Abstract
Background
Community pharmacy staff have an opportunity to play a pivotal role in antimicrobial stewardship (AMS) due to their expertise in medicines and accessibility to patients.
Objectives
To develop and test the feasibility of a pharmacy AMS intervention (PAMSI) to increase community pharmacy staff’s capability, opportunity and motivation to check antibiotic appropriateness and provide self-care and adherence advice when dispensing antibiotics.
Methods
The PAMSI was centred around an Antibiotic Checklist, completed by patients and pharmacy staff, to facilitate personalized advice to the patient, based on their reported knowledge. An educational webinar for staff and patient-facing materials were also developed. Staff and patients completing Antibiotic Checklists were invited to provide feedback via questionnaires.
Results
In February 2019, 12 community pharmacies in England trialled the intervention. Forty-three pharmacy staff evaluated the educational webinar and reported increases in their understanding, confidence, commitment and intention to use the tools provided to give adherence and self-care advice. Over 4 weeks, 931 Antibiotic Checklists were completed. Staff reported being more focused on giving advice and able to address patients’ knowledge gaps (mainly: likely symptom duration; alcohol and food consumption advice; possible side effects from antibiotics; returning unused antibiotics to the pharmacy), resulting in increased self-reported effective and meaningful conversations.
Conclusions
Implementation of a PAMSI is feasible and effectively promotes AMS. Pharmacy staff and commissioners should consider this within their AMS plans. An optional digital format of the Antibiotic Checklist should be explored, for patients who are not collecting their antibiotic prescriptions themselves, and to save printing costs.
Introduction
Antibiotic resistance is driven by the overuse and inappropriate use of antibiotics, including taking the wrong kind of antibiotic, not using them as directed or using them at inappropriate doses.1 Despite reductions in antibiotic use, England continues to dispense twice as many as the lowest-using country in Europe,2 and antibiotic-resistant infections continue to increase.2 The UK’s 2019–24 antimicrobial resistance (AMR) national action plan focuses on three key ways of tackling AMR: reducing the need for and unintentional exposure to antibiotics; optimizing use of antibiotics; and investing in innovation, supply and access.3 In 2018, 80% of antibiotics were prescribed in the community,4 highlighting the need for antibiotic stewardship in the community and primary care settings.
As about 1.6 million people visit a pharmacy in England daily,5 pharmacy staff are among the most accessible healthcare professionals,6 with an opportunity to play a pivotal role in antimicrobial stewardship (AMS).7 Pharmacy staff believe that they have a role in tackling AMR, through educating the general public and by advising patients on effective self-care treatments for common infections, appropriateness of antibiotics, antibiotic adherence and the negative consequences of using antibiotics incorrectly.7 Supporting EU guidelines on prudent use of antimicrobials,8 recommendations for AMS and interventions in community pharmacy include the following:
Increasing the capability of pharmacy staff to fulfil their AMS role, through education and training.
Increasing the opportunity for pharmacy staff to give advice, by providing details of diagnosis so that staff can check the antibiotic appropriateness, tailor patient advice, and ensure easy access to relevant patient-facing materials.
Motivating staff by giving feedback about their patient advice and informing them how their adherence and self-care advice can help patients get better more quickly, prevent treatment failure and re-infection, and reduce antibiotic use and AMR.7
The UK’s Community Pharmacy Contractual Framework for 2019–20 to 2023–24 lays out priorities for a clinical future in a new context, covering urgent care, prevention, medicines optimization and safety.9 As the regulations for AMS in the community continue to evolve, and optimal stewardship strategies are defined, pharmacists must be leaders in the implementation of these programmes,8,10 but require support to do so. Much of the support, to date, has focused on educating patients about when antibiotics are appropriate and reducing inappropriate prescribing. This is covered in the national Keep Antibiotics Working11 and Antibiotic Guardian12 campaigns, and Treat Antibiotics Responsibly: Guidance, Education, Tools (TARGET).13 However, there is a gap in support at the other end of the community pathway, when an antibiotic has been prescribed.
Aim
To increase community pharmacy staff’s capability, opportunity and motivation to check antibiotic appropriateness and provide self-care and adherence advice to patients/carers collecting antibiotics.
