Abstract
Objective
To describe the immediate impact of the COVID‐19 pandemic on cervical screening, colposcopy and treatment volumes in Ontario, Canada.
Design
Population‐based retrospective observational study.
Setting
Ontario, Canada.
Population
People with a cervix age of 21–69 years who completed at least one cervical screening cytology test, colposcopy or treatment procedure for cervical dysplasia between January 2019 and August 2020.
Methods
Administrative databases were used to compare cervical screening cytology, colposcopy and treatment procedure volumes before (historical comparator) and during the first 6 months of the COVID‐19 pandemic (March–August 2020).
Main outcome measures
Changes in cervical screening cytology, colposcopy and treatment volumes; individuals with high‐grade cytology awaiting colposcopy.
Results
During the first 6 months of the COVID‐19 pandemic, the monthly average number of cervical screening cytology tests, colposcopies and treatments decreased by 63.8% (range: −92.3 to −41.0%), 39.7% (range: −75.1 to −14.3%) and 31.1% (range: −43.5 to −23.6%), respectively, when compared with the corresponding months in 2019. Between March and August 2020, on average 292 (−51.0%) fewer high‐grade cytological abnormalities were detected through screening each month. As of August 2020, 1159 (29.2%) individuals with high‐grade screening cytology were awaiting follow‐up colposcopy.
Conclusions
The COVID‐19 pandemic has had a substantial impact on key cervical screening and follow‐up services in Ontario. As the pandemic continues, ongoing monitoring of service utilisation to inform system response and recovery is required. Future efforts to understand the impact of COVID‐19‐related disruptions on cervical cancer outcomes will be needed.
Tweetable abstract
COVID‐19 has had a substantial impact on cervical screening and follow‐up services in Ontario, Canada.
Keywords: Cervical screening, colposcopy, COVID‐19, cytology, service utilisation
Tweetable abstract
COVID‐19 has had a substantial impact on cervical screening and follow‐up services in Ontario, Canada.
Introduction
On 11 March 2020, the coronavirus disease 2019 (COVID‐19) was declared a global pandemic affecting countries worldwide, including Canada. 1 As of 1 March 2021, Canada has had 870 033 COVID‐19 cases and 22 017 deaths, of which 301 839 cases and 6968 deaths have been in the province of Ontario. 2
In March 2020, the Ontario government directed all hospitals and regulated healthcare professionals to ramp down elective and non‐emergent clinical services in order to limit the transmission of COVID‐19 and preserve health system capacity to treat COVID‐19 cases and other critical illnesses. 3 , 4 Following this, Ontario Health (Cancer Care Ontario), a provincial agency that oversees healthcare delivery across the province, released guidance for the provision of cancer services during the pandemic. 5 , 6 Consistent with provincial guidance 5 , 6 , on 23 March 2020, it was recommended that all routine cancer screening services be paused. Invitation, recall and reminder correspondence to eligible screening participants, a key element of Ontario's organised cancer screening programmes, was suspended. Following a decrease in COVID‐19 transmission in Ontario, at the end of May 2020, the gradual resumption of deferred services was permitted. 7
In 2020, it was estimated that 553 individuals in Ontario would be diagnosed with invasive cervical cancer and 185 would die from the disease. 8 Most invasive cervical cancer is preventable with human papillomavirus (HPV) immunisation, regular screening, and appropriate and timely follow‐up of abnormal screening results. 9 Organised cervical screening programmes, including the Ontario Cervical Screening Program (OCSP), seek to detect and treat cervical cancer precursors to prevent the progression to invasive cervical cancer. 10 The OCSP currently recommends individuals aged 21–69 years with a cervix be screened with cervical cytology every 3 years. 11 To support the prioritisation of cases in colposcopy (a diagnostic procedure following abnormal cervical screening results 12 ) during the pandemic, some screening‐related colposcopy services were recommended to continue (i.e. follow‐up of high‐grade screening results), whereas others were recommended to be reduced and deferred (i.e. follow‐up of low‐grade screening results). 5 , 6
The objective of this study was to describe the impact of the first 6 months of the COVID‐19 pandemic on the delivery of cervical screening, colposcopy and treatment services in Ontario.
