Abstract
Background
Adherence to local standard guidelines is seen as a pragmatic way to measure and improve the quality of future prescribing in ambulatory care to reduce morbidity, mortality and healthcare costs.
Objectives
To evaluate adherence to the Ghana Standard Treatment Guidelines (STGs) for the empirical antibiotic treatment of ambulatory care patients with community-acquired pneumonia (CAP) in a region in Ghana and factors associated with it.
Methods
A cross-sectional survey was conducted using a checklist to collect data from the hospital electronic database, which included sociodemographic details, payment type and clinical information of all ambulatory patients attending Keta Municipal Hospital, diagnosed and managed for CAP from September 2018 to January 2019. Prescriptions were assessed for adherence to the Ghana STG based on choice of antibiotics. A χ2 test and multiple logistic regression were subsequently conducted.
Results
A total of 1929 patient records with diagnosis of CAP within the study period at the ambulatory clinic were identified. The overall rate of adherence to the Ghana STG was 32.50% (n = 627). From the patient records collected, 62.50% were female, 41.84% were children (0–12 years), and 97.15% had a valid national health insurance status. Adherence was associated with the duration of antibiotic prescribing, number of additional antibiotics prescribed and some patients’ clinical characteristics.
Conclusions
The rate of adherence to Ghana STG among the study population was low. Efforts must be made to train and encourage prescribers to follow empirical guidelines to reduce inappropriate selection of antibiotics in the ambulatory care settings.
Introduction
There are ongoing concerns across countries, especially among lower- and middle-income countries (LMICs), that inappropriate prescribing of antibiotics will increase antimicrobial resistance (AMR) rates, leading to increasing morbidity, mortality and costs.1–4 This is of particular concern in ambulatory care where the majority of antimicrobials are prescribed empirically.4–6 It is increasingly recognized that adherence to standard treatment guidelines (STGs), including guidelines that reserve the prescription of antibiotics such as those in the Watch or Reserve group of the WHO Access, Watch, Reserve (AWaRe) list, is seen as critical to improving the quality of antibiotic prescribing.7–9 There are concerns that the current WHO/International Network of Rational Use of Drugs (INRUD) criteria that are commonly used to assess the quality of prescribing in ambulatory care in LMICs do not necessarily measure the actual quality of prescribing exacerbated by the lack of diagnostic information.7,10,11 Consequently, adherence to local STGs is seen as a more pragmatic way to measure and improve future prescribing in ambulatory care.6,7,11,12 This measure has also been used to determine the quality of managing community-acquired pneumonia (CAP) and other infections in various hospitals,13–15 and involves matching the antibiotic prescribed with the indication.
Encouragingly, adherence to empirical antibiotic guidelines for managing patients with CAP in hospitals has reduced mortality and morbidity, shortened hospital length of stay and decreased healthcare costs.13,14 This is similar to the positive impact seen with the introduction of antimicrobial stewardship programmes (ASPs) in hospitals.16,17 However, there are concerns with adherence to guidelines, including those for CAP, in practice as adherence rates have generally been suboptimal.18–20 Documented reasons for poor adherence to STGs for respiratory problems include the poor socioeconomic status of patients and prescriber workloads.21–24 Previous studies conducted in this and other hospital settings in Ghana have shown that there has been good adherence to antimicrobial guidelines among patients managed in inpatient medical wards as well as adherence to ceftriaxone-specific guidelines in hospitals.21,22 However, there is a lack of evidence around current adherence to prescribing guidance for infections managed in ambulatory care in Ghana. This is important as Ghana has recently introduced a national action plan to improve future antimicrobial use to reduce AMR rates along with STGs.4,23 In addition, we are aware that whilst only 40% of patients in Ghana are currently covered by the National Health Insurance Scheme, the remainder are subject to 100% co-payment via out-of-pocket payments for their medicines, which could adversely affect usage patterns. The ultimate goal is universal healthcare among all citizens in Ghana mirroring the situation in Namibia and South Africa.24–26
The first edition of the Ghana STGs was published in 1988 to enhance prescribing, particularly in ambulatory care. Since then, six editions have been published with the latest being the 2017 edition. The STGs are evidence-based with a rigorous review process by the National Medicine Selection Committee, Ghana National Drug Programme and stakeholder engagement to engender consensus, credibility and acceptance of the final document.27,28 This is similar to processes in higher income countries and regions including Stockholm County Council in Sweden (Regional Health Authority) where robust evidence-based criteria, rigorous processes including the ability to question key personnel, strong conflict-of-interest statements and regular follow-up have ensured high adherence rates to recommended treatments and guidelines.29,30
Consequently, the objectives of this study were: firstly, to evaluate adherence to the latest Ghanaian STGs as adopted by the facility’s Drug and Therapeutic Committee (DTC) for empirical antibiotic treatment of ambulatory CAP patients in a region in Ghana; and secondly, to identify key factors associated with adherence to current guidelines to improve future care. CAP was chosen for this study as it is one of the top five causes of patients’ attendance to the hospital ambulatory clinic, and currently ranks as the third most common infectious disease leading to admissions that require antibiotic use.22 This makes CAP a suitable condition to study as any recommendation may have a cascading effect on improving the appropriate use of antibiotics in the ambulatory care clinic to reduce future morbidity and mortality.13,14
Methods
Study design and setting
A cross-sectional survey was conducted by extracting the medical records of all patients diagnosed with CAP and managed at the ambulatory care clinic of Keta Municipal Hospital (KMH) from September 2018 to January 2019 using the hospital’s electronic database.
