Abstract
BACKGROUND
Teledermatology has evolved as a valuable option to outpatient visits during the current pandemic. We set up a smartphone‐based hybrid model of teledermatology services providing direct care to patients at our center. To analyse patient and physician‐experience and acceptability for teledermatology over a 6‐month‐period, along with clinicodemographic profile of patients.
METHODOLOGY
Single‐center, retrospective study conducted from May 20, 2020 to October 31, 2020. Patient satisfaction level for teledermatology was assessed on a 4‐point scale and compared with the satisfaction level during their previous physical visits prior to COVID‐19 pandemic. A physician assessment form was utilised to record the experience of dermatologists while providing teledermatology services.
RESULTS
Of 7530 patients registered, a successful consult was provided to 6125 patients (81.34%). Average number of teleconsultations/day rose from 23.60 in May 2020 to 77.96 in October 2020. Mean age of patients availing teledermatology services was 33.60 ± 16.99 years. Average distance to care and travel time were 100.90 ± 171.77 km and 135 ± 222.32 min, respectively. A definitive diagnosis could be ascertained in 5724 patients (93.45%) and in‐person visit was recommended to 133 patients (2.2%). Out of 6125 patients, 5229 could be contacted for feedback, 935 (18.18%), 2230 (42.65%), 1749 (33.45%), and 300 patients (5.70%) reported being very satisfied, satisfied, partially satisfied, and unsatisfied, respectively. Of 1914 patients, who had availed in‐person OPD facilities prior to the pandemic, 914 patients (49.62%) preferred in‐person visits. Of 34 dermatologists surveyed, 88.2% felt comfortable providing teleconsultations and 82.4% felt the need to continue teledermatology services in the upcoming months.
CONCLUSIONS
Overall, teledermatology is a valid alternative for in‐person dermatology visits during the current crisis; helping with initial triage and further patient management. Further refinement of the process could lead to even more acceptability.
Keywords: access, COVID‐19, remote care, teledermatology, telehealth
1. INTRODUCTION
Teledermatology is an old, yet poorly adopted concept in routine dermatological care. The outbreak of COVID‐19 was declared as a global pandemic by the World Health Organization on March 11, 2020. To ensure effective social distancing as an infection control strategy, many nations had declared lockdown. Access to standard health care had become more difficult with the strict imposition of laws and restriction of mobility. Telemedicine emerged as a solution to these problems in various specialties, including dermatology.
Dermatology is essentially a visual specialty, and hence, ideally suited for the use of telecommunication technology to support health care at a distance. A high rate of concordance regarding the diagnosis and management has been previously observed between the face‐to‐face and teledermatology consultations. 1 Teledermatology also provides an opportunity for initial triage in order to choose the patients who need an in‐person visit and identifying those whose management can be further continued on teledermatology platform, thus obviating non‐essential face‐to‐face visits. Indirectly, it also brings down the cost of health care for patients and helps service providers channelise men and materials towards COVID services. These potential benefits can make telemedicine the future of health care services, even after the pandemic ends, especially in large‐volume health care services like India where majority of the patients were previously being seen without prior appointments, even in tertiary care centers.
This retrospective study was conducted to provide an audit and insight into our experience with teledermatology services. Our objective was to evaluate the acceptability of this practice by analyzing the patient and physician‐experience with teledermatology.
2. MATERIALS AND METHODS
2.1. Setting
This was a single‐center, retrospective, observational study conducted at a tertiary care center in North India. After obtaining approval of the Institutional ethics committee, we conducted a retrospective chart review of telemedicine services at our center from May 20, 2020 to October 31, 2020.
2.2. Services
Two major models of teledermatology include store and forward teledermatology (S&F TD) and real‐time teledermatology (RTTD). S&F TD utilises images that are assessed asynchronously by the physician. RTTD is based on live interaction between the physician and the patient via video conferencing, with the advantage of immediate clarification of patient complaints. In a hybrid model, images are procured which is followed by the physicians having a real‐time interaction with the patients. Over three‐fourth of world population has now access to mobile phones with internet access. 2 , 3 With the ever‐improving quality of smartphone cameras, mobile teledermatology can be accessible to all, and helps obviate complicated set‐up difficulties, especially at the end of the patients, while using teledermatology services.