Methods
Study design and population
A population‐based retrospective observational study was conducted to compare volumes of cervical screening, colposcopy and treatment services in Ontario, Canada, immediately prior to (i.e. January 2019–February 2020) and during the early months (i.e. March 2020–August 2020) of the COVID‐19 pandemic. The province of Ontario has a publicly funded single‐payer healthcare system. Throughout the province, 14 regional cancer programmes are involved in providing cancer prevention, screening, diagnostic, treatment and other support services. The OCSP, a population‐based organised cervical screening programme, currently recommends individuals aged 21–69 years with a cervix be screened with cervical cytology every 3 years. 11 Approximately 1 million people undergo 1.1 million cervical cytology tests annually in Ontario. Following a high‐grade cytology result, individuals are recommended to receive colposcopy, whereas those with low‐grade results are recommended to repeat cytology in 6 months. 11 Colposcopy allows a clinician to identify a cervical lesion, confirm a diagnosis by biopsy and advise either treatment for cervical cancer precursors or conservative management in the absence of cancer precursors. 12 All individuals aged 21–69 years with a cervix who received cervical screening cytology, colposcopy or treatment between January 2019 and August 2020 were included in the study. Individuals younger than 21 years, or 70 years and older were excluded.
Ontario Health (Cancer Care Ontario) is designated a ‘prescribed entity’ and as such, under section 45(1) of the Personal Health Information Protection Act of 2004, is authorised to collect personal health information from health information custodians without the consent of the patient. Such personal health information can be used for analysis or compiling statistical information with respect to the management, evaluation or monitoring of the allocation of resources to or planning for all or part of the health system, including the delivery of services. Because this study is in compliance with privacy regulations, ethics review was not required. There was no public or patient involvement in the study design or interpretation of results. This study was conducted with the support of Ontario Health (Cancer Care Ontario) through in‐kind contributions.
Data sources
Several population‐based administrative databases were used to identify the study population and variables of interest. CytoBase, a centralised database that includes cervical cytology tests analysed in some community‐based laboratories throughout Ontario 13 , was used to identify cervical cytology results. CytoBase contains approximately 90% of all cervical screening cytology test results completed in Ontario. Cytology results are reported according to the current Bethesda classification. 14 The Ontario Health Insurance Plan (OHIP) database contains information on healthcare billings for services delivered by physicians in Ontario. In the absence of a dedicated colposcopy database, the OHIP database was used to identify colposcopy visits and cervical treatment procedures including the date of service. Procedures used for the treatment of cervical dysplasia included local electrosurgical excision procedure, cone biopsy, cryoconisation, electroconisation, CO2 laser therapy, electrocautery and cryotherapy. The Registered Persons Database contains information on Ontarians eligible for OHIP 15 and was used to capture the demographic information (i.e. age and postal code) of participants. All databases were linked using the individual health card number as a unique identifier. As the objective of this study was to assess changes to service utilisation, the use of core outcome sets was not relevant.
Data analysis
Differences between monthly cervical screening cytology test, colposcopy and cervical treatment volumes during the first 6 months of the pandemic (i.e. March 2020–August 2020) and the corresponding monthly volumes in 2019 were calculated. Descriptive statistics were reported as absolute volumes with 95% confidence intervals and relative proportions with ranges of minimum and maximum values. The number of individuals with a high‐grade screening cytology result (i.e. high‐grade squamous intraepithelial lesion, atypical squamous cells cannot exclude high‐grade squamous intraepithelial lesion, atypical glandular cells or adenocarcinoma in situ) who received follow‐up colposcopy or were still awaiting follow‐up as of August 2020 was also computed. All analyses were performed using SAS, Version 9.4 (SAS Institute, Cary, NC, USA).
Results
From March to August 2020, monthly cervical screening cytology test volumes were substantially reduced compared with the same months 1 year prior (Figure 1, Table S1). The largest monthly reduction in cervical cytology test volumes (−92.3%) was observed in April 2020. Between May and August 2020, cervical cytology test volumes began to gradually increase but they were still reduced compared with the same months in 2019 (range: −85.8 to −41.0%). The average number of cervical screening cytology tests completed between March and August 2020 was 29 147 tests, compared with 81 877 for the same months in 2019, representing an average monthly decrease of 63.8% (range: −92.3 to −41.0%), or 52 730 tests (95% CI 36 367–69 093). The reduction in cervical cytology test volumes was consistent across all 14 of Ontario's regional cancer programmes (Figures S1 and S2).