Materials and methods
Intervention development
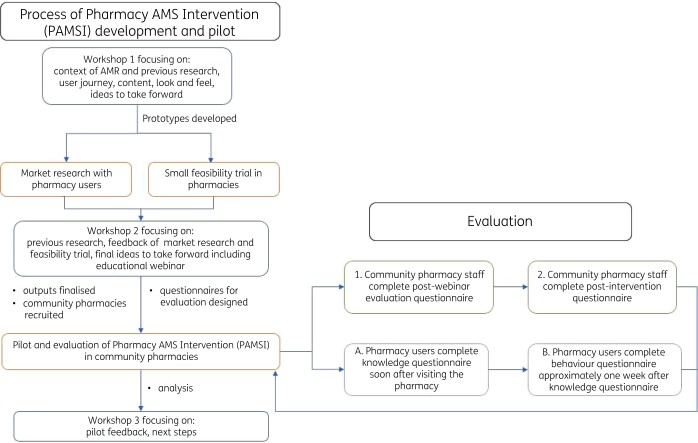
The pharmacy AMS intervention (PAMSI) was based on: the contents of the Royal Pharmaceutical Society’s AMS checklist;14 qualitative research that identified gaps in community pharmacy staff’s capability, opportunity and motivation (COM) to provide AMS advice;7 and ideas developed at an Information Design and Architecture in Persuasive Pharmacy Space: combating AMR (IDAPPS) workshop.15 The intervention was development over three workshops through 2018–19, involving community pharmacists from independent and large chain pharmacies, pharmacy users of different ages and genders, behavioural researchers, information designers, health literacy experts and AMR experts (Figure 1). Following the first workshop and the production of the initial prototypes, market research was conducted with pharmacy users, and four community pharmacies trialled the Antibiotic Checklist to assess feasibility of use in daily practice. The pilot intervention components and feedback were discussed at the second workshop, finalized and then evaluated in community pharmacies within one locality.
Figure 1.
Process of intervention development, pilot and evaluation.
PAMSI
Underpinned by the capability, opportunity, motivation and behaviour (COM-B) model,16,17 the PAMSI included the following:
A 20 min educational webinar to give pharmacy staff the capability and motivation to check antibiotic appropriateness and provide self-care and adherence advice to patients/carers collecting antibiotics (Appendix S1, available as Supplementary data at JAC-AMR Online). This covered the importance of AMS for pharmacy staff, and how the Antibiotic Checklist could be used in their pharmacy with the other reinforcing patient-facing materials.
-
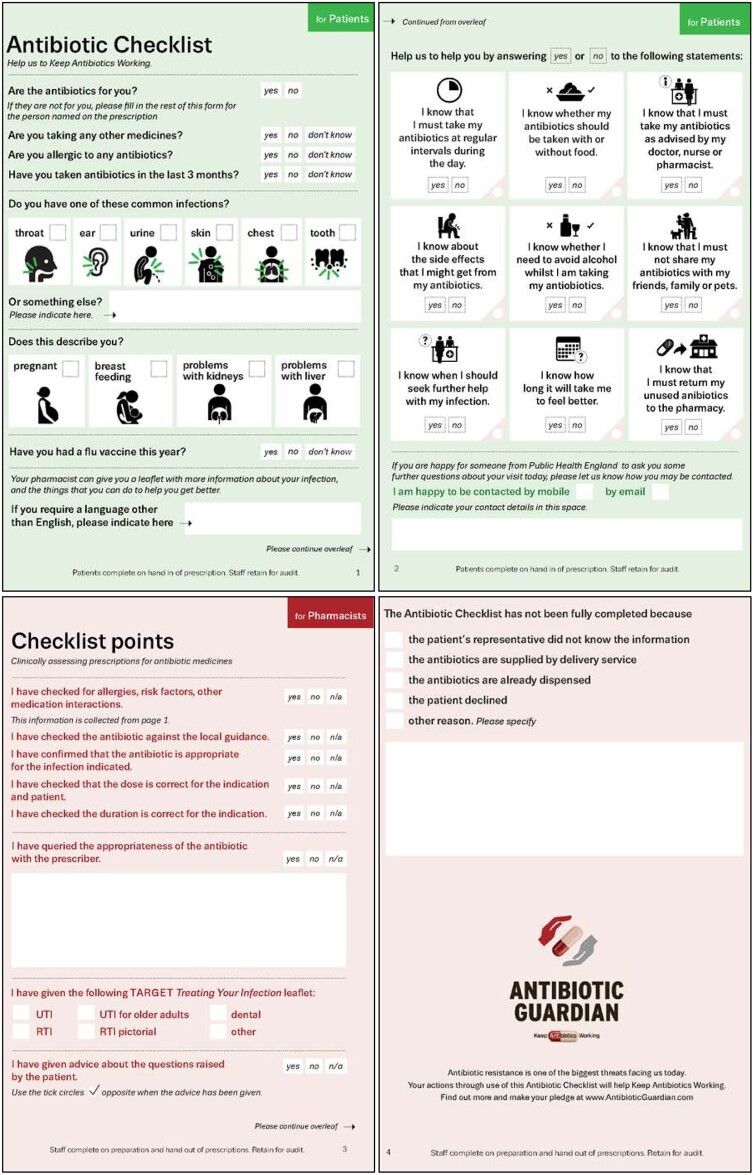
An Antibiotic Checklist to give pharmacy staff the capability and opportunity to check antibiotic appropriateness and provide self-care and adherence advice tailored to the individual patient and antibiotic (Figure 2). The Checklist was mainly tick boxes next to simple sentences with patient-friendly graphics describing the text. The A5 folded paper Antibiotic Checklist was designed to fit into the prescription baskets used by most pharmacies and followed the antibiotic prescription’s journey from hand-in to dispensing.