We started with KMH as this is a leading public primary care hospital located in the Keta Municipality that lies at the southern part of the Volta region of Ghana. The Volta region covers an area of 20 570 square kilometres with a population of just over 2.1 million people (8.6% of the total population of Ghana).31 KMH is a government-owned primary healthcare facility with a 110 bed capacity providing general services, dental services, eye care services and mental health services to an average of 200 ambulatory patients who seek their services on a daily basis, as well as inpatient services. It is one of the top five facilities in the Volta region of Ghana,32 with 309 permanent staff as well as temporary staff comprising 4 junior medical officers, 1 paediatrician, 2 pharmacists and 17 pharmacy support staff and 157 nurses and midwives alongside 127 paramedics.22
Data collection
A checklist was developed based on information routinely collected from patients attending the ambulatory clinic using the hospital electronic database designed for prescribing and dispensing of medicines, called the Patient Clinical and Health Information System (PHIS). The PHIS software was instigated in the hospital to ensure data security and accessibility of information on prescribing and dispensed drugs where each patient is given a unique identifying number, and to aid drug and non-drug inventory. Retrospective data were collected from September 2018 to January 2019 to serve as part of the baseline information of the facility performance on the rational use of antimicrobials at the start of a 2 year Fleming Fund-supported project on antimicrobial stewardship in the facility with the support of Health Improvement Scotland.22 The type of information collected for this study was based on the medical records routinely collected for patients diagnosed with CAP, who reported to the ambulatory clinic and were captured in the PHIS. This included sociodemographic information incorporating age, gender, marital status, employment status and payment type, i.e. national health insurance (NHI) or 100% co-payment via cash payments. Clinical information comprising the diagnosis, extent of respiratory symptoms, duration of symptoms and primary antibiotic prescribed for pneumonia was also collected along with data on previous antibiotic use. However, other medicines prescribed for comorbid disorders and the type of disorder were not collected as this information could not be readily retrieved from the PHIS in a format that allowed for analysis.
A clinical pharmacist (D.O.E.) was trained to retrieve the data using the checklist. After the data entry, a detailed data audit process was conducted by a team of pharmacists to check for accuracy and consistency and any mistakes identified were corrected. All patients with a diagnosis of CAP who were managed empirically as ambulatory care patients within the study period were included in the study. There was no calculation of potential patient numbers for this study as there was no prior history. However, based on our experiences with inpatient studies in Ghana,22 and the envisaged number of patients that could potentially be sourced during the study period, we believed this study period would generate an acceptable number for analysis. Consequently, we included the medical records of all suitable patients for the review as long as they visited the ambulatory clinic of KMH within the study period and were diagnosed with CAP.
The study outcome measure was adherence to treatment recommended for CAP in the Ghana STG and adopted by KMH DTC. An antibiotic prescription for empirical treatment of CAP at the ambulatory clinic was considered to have adhered to the guideline when either the first-line choice of antibiotics, i.e. a choice between oral amoxicillin with or without azithromycin, or erythromycin if patient is penicillin allergic, or a second-line choice of oral cefuroxime for both adult and children or oral doxycycline for adults was made.33
Data analysis
All data collected were entered on Microsoft Excel version 2013 and imported into STATA version 14 (StataCorp, TX, USA) for analysis. The analysis comprised descriptive statistics as well as χ2 test of independence (or Fisher’s exact test where appropriate) to determine any association between the study outcome and the independent variables at a significance level of 95%.
Multivariate logistic regression was subsequently conducted by including all independent variables that had statistically significant association with the outcome variable in the bivariate analysis. This was done to determine factors associated with adherence to the guideline while adjusting for possible confounders.
Ethical clearance
No formal ethical exemption was sought as there was no direct patient contact, and all data were anonymized and kept securely locked at all times accessible only to the researchers. Administrative approval was however given by the management of the hospital. This is in line with our previous study on antimicrobial use in the hospital.22
Results
Overall, 1929 medical records of ambulatory patients diagnosed with CAP were considered over the 5 month study period from September 2018 to January 2019 (Table 1). The proportion of prescribers’ adherence to the Ghana STGs on the choice of antibiotics for CAP for ambulatory patients was 32.50% (n = 627/1929). In all, 62.50% of the patients whose records were reviewed were female, and most (41.84%) of them were young children (0–12 years) followed by 32.14% who were adults (19–60 years). Again, 73.70% were unmarried, 64.40% were unemployed and 97.15% had a valid NHI status.