Figure 1.
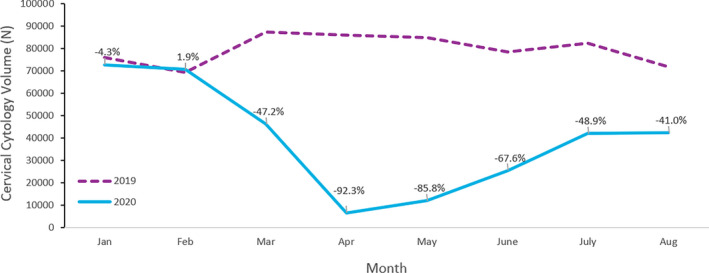
Cervical screening cytology tests completed in Ontario between January and August 2019 versus January and August 2020.
As expected due to the decrease in the number of cervical cytology tests completed, the number of individuals with a high‐grade screening cytology test result also decreased during the first few months of the COVID‐19 pandemic (Table 1). Between November 2019 and February 2020, an average of 572 individuals with a high‐grade cytology result were identified each month; in contrast, from March to August 2020, the average number of individuals with a high‐grade cytology result identified per month was 280. Therefore, since the beginning of the pandemic in March 2020, on average 292 (−51.0%) fewer individuals with a high‐grade cytology result were identified each month through screening. Among the 3967 participants who had a high‐grade screening cytology result between November 2019 and August 2020, 1159 (29.2%) were still awaiting colposcopy follow‐up as of August 2020. Of those, 385 (33.2%) had received their high‐grade screening cytology result before the start of the pandemic (i.e. November 2019–February 2020).
Table 1.
Individuals with high‐grade cytology test results who received or were awaiting colposcopy in Ontario between November 2019 and August 2020
| Nov‐19 | Dec‐19 | Jan‐20 | Feb‐20 | Mar‐20 | Apr‐20 | May‐20 | Jun‐20 | Jul‐20 | Aug‐20 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Individuals who had a high‐grade cytology test result | 653 | 549 | 574 | 512 | 325 | 117 | 180 | 308 | 435 | 314 | 3967 |
| Received colposcopy |
565 (86.5%) |
446 (81.2%) |
478 (83.3%) |
414 (80.9%) |
247 (76.0%) |
71 (60.7%) |
122 (67.8%) |
184 (59.7%) |
216 (49.7%) |
65 (20.7%) |
2808 (70.8%) |
| Awaiting colposcopy |
88 (13.5%) |
103 (18.8%) |
96 (16.2%) |
98 (19.1%) |
78 (24.0%) |
46 (39.3%) |
58 (32.2%) |
124 (40.3%) |
219 (50.3%) |
249 (79.3%) |
1159 (29.2%) |
Reductions in colposcopy services including treatment volumes were also observed during the first 6 months of the pandemic (Figures 2 and 3, Tables S2 and S3). Between March and August 2019, an average of 8614 colposcopy assessments and 737 procedures for the treatment of cervical dysplasia were completed each month. Between March and August 2020, the average monthly decrease in colposcopy volumes was 3555 colposcopies (95% CI 1844–5265), or 39.7% (range: −75.1% to −14.3%) compared with the same months in 2019 (Figure 2, Table S2). During this same time period, the average monthly decrease in cervical treatment volumes was 31.1% (range: −43.5% to −23.6%) or 288 (95% CI 147–310) cervical treatments compared with the same months in 2019 (Figure 3, Table S3). The largest reduction in colposcopy volumes (−75.1%) was observed in April 2020, whereas the largest reduction in treatment volumes (−43.5%) was observed in July 2020, which likely reflects earlier reductions observed in screening volumes observed in March to May 2020.
Figure 2.