Our department chose to have a hybrid model telemedicine service (using an android smartphone with 4G internet connectivity) in place catering to both new and follow‐up patients. A telemedicine contact number was provided on the institutional website and the patients registered themselves on the forthcoming available dates by calling on this number between 8 and 10 a.m. Prior registration could also be done directly on the institutional website. Teledermatology consultation was provided by a set of doctors from 10 a.m. to 1 p.m. on all working days under the supervision of the faculty. A list of registered patients for the day and their cards were provided to the working team by the Central Registration Department.
Phone calls were used to initially talk to the patients in order to obtain history and understand their concerns. This was followed by the patients sending their images, previous records and investigations through smartphone‐based application WhatsApp Messenger. Further calls were made if needed to obtain additional images or history. For each consult, patient's chief complaints, total duration of illness and status of disease was noted. Medical management was provided to all patients where a diagnosis could be ascertained. In patients where the diagnosis was not clear, patients were managed symptomatically where obtaining a diagnosis was not deemed urgent/emergent. In‐person visits were recommended for patients needing hospital admission for dermatological emergencies, injectable medications or urgent skin biopsies to ascertain diagnosis and further management.
2.3. Participants
Data were collected from the consultation cards only for the patients in whom a successful teleconsultation could be conducted. Patients who registered for teledermatology services but could not be contacted for real‐time teleconsultation were excluded from the final analysis.
Demographic parameters such as age, sex and address were noted from the registration details of the patients. Distance to care and travel time (assuming road travel using private vehicle with traffic conditions at 9 a.m. on a Wednesday) from patient's address to our outpatient department was measured using Google maps. Other variables that were collected included type of visit (initial vs. established/follow‐up), duration of disease, disease status, definitive diagnosis (if ascertained) and the need for an in‐person visit (and reason for the same).
The patients included in the study were later called by a team of independent persons not involved in direct patient care in order to rate their satisfaction with the teledermatology service on a 4‐point scale: very satisfied (4), satisfied (3), partially satisfied (2) and unsatisfied (1). Patients who had availed both, an in‐person outpatient consult prior to the pandemic and a telemedicine consult during pandemic, were inquired regarding their preferred mode of visit.
Feedback regarding teledermatology services was obtained at the end of October 2020 from the dermatologists who provided teledermatology services during the studied period (Supporting Information, Appendix S1) in terms of satisfaction, comfort and challenges faced while providing teledermatology services, along with their willingness to continue telemedicine services once the pandemic was over. Latest national telemedicine guidelines were followed throughout. 4
2.4. Statistical methods
Descriptive variables are presented as median (interquartile range IQR) and count (percentage) as appropriate. The significance level was set at p < 0.05. Values are given as the absolute number of patients or as the percentage of the respective group. Variance was calculated as standard deviation. Kendall's tau was used to analyse correlation between variables. Missing data was handled by excluding participants with missing information and performing a complete‐case analysis.
3. RESULTS
3.1. Utilization of teledermatology services
A total of 7530 patients registered for teledermatology services, a successful consult could be provided in 6125 patients (81.34%). Barriers to a successful teleconsultation included duplicate entries (n = 227, 3.01%), incorrect contact details (n = 219, 2.91%), connectivity issues (n = 532, 7.06%) and technological inability of the patient/ next to kin to send pictures (n = 436, 5.79%). A rising trend in number of teleconsultation requests was observed throughout the study period (Figure 1). Average number of teleconsultations per day was 23.60 in May 2020, which increased to 30.70 in June, 44.88 in July, 59.12 in August, 69.23 in September and 77.96 in October.
FIGURE 1.