Upon handing in the antibiotic prescription, the patient/carer completed page 1—patient history, e.g. infection, previous antibiotic use, risk factors—and page 2—patient/carer knowledge on antibiotic use.
Upon dispensing, the pharmacist completed page 3—using the user information collected on page 1, to report if they had checked for allergies, risk factors and interactions, checked the antibiotic dose and duration against guidance, or needed to query the antibiotic with the prescriber.
Upon handing out the antibiotic, the pharmacy staff completed page 2—to give verbal antibiotic advice tailored to reported knowledge gaps ticked by patients/carers and infection-specific self-care advice to prevent future infections—and page 3—to tick which (if any) patient information leaflet was shared with the patient/carer. The respiratory, urinary, dental or children’s leaflets freely available from www.rcgp.org.uk/TARGETantibiotics13 supported the verbal adherence and self-care advice.
Other patient and staff AMS reinforcing materials, which included posters, shelf signs, counter mats and prescription bag stickers. These gave the opportunity to share key capability and motivation messages such as: always taking antibiotics as advised; not sharing or keeping unused antibiotics; and returning unused antibiotics to the pharmacy.
Feedback to pharmacy staff about percentage of Antibiotic Checklist completion in their pharmacy and follow-up data from pharmacy users after visiting the pharmacy.
Figure 2.
Antibiotic Checklist designed to follow the prescription’s journey and personalize the patient’s adherence advice.
Feasibility of PAMSI implementation
Recruitment of pharmacies
In January 2019, the Local Pharmaceutical Committee (LPC) used PharmOutcomes (a web-based system that helps community pharmacies provide services more effectively and makes it easier for commissioners to audit and manage these services)18 to invite all 111 community pharmacy teams in one locality in England to express interest in testing an intervention to support patients in the appropriate use of antibiotics. A researcher rang each pharmacist that responded, to give an overview of the intervention, answer questions and collect informed consent to participate.
Data collection
Antibiotic Checklist
For 4 weeks, a researcher visited each participating pharmacy, weekly, to answer staff questions, collect completed Antibiotic Checklists and replenish intervention resources. Weekly, pharmacy staff also reported on the total number of antibiotics dispensed. These data were used to calculate the percentage of prescriptions an Antibiotic Checklist was completed for.
Questionnaires
Four electronic questionnaires were used to evaluate and collect feedback on feasibility and acceptability of the intervention, in practice. The questions were generally tick boxes with free-text comment boxes requesting more participant feedback.
Staff questionnaires Post-webinar staff Questionnaire 1 (Appendix S2) was used to assess learning and provide webinar feedback and reflection on actions they may take forward following the webinar.
Post-intervention staff Questionnaire 2 (Appendix S3) was based on a conceptual framework for implementation fidelity;19 this questionnaire aimed to assess how well the educational webinar and supporting tools facilitated community pharmacy staff in their various AMS roles.
Upon completion of each questionnaire, community pharmacy staff were offered a certificate to evidence continuing professional development (CPD).
Pharmacy user questionnaires Pharmacy user Questionnaire A (Appendix S4), completed soon after visiting the community pharmacy, was designed to assess knowledge about how to take antibiotics (capability) and intention to follow pharmacy staff’s advice (motivation), essential components of the intervention.
Pharmacy user Questionnaire B (Appendix S5), completed approximately a week after Questionnaire A, was designed to assess patients’ antibiotic adherence behaviour.
When completing the Antibiotic Checklist, pharmacy users were given the opportunity to provide their contact details (e-mail or mobile number) to be followed up about their pharmacy visit. Weekly, the patients/carers who had provided contact details were sent a link to complete Questionnaire A. At questionnaire completion, pharmacy users were offered a £10 high street voucher and asked to indicate whether they could be contacted again to complete Questionnaire B; they were not offered any further financial incentive. Non-responders to e-mails or text messages were given one reminder.
Data analysis
Antibiotic Checklist data were manually inputted using Epidata software. Questionnaire data from SelectSurvey and the Antibiotic Checklist data were exported to Excel for descriptive analysis.
Ethics
The study design was reviewed and approved by the PHE Research Ethics and Governance Group (REGG) (R&D Ref: NR0147).
Results
Pharmacy recruitment
Fifteen percent (17/111) of community pharmacies responded to the expression of interest; 14% (15/111) gave informed consent to test the PAMSI in their pharmacy. During the intervention period, two pharmacies formally withdrew, and one did not respond throughout. Reasons not to participate or to withdraw included lack of funding, workload pressure and that the webinar was too quiet to listen to in the busy pharmacy. Therefore, 11% (12/111) of pharmacies in one locality trialled the intervention. These included a mixture of independent, multiple, rural and urban pharmacies. Appendix S6 shows the characteristics of the participating pharmacies.