Table 1.
Association between compliance with Ghana STGs for ambulatory pneumonia management and patients’ sociodemographic factors
| Variable | Total, n (%) | Compliance with STG |
P value | |
|---|---|---|---|---|
| yes, n (%) | no, n (%) | |||
| Gender | 0.547 | |||
| male | 723 (37.50) | 241 (33.3) | 482 (66.7) | |
| female | 1206 (62.50) | 386 (32.0) | 820 (68.0) | |
| Marital status | 0.000 | |||
| single | 1422 (73.70) | 509 (35.80) | 913 (64.20) | |
| married | 507 (26.30) | 118 (23.30) | 389 (76.70) | |
| Employment status | 0.000 | |||
| employed | 687 (35.60) | 168 (24.50) | 519 (75.55) | |
| unemployed | 1242 (64.40) | 459 (37.00) | 783 (63.04) | |
| Payment type | 0.229 | |||
| out-of-pocket | 55 (2.85) | 22 (40.00) | 33 (60.00) | |
| NHIS | 1874 (97.15) | 605 (32.30) | 1269 (67.70) | |
| Age category | 0.000 | |||
| 0–12 years | 807 (41.84) | 332 (41.14) | 475 (58.86) | |
| 13–18 years | 164 (8.50) | 68 (41.46) | 96 (58.54) | |
| 19–60 years | 620 (32.14) | 146 (23.55) | 474 (76.45) | |
| >60 years | 338 (17.52) | 81 (23.96) | 257 (76.04) | |
Variables with P values highlighted in bold showed statistically significant association with adherence to guideline after χ2 test.
NHIS, National Health Insurance Scheme.
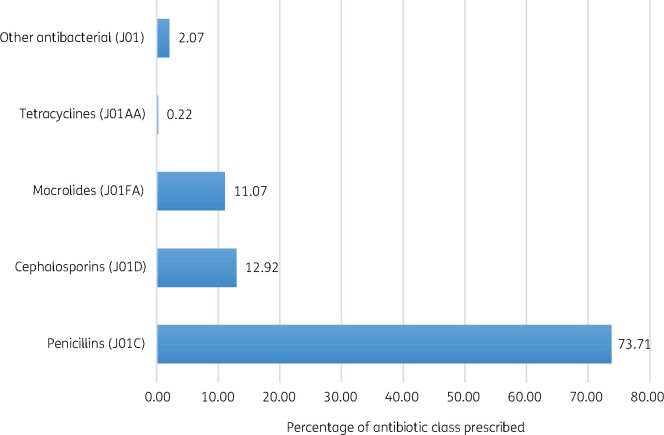
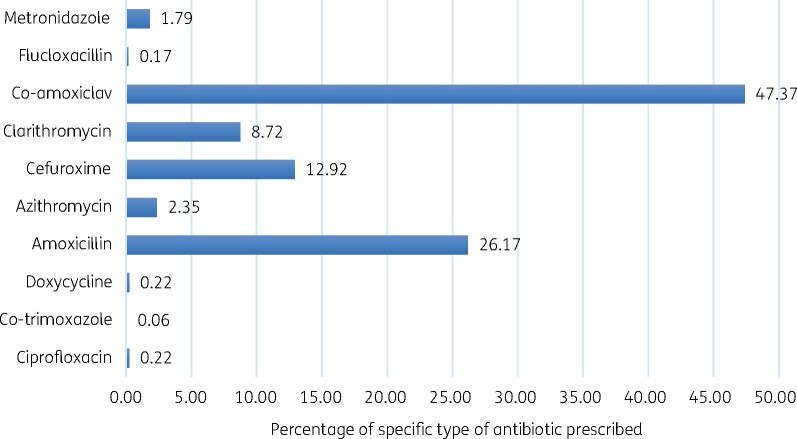
Of the study population, 7.31% representing 141 patients did not receive antibiotics as part of the treatment regimen for CAP. The major class of antibiotics that were prescribed for the ambulatory care management of CAP were the penicillins (73.71%; n = 1318) followed by cephalosporins (12.92%; n = 231) and macrolides (11.07%; n = 198) (Figure 1). The specific primary antibiotics that were frequently prescribed in descending order included co-amoxiclav, amoxicillin, cefuroxime and clarithromycin (Figure 2).
Figure 1.
Percentage of antibiotic classes prescribed for ambulatory management of CAP according to their ATC classification.
Figure 2.
Percentage of specific types of antibiotic prescribed for ambulatory management of CAP.