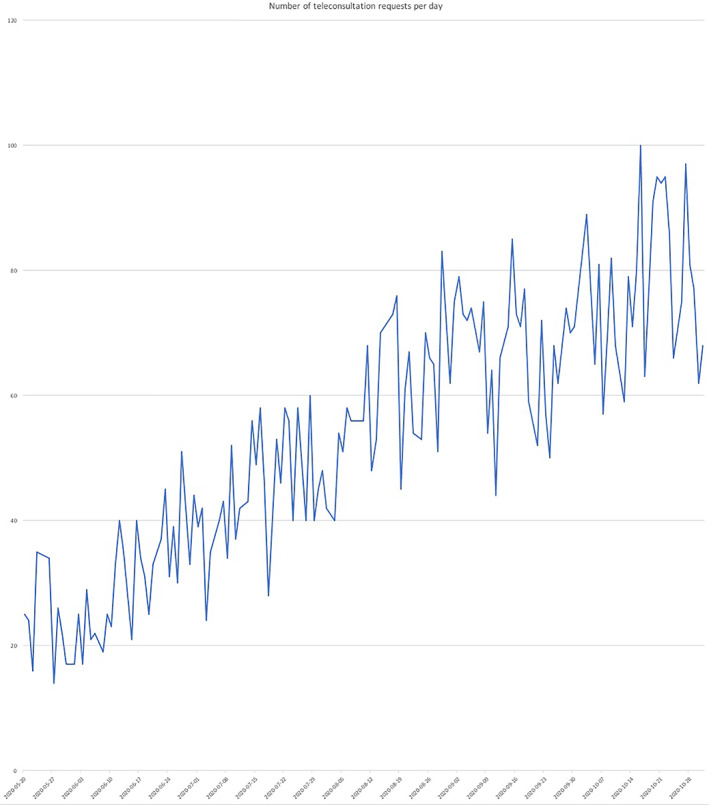
Trend in number of teleconsultation requests during the study period from May to October 2020
3.2. Patient characteristics
Mean age of patients availing teledermatology services was 33.60 ± 16.99 years (range 7 days–96 years). Of 6125 patients, 3180 (51.9%) were males and 2945 (48.1%) were females. Majority of patients (n = 3657, 59.7%) were from outside city limits while 40.2% (n = 2461) were local. Average distance of patients' residence from the institute was 100.90 ± 171.77 km (range 0.1–2000 km). Mean time of road travel saved accordingly was calculated to be 135 ± 222.32 minutes (range 2–1259 minutes). Demographic details of study population are summarised in Table 1.
TABLE 1.
Demographic parameters of study population
| Characteristics | Values |
|---|---|
| Mean age | 33.60 ± 16.99 years (7 days–96 years) |
| Sex ratio | 1.079:1 |
| Mean duration of illness | 18.14 ± 34.81 months (1 day–420 months) |
| Mean distance to care | 100.90 ± 171.77 km (0.1–2000 km) |
| Mean travel time | 135 ± 222.32 minutes (2–1259 minutes) |
| Previous follow‐ups | 1914 (31.2%) |
| New registrations | 4211 (68.8%) |
3.3. Disease characteristics
While 1914 patients (31.2%) had been previously registered and had availed an in‐person outpatient consult any time prior to the onset of pandemic, majority of consults (n = 4211, 68.8%) were new registrations. Average duration of illness was 18.14 ± 34.81 months (range 1 day–420 months). Status of disease was assessed to be active in 4855 patients (79.3%), controlled on therapy in 854 patients (13.9%) and inactive in 415 patients (6.8%).
