Abstract
This is a case report of emphysematous cystitis with spontaneous intraperitoneal bladder perforation in postoperative period of pedicle fixation surgery for prolapse intervertebral disc (L3–L4). The patient developed urinary retention with overflow incontinence with abdominal tenderness and fever 3 days after orthopedic procedure which on computed tomography (CT) scan found to have abundant air in urinary bladder with multiple air foci in bladder wall with suspected leak into intraperitoneal pelvic cavity, proven only after CT cystogram.
Keywords: Bladder perforation, emphysematous cystitis, Escherichia coli
INTRODUCTION
This is a case report of emphysematous cystitis with spontaneous intraperitoneal bladder perforation in postoperative period of pedicle fixation surgery for prolapse intervertebral disc. Very few cases of emphysematous cystitis are reported; largest data were published by Thomas et al. of 135 patients. Spontaneous bladder perforation in emphysematous cystitis is even rare.
CASE REPORT
A 55-year-old female presented with difficulty in walking for 15 days; on evaluation, she was found to have prolapsed intervertebral disc at L3–L4 region. The patient did not have any other neurological deficit or bladder-bowel symptoms. The patient underwent L3–L4 pedicle screw fixation in orthopedics department. The patient was on per urethral catheter for 3 days in postoperative period. After catheter removal, the patient developed difficulty in voiding urine with decreased bladder sensation with urinary retention and overflow incontinence. She had two episodes of fever with chills with lower abdominal pain, tenderness, and mild hematuria. The patient was treated conservatively, but still patient had persistent fever with increasing lower abdominal pain and distension of abdomen. General surgery opinion was taken considering acute abdomen. Ultrasonography abdomen was inconclusive. The patient underwent contrast-enhanced computed tomography (CT) scan of abdomen and pelvis in emergency department; it was showing overdistended urinary bladder with the presence of large pocket of air in bladder with air–fluid level and multiple foci of air specks in entire bladder wall with dilated gaseous bowel loops with small collection in pelvic cavity [Figures 1 and 2]. There were no free air specks in intraperitoneal cavity. On CT cystogram, there was suspicion of small amount contrast leak into the intraperitoneal pelvic collection [Figure 3]. Urology reference was given after above findings. On examination, the patient was febrile with pulse rate of 130 and blood pressure of 110/80 mmHg. She had lower abdominal tenderness with guarding and generalized abdominal distension. Her total leukocyte count was 13,000/mm3, hemoglobin – 9.9 g/dl, and creatinine – 0.8 mg/dl with normal electrolytes and liver function test. Per urethral catheter drained approximately 1000 ml of turbid urine. She did not have any other medical comorbidities.
Figure 1.
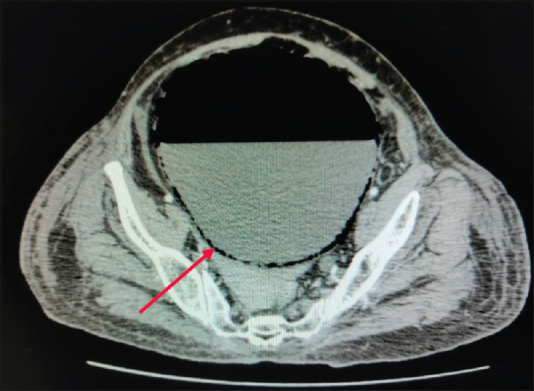
Axial computed tomography scan showing distended bladder with air–fluid level and multiple small foci of air specks in bladder wall (red arrow)
Figure 2.

Axial computed tomography scan showing multiple air foci in bladder wall with pelvic collection (red arrow)
Figure 3.
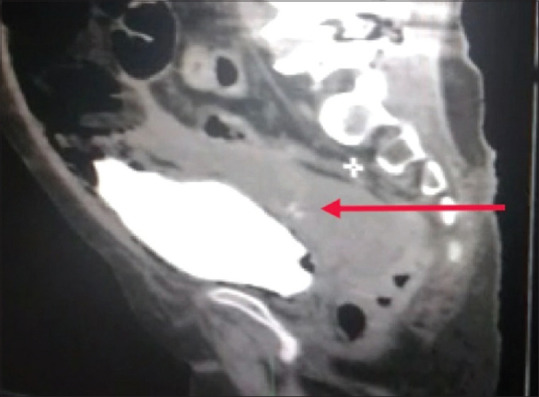
Sagittal computed tomography scan with cystogram showing thin stream of bladder contrast (red arrow) going into intraperitoneal pelvic collection
The patient was started on broad-spectrum intravenous antibiotics, fluids, and blood, and urine culture was sent, hemodyanamics were monitored, and she underwent emergency exploratory laparotomy. The peritoneal cavity had seropurulent collection in pelvic region and approximately 3–4 cm diameter irregular perforation at the junction of dome and posterior wall of bladder with necrotic sloughed edges and edematous thickened entire bladder wall with the presence of whitish pus flakes attached to mucosal surfaces [Figure 4]. Trigone and ureteric orifices were away with normal urine jets. Bowel loops were dilated but normal, and there was no any other collection intraperitoneally. Edges of bladder perforation were debrided till fresh margin, collection fluid sent for culture, and copious wash of saline was given in pelvic cavity and intravesically. Suprapubic catheter kept through separate opening, per urethral catheter kept in situ, and bladder closed in two layers with absorbable suture. Wide bore drain kept in pelvic cavity and abdomen closure was done.