Bivariate analysis between guideline adherence and patients’ characteristics
Adherence to guideline was statistically associated with marital status (P < 0.0001), employment status (P < 0.0001), age category of the patient (P < 0.0001), class of primary antibiotic (P < 0.0001), number of additional antibiotics to the primary antibiotic (P < 0.0001), duration of antibiotic use (P < 0.0001), respiratory symptom complained of (P < 0.0001), documentation of temperature (P < 0.0001), documentation of blood pressure (P < 0.0001), documentation of heart rate (P < 0.0001) and chest X-ray radiograph requested (P < 0.0001) (Tables 1 and 2).
Table 2.
Association between compliance with Ghana STGs for ambulatory pneumonia management and patients’ clinical parameters
| Variable | Total, n (%) | Compliance with STGs |
P value | |
|---|---|---|---|---|
| yes, n (%) | no, n (%) | |||
| Guideline adherence | 1929 | 627 (32.5) | 1302 (67.5) | |
| Number of additional antibiotics | ||||
| none | 1636 (84.81) | 623 (38.1) | 1013 (61.9) | 0.000 |
| one | 289 (14.98) | 4 (1.4) | 285 (98.6) | |
| two | 4 (0.21) | 0 (0.0) | 4 (100.0) | |
| Duration of antibiotics | 0.000 | |||
| 1–7 days | 372 (19.28) | 203 (54.57) | 169 (45.43) | |
| 8–15 days | 1557 (80.72) | 424 (27.23) | 1133 (72.77) | |
| Previous exposure to antibiotic documented | 0.653 | |||
| yes | 42 (2.18) | 15 (35.71) | 27 (64.29) | |
| no | 1887 (97.82) | 612 (32.43) | 1275 (67.57) | |
| CURB-65 documentation | 0.488 | |||
| yes | 1 (0.05) | 0 (0) | 1 (100) | |
| no | 1928 (99.95) | 627 (32.52) | 1301 (67.48) | |
| Respiratory symptoms complained of | 0.000* | |||
| none | 368 (19.08) | 90 (24.46) | 278 (75.54) | |
| cough | 1482 (76.83) | 503 (33.94) | 979 (66.06) | |
| productive cough | 77 (3.99) | 33 (42.86) | 44 (57.14) | |
| nasal congestion | 2 (0.10) | 1 (50) | 1 (50) | |
| Temperature recorded | 0.000 | |||
| yes | 946 (49.04) | 373 (39.43) | 573 (60.57) | |
| no | 983 (50.96) | 254 (25.84) | 729 (74.16) | |
| Blood pressure recorded | 0.000 | |||
| yes | 1021 (52.93) | 247 (24.19) | 774 (74.81) | |
| no | 908 (47.07) | 380 (41.85) | 528 (58.15) | |
| Heart rate recorded | 0.000 | |||
| yes | 721 (37.38) | 188 (26.07) | 533 (73.93) | |
| no | 1208 (62.62) | 439 (36.34) | 769 (63.66) | |
| Respiratory rate recorded | 0.276 | |||
| yes | 141 (7.31) | 40 (28.37) | 101 (71.63) | |
| no | 1788 (92.69) | 587 (32.83) | 1201 (67.17) | |
| Chest X-ray requested | 0.000 | |||
| yes | 694 (35.98) | 181 (26.08) | 513 (73.92) | |
| no | 1235 (64.02) | 446 (36.11) | 789 (63.89) | |
| Full blood count requested | 0.358 | |||
| yes | 11 (0.57) | 5 (45.45) | 6 (54.55) | |
| no | 1918 (99.43) | 622 (32.43) | 1296 (67.57) | |
Variables with P values highlighted in bold showed statistically significant association with adherence to guideline after χ2 test and those with an asterisk (*) were obtained from Fisher’s exact test.
Multivariate logistic regression between guideline adherence and patient characteristics
Table 3 shows results of adjusted ORs, confidence intervals and P values from the assessment of the predictors of adherence to STG using all the statistically significant characteristics from the bivariate analysis (Table 2). Clinicians’ adherence to the STGs for ambulatory care management of CAP was independently predicted by the number of additional antibiotics prescribed, duration of the primary antibiotic and documentations of respiratory symptoms, blood pressure, chest X-ray radiograph requested and previous exposure to an antibiotic within the past three months.
Table 3.
Logistic regression between independent variables that showed statistically significant association and guideline adherence status
| Independent variables | aOR | 95% CI | P value |
|---|---|---|---|
| Number of additional antibiotics prescribed | |||
| none | 1.0 | ||
| one | 0.03 | 0.01–0.08 | 0.000 |
| two | 1.0 | ||
| Duration of prescription of primary antibiotic (days) | |||
| 1–7 | 1.0 | ||
| 8–15 | 0.33 | 0.25–0.42 | 0.000 |
| Previous exposure to antibiotics (<3 months) documented | |||
| no | 1.0 | ||
| yes | 2.41 | 1.09–5.33 | 0.029 |
| Respiratory symptom documented | |||
| none | 1.0 | ||
| cough | 1.29 | 0.96–1.72 | 0.086 |
| productive cough | 2.02 | 1.15–3.55 | 0.015 |
| nasal congestion | 6.40 | 0.39–106.41 | 0.195 |
| Blood pressure documented | |||
| no | 1.0 | ||
| yes | 0.39 | 0.23–0.68 | 0.001 |
| Chest X-ray request documented | |||
| no | 1.0 | ||
| yes | 0.71 | 0.55–0.91 | 0.007 |
Variables that did not show significant association after the logistic regression analysis—including patient age, marital status, employment status, temperature recorded and heart rate recorded—were excluded from the table above.