A definitive diagnosis could be ascertained in 5724 patients (93.45%). As a group, infectious dermatoses were the most common diagnosis, constituting 27.72% (n = 1587) of all cases. Fungal and ectoparasitic infections were diagnosed in 1118 patients (19.53%). Papulosquamous disorders (n = 753, 13.16%), eczematous disorders (n = 606, 10.59%), hair and nail disorders (n = 502, 8.77%) and dyschromias (n = 469, 8.19%) were next in frequency (Table 2). In‐person visit was recommended to 133 patients (2.2%). The purpose of the visit was an urgent need to establish a diagnosis (93 patients, 1.51%) and/or initiate/continue therapy in 40 patients (0.65%). Within each group, the proportion of patients requiring physical visit was highest for neoplasms (31.03%), followed by immunobullous disorders (5.60%) and leprosy (5.42%). Patients with acne and dermatophyte/ectoparasitic infections could be managed exclusively with teleconsultations.
TABLE 2.
Frequency of dermatoses in study population
| Diagnosis | Number of patients | Percentage |
|---|---|---|
| Fungal/ectoparasite infections | 1118 | 19.53 |
| Papulosquamous disorders | 753 | 13.16 |
| Dermatitis/eczematous disorders | 606 | 10.59 |
| Hair and nail disorders | 502 | 8.77 |
| Dyschromia/Pigmentary disorders | 469 | 8.19 |
| Urticaria | 436 | 7.62 |
| Acne vulgaris | 416 | 7.27 |
| Immunobullous disorders | 268 | 4.68 |
| Viral infections | 169 | 2.95 |
| Bacterial infections | 130 | 2.27 |
| Leprosy | 129 | 2.25 |
| Connective tissue diseases | 119 | 2.08 |
| Neoplastic disorders | 58 | 1.01 |
| Sexually transmitted disorders | 41 | 0.71 |
| Other | 510 | 8.90 |
| Total | 5724 | 100 |
3.4. Patient satisfaction
A total of 5229 patients could be contacted for feedback regarding their experience with teledermatology consultation. Nine hundred and fifty patients (18.18%) reported being very satisfied, 2230 patients (42.65%) were satisfied, 1749 patients (33.45%) were partially satisfied whereas 300 patients (5.70%) reported being unsatisfied with teledermatology services.
Level of satisfaction was found to be independent of age (Kendall's tau = −0.019), gender (Kendall's tau = −0.029) and distance to care (Kendall's tau = 0.014). Level of satisfaction was similar among new and previously registered patients. Highest levels of satisfaction were noted in patients of fungal/ectoparasitic infections and bacterial infections, in whom 69.83% and 65.38% patients, respectively, reported being either satisfied or very satisfied with the teleconsultation services.
Of 1914 patients who had had availed both, an in‐person outpatient consult prior to the onset of pandemic and a telemedicine consult during pandemic, 1842 could be contacted for a subjective comparison of teledermatology vis‐à‐vis in‐person visits. Majority of patients (n = 914, 49.62%) felt that in‐person visits were better, while 474 patients (25.73%) rated teledermatology more favorable. Four hundred and fifty one patients (24.48%) found the two modes of consultation comparable.
3.5. Physician experience
Thirty‐four dermatologists completed the assessment. When enquired about the number of teleconsultations after which they started feeling comfortable with providing teledermatology services, six physicians (17.6%) reported being comfortable after less than five teleconsults. Twelve physicians (35.3%) felt comfortable after 6 to 10 teleconsults and an equal number required more than 10 teleconsults to feel comfortable. Four physicians (11.8%) were not able to establish their comfort with providing teledermatology services at the end of October 2020.
Major challenges faced by physicians included difficulty in assessing morphology and topography of lesions (91.2%), higher time per consultation (82.4%), difficulty in establishing rapport (79.4%) and technical or connectivity issues (52.9%). Need for multiple rounds of communication, inability to perform additional testing and possibility of prescription misuse were highlighted by four physicians each. Most of the physicians (n = 28, 82.4%) felt the need to continue teledermatology services in the upcoming months. Physicians were asked to grade the ease of communication, convenience and satisfaction with provided services along with willingness to continue the services on a 10‐point Likert scale. Summary of the responses received is presented in Table 3.
TABLE 3.
