Care Safely During COVID‐19 . HHS.gov website. https://www.hhs.gov/coronavirus/telehealth/index.html. Updated July 15, 2020. Accessed February 23, 2021.
- 54. Medicare Centers for and Services Medicaid. Additional Background: Sweeping regulatory changes to help U.S. healthcare system address COVID‐19 patient surge.Fact sheet . https://www.cms.gov/newsroom/fact‐sheets/additional‐backgroundsweeping‐regulatory‐changes‐help‐us‐healthcare‐system‐address‐covid‐19‐patient. Published March 30, 2020. Accessed February 23, 2021.
- 55. American College of Physicians . ACP recommendations for maintaining certain telehealth policies and waivers after the public health emergency [letter]. June 4, 2020. https://www.acponline.org/acp_policy/letters/acp_letter_to_cms_regarding_extending_telehealth_policy_changes_after_the_phe_june_2020.pdf. Accessed April 20, 2021.
- 56. Hammersley V, Donaghy E, Parker R, et al. Comparing the content and quality of video, telephone, and face‐to‐face consultations: a non‐randomised, quasi‐experimental, exploratory study in UK primary care. Br J Gen Pract. 2019;69(686):e595‐e604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Horn D. Telemedicine is booming during the pandemic. But it's leaving people behind. Washington Post. July 9, 2020. https://www.washingtonpost.com/outlook/2020/07/09/telemedicine-is-booming-during-pandemic-its-leaving-people-behind. Accessed April 20, 2021. [Google Scholar]
- 58. Glueckauf R, Hufford B, Whitton J, et al. Telehealth: emerging technology in rehabilitation and health care. In: Flanagan SR, Zaretsky H, Monoz A, eds. Medical Aspects of Disability: A Handbook for the Rehabilitation Professional, 2nd ed. New York: Springer; 1999: 625–639. [Google Scholar]
- 59. American College of Physicians Division of Governmental Affairs and Public Policy . Payment for telehealth and telephone consultations during COVID‐19. https://www.acponline.org/advocacy/state-health-policy/covid-19-action-toolkit/payment-for-telehealth-and-telephone-consultations-during-covid-19. Published April 17, 2020. Accessed April 20, 2021. [Google Scholar]
- 60. Center for Connected Health Policy . Telehealth coverage policies in the time of COVID‐19. https://www.cchpca.org/resources/covid-19-telehealth-coverage-policies. Published September 20, 2020. Accessed April 20, 2021. [Google Scholar]
- 61. New York State Department of Health . Frequently asked questions regarding use of telehealth including telephonic services during the COVID‐19 state of emergency. https://health.ny.gov/health_care/medicaid/covid19/docs/faqs.pdf. Published May 1, 2020. Accessed April 20, 2021. [Google Scholar]
- 62. Federal Communications Commission . 2018. broadband deployment report. https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2018-broadband-deployment-report. Published February 2, 2018. Accessed April 21, 2021.
- 63. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid‐19. N Engl J Med. 2020;382(18):1679‐1681. 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]