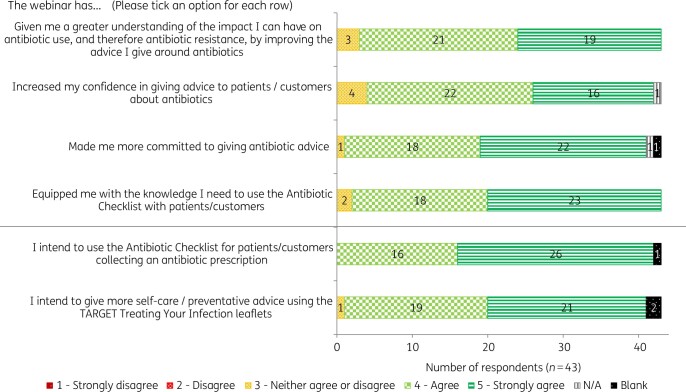
Educational webinar
Forty-three pharmacy staff (15 pharmacists, 2 pre-registration trainee pharmacists, 5 healthcare counter staff, 17 dispensary staff, 2 technicians, 1 pharmacy manager and 1 pharmacy assistant) watched and evaluated the educational webinar. Community pharmacy staff reported that the webinar increased their understanding, confidence, commitment and intention to use the tools provided to give adherence and self-care advice to patients/carers collecting antibiotics (Figure 3).
Figure 3.
Community pharmacy staff’s responses to post-webinar evaluation questionnaire (n = 43).
When asked to describe how the webinar could be improved, responses included shortening the length, improving the sound quality and hosting on a platform that is not restricted in the community pharmacy.
Antibiotic Checklist completion
In one month, 931 Antibiotic Checklists were completed for an average of 40% (53/133) of antibiotics dispensed (range of 3%–100%; 24–302 antibiotics dispensed in each pharmacy). Staff from one pharmacy gave informal feedback that they had put the Antibiotic Checklists by the front counter, to act as a reminder to use them when a patient/carer presented with an antibiotic prescription. Page 1 of the Antibiotic Checklist was completed by 756/931 (81%) patients/carers at hand-in and the antibiotic indication was reported by 701/756 (93%): 49% (340/701) reported a respiratory tract infection; 22% (157/701) urinary tract infection; 14% (98/701) dental infection; and 9% (62/701) skin infection (Table 1).
Table 1.
Indication reported on Antibiotic Checklist by patient/carer (N = 701)
| Indication | Number of responses (n) | Percentage |
|---|---|---|
| Respiratory tract infection | 340 | 49 |
| throat | 114 | 16 |
| ear | 62 | 9 |
| chest | 194 | 28 |
| Urine | 157 | 22 |
| Skin | 62 | 9 |
| Tooth | 98 | 14 |
| Other | 112 | 16 |
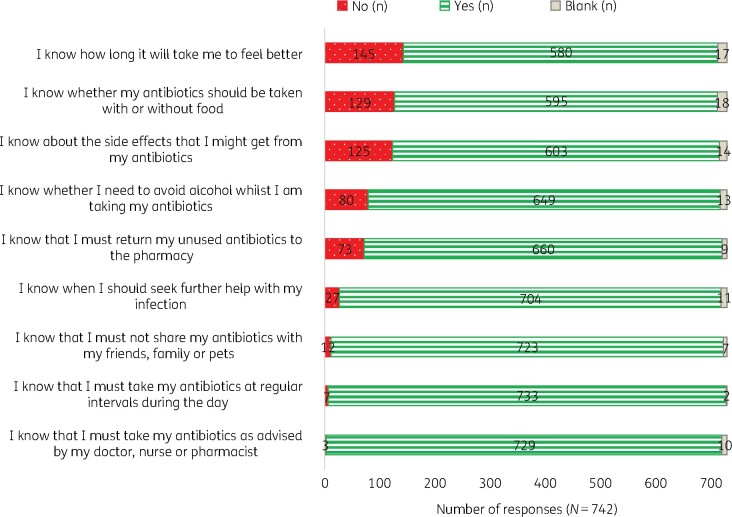
Reported patient/carer antibiotic knowledge and adherence behaviour
Antibiotic knowledge (Figure 2, page 2) was completed by 742/931 (80%) patients/carers: 60% (446/742) indicated that ‘yes’, they already knew about the nine topics. The topics that more patients/carers reported not knowing included: how long it would take them to feel better (20% did not know; 145/742); whether they should take their antibiotics with or without food (17%; 129/742); side effects they might get (17%; 125/742); whether they needed to avoid alcohol whilst taking their antibiotics (11%; 80/742); and returning unused antibiotics to the pharmacy (10%; 73/742) (Figure 4).
Figure 4.
Patient/carers’ reported knowledge about their antibiotics upon arrival at the community pharmacy.