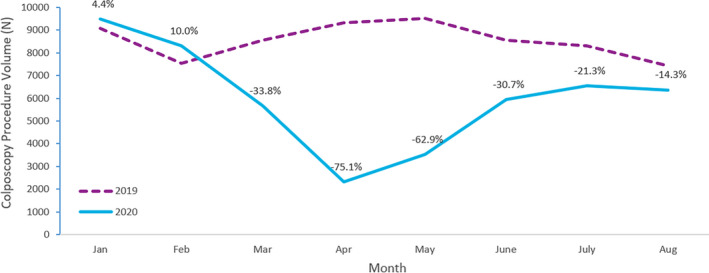
Colposcopy procedures completed in Ontario between January and August 2019 versus January and August 2020.
Figure 3.
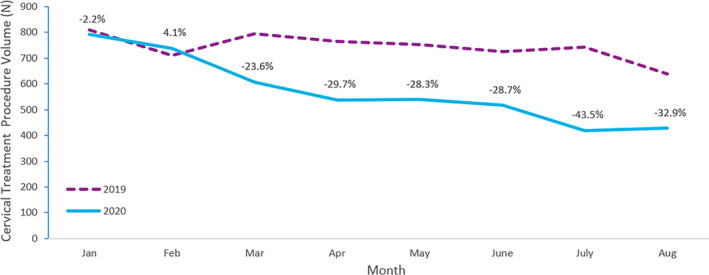
Cervical treatment procedures completed in Ontario between January and August 2019 versus January to August 2020.
Discussion
Main findings
During the first 6 months of the COVID‐19 pandemic, cervical screening, colposcopy and treatment volumes decreased considerably in Ontario from pre‐pandemic levels. Concordant with the reduction in cervical screening, on average 292 (−51.0%) fewer high‐grade cytological abnormalities were detected each month between March and August 2020. Although cervical screening, colposcopy and treatment volumes in Ontario had started to recover by August 2020, they had yet to reach pre‐pandemic levels based on historical data. As the pandemic continues, it is expected that these services may continue to be reduced for some time for several reasons. First, the rigorous infection prevention and control measures that remain in place reduce the volume of interactions that colposcopists and primary care providers (PCPs) are able to engage in. Secondly, some PCPs have not resumed in‐person visits for preventive care. Finally, as of March 2021, cervical screening correspondence letters inviting people to get screened have remained paused.
Interpretation
Similar COVID‐19‐related reductions in cervical screening volumes have been observed internationally. 16 , 17 , 18 , 19 , 20 Of particular concern in Ontario, is the approximately 50% fewer high‐grade screening cytology results identified in each of the first 6 months of the pandemic as compared with each of the previous 4 months. Additionally, among the 3967 individuals with high‐grade cytology identified between November 2019 and August 2020, almost a third (29.2%) had not received colposcopy as of August 2020. Of these, a third (33.2%) have been awaiting follow‐up since before the pandemic (i.e. February 2020 or earlier, ≥6 months). In contrast, between 2016 and 2018, 13.5–15.7% of individuals with high‐grade cytology in Ontario did not receive colposcopy within 6 months. 21 Timely detection and follow‐up of abnormal screening results, and treatment as appropriate, are a crucial element of reducing the risk of progression to invasive cervical cancer. 9 , 22 A population‐based study from Ontario found that 1.1–2.9% of individuals with high‐grade cytology had underlying invasive cervical cancer. 23 During the first few months of the pandemic in Ontario, some individuals with high‐grade cytology results had their follow‐up colposcopy visit delayed, which could have delayed the diagnosis and possible treatment of cervical pre‐cancers. The longer these individuals wait, the risk of them being lost to follow‐up, and potentially present at a later date with a more advanced cancer that is more difficult to treat and cure, increases.
Although it is not yet possible to measure the impact of the COVID‐19‐related service reductions on cervical cancer outcomes, modelling from Australia suggests that COVID‐19‐related disruptions to routine screening in 2020 could result in a 1.1–3.6% increase in cervical cancer diagnoses in that country. 24 It was also estimated that in Australia, between 2020 and 2022, more cervical cancers would be diagnosed at a later stage (~30–97 individuals), resulting in additional cervical cancer mortality, morbidity or both over the long term (~6–20 deaths). 24 Careful ongoing assessment of the downstream impacts of COVID‐19‐related service disruptions on cervical pre‐cancer and cancer outcomes in Ontario will be necessary to plan provision of services and to minimise negative outcomes.