Variables with P values highlighted in bold showed statistically significant association with adherence to guideline (P < 0.05).
aOR, adjusted OR.
Discussion
Adherence to STGs has been shown to be an important strategic intervention to enhance the quality of prescribing with beneficial consequences, including a reduction in mortality and the cost of healthcare provision.6,7,15 The study showed that the rate of adherence to the locally adapted Ghana STGs for ambulatory care management of CAP was 32.5%. This is a concern given the high adherence rates to empirical guidelines on antimicrobial prescribing for inpatients seen in our earlier study in the same hospital.22 In addition, it falls short of the target of 80% adherence established by WHO in their INRUD criteria that has often been used by Governments and others in Botswana and Namibia when reviewing the performance of ambulatory care clinics.7,11,12 However, this low level of adherence is similar to studies conducted by Huijts et al. (2013)34 when CURB-65 severity classification for CAP was used as well as Salih et al. (2014).35 Non-adherence to guidelines has been observed to be both intentional and unintentional as many prescribers find it difficult to keep pace with rapidly changing advancements in pharmacotherapy coupled with busy clinics, inaccessible STGs, lack of training on appropriate use of guidelines, clinicians’ skepticism about scientific accuracy of guideline recommendations, issues about guidelines infringing on autonomy in clinical care, lack of auditing and follow-up, and sometimes an unwillingness to change well-established prescribing behaviours especially if linked to financial incentives.9,12,36–40 Having said this, we are aware that regular follow-up of guidelines, including benchmarking of adherence rates, enhances adherence rates in practice as seen in Scotland and Sweden.29,30,41 In addition, easy-to-follow and up-to-date guidelines, coupled with support systems for continuing education, enhances their use among African countries.12 It has been observed that regular involvement of pharmacists in clinical care in the hospitals in Ghana increased adherence rates in previous studies;21,22 however, this was lacking in ambulatory care. We believe that these documented reasons may have contributed to the observed low adherence rates; however, these were not assessed in this study. We will be following this up in future research projects.
However, one potential reason that may have accounted for the low level of adherence in our study may be due to prescribers’ reluctance to admit patients with severe symptoms due to a number of factors, including inconvenience and cost. This may have resulted in high prescribing rates of co-amoxiclav (Figure 2), an antibiotic that is not recommended by the Ghana STG for outpatient management of CAP, despite being reserved for inpatients. The high usage of co-amoxiclav for ambulatory patients with CAP may also be due to prescriber’s preference for antibiotics with a broader spectrum for empirical treatment. Overall, an appreciable number of patients (47.37%) received co-amoxiclav for CAP versus 26.17% who received amoxicillin. This is similar to observations by Gasson et al. (2018)6 who found that one of the commonest reasons for non-adherence to STGs is the prescribing of antibiotic that is not recommended for the diagnosis. In the Ghana STG, a high dose of oral amoxicillin is preferred as the first-line empirical choice for ambulatory care management of CAP while parenteral co-amoxiclav followed by its oral dosage form are reserved for inpatients based on their CURB-65 score34 as the patient’s condition improves and they can tolerate oral antibiotics. The reasons for the observed low adherence rates are still not fully clear and will be followed up. Encouragingly, the study showed a high rate (73.71%) of prescriptions for penicillins (mainly amoxicillin and co-amoxiclav), which were mainly broad spectrum for the management of CAP and belonged to the Access category of the WHO AWaRe classification of antibiotics (Figure 2). This observation is appropriate for empirical treatment due to the known spectrum nature of bacteria commonly implicated in CAP and the low association of this category of antibiotics with AMR development.13
The number of antibiotics prescribed and documentation of past exposure to antibiotics within 3 months were associated with STG adherence. The study showed that those who received more than one antibiotic, together with those who had had a past exposure to antibiotics within the past 3 months, were less likely to be prescribed STG-recommended antibiotics for ambulatory care management of their CAP. This finding is important because the STG recommends the prescription of amoxicillin (or erythromycin in penicillin-allergic patients) as first-line treatment and cefuroxime or doxycycline as second line treatment for CAP at the ambulatory clinic as STG adherent. This preferred stepwise use of antibiotics may t change depending on which of these options the patient has been exposed to within past three months. Prescribers who are aware of these essential requirements in the STGs are more likely to adhere to them, especially if prescribing practices are being regularly reviewed.29,41
Blood pressure (BP) was recorded in more than half of the patients and the rate of documentation of this patient vital was independently associated with adherence to the STG. This implies that prescribers may have used raw BP data in their clinical decisions instead of using it for CURB-65 score calculation since the documentation of the latter was relatively low. However, further studies are needed before we can make any definitive statements. Our study showed though that there was very poor recording of the CURB-65 score, which is of particular concern since the STG antibiotic recommendations are based on this score. This score is useful because it incorporates patients’ mental status, levels of blood urea nitrogen, respiratory rate, systolic blood pressure and age to determine the severity of CAP and therefore the choice of antibiotics. Chest X-rays were requested for about one-third of the patients with less than 30% of these being adherent to the Ghana STG, which is also a concern. This is because chest X-rays were most likely requested for patients with severe symptoms who were mostly prescribed co-amoxiclav instead of amoxicillin at the ambulatory clinic. These observations may partly explain why documentation of patients’ BP, heart rate and temperature by clinicians were associated with the choice of antibiotics for empirical treatment of ambulatory patients with CAP (Table 2).