Twenty-two percent (201/931) of patients/carers provided contact details for someone from PHE to follow them up to ask some further questions about their pharmacy visit. Of these, 34% (68/201) responded to the e-mail/text message and completed Questionnaire A (Appendix S4): 48% (30/62; six did not complete these questions) of respondents now intended to return unused antibiotics to the pharmacy; 50% (31/62) reported that they already did this. Seventy-eight percent (53/68) of patients/carers agreed to be followed up for Questionnaire B; 45% of these (24/53) completed Questionnaire B (Appendix S5). All (n = 24) patients/carers reported that they had followed advice and had taken the antibiotics at regular intervals, as their doctor/nurse/pharmacist advised. At this time, no-one reported that they had shared their antibiotics with friends, family or pets.
Pharmacy staff’s feedback on the PAMSI
Thirteen pharmacy staff completed a post-intervention questionnaire: 12/13 reported that the educational webinar and supporting tools facilitated them well or very well in their AMS role (see Table 2 for example quotes).
Table 2.
Pharmacy staff post-intervention quotes regarding the aims of the intervention
| Topic of questioning | Quote from pharmacy staff |
|---|---|
| Assessing the appropriateness of the antibiotic using the Antibiotic Checklist | ‘I have slightly better understanding of which antibiotics are prescribed in different situations and the importance of questioning the choice of antibiotic if I have a concern.’ |
| Querying the appropriateness of the antibiotic with the prescriber | ‘The example provided gave me more confidence to query the appropriate prescribing of antibiotics with the prescribers. GPs tend to be quite resistant to any challenges but I felt more empowered to do this.’ |
| Giving adherence advice to patients/carers collecting antibiotics | ‘The pilot made me much more focused in giving advice. The questions allowed me to address the main issues where the patient lacked knowledge. The conversations I had with patient were much more effective and meaningful.’ |
| Giving self-care advice to patients/carers collecting antibiotics | ‘I feel like it has now become easier to give additional self-care advice to help prevent/ reduce recurring infections.’ |
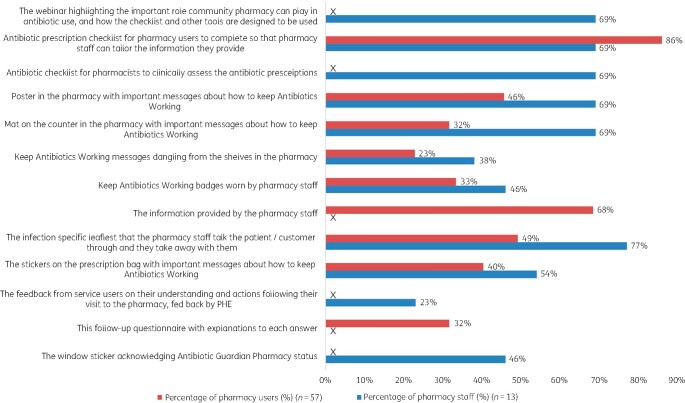
When asked which parts of the intervention were essential to support the key messages of how to keep antibiotics working, 77% of community pharmacy staff (10/13) indicated the infection-specific patient information leaflets; the figure was 69% (9/13) each for the webinar, Antibiotic Checklist, poster and counter mat. Pharmacy users indicated the Antibiotic Checklist (86%; 49/57) and information provided by the pharmacy staff (68%; 39/57) were essential; less than half indicated the other components were essential (Figure 5).
Figure 5.
Pharmacy staff and users’ views about which part of the intervention are essential to support the key messages about how to keep antibiotics working.
Discussion
When trialled in pharmacies in February 2019, the Antibiotic Checklist was feasible to implement as it fitted into operational practice. The educational webinar increased community pharmacy staff’s understanding, confidence, commitment and intention to use the tools provided to give advice to patients/carers collecting antibiotics. The Antibiotic Checklist allowed staff to address the main issues where the patient lacked knowledge, resulting in much more effective and meaningful conversations. Pharmacy users agreed that the information provided by the pharmacy staff was essential, and this was facilitated by both the Antibiotic Checklist and infection-specific information leaflets.
The Antibiotic Checklist highlighted that patient advice was most needed about: likely duration of symptoms; when their antibiotic should be taken relative to food; side effects of antibiotics; whether they should avoid alcohol whilst taking their antibiotic; and that they should return unused antibiotics to the pharmacy.
These findings are promising in supporting and improving current AMS practice in community pharmacies. This is encouraging as community pharmacy staff are likely to play a greater role in minor illnesses, as part of a scheme to release NHS resources (especially in relation to GP consultations) by preventing (or minimizing) patient use of alternative and more costly branches of the NHS.20 The NHS Community Pharmacist Consultation Service (CPCS), launched by NHS England and Improvement is a scheme whereby patients can be referred to a convenient pharmacy either following an initial assessment by an NHS 111 call handler21 or by their GP surgery.22 The CPCS provides advice and treatment for a range of minor illnesses or an urgent supply of a previously prescribed medicine. The service is designed to alleviate pressure on GP appointments and emergency departments, in addition to harnessing the skills and medicines knowledge of pharmacists.
Support for community pharmacies’ AMS involvement is apparent in the literature, as pharmacists are respected by the medical community and the public and are therefore listened to when they take a vocal position on issues involving medications.6,23 This includes providing adherence, self-care and safety netting advice, whilst also checking appropriateness of the antibiotic against local guidelines.