Physician experience regarding teledermatology services on a 10‐point Likert scale
| Range | Mean | Median | |
|---|---|---|---|
| Satisfaction | 2–9 | 6.43 ± 1.81 | 7 |
| Ease of communication | 3–10 | 6.66 ± 1.84 | 7 |
| Convenience | 1–10 | 6.83 ± 2.35 | 7 |
| Willingness to continue teleconsultation post‐pandemic | 1–10 | 5.77 ± 2.90 | 7 |
4. DISCUSSION
During the novel coronavirus (COVID‐19) pandemic, the use of telemedicine services has dramatically surged in order to provide health care while maintaining least physical contact. This study is an attempt to audit and gain an insight into our experience with the teledermatology services that our department provided over a 6‐months‐duration.
A steady yet significant increase in number of patients utilizing telehealth services was seen throughout the study period, with an average number of 24 consultations per day in May that rose three folds to 78 daily consultations in October. This number, however, is significantly lower than the average number of outpatients seen physically by our center during the pre‐COVID era, underscoring reduced access to health care also noted by several other studies. 5 , 6
Demographic parameters showed similar distribution of males and female patients accessing teledermatology. While 31.2% patients were previously registered in the department during pre‐COVID times, 68.8% were new registrations. Patients registered from as far as 2000 km, highlighting the improved accessibility to health care. A retrospective review by Krueger et al. 7 also reported increased utilization of services by patients living out‐of‐state via teleconsultations as compared to in‐person visits.
We chose to conduct teleconsultation via WhatsApp, a social media app, as this platform is convenient, user friendly and widely utilised by the general population. A study compared the diagnostic agreement between the images obtained from social media and standard teledermatology services, and did not find a significant difference between the two groups regarding the percentage of accurate diagnosis. 8
In this study, a diagnosis could be ascertained online in 93.45% of cases. Accuracy of these diagnoses, however, could not be analysed, because we tried to limit in‐person visits to patients who urgently required it. Several studies have shown accuracy of teledermatology consults to be comparable to or slightly lower than in‐person visits, 9 , 10 although this may be dependent on provider experience. 11
In person visits were recommended to only 2.2% of cases, drastically cutting down the physical interactions as compared to the pre‐COVID era. Up to one‐third of patients with neoplasms required an in‐person visit, while none of the patients with acne, dermatophyte or ectoparasitic infections had to be seen in person. Previous studies have also reported conditions such as acne, atopic dermatitis, seborrheic dermatitis, xerosis and dermatophytosis to be particularly suited for telemedicine. 12 , 13 , 14 Two retrospective studies from Brazil reported high degree of accuracy with teledermatology in inflammatory dermatoses and moderate accuracy for neoplasms. 15 , 16
High levels of satisfaction with teleservices has been reported previously in patients having acne. 17 In this study, 62% of acne patients reported being satisfied or very satisfied with teleconsultation services.
In order to understand how patients perceived teledermatology in comparison to in‐person visits, the patients who had been following up at our center prior to the pandemic were asked their preferred mode of consultation. Approximately half of the patients preferred face‐to‐face visits. Many patients believe their condition cannot be sufficiently evaluated over the phone. Another advantage of in‐person visit includes better establishment of rapport, which may impact the compliance, a shortcoming reported by 79.4% of the physicians. This limitation can be minimised by use of synchronous teledermatology services using video calling, although poorer quality visuals might be an issue.