Other important patient data were included in the study such as marital status, employment status, and payment type as they partly influence the sociocultural and economic status of the patient. These were included because some studies have shown how socioeconomic status (SES) of patients may influence patients’ early access to healthcare, especially those in LMICs.42–44 A prescriber’s choice of antibiotics may therefore be guided by issues of affordability.45 It has been observed that patients may be given guideline-recommended antibiotics usually covered by NHI in Ghana to reduce cost barriers to access of care and medicines while those with high SES may be prescribed antibiotics outside of guidelines which are sometimes originators to be purchased out-of-pocket.39,46–48 However, our study showed that these SES factors did not independently predict prescribers’ choice of antibiotics despite a high percentage of co-payments observed among patients in Ghana having valid NHI.
We acknowledge a number of limitations with this study mainly due to the nature of data collection and the non-availability of some pertinent information in the patient medical records for analysis. These include the inability to collect details of the type of prescribers to understand the rationale behind their choice of antibiotics, the retrospective nature of the study, the lack of data on the availability of the recommended antibiotics within this public healthcare facility, co-morbidities and the lack of estimation of the sample size. Having said this, we believe the large sample size reported provides important cross-sectional data regarding antibiotic prescribing practices and associated factors in ambulatory care within an African country with concerns with AMR. Further studies though delineating these factors are needed.
Conclusions
The rate of adherence to Ghana STGs among the study population was suboptimal compared with WHO/INRUD guidance as well as guidance from other African countries. Adherence was associated with the duration of the primary antibiotic, number of additional antibiotics prescribed and the documentation of patients’ BP, respiratory symptoms, chest X-ray requests and previous exposure to antibiotics.
Prescribers must be trained and encouraged to be conversant with agreed STGs to improve future antibiotic prescribing. Alongside this, barriers to their acceptance and utilization must be ascertained and addressed to reduce future inappropriate selection of antibiotics for the empirical management of CAP, especially in ambulatory care.
Funding
This study was conducted as part of our routine work.
Transparency declarations
None to declare.
References
- 1. Founou RC, Founou LL, Essack SY.. Clinical and economic impact of antibiotic resistance in developing countries: a systematic review and meta-analysis. PLoS One 2017; 12: e0189621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tadesse BT, Ashley EA, Ongarello S. et al. Antimicrobial resistance in Africa: a systematic review. BMC Infect Dis 2017; 17: 616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jinks T, Lee N, Sharland M. et al. A time for action: antimicrobial resistance needs global response. Bull World Health Organ 2016; 94: 558-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Godman B, Haque M, McKimm J. et al. Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: findings and implications for the future. Curr Med Res Opin 2020; 36: 301–27. [DOI] [PubMed] [Google Scholar]
- 5. Costelloe C, Metcalfe C, Lovering A. et al. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ 2010; 340: c2096. [DOI] [PubMed] [Google Scholar]
- 6. Gasson J, Blockman M, Willems B.. Antibiotic prescribing practice and adherence to guidelines in primary care in the Cape Town Metro District, South Africa. S Afr Med J 2018; 108: 304–10. [DOI] [PubMed] [Google Scholar]
- 7. Niaz Q, Godman B, Massele A. et al. Validity of World Health Organisation prescribing indicators in Namibia's primary healthcare: findings and implications. Int J Qual Health Care 2019; 31: 338–45. [DOI] [PubMed] [Google Scholar]
- 8. Klein EY, Milkowska-Shibata M, Tseng KK. et al. Assessment of WHO antibiotic consumption and access targets in 76 countries, 2000-15: an analysis of pharmaceutical sales data. Lancet Infect Dis 2021; 21: 107–15. [DOI] [PubMed] [Google Scholar]
- 9. Matsitse TB, Helberg E, Meyer JC. et al. Compliance with the primary health care treatment guidelines and the essential medicines list in the management of sexually transmitted infections in correctional centres in South Africa: findings and implications. Expert Rev anti Infect Ther 2017; 15: 963–72. [DOI] [PubMed] [Google Scholar]
- 10. Ofori-Asenso R, Brhlikova P, Pollock AM.. Prescribing indicators at primary health care centers within the WHO African region: a systematic analysis (1995-2015.). BMC Public Health 2016; 16: 724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mashalla Y, Setlhare V, Massele A. et al. Assessment of prescribing practices at the primary healthcare facilities in Botswana with an emphasis on antibiotics: findings and implications. Int J Clin Pract 2017; 71: e13042. [DOI] [PubMed] [Google Scholar]