Comparison with other AMS interventions
A Cochrane overview of systematic reviews of interventions to improve safe and effective medicines use by consumers found that interventions involving pharmacists had positive effects on adherence and use, medicines problems and clinical outcomes.24
The same review found several other prescriber-facing strategies that showed some positive effects, particularly relating to adherence, including: (i) delayed antibiotic prescriptions; (ii) practical strategies like reminders, cues and/or organizers, reminder packaging and material incentives; (iii) education delivered with self-management skills training, counselling, support, training or enhanced follow-up; information and counselling delivered together; or education/information as part of pharmacist-delivered packages of care; and (iv) financial incentives.
The PAMSI incorporated education of both the community pharmacy staff and the pharmacy user. Additionally, the Antibiotic Checklist acted as a reminder of the key antibiotic checks during dispensing and a cue to tailor advice to the patient/carer. Delayed antibiotic prescriptions are not currently used in pharmacy settings. Pharmacy financial incentives were not incorporated into the design of this intervention but could be explored in the future.
A Spanish study found that patients’ antibiotic adherence behaviour was improved when verbal education was provided in the pharmacy, compared with the control group;25 this supports the approach of incorporating adherence advice in the PAMSI.
Other studies have also shown that knowledge of the proper use of antibiotics can be improved during patient consultations when physical educational materials are incorporated compared with verbal advice alone.6,26 The optimal method to increase patients’ knowledge is by combining face-to-face education with provision of a pictorial educational leaflet.27 This evidence supports the design of the PAMSI, which incorporated both verbal and written materials to improve knowledge and behaviour. Moreover, a Canadian study found that patient telephone follow-up by community pharmacists, during their antibiotic course, was simple and quick and created opportunities to intervene with patients.28 This could be a future intervention feature to explore.
Strengths and limitations
A major strength of this study is the broad range of stakeholder engagement throughout the design and evaluation of the intervention. The input from individuals with different areas of expertise and experiences was a real benefit as it gave a range of perspectives. This was crucial in order to effectively communicate information about AMR, which also benefitted by having information-design specialists involved in the whole process.29,30 Furthermore, buy-in from the pharmacy staff meant that they had ownership over the intervention, through their involvement in the development. This also meant that the PAMSI was fit for purpose in everyday practice. For example, staff often work across different pharmacies or other venues; therefore educational methods should be varied and tailored to the needs of individual staff.29 This supports the online webinar in this intervention, which could be accessed remotely at a time to suit participants.
A previous weakness of AMS interventions, as highlighted by the All-Party Parliamentary Group for Dentistry and Oral Health,31 has been that community pharmacy staff did not have information on the conditions for which prescriptions are issued, meaning that they could not check dosages, challenge decisions appropriately or educate patients on how to prevent recurrence of the infections. A strength of the PAMSI is that it overcomes this, as the Antibiotic Checklist directly asks about the type of infection.
The Antibiotic Checklist was developed in paper form to follow the antibiotic prescription’s journey. This was appropriate at the time of intervention development, but due to COVID-19, working practices have changed to reduce transmission of COVID-19. The concept of the Antibiotic Checklist is still appropriate, but implementation in practice should be explored further to support COVID-19 infection-prevention measures. During development, pharmacy staff reported that a digital format was probably not feasible, but this may now be much more widely acceptable; the study group are exploring this.
Although 931 pharmacy users completed the Antibiotic Checklist, providing robust data for these questions, only 12 community pharmacies in one locality piloted the intervention, of which 43 pharmacy staff evaluated the educational webinar and 13 gave feedback post intervention; therefore, results are not necessarily representative of other locations in England. Furthermore, there was a drop-off in responses from pharmacy users, with 68 responses to Questionnaire A, which reduced to 24 for Questionnaire B. Drop-off is expected, but it is recommended to scale up the evaluation in more pharmacies to provide more robust evidence to inform future implementation. In a feedback workshop with all involved in the intervention development, pharmacy staff explained that February is an especially busy time for community pharmacy staff due to deadlines to submit data for national quality schemes, which may explain the low recruitment rate; although the research team considered this response rate normal for unfunded research activity. This should be taken into consideration for any further research in community pharmacies. It was also suggested that, to be implemented nationally, the PAMSI should be recommended from a national perspective and rolled out through local pharmaceutical committees.
As 931 pharmacy users completed the Antibiotic Checklist, these data could be used to inform future intervention development for the public, focusing on areas that they reportedly lacked knowledge on.
A further strength is the design of the evaluation, as it not only focused on the primary outcome of changing behaviour of pharmacy staff, but also assessed change in knowledge and reported behaviour of pharmacy users. Other interventions have assessed adherence in terms of completing the course,25 but our PAMSI also explored other outcomes such as reported return of unused antibiotics to the pharmacy.