Although most cervical screening correspondence remains paused and managing the COVID‐19 pandemic remains a top priority for healthcare system leaders, continued access to screening and colposcopy services during the pandemic will be essential to preventing avoidable cervical cancer morbidity and mortality that may arise as a result of delayed or inadequate screening and follow‐up. To support PCPs and colposcopists, in June 2020, Ontario Health (Cancer Care Ontario) released two tip sheets outlining considerations for resuming cervical screening and colposcopy services including risk‐based priority classification frameworks. 25 , 26 Recommendations from these tip sheets include that where colposcopy capacity is limited, patients with high‐grade cytology should be prioritised for colposcopy, as their immediate risk of high‐grade cervical dysplasia is high. 25 In addition, for patients with first‐time low‐grade cytology results, colposcopy referral is discouraged; instead, PCPs are encouraged to repeat cytology within 12 months, as the risk of high‐grade cervical dysplasia is low and cytological changes generally reflect transient HPV infection that will not cause cervical cancer. 25 , 26 Finally, PCPs are encouraged to adopt the planned change of initiating cervical screening at age 25 years 26 (rather than 21 years), given the strong evidence that screening prior to that age is highly unlikely to be of benefit. 27 Similar recommendations could be considered by other jurisdictions facing similar capacity constraints.
As the pandemic continues, it is anticipated that constraints on colposcopy capacity may be prolonged and may vary depending on local COVID‐19 transmission and resource availability. While ensuring individual providers understand the importance of appropriate screening and colposcopy referral is imperative, facility‐ or regional‐level strategies for optimising resource use to manage the colposcopy backlog will also be required. For example, facilities and regional cancer programmes could consider implementing centralised referral intake (i.e. coordinated points of entry for receiving referrals) and colposcopy waitlists (i.e. patients are booked for the next available appointment with an appropriate provider in their region). 25 Ongoing monitoring of local data will also be important for recovery planning. 25 To support this, Ontario Health (Cancer Care Ontario) has created a tool that allows for both provincial and local monitoring of screening, colposcopy and treatment volumes, as well as the number of individuals with high‐grade cytology awaiting follow‐up. 28 Regional cancer programmes have reported that the tool has been used to support local planning, recovery and communication efforts. Other jurisdictions could consider similar tools and strategies to assist with monitoring, recovery and planning efforts.
Strengths and limitations
This observational study has several strengths, including its large size, high coverage of the provincial population, and use of high‐quality administrative health databases. To our knowledge, Ontario is one of the first jurisdictions comprehensively to report on colposcopy and cervical dysplasia treatment service utilisation during the COVID‐19 pandemic.
This study has several limitations. First, the use of a pre‐/post‐analysis could not account for events other than the pandemic that could have impacted service utilisation. Secondly, quantification of the impact of the reduction in service volumes on cervical pre‐cancer and cancer outcomes was not possible. Thirdly, the total number of screening‐related cytology tests in the province is underestimated, as the small proportion (<10%) that are completed in hospital are not captured through CytoBase. Additionally, it is difficult to determine whether a cytology test in CytoBase was done for screening or diagnostic purposes, and therefore a small number of cytology tests included in these analyses may have been performed for diagnostic purposes. Finally, as colposcopy and treatment service volumes were determined through physician billings, the indication for colposcopy (e.g. abnormal screening result follow‐up, non‐screening‐related indications) or treatment could not be determined.
Conclusion
The COVID‐19 pandemic has had a substantial impact on key cervical screening and follow‐up services in Ontario. As the pandemic continues to evolve, there will be a need for ongoing monitoring of service volumes to inform ongoing system response, recovery and future planning efforts. Resumption of letters to invite, remind or recall eligible individuals to be screened may assist with recovery efforts. It will also be critically important to evaluate the downstream impacts on cervical screening and colposcopy quality, and clinical cervical cancer outcomes. Lastly, the findings underscore the urgency of continuing to identify and implement strategies to improve colposcopy efficiency and ensure appropriate management of available resources.