- 12. Niaz Q, Godman B, Campbell S. et al. Compliance to prescribing guidelines among public health care facilities in Namibia; findings and implications. Int J Clin Pharm 2020; 42: 1227–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lui G, To HKW, Lee N. et al. Adherence to treatment guideline improves patient outcomes in a prospective cohort of adults hospitalized for community-acquired pneumonia. Open Forum Infect Dis 2020; 7: ofaa146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Adler N, Weber H, Gunadasa I. et al. Adherence to therapeutic guidelines for patients with community-acquired pneumonia in Australian hospitals. Clin Med Insights Circ Respir Pulm Med 2014; 8: 17–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wathne JS, Harthug S, Kleppe LKS. et al. The association between adherence to national antibiotic guidelines and mortality, readmission and length of stay in hospital inpatients: results from a Norwegian multicentre, observational cohort study. Antimicrob Resist Infect Control 2019; 8: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nathwani D, Varghese D, Stephens J. et al. Value of hospital antimicrobial stewardship programs [ASPs]: a systematic review. Antimicrob Resist Infect Control 2019; 8: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Huebner C, Flessa S, Huebner NO.. The economic impact of antimicrobial stewardship programmes in hospitals: a systematic literature review. J Hosp Infect 2019; 102: 369–76. [DOI] [PubMed] [Google Scholar]
- 18. Triantafyllidis C, Kapordelis V, Papaetis GS. et al. Guidelines adherence for patients with community acquired pneumonia in a Greek hospital. Eur Rev Med Pharmacol Sci 2012; 16: 1–9. [PubMed] [Google Scholar]
- 19. Almatar M, Peterson GM, Thompson A. et al. Clinical pathway and monthly feedback improve adherence to antibiotic guideline recommendations for community-acquired pneumonia. PLoS One 2016; 11: e0159467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Grigoryan L, Zoorob R, Wang H. et al. Low concordance with guidelines for treatment of acute cystitis in primary care. Open Forum Infect Dis 2015; 2: 159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Afriyie DK, Amponsah SK, Dogbey J. et al. A pilot study evaluating the prescribing of ceftriaxone in hospitals in Ghana: findings and implications. Hosp Pract (1995) 2017; 45: 143–9. [DOI] [PubMed] [Google Scholar]
- 22. Afriyie DK, Sefah IA, Sneddon J. et al. Antimicrobial point prevalence surveys in two Ghanaian hospitals: opportunities for antimicrobial stewardship. JAC Antimicrob Resist 2020; 2: dlaa001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ghana Ministry of Health, Ministry of Food and Agriculture, Ministry of Environment, Science, Technology and Innovation, Ministry of Fisheries and Aquaculture Development. Ghana National Action Plan for Antimicrobial Use and Resistance: 2017. - 2021. http://www.moh.gov.gh/wp-content/uploads/2018/04/NAP_FINAL_PDF_A4_19.03.2018-SIGNED-1.pdf.
- 24. Nashilongo MM, Singu B, Kalemeera F. et al. Assessing adherence to antihypertensive therapy in primary health care in Namibia: findings and implications. Cardiovasc Drugs Ther 2017; 31: 565–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Meyer JC, Schellack N, Stokes J. et al. Ongoing initiatives to improve the quality and efficiency of medicine use within the public healthcare system in South Africa; a preliminary study. Front Pharmacol 2017; 8: 751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ankrah D, Hallas J, Odei J. et al. A review of the Ghana National Health Insurance Scheme claims database: possibilities and limits for drug utilization research. Basic Clin Pharmacol Toxicol 2019; 124: 18–27. [DOI] [PubMed] [Google Scholar]
- 27. Koduah A, Asare BA, Gavor E. et al. Use of evidence and negotiation in the review of national standard treatment guidelines and essential medicines list: experience from Ghana. Health Policy Plan 2019; 34: 104–20. [DOI] [PubMed] [Google Scholar]
- 28. Sinclair D, Gyansa-Lutterodt M, Asare B. et al. Integrating global and national knowledge to select medicines for children: the Ghana National Drugs Programme. PLoS Med 2013; 10: e1001449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gustafsson LL, Wettermark B, Godman B. et al. The ‘wise list’- a comprehensive concept to select, communicate and achieve adherence to recommendations of essential drugs in ambulatory care in Stockholm. Basic Clin Pharmacol Toxicol 2011; 108: 224–33. [DOI] [PubMed] [Google Scholar]
- 30. Eriksen J, Gustafsson LL, Ateva K. et al. High adherence to the ‘Wise List’ treatment recommendations in Stockholm: a 15-year retrospective review of a multifaceted approach promoting rational use of medicines. BMJ Open 2017; 7: e014345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ghana Statistical Service. 2010. Population and Housing Census Report. https://www2.statsghana.gov.gh/docfiles/publications/2010phc_monograph_women_&_men_in_Gh.pdf.