Conclusions/recommendations
As a result of feedback, the educational webinar has been modified into an interactive e-learning session, hosted on e-Learning for Healthcare (e-LfH).32 It is recommended that implementation of the Antibiotic Checklist is revisited with community pharmacy staff, to support appropriate COVID-19 infection prevention measures. Following this, the PAMSI should be evaluated to explore implementation on a wider scale in several areas of the UK, with a range of pharmacy staff and users.
This PAMSI—an Antibiotic Checklist combined with an educational webinar, infection-specific patient information leaflets and access to local antimicrobial prescribing guidelines—could be a very useful intervention to increase community pharmacy staff’s capability, opportunity and motivation to check antibiotic appropriateness and provide self-care and adherence advice when dispensing antibiotics. It should be a valuable addition to the national TARGET antibiotic resources.13 Re-establishing AMS programmes is especially pertinent during the ongoing COVID-19 pandemic, as AMR could be amplified due to increased rates of antimicrobial prescribing and breakdowns in existing AMS programmes.33
As part of the NHS CPCS, launched by NHS England and Improvement,22 PAMSI could be used to support and improve AMS practice in community pharmacy, such as the following.
Taking a patient’s history (using page 1 of the Antibiotic Checklist).
Assessing the antibiotic prescription against NICE/local guidance (facilitated by the information collected on page 1 of the Antibiotic Checklist).
Giving adherence advice to patients/carers collecting antibiotics (facilitated by the Antibiotic Checklist).
Supporting patients to self-care (facilitated by a patient information leaflet).
Giving safety netting advice (facilitated by a patient information leaflet).
Offering the annual influenza vaccine (facilitated by the vaccination question on the Antibiotic Checklist).
Using opportunities in the patient pathway to make further use of clinical scoring tools for self-limiting infections, e.g. clinical assessment tools such as FEVERPAIN for acute sore throat (facilitated by the educational webinar).
Supporting pharmacy staff when they dispense antibiotics under a patient group directive (PGD) and/or give advice after patient referral from the GP surgery or NHS 111.
Supplementary Material
Acknowledgements
We wish to thank the Pharmacy Antibiotic Prescription Checklist (PAPC) Group, Gloucestershire Local Pharmaceutical Group, Gloucestershire Clinical Commissioning Group and all of the community pharmacy teams in Gloucestershire and patient representatives that contributed to the development of the tools and/or were involved in the pilot. We also wish to thank Julie Brooke from PHE, for inputting the data from all 931 Antibiotic Checklists.
Funding
This project was supported by an HEE innovation fund.
Transparency declarations
R.A., D.A.-O., L.F.J. and C.A.M.M. are all employed by PHE and work in the HCAI&AMR division. P.H. is president of BSAC. T.T. is an employee of Boots UK but does not hold any stock or options in Boots UK. All other authors: none to declare.
Supplementary data
Appendices S1 to S6 are available as Supplementary data at JAC-AMR Online.
Contributor Information
Sarah Chapman, The Letter g, Harpenden, UK.
Philip Howard, University of Leeds, Leeds, UK.
Tracey Thornley, University of Nottingham, Nottingham, UK; Boots UK, Nottingham, UK.
Diane Ashiru-Oredope, Public Health England, Gloucester, UK.
Sue Walker, The University of Reading, Reading, UK.
Leah F Jones, Public Health England, Gloucester, UK.
Cliodna A M McNulty, Public Health England, Gloucester, UK.
References
- 1. Thomas F, Depledge M. Medicine ‘misuse’: implications for health and environmental sustainability. Soc Sci Med 2015; 143: 81–7. [DOI] [PubMed] [Google Scholar]
- 2. Department of Health and Social Care. UK 20-Year Vision for Antimicrobial Resistance. https://www.gov.uk/government/publications/uk-20-year-vision-for-antimicrobial-resistance.
- 3. Department of Health and Social Care. UK 5-Year Action Plan for Antimicrobial Resistance 2019 to 2024. https://www.gov.uk/government/publications/uk-5-year-action-plan-for-antimicrobial-resistance-2019-to-2024.
- 4. PHE. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report: 2018–2019. https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report.
- 5. Pharmaceutical Services Negotiating Committee. About Community Pharmacy. https://psnc.org.uk/psncs-work/about-community-pharmacy/.
- 6. Bishop C, Yacoob Z, Knobloch MJ et al. Community pharmacy interventions to improve antibiotic stewardship and implications for pharmacy education: a narrative overview. Res Soc Adm Pharm 2019; 15: 627–31. [DOI] [PubMed] [Google Scholar]
- 7. Jones LF, Owens R, Sallis A et al. Qualitative study using interviews and focus groups to explore the current and potential for antimicrobial stewardship in community pharmacy informed by the Theoretical Domains Framework. BMJ Open 2018; 8: e025101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ECDC. Proposals for EU Guidelines on the Prudent Use of Antimicrobials in Humans. https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Publications/EU-guidelines-prudent-use-antimicrobials.pdf.
