Abstract
Genitourinary tract arteriovenous malformations are extremely rare. Most of the lesions are found either in the kidney or urinary bladder. So far, to the best of our knowledge, only five cases of arteriovenous malformation of the ureter have been reported in the literature. Here, we present, a young male, clinically presented with pain in the left flank with no other significant history. On radiological evaluation found to have left hydroureteronephrosis with stricture of the left distal ureter at the level of iliac vessel crossing. Urine routine, cytology, and cystoscopy were unremarkable. Left retrograde pyelogram showed distal ureteric stricture. Patient underwent excision of left distal ureteric stricture segment and ureteric reimplantation with psoas hitch. Histopathological examination revealed the features of arteriovenous malformation of the left ureter. The patient is asymptomatic and has no recurrence on follow-up until 12 weeks after surgery.
Keywords: Arteriovenous malformation, hematuria, ureteric reimplantation, ureteric stricture
INTRODUCTION
Arteriovenous malformations in the genitourinary tract are very uncommon. The direct communication between arterioles and venules can either be congenital or acquired. In 1928, Varela reported the first case of arteriovenous malformations of the urinary tract.[1] Most of the reported lesions are either in the kidney or in the urinary bladder. Arteriovenous malformations of the ureter are extremely rare and to date, to our knowledge, there have been only five cases reported in the literature, all of which presented with hematuria. The first one was reported by Kaplan et al. in 1992[2] in a young female patient who presented with intermittent gross hematuria. We present the sixth case of arteriovenous malformation of the ureter in a male patient with no hematuria.
CASE REPORT
A 34-year-old male presented with a 2-year history of intermittent left flank pain. There was no hematuria, urolithiasis, dysuria, or pyuria. Physical examination was within the normal limits. Ultrasonogram of the kidney, ureter, and bladder (KUB) region revealed left hydroureteronephrosis and urine analysis showed no hematuria/leukocytes/granular cast/bacteria. Urine tuberculosis-polymerase chain reaction was negative. Computed tomogram of the KUB region showed prompt excretion of contrast by both the kidneys, and it also demonstrated left moderate hydroureteronephrosis with narrowing/stricture at left distal ureter – probable due to an extrinsic compression [Figure 1]. DiethyleneTriamine Penta Acetic acid (DTPA) renogram showed enlarged left kidney with 34% relative uptake with obstruction at the level of the lower ureter [Figure 2a and b]. The patient underwent cystoscopy which was normal and left retrograde pyelography which showed tortuous dilated left ureter, left hydroureteronephrosis, and left distal ureteral stricture [Figure 3]. Urine cytology was unremarkable.
Figure 1.

Computed tomography urogram showing dilated and tortuous left ureter with distal narrowing/stricture
Figure 2.
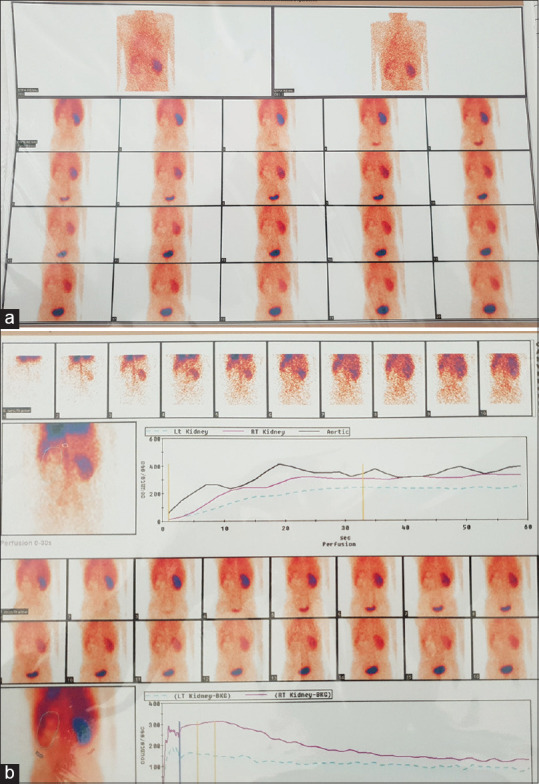
(a and b) DTPA urogram
Figure 3.

Retrograde pyelography of the left ureter showing distal ureteric narrowing
The patient underwent open excision of the stenosed part of the left lower ureter followed by ureteric reimplantation with Psoas hitch. Histopathological examination of the specimen showed ulceration of mucosa, edematous lamina propria containing ectatic blood vessels containing red blood cells along with moderate infiltration by neutrophils and lymphocytes. The muscular layer and adventitia contain variable-sized dilated irregular blood vessels (capillaries, arteries, and venules) with a few vessels showing variable thickness of tunica media. These findings were consistent with the diagnosis of arteriovenous malformation with acute on chronic ureteritis [Figure 4a and b]. The patient had an uneventful postoperative recovery. On regular follow-up at 3, 7, and 12 weeks, he is asymptomatic, and there is no evidence of recurrence.