A survey conducted among 184 dermatologists in India reported that 85% of the responders were already providing teleconsultations and 70% were willing to continue them in the future. 18 In this study, 82.4% of the physicians agreed that the teledermatology services would continue in the following months, however, the average willingness to continue them on a Likert scale of 1–10 was only 5.77. Since ours is an academic institution, reduced learning opportunities might be a major factor impacting provider preferences. A survey from India reported that two‐thirds of the 260 responders did not have a system in place to train their residents. 5 Another study from California, however, reported more than twofold increase in residents' productivity ratio during teledermatology sessions as compared to regular clinics. 19
There are several shortcomings that need to be considered. The aim of teledermatology is to improve accessibility to health care. However, the underserved patients belonging to rural communities, older patients and populations with low literacy rates are less likely to adapt to this mode. 20 Telehealth may thus be widening health care disparity rather than bridging the gap. Both physical outpatient services and teleconsultations should hence be conducted side by side for wider accessibility to health care. Also, even though dermatologists may judge dermatoses such as acne to be well managed over teleconsultation, up to one‐third of patients may not be satisfied with the quality of care. Video visits and higher time per consultation may help in mitigating this issue. Unwillingness to be photographed and risk of privacy breach are other barriers to teledermatology. The Indian guidelines for telemedicine place the entire onus of maintaining records on the physician and do not provide any clarity on duration of data storage. Designing electronic medical records adapted for smartphones will aid in better documentation of smartphone‐based teleconsultations. Standardization of clinical photography for teleconsultation will also be helpful. This may be performed by providing a basic instruction manual to patients at the time of registration.
4.1. Strengths
Our study provides data of a large number of patients managed by teledermatology, delineating the patient characteristics and diseases best suited for management via teleconsultation.
4.2. Limitations
Limitations of our study include a single center retrospective design. Accuracy of diagnosis could not be commented upon, because majority of patients were not evaluated in person.
5. CONCLUSION
Overall, teledermatology is a valid alternative for in‐person dermatology visits during the current crisis for triaging as well as managing the patients. With the widespread vaccination drive and returning of hospital functions to normalcy, teleconsultations may be continued for patients with straightforward diagnosis and management. Further refinement of the process, however, is desirable.
CONFLICT OF INTEREST
The author declares that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
AUTHOR CONTRIBUTIONS
The manuscript has been read and approved by all the authors, the requirements for authorship have been met, and that each author believes that the manuscript represents honest work. Full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis: Dr. Sanjeev Handa and Dr. Hitaishi Mehta. Study concept and design: Sanjeev Handa, Anuradha Bishnoi, Keshavamurthy Vinay, Rahul Mahajan, Davinder Parsad. Acquisition, analysis, and interpretation of data: Sanjeev Handa, Hitaishi Mehta, Anuradha Bishnoi, Muthu Sendhil Kumaran. Drafting of the manuscript: Sanjeev Handa, Hitaishi Mehta, Anuradha Bishnoi. Critical revision of the manuscript for important intellectual content: Sanjeev Handa, Keshavamurthy Vinay, Rahul Mahajan, Tarun Narang, Muthu Sendhil Kumaran, Dipankar De, Sunil Dogra, Davinder Parsad. Statistical analysis: Sanjeev Handa, Hitaishi Mehta, Anuradha Bishnoi, Keshavamurthy Vinay, Rahul Mahajan. Administrative, technical, or material support: Tarun Narang, Muthu Sendhil Kumaran, Dipankar De, Sunil Dogra, Davinder Parsad. Study supervision: Sanjeev Handa, Sunil Dogra, Davinder Parsad.
Supporting information
Appendix S1. Supporting information.
ACKNOWLEDGMENTS
All authors have contributed equally and sufficiently.
Handa S, Mehta H, Bishnoi A, et al. Teledermatology during the COVID‐19 pandemic: Experience at a tertiary care centre in North India. Dermatologic Therapy. 2021;34(4):e15022. 10.1111/dth.15022
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Tensen E, van der Heijden JP, Jaspers MW, Witkamp L. Two decades of teledermatology: current status and integration in National Healthcare Systems. Curr Dermatol Rep. 2016;5:96‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. International Telecommunication Union (ITU) World Telecommunication/ICT Indicators Database . (2019) Mobile cellular subscriptions (per 100 people)—India. Available at: https://data.worldbank.org/indicator/IT.CEL.SETS.P2?locations=IN [Accessed 15th April 2021].