- 9. Department of Health and Social Care, NHS England and NHS Improvement, Pharmaceutical Services Negotiating Committee (PSNC). The Community Pharmacy Contractual Framework for 2019/20 to 2023/24: Supporting Delivery for the NHS Long Term Plan. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/819601/cpcf-2019-to-2024.pdf.
- 10. Blanchette L, Gauthier T, Heil E et al. The essential role of pharmacists in antibiotic stewardship in outpatient care: an official position statement of the Society of Infectious Diseases Pharmacists. J Am Pharm Assoc (2003) 2018; 58: 481–4. [DOI] [PubMed] [Google Scholar]
- 11. PHE. Keep Antibiotics Working. https://campaignresources.phe.gov.uk/resources/campaigns/58-keep-antibiotics-working/Overview.
- 12. PHE. Antibiotic Guardian. https://antibioticguardian.com/.
- 13. PHE. TARGET Antibiotics Toolkit. https://www.rcgp.org.uk/clinical-and-research/resources/toolkits/amr/target-antibiotics-toolkit.aspx. [DOI] [PMC free article] [PubMed]
- 14. Royal Pharmaceutical Society. Appendix 2: Antimicrobial Stewardship—Checklist for Community Pharmacy. https://www.rpharms.com/resources/quick-reference-guides/antimicrobial-stewardship-ams-qrg#APP2.
- 15. Walker S, Hignett S, Lim R et al. Explaining drug-resistant infection in community pharmacies through effective information design. Design Health 2020; 4: 82–104. [Google Scholar]
- 16. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011; 6: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jackson C, Eliasson L, Barber N et al. Applying COM-B to medication adherence: a suggested framework for research and interventions. Eur Health Psychol 2014; 16: 7–17. [Google Scholar]
- 18. Pinnacle Health Partnership LLP. PharmOutcomes. https://pharmoutcomes.org/pharmoutcomes/.
- 19. Carroll C, Patterson M, Wood S et al. A conceptual framework for implementation fidelity. Implement Sci 2007; 2: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Baqir W, Learoyd T, Sim A et al. Cost analysis of a community pharmacy ‘minor ailment scheme’ across three primary care trusts in the North East of England. J Public Health 2011; 33: 551–5. [DOI] [PubMed] [Google Scholar]
- 21. Nazar H, Evans C, Kyei N et al. A service evaluation and stakeholder perspectives of an innovative digital minor illness referral service from NHS 111 to community pharmacy. PLoS One 2020; 15: e0230343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Primary Care Strategy and NHS Contracts Team. Advanced Service Specification—NHS Community Pharmacist Consultation Service. https://www.england.nhs.uk/publication/advanced-service-specification-nhs-community-pharmacist-consultation-service/.
- 23. McNulty CA, Collin SM, Cooper E et al. Public understanding and use of antibiotics in England: findings from a household survey in 2017. BMJ Open 2019; 9: e030845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ryan R, Santesso N, Lowe D et al. Interventions to improve safe and effective medicines use by consumers: an overview of systematic reviews. Cochrane Database Syst Rev 2014; issue 4: CD007768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Muñoz EB, Dorado MF, Guerrero JE et al. The effect of an educational intervention to improve patient antibiotic adherence during dispensing in a community pharmacy. Aten Primaria 2014; 46: 367–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Angoulvant F, Rouault A, Prot-Labarthe S et al. Randomized controlled trial of parent therapeutic education on antibiotics to improve parent satisfaction and attitudes in a pediatric emergency department. PLoS One 2013; 8: e75590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hu H, Wu FL, Hu FC et al. Effectiveness of education programs about oral antibiotic suspensions in pediatric outpatient services. Pediatr Neonatol 2013; 54: 34–42. [DOI] [PubMed] [Google Scholar]
- 28. Beaucage K, Lachance-Demers H, Ngo TT et al. Telephone follow-up of patients receiving antibiotic prescriptions from community pharmacies. Am J Health Syst Pharm 2006; 63: 557–63. [DOI] [PubMed] [Google Scholar]
- 29. Walker S. Effective antimicrobial resistance communication: the role of information design. Palgrave Commun 2019; 5: 24. [Google Scholar]
- 30. Walker S. The contribution of typography and information design to health communication. In: Cooper R, Tsekleves E, eds. Design for Health. Routledge, 2017: 92–109. [Google Scholar]
- 31. All-Party Parliamentary Group for Dentistry and Oral Health. Tackling Antimicrobial Resistance in the Primary Care Setting. http://appg-on-antibiotics.com/assets/Primary-Care-JointReport-FINAL-1.pdf.
- 32. Antimicrobial Stewardship for Community Pharmacy Staff e-learning. https://www.e-lfh.org.uk/programmes/antimicrobial-resistance-and-infections/.
- 33. Rawson TM, Moore LSP, Castro-Sanchez E et al. COVID-19 and the potential long-term impact on antimicrobial resistance. J Antimicrob Chemother 2020; 75: 1681–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.