Disclosure of interests
None declared. Completed disclosure of interests forms are available to view online as supporting information.
Contribution to authorship
All authors contributed to the conception and design of the study. JG and NJ analysed the data. JG, NJ, OM and MW interpreted the data and drafted the article. RK, KJM, LR and MR reviewed the article and critically revised it for important intellectual content. All authors reviewed and approved the final article for publication.
Details of ethics approval
Ontario Health (Cancer Care Ontario) has been designated a ‘prescribed entity’ for the purposes of section 45(1) of the Personal Health Information Protection Act of 2004. As a prescribed entity, Ontario Health (Cancer Care Ontario) is authorised to collect personal health information from health information custodians without the consent of the patient, and to use such personal health information for the purpose of analysis or compiling statistical information with respect to the management, evaluation or monitoring of the allocation of resources to or planning for all or part of the health system, including the delivery of services. Because this study is in compliance with privacy regulations, ethics review was not required.
Funding
This study was conducted with the support of Ontario Health (Cancer Care Ontario) through in‐kind contributions. The opinions, results, views and conclusions reported in this publication are those of the authors and do not necessarily reflect those of Ontario Health (Cancer Care Ontario). No endorsement by Ontario Health (Cancer Care Ontario) is intended or should be inferred.
Acknowledgements
Ontario Cervical Screening Program/Colposcopy COVID‐19 Working Group contributors: Melissa Coulson, Ontario Health (Cancer Care Ontario); Bronwen R McCurdy, Ontario Health (Cancer Care Ontario); Christine Stogios, Ontario Health (Cancer Care Ontario); Justine Wallace, Ontario Health (Cancer Care Ontario); Li Wang, Ontario Health (Cancer Care Ontario).
Supporting information
Figure S1. Cervical screening cytology test volumes in April 2019 and April 2020 for the 14 regional cancer programmes in Ontario.
Figure S2. Cervical screening cytology test volumes in August 2019 and April 2020 for the 14 regional cancer programmes in Ontario.
Table S1. Cervical screening cytology tests completed in Ontario between January and August 2019 versus January and August 2020.
Table S2. Colposcopy procedures completed in Ontario between January and August 2019 versus January and August 2020.
Table S3. Cervical treatment procedures completed in Ontario between January and August 2019 versus January to August 2020.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Meggetto O, Jembere N, Gao J, Walker MJ, Rey M, Rabeneck L, Murphy KJ, Kupets R; on behalf of the Ontario Cervical Screening Program/Colposcopy COVID‐19 Working Group . The impact of the COVID‐19 pandemic on the Ontario Cervical Screening Program, colposcopy and treatment services in Ontario, Canada: a population‐based study. BJOG 2021; 128:1503–1510.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.
References
- 1. World Health Organization . Timeline: WHO's COVID‐19 response [Internet]. Geneva: World Health Organization; 2020. [https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/interactive‐timeline]. Accessed 4 November 2020. [Google Scholar]
- 2. Government of Canada . Coronavirus Disease (COVID‐19): Outbreak Update [Internet]. Ottawa: Government of Canada; 2021. [https://www.canada.ca/en/public‐health/services/diseases/2019‐novel‐coronavirus‐infection.html]. Accessed 1 March 2021. [Google Scholar]
- 3. COVID‐19 Directive #2 for Health Care Providers (regulated health Professionals or Persons Who Operate a Group Practice of Regulated Health Professionals), Issued under Section 77.7 of the Health Protection and Promotion Act (HPPA), R.S.O. 1990, c. H.7. Toronto: Ministry of Health; 2020, 19 March. [https://www.ctcmpao.on.ca/resources/CMOH_Directive_2‐RHPA_professionals_2020‐03‐19.pdf]. Accessed/cited 4 November 2020. [Google Scholar]