- 3. International Telecommunication Union (ITU) World Telecommunication/ICT Indicators Database . (2019) Mobile cellular subscriptions (per 100 people). Available at: https://data.worldbank.org/indicator/IT.CEL.SETS.P2 [Accessed 15th April 2021].
- 4. Ministry of Health and Family Welfare . (2020) Telemedicine Practice Guidelines. Available at: guidelines https://www.mohfw.gov.in/pdf/Telemedicine.pdf [Accessed 15th June 2021].
- 5. Bhargava S, Sarkar R. Impact of COVID‐19 pandemic on dermatology practice in India. Indian Dermatol Online J. 2020;11(5):712‐719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rogers MC, Wallace MM, Wheless L, Dewan AK. Impact of the COVID‐19 pandemic on inpatient dermatology consult patterns at a tertiary care hospital: a retrospective cohort study. J Am Acad Dermatol. 2021;84(1):156‐158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Krueger S, Leonard N, Modest N, et al. Identifying trends in patient characteristics and visit details during the transition to teledermatology: experience at a single tertiary referral center. J Am Acad Dermatol. 2020;S0190‐9622(20):33084–x. 10.1016/j.jaad.2020.11.040. [DOI] [PubMed] [Google Scholar]
- 8. Serhrouchni S, Malmartel A. Diagnostic agreement between telemedicine on social networks and teledermatology centers. Ann Fam Med. 2021;19(1):24‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Finnane A, Dallest K, Janda M, Soyer HP. Teledermatology for the diagnosis and management of skin cancer: a systematic review. JAMA Dermatol. 2017;153(3):319‐327. [DOI] [PubMed] [Google Scholar]
- 10. Lee JJ, English JC 3rd. Teledermatology: a review and update. Am J Clin Dermatol. 2018;19(2):253‐260. [DOI] [PubMed] [Google Scholar]
- 11. Bashshur RL, Shannon GW, Tejasvi T, Kvedar JC, Gates M. The empirical foundations of teledermatology: a review of the research evidence. Telemed J E Health. 2015;21(12):953‐979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Giavina Bianchi M, Santos A, Cordioli E. Dermatologists' perceptions on the utility and limitations of teledermatology after examining 55,000 lesions. J Telemed Telecare. 2021;27(3):166‐173. 10.1177/1357633X19864829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Giavina Bianchi M, Santos AP, Cordioli E. The majority of skin lesions in pediatric primary care attention could be managed by teledermatology. PLoS One. 2019;14(12):e0225479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Su MY, Smith GP, Das S. Trends in teledermatology use during clinic reopening after COVID‐19 closures. J Am Acad Dermatol. 2021;84(4):e213‐e214. 10.1016/j.jaad.2020.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Giavina‐Bianchi M, Azevedo MFD, Sousa RM, Cordioli E. Part II: accuracy of teledermatology in skin neoplasms. Front Med (Lausanne). 2020;7:598903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Giavina‐Bianchi M, Sousa R, Cordioli E. Part I: accuracy of teledermatology in inflammatory dermatoses. Front Med (Lausanne). 2020;7:585792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ruggiero A, Megna M, Annunziata MC, et al. Teledermatology for acne during COVID‐19: high patients' satisfaction in spite of the emergency. J Eur Acad Dermatol Venereol. 2020;34(11):e662‐e663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sharma A, Jindal V, Singla P, Goldust M, Mhatre M. Will teledermatology be the silver lining during and after COVID‐19? Dermatol Ther. 2020;33(4):e13643‐e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zakaria A, Maurer T, Amerson E. Impact of teledermatology program on dermatology resident experience and education Telemedicine and e‐Health. 2020. 10.1089/tmj.2020.0350. [DOI] [PubMed] [Google Scholar]
- 20. National Telecommunications and Information Administration . (2013) Exploring the digital nation: America's emerging online experience. Available at: https://www.ntia.doc.gov/files/ntia/publications/exploring_the_digital_nation_-_americas_emerging_online_experience.pdf [Accessed 15th April 2021].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


