Abstract
Only 5% of all urological tumors are accounted as Testicular tumors. Furthermore, a well differentiated chondrosarcoma of the testis is extremely rare. Thus, we are representing a rare case of testicular chondrosarcoma. A 43-year-old male with right scrotal swelling did Doppler Ultrasonography demonstrating a large heterogenous hypervascular mass. Patient has had uneventful radical inguinal orchiectomy. The histopathology of the resected tumor reveled 50% seminoma – 50% teratoma with somatic type malignancy (well differentiated chondrosarcoma). Only few cases were reported in the medical literature for testicular chondrosarcoma. Thus, reporting such cases will add to the literature and shall help in establishing a management strategy.
Keywords: Testicular chondrosarcoma, testicular tumor, urological tumor
INTRODUCTION
Testicular tumors are uncommon tumors accounting for only 5% of all urological tumors.[1] However, the incidence of testicular tumors in young males has been increased in the last decade. In 2018, the American Cancer Society revealed that around 9000 new cases and 400 deaths from testicular cancer were expected.[2] There are two main types of testicular tumors including germ cell and nongerm cell tumors. Germ cell tumors can be further classified based on histologic type into seminoma and nonseminoma. Teratomas are consider nonseminoma germ cell tumors, and they account for only 4% of all testicular tumors.[3] Benign chondroid differentiation of teratoma is common; however, a well-differentiated chondrosarcoma of the testis is extremely rare.[4] Thus, we represent a rare case of testicular chondrosarcoma.
CASE REPORT
A 43-year-old male presented to the hospital with a history of right scrotal swelling associated with mild testicular discomfort for 4 months before the presentation. There was no history of trauma, lower urinary tract symptoms, or urinary tract infection. He denied any history of weight loss, fever, or anorexia. Physical examination revealed a healthy man with a hard swelling localized to the right hemiscrotum. His laboratories were within normal range including tumor markers (alpha-fetoprotein, lactate dehydrogenase and human chorionic gonadotropin). Scrotal Doppler ultrasound scan [Figure 1] demonstrated a large heterogeneous hypervascular mass almost replacing the right testicle, with multiple internal calcifications and cystic changes. The patient underwent uneventful radical inguinal orchiectomy. The histopathology of the resected tumor revealed a mixed germ cell tumor: 50% seminoma – 50% teratoma with somatic-type malignancy (well-differentiated chondrosarcoma).
Figure 1.

Large heterogeneous hypervascular mass occupying almost all the right testicle measuring about 4.3 cm × 3.5 cm × 3.0 cm with multiple internal calcifications and cystic changes
Pathology description
Received is a testis showing a 4.5 cm × 3.5 cm × 2.0 cm white-tan, lobulated tumor mass with cartilaginous component, occupying the entire testis. Microscopic study of hematoxylin and eosin section of the tumor showed two main components: seminoma (50%) and teratoma (50%) [Picture 1]; the teratoma component has mainly mature cartilage; the cells within cartilage showed increase cellularity with moderate cytological atypia, frequent mitosis, and multinucleation; all are features consistent with well-differentiated chondrosarcoma [Picture 2].
Picture 1.
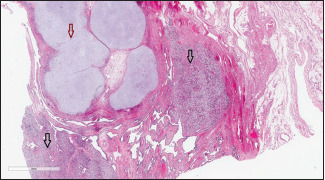
Low power image (H and E, ×4) showing seminoma (black arrow) and cartilaginous component (red arrow)
Picture 2.
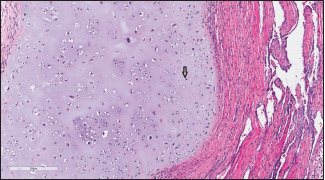
Higher view of the cartilage tissue showing increase cellularity, atypia, and mitosis (black arrow) (H and E, ×20)
DISCUSSION
Testicular teratoma is a nonseminoma germ cell tumor. It is considered a rare malignant tumor which has the potential to metastasize.[5] Although chondroid differentiation of testicular teratoma is common, accounting for 75% of benign teratomas and 54% of malignant teratomas, a primary testicular chondrosarcoma is extremely rare.[4] Only few cases were reported in the medical literature for testicular chondrosarcoma. In 1993, Füzesi et al. reported the first case of a differentiated testicular chondrosarcoma with a metastatic spread into the retroperitoneal space, which they had drawn a particular attention to the cytogenic analysis of such tumor.[6] The case was approached by removing the affected testis followed by adjuvant chemotherapy and retroperitoneal lymph node dissection (RPLND). The second case was reported by Yalçinkaya for a patient with testicular chondrosarcoma with no metastasis who was managed by radical orchiectomy. In both formerly reported cases, a remission of 24 months was achieved. Owing to rarity of such cases, well-established treatment guidelines are lacking. Treatment approaches are varying and best to be tailored for each case. Thus, our case was discussed in tumor board, and neither adjuvant chemotherapy nor RPLND was offered due to lack of evidence for either treatment. The patient was followed closely for 6 months postoperatively with no sign of relapse. In conclusion, reporting such cases will add to the literature and shall help in establishing a management strategy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rosen A, Jayram G, Drazer M, Eggener SE. Global trends in testicular cancer incidence and mortality. Eur Urol. 2011;60:374–9. doi: 10.1016/j.eururo.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 3.von Hochstetter AR, Hedinger CE. The differential diagnosis of testicular germ cell tumors in theory and practice. A critical analysis of two major systems of classifiction and review of 389 cases. Virchows Arch A Pathol Anat Histol. 1982;396:247–77. doi: 10.1007/BF00431386. [DOI] [PubMed] [Google Scholar]
- 4.Collins DH, Pugh RC. Pathology of the Testis. Oxford: Blackwell Scientific; 1976. pp. 195–244. [Google Scholar]
- 5.Avances C, Camparo P, Durand X, Flechon A, Murez T, Sebe P, et al. Management of testicular teratoma: Update by the Oncology Committee of the French Urology Association, section of External Genital Organs (CCAFU-OGE) Prog Urol. 2014;24:1050–3. doi: 10.1016/j.purol.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Füzesi L, Rixen H, Kirschner-Hermanns R. Cytogenetic findings in a metastasizing primary testicular chondrosarcoma. Am J Surg Pathol. 1993;17:738–42. doi: 10.1097/00000478-199307000-00012. [DOI] [PubMed] [Google Scholar]