Figure 4.
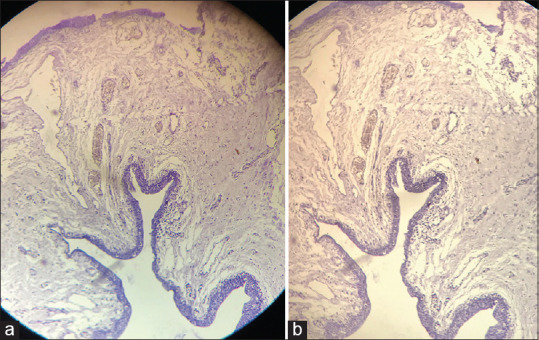
(a and b) Hematoxylin and eosin staining of the excised ureteric specimen
DISCUSSION
Arteriovenous malformations of the ureter are extremely uncommon. To the best of our knowledge, so far, there are only five cases have been reported in the English literature. Kaplan et al., in 1992, reported the first case, a 34-year-old woman, with gross hematuria often accompanied by mild left flank pain. Urine cytology showed malignant cells, further evaluation showed only benign cells of nontransitional origin. Ureteroscopy on the left side showed a polyp in the mid-ureter. An excision biopsy of which revealed superficially located numerous large and small blood vessels with irregular and asymmetry in the walls confirming the diagnosis of arteriovenous malformation. The second case was reported by Tang et al. in 1997,[3] a 19-year-old female with gross hematuria with intermittent episodes of right loin discomfort. Retrograde pyelography demonstrated a tubular filling defect in the right distal ureter. Ureteroscopy revealed “cobblestone” mucosa in the lower ureter with ulcerations. Suspecting vascular malformation right renal arteriography was performed selectively which revealed tortuous vessels around the right ureter which was selectively embolized. Sech et al.[4] reported the third case, a 29-year-old woman, with gross intermittent hematuria and right lower abdominal pain. Right retrograde pyelography showed a filling defect which on ureteroscopy was a polyp. Histopathological examination of the excision biopsy specimen revealed similar findings as the first case. The fourth case was reported by Ten Donkelaar et al.[5] in 2017, a 41-year-old female who was incidentally noted to hematuria during in-vitro fertilization. Urine cytology revealed atypical transitional cells. Retrograde pyelography of the left ureter showed a filling defect at L4–L5. Ureteroscopy showed a 3 cm polypoidal lesion which was excised and histopathological examination confirmed arteriovenous malformation of the ureter. The fifth case, a 60-year-old female with microscopic hematuria of unclear etiology which was diagnosed on computed tomography urogram was reported by Calabrese et al., in 2018.[6] We report the first case of arteriovenous malformation of the ureter in a male. Another peculiarity is that the patient had the features of obstruction alone, and there was no evidence of hematuria as seen in all the above-mentioned cases. For arteriovenous malformations excision is preferred, many advise laser excision as it reduces the risk of hemorrhage. Selective embolization is an alternative option. We performed excision biopsy, as the patient had distal ureteric stricture causing an obstruction.
CONCLUSION
To conclude, arteriovenous malformation of the ureter is a rare phenomenon that usually presents with hematuria as a significant symptom. However, patients can present with symptoms of obstruction with no evidence of hematuria. Hence, a high index of suspicion is necessary to diagnose this uncommon entity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr Gaurvi Piplani, Junior Resident and Dr Teerthanath S, Professor, Department of Pathology, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
REFERENCES
- 1.Varela ME. Aneurisma arteriovenosa de los vasos renales yasistolia consecutiva. Rev Med Latino-Amer. 1928;14:3244. [Google Scholar]
- 2.Kaplan SA, Brown W, Bixon R, O’Toole K, Benson MC. Arteriovenous malformation of the ureter. Urology. 1992;40:450. doi: 10.1016/0090-4295(92)90462-6. [DOI] [PubMed] [Google Scholar]
- 3.Tang CN, Law IC, Iu PP, Yip AW. Arteriovenous malformation of the ureter–a rare cause of haematuria. Br J Urol. 1997;80:500–1. doi: 10.1046/j.1464-410x.1997.00384.x. [DOI] [PubMed] [Google Scholar]
- 4.Sech SM, Saboorian MH, Ashfaq R, Somerville PJ, Pearle MS. Polypoid arteriovenous malformation of the ureter. J Urol. 1997;158:1903–4. doi: 10.1016/s0022-5347(01)64166-1. [DOI] [PubMed] [Google Scholar]
- 5.Ten Donkelaar CS, Houwert AC, Ten Kate FJW, Lock MTWT. Polypoid arteriovenous malformation of the ureter mimicking a fibroepithelial polyp, a case report. BMC Urol. 2017;17:55. doi: 10.1186/s12894-017-0237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calabrese E, Baghdanian AH, Zagoria RJ, Behr SC. Arteriovenous malformation of the ureter diagnosed by CT urogram. Urol Case Rep. 2018;19:20–2. doi: 10.1016/j.eucr.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


