Graphical Abstract
Graphical Abstract.
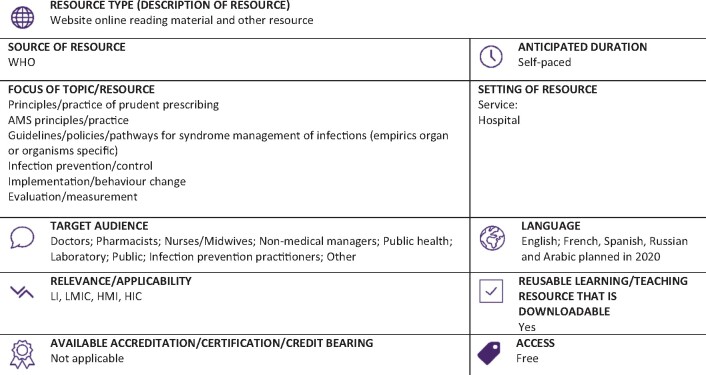
LI, low-income countries; LMIC, low- and middle-income countries; HMI, high- and middle-income countries; HIC, high-income countries.
Resource web link: https://apps.who.int/iris/bitstream/handle/10665/329404/9789241515481-eng.pdf (Full classification scheme available at: http://bsac.org.uk/wp-content/uploads/2019/03/Educational-resource-review-classification-scheme.pdf)
WHO region and country (World Bank): European Region, Switzerland (HIC)
Peer review commentary
This is an outstanding antimicrobial stewardship (AMS) toolkit for implementation in hospitals primarily in LMICs. Whilst developed by WHO in Geneva, the development and testing of the toolkit has had input from relevant experienced stakeholders and clinicians working in LMICs and elsewhere. The emphasis of the toolkit is on ‘doing and measuring’ AMS. There is a very elegant blend of theoretical narrative and pragmatic examples, solutions, case studies and other resources to help the practiotioner who may wish to simply start a very basic programme, to someone who requires information and support to do more complex or advanced interventions. The toolkit is relevant to the context of the setting, and planned translations into other languages will make its adoption easier.
Navigating the toolkit is eased by good structure and there is a sensible and intuitive stepwise approach to the AMS programme—structures required at state/regional and hospital/health facility level, planning, performing including concepts of improvement and behaviour change, assessing (measurement) and delivering training. The recognition of the importance of e-learning resources to augment face-to-face learning and signposting to such available resources is a particular strength of the tooklit as is the planned open-access tutor and trainer teaching resources (slide deck) to compliment the toolkit. The annex to the toolkit has good examples of practical things like terms of references for AMS groups/committees, exemplar AMS pre-authorization and post-prescription review forms as well as a sample bug–drug chart. The incorporation of the importance of point prevalence studies or surveys (PPS) in AMS provides practical support to the recent publication of the WHO PPS methology. Similarly, the summary of the competency framework within the toolkits is valuable for health facilities and aligned to the WHO healthcare professional competency framework and recently published curricula guide.
There are many resources out there to support AMS hospital implementation and they are all welcome. This resource standsout in my view in that it brings together all the relevant material/resources that are applicable to the LMIC setting, is aligned and consistent with other WHO and other geographic and context-relevant resources and most importantly is presented in a very practical way that is useful to the busy practitioner. Like all such resources the importance of keeping it updated and relevant will remain a challenge to the authors and WHO. Otherwise, happy AMS implementation!