Figure 4.
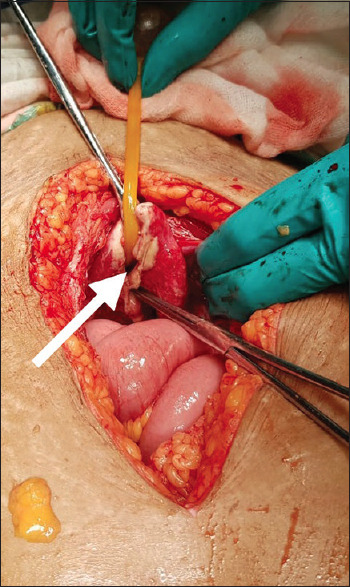
Intraoperative photograph showing bladder perforation near the dome (white arrow) with necrotic sloughed edges with thickened edematous bladder wall and Foley's catheter can be seen coming out through the rent (foot end)
Postoperative recovery was uneventful. Pelvic fluid collection culture was positive for Escherichia coli. Drain removed after 5 days and the patient discharged after 8 days with both catheter in situ and received oral antibiotics for 2 weeks. Per urethral catheter was removed after 3 weeks after doing fluoroscopic cystogram and ruling out any leak with adequate bladder capacity. Suprapubic catheter kept clamped and after confirming successful voiding trial catheter removed after 7 days. The patient also recovered satisfactorily from her initial orthopedic procedure without any neurological deficit.
DISCUSSION
Emphysematous cystitis is gas-forming infection of bladder wall most commonly caused by E. coli, other less common organisms such as Klebsiella pneumoniae, Enterobacter aerogenes, Clostridium perfringens, and Candida albicans can also cause emphysematous cystitis.[1] It can be potentially life-threatening condition which can lead to necrosis of entire bladder wall, leading to perforation, peritonitis, and septicemic shock, most commonly seen in women during the fifth or sixth decades of life.Risk factors are diabetes mellitus, immunocompromised status, neurogenic bladder, and bladder outlet obstruction with urinary retention.[1] Emphysematous cystitis is less common occurrence than its renal counterpart-emphysematous pyelonephritis.
The patient presents with vague symptoms which may be difficult to differentiate from other abdominal acute conditions. CT scan helps in diagnosis which can show air in the bladder or multiple air foci in the wall of a bladder appearing as “beaded necklace” appearance.[2] Spontaneous bladder perforation is rare[3] and may be difficult to diagnose, but CT cystography may help in such situation to rule out perforation. X-ray abdomen and ultrasonography may not be able to diagnose this condition conclusively.
In this case, there is possibility that the patient had undetected bladder problems preoperatively due to PID or developed postoperatively due to spinal shock. This could have led to distended bladder and overflow incontinence which was missed during initial periods by treating surgeons due to its subtle presentation. It was only after CT cystogram the minute leak was identified which helped to subject the patient timely intervention.
Majority of patients can be managed conservatively with bladder drainage and culture-guided course of antibiotics. Hyperbaric oxygen therapy can be used in such patients.[4] Approximately 10% of patients require surgical intervention such as partial or total cystectomy due to advance nature of disease or due to its complications. Overall mortality can reach up to 7%.[1]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Thomas AA, Lane BR, Thomas AZ, Remer EM, Campbell SC, Shoskes DA. Emphysematous cystitis: A review of 135 cases. BJU Int. 2007;100:17–20. doi: 10.1111/j.1464-410X.2007.06930.x. [DOI] [PubMed] [Google Scholar]
- 2.Hudnall MT, Jordan BJ, Horowitz J, Kielb S. A case of emphysematous cystitis and bladder rupture. Urol Case Rep. 2019;24:100860. doi: 10.1016/j.eucr.2019.100860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roels P, Decaestecker K, De Visschere P. Spontaneous bladder wall rupture due to emphysematous cystitis. J Belg Soc Radiol. 2016;100:83. doi: 10.5334/jbr-btr.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCabe JB, Mc-Ginn Merritt W, Olsson D, Wright V, Camporesi EM. Emphysematous cystitis: Rapid resolution of symptoms with hyperbaric treatment: A case report. Undersea Hyperb Med. 2004;31:281–4. [PubMed] [Google Scholar]