- 4. Ramping Down Elective Surgeries and Other Non‐emergent Activities [Memorandum to Ontario Health and Hospitals]. Toronto: Ministry of Health; 2020, 15 March. [http://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/memos/DM_OH_CMOH_memo_COVID19_elective_surgery_March_15_2020.pdf]. Accessed 4 November 2020. [Google Scholar]
- 5. Ontario Health (Cancer Care Ontario) . Pandemic Planning Clinical Guideline for Patients with Cancer [Internet]. Toronto: Ontario Health (Cancer Care Ontario); 2020. [https://www.cancercareontario.ca/en/guidelines‐advice/types‐of‐cancer/64736]. Accessed 4 November 2020. [Google Scholar]
- 6. Ontario Health (Cancer Care Ontario) . COVID‐19 Supplemental Clinical Guidance for Patients with Cancer [Internet]. Toronto: Ontario Health (Cancer Care Ontario); 2020. [https://www.ontariohealth.ca/sites/ontariohealth/files/2020‐04/Ontario%20Health%20Cancer%20Care%20Ontario%20COVID‐19%20Supplemental%20Clinical%20Guidance%20for%20Patients%20with%20Cancer_29Mar20%20PDF.pdf]. Accessed 4 November 2020. [Google Scholar]
- 7. COVID‐19 Directive #2 for Health Care Providers (Regulated Health Professionals or Persons Who Operate a Group Practice of Regulated Health Professionals), Issued under Section 77.7 of the Health Protection and Promotion Act (HPPA). R.S.O. 1990, c. H.7 [Internet]. Toronto: Ministry of Health; 2020, 26 May. [http://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/directives/RHPA_professionals.pdf]. Accessed 4 November 2020. [Google Scholar]
- 8. Ontario Health (Cancer Care Ontario) . Ontario Cancer Statistics 2020 [Internet]. Toronto: Ontario Health (Cancer Care Ontario); 2020. [https://www.cancercareontario.ca/en/statistical‐reports/ontario‐cancer‐statistics‐2020]. Accessed 4 November 2020. [Google Scholar]
- 9. World Health Organization . Comprehensive Cervical Cancer Control: A Guide to Essential Practice [Internet]. Geneva: World Health Organization; 2014. [https://www.who.int/reproductivehealth/publications/cancers/cervical‐cancer‐guide/en/]. Accessed 4 November 2020. [PubMed] [Google Scholar]
- 10. Safaeian M, Solomon D, Castle PE. Cervical cancer prevention—cervical screening: science in evolution. Obstet Gynecol Clin North Am 2007;34:739–ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cancer Care Ontario . Ontario Cervical Screening Recommendations Summary [Internet]. Toronto: Cancer Care Ontario; 2020. [https://www.cancercareontario.ca/en/system/files_force/derivative/OCSPScreeningGuidelines.pdf]. Accessed 1 March 2021. [Google Scholar]
- 12. Bentley J. Colposcopic management of abnormal cervical cytology and histology. J Obstet Gynaecol Can 2012;34:1188–202. [DOI] [PubMed] [Google Scholar]
- 13. Inscyte Corporation [Internet]. Toronto: Inscyte Corporation; 2020. [https://www.inscyte.org/]. Accessed 4 November 2020. [Google Scholar]
- 14. Nayar R, Wilbur DC. The Bethesda System for Reporting Cervical Cytology: Definitions, Criteria, and Explanatory Notes. New York: Springer International Publishing; 2015. [Google Scholar]
- 15. Government of Ontario . Registered Persons Database (RPDB) [Internet]. Toronto: Government of Ontario; 2018. [https://data.ontario.ca/dataset/registered‐persons‐database‐rpdb]. Accessed 4 November 2020. [Google Scholar]
- 16. de Pelsemaeker MC, Guiot Y, Vanderveken J, Galant C, Van Bockstal MR. The impact of the COVID‐19 pandemic and the associated Belgian governmental measures on cancer screening, surgical pathology and cytopathology. Pathobiology 2020;7:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. EPIC Health Research Network . Preventive Cancer Screenings during COVID‐19 Pandemic [Internet]. Verona, WI: EPIC Health Research; 2020. [https://www.ehrn.org/articles/delays‐in‐preventive‐cancer‐screenings‐during‐covid‐19‐pandemic]. Accessed 4 November 2020. [Google Scholar]