- 32. USAID. District Health Information Management System (DHIMS)2 Digitization. 2016. https://partnerships.usaid.gov/partnership/district-health-information-management-system-dhims2-digitization.
- 33. Ministry of Health, Republic of Ghana. Ghana Standard Treatment Guidelines (2nd edition). 2017. https://www.moh.gov.gh/wp-content/uploads/2020/07/GHANA-STG-2017-1.pdf.
- 34. Huijts SM, van Werkhoven CH, Boersma WG. et al. Guideline adherence for empirical treatment of pneumonia and patient outcome. Treating pneumonia in the Netherlands. Neth J Med 2013; 71: 502–7. [PubMed] [Google Scholar]
- 35. Salih KEM, Bilal JA, Alfadeel MA. et al. Poor adherence to the World Health Organization guidelines of treatment of severe pneumonia in children at Khartoum, Sudan. BMC Res Notes 2014; 7: 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bos JM, Natsch S, van den Bemt PMLA. et al. A multifaceted intervention to reduce guideline non-adherence among prescribing physicians in Dutch hospitals. Int J Clin Pharm 2017; 39: 1211–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mashalla YJ, Sepako E, Setlhare V. et al. Availability of guidelines and policy documents for enhancing performance of practitioners at the Primary Health Care (PHC) facilities in Gaborone, Tlokweng and Mogoditshane, Republic of Botswana. J Public Health Epidemiol 2016; 8: 127–35. [Google Scholar]
- 38. Rezal RS, Hassali MA, Alrasheedy AA. et al. Prescribing patterns for upper respiratory tract infections: a prescription-review of primary care practice in Kedah, Malaysia, and the implications. Expert Rev Anti Infect Ther 2015; 13: 1547–56. [DOI] [PubMed] [Google Scholar]
- 39. Hassali MA, Kamil TK, Md Yusof FA. et al. General practitioners' knowledge, attitude and prescribing of antibiotics for upper respiratory tract infections in Selangor, Malaysia: findings and implications. Expert Rev Anti Infect Ther 2015; 13: 511–20. [DOI] [PubMed] [Google Scholar]
- 40. Md Rezal RS, Hassali MA, Alrasheedy AA. et al. Physicians' knowledge, perceptions and behaviour towards antibiotic prescribing: a systematic review of the literature. Expert Rev Anti Infect Ther 2015; 13: 665–80. [DOI] [PubMed] [Google Scholar]
- 41. Leporowski A, Godman B, Kurdi A. et al. Ongoing activities to optimize the quality and efficiency of lipid-lowering agents in the Scottish national health service: influence and implications. Expert Rev Pharmacoecon Outcomes Res 2018; 18: 655–66. [DOI] [PubMed] [Google Scholar]
- 42. Aregbeshola BS, Khan SM.. Out-of-pocket payments, catastrophic health expenditure and poverty among households in Nigeria 2010. Int J Health Policy Manag 2018; 7: 798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kastor A, Mohanty SK.. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: do Indian households face distress health financing? PLoS One 2018; 13: 0196106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rahman MM, Zhang C, Swe KT. et al. Disease-specific out-of-pocket healthcare expenditure in urban Bangladesh: a Bayesian analysis. PLoS One 2020; 15: e0227565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fadare JO, Enwere OO, Adeoti AO. et al. Knowledge and attitude of physicians towards the cost of commonly prescribed medicines: a case study in three Nigerian healthcare facilities. Value Health Reg Issues 2020; 22: 68–74. [DOI] [PubMed] [Google Scholar]
- 46. Tiroyakgosi C, Matome M, Summers E. et al. Ongoing initiatives to improve the use of antibiotics in Botswana: University of Botswana symposium meeting report. Expert Rev Anti Infect Ther 2018; 16: 381–4. [DOI] [PubMed] [Google Scholar]
- 47. Dallas A, Magin P, Morgan S. et al. Antibiotic prescribing for respiratory infections: a cross-sectional analysis of the ReCEnT study exploring the habits of early-career doctors in primary care. Fam Pract 2015; 32: 49–55. [DOI] [PubMed] [Google Scholar]
- 48. Soleymani F, Godman B, Yarimanesh P. et al. Prescribing patterns of physicians working in both the direct and indirect treatment sectors in Iran; findings and implications. J Pharm Health Serv Res 2019; 10: 407–13. [Google Scholar]