- 18. Tsai HJ, Chang YL, Chen FM. The feasibility and necessity of cancer screening events in the community during the COVID‐19 pandemic in Taiwan. J Med Screen 2020;28:55–6. [DOI] [PubMed] [Google Scholar]
- 19. Nathoo A, Weng I, Kim J, Ortuno A. Routine Chronic Disease Screenings and Oncology Biomarker Tests Plummet during COVID‐19. New York: Komodo Health; 2020. [https://www.komodohealth.com/insights/2020/04/routine‐chronic‐disease‐screenings‐and‐oncology‐biomarker‐tests‐plummet‐during‐covid‐19]. Accessed 4 November 2020. [Google Scholar]
- 20. Vigliar E, Iaccarino A, Bruzzese D, Malapelle U, Bellevicine C, Troncone G. Cytology in the time of coronavirus disease (COVID‐19): an Italian perspective. J Clin Pathol 2021;74:261–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ontario Health (Cancer Care Ontario) . Ontario Cancer Screening Performance Report 2020 [Internet]. Toronto, ON: Ontario Health; 2021. [https://www.cancercareontario.ca/sites/ccocancercare/files/assets/OntarioCancerScreeningReport2020.pdf]. Accessed 2 February 2020. [Google Scholar]
- 22. Duggan MA, Nation J. An audit of the cervical cancer screening histories of 246 women with carcinoma. J Low Genit Tract Dis 2012;16:263–70. [DOI] [PubMed] [Google Scholar]
- 23. Kupets R, Paszat L. How are women with high grade Pap smear abnormalities managed? A population based study. Gynecol Oncol 2011;121:499–504. [DOI] [PubMed] [Google Scholar]
- 24. Smith M, Hall M, Simms K, Killen J, Sherrah M, O'Farrell X, et al. Modelled Analysis of Hypothetical Impacts of COVID‐19 Related Disruptions on the National Cervical Screening Program. Report to the Department of Health (May 2020) [Internet]. New South Wales: Cancer Research Division, Cancer Council NSW; 2020. [https://www.health.gov.au/resources/publications/modelled‐analysis‐of‐hypothetical‐impacts‐of‐covid‐19‐related‐disruptions‐to‐the‐national‐cervical‐screening‐program]. Accessed 4 November 2020. [Google Scholar]
- 25. Ontario Health (Cancer Care Ontario) . COVID‐19 Tip Sheet for Facilities Performing Colposcopy. 12 – Guidance for Increasing Colposcopy Services – 2020‐06‐19. Toronto: Ontario Health (Cancer Care Ontario); 2020. [https://www.cancercareontario.ca/sites/ccocancercare/files/assets/COVID‐19TipSheet12‐GuidanceForIncreasingColposcopyServices.pdf]. Accessed 4 November 2020. [Google Scholar]
- 26. Ontario Health (Cancer Care Ontario) . COVID‐19 Cancer Screening Tip Sheet for Primary Care Providers. 15 – Guidance for Primary Care Providers Resuming Breast, Cervical and Colorectal Cancer Screening – 2020‐06‐30. Toronto: Ontario Health (Cancer Care Ontario); 2020. [https://www.cancercareontario.ca/sites/ccocancercare/files/assets/COVID‐19TipSheet15‐GuidanceForPrimaryCareProvidersResumingCancerScreening.pdf]. Accessed 4 November 2020. [Google Scholar]
- 27. Canadian Task Force on Preventive Health Care . Recommendations on screening for cervical cancer. CMAJ 2013;185:35–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ontario Health (Cancer Care Ontario) . COVID‐19 Ontario Cervical Screening Program (OCSP) Regional Monitoring and Planning Tool (Unpublished Work). Toronto: Ontario Health (Cancer Care Ontario); 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Cervical screening cytology test volumes in April 2019 and April 2020 for the 14 regional cancer programmes in Ontario.
Figure S2. Cervical screening cytology test volumes in August 2019 and April 2020 for the 14 regional cancer programmes in Ontario.
Table S1. Cervical screening cytology tests completed in Ontario between January and August 2019 versus January and August 2020.
Table S2. Colposcopy procedures completed in Ontario between January and August 2019 versus January and August 2020.
Table S3. Cervical treatment procedures completed in Ontario between January and August 2019 versus January to August 2020.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.


