Abstract
Diabetes, Hypertension, Heart Disease, and Stroke Mortality Among Black and White Adults, 1999–2018
In the United States, cardiovascular mortality rates in rural areas are markedly higher than in urban areas (1). Black adults living in rural areas may be at particular risk for poor outcomes, given a higher burden of cardiovascular risk factors and worse access to care (2). Although public health and policy initiatives have focused on reducing racial health disparities, it is unclear whether these efforts have benefited Black persons living in rural and urban areas equally. Therefore, we evaluated how mortality rates of diabetes, hypertension, heart disease, and stroke have changed for Black and White adults in rural versus urban areas and whether racial disparities have improved in these areas of the United States over the last 2 decades.
We used data from the Centers for Disease Control and Prevention Wonder Database for 1999 to 2018 (3). Cause of death (diabetes, hypertension, heart disease, stroke) was obtained from International Classification of Diseases-10th Revision codes. Information about race was obtained from the death certificate. We compared annual age-adjusted mortality rates (per 100,000 individuals) for Black and White adults 25 years of age or older, stratified by rural or urban area, by using weighted least squares. We determined whether disparities in Black versus White mortality rates for each condition changed differentially in rural areas compared with urban areas from 1999 to 2018 by using an interaction term for race, rurality, and time (modeled as a linear effect). Estimates were age adjusted to the 2000 U.S. census. Statistical analyses were performed using R software version 3.5.2 (R Foundation, Vienna, Austria). Institutional Review Board approval from Beth Israel Deaconess Medical Center (Boston, Massachusetts) was not sought for this analysis because of the use of publicly available, deidentified data, according to institutional policy.
Over the entire study period, annual age-adjusted mortality rates in rural areas were substantially higher for Black adults compared with White adults for all conditions: diabetes (average mortality rate 1999 to 2018 [SE], 76.2 [0.42] vs. 37.2 [0.07] deaths per 100,000; p < 0.001); hypertension (31.3 [0.27] vs. 10.9 [0.04]; p < 0.001); heart disease (425.0 [0.99] vs. 331.7 [0.22]; p < 0.001); and stroke (112.6 [0.51] vs. 73.9 [0.10]; p < 0.001). In urban areas, Black adults also had higher average age-adjusted mortality rates than White adults: diabetes (63.0 [0.14] vs. 30.7 [0.03]; p < 0.001); hypertension (25.3 [0.09] vs. 10.9 [0.02]; p < 0.001); heart disease (371.0 [0.34] vs. 291.8 [0.10]; p < 0.001); and stroke (89.4 [0.17] vs. 63.6 [0.05]; p < 0.001). Between 1999 and 2018, the gap in annual age-adjusted mortality rates between Black and White adults narrowed more rapidly in urban compared with rural areas for diabetes (change in the Black vs. White difference, −0.94 [0.07] vs. −0.24 [0.10] deaths per 100,000 per year; p < 0.001 for interaction between rural area and time) and hypertension (−0.30 [0.04] vs. −0.09 [0.07]; p = 0.03) (Figure 1). In contrast, the racial gap in heart disease mortality declined at a similar rate in urban and rural areas (−3.21 [0.26] vs. −3.65 [0.34]; p = 0.46), but it declined more rapidly for stroke in rural areas (−0.80 [0.10] vs. −1.35 [0.13]; p = 0.02).
FIGURE 1. Age-Adjusted Mortality Rates for Black and White Adults in Rural and Urban Areas of the United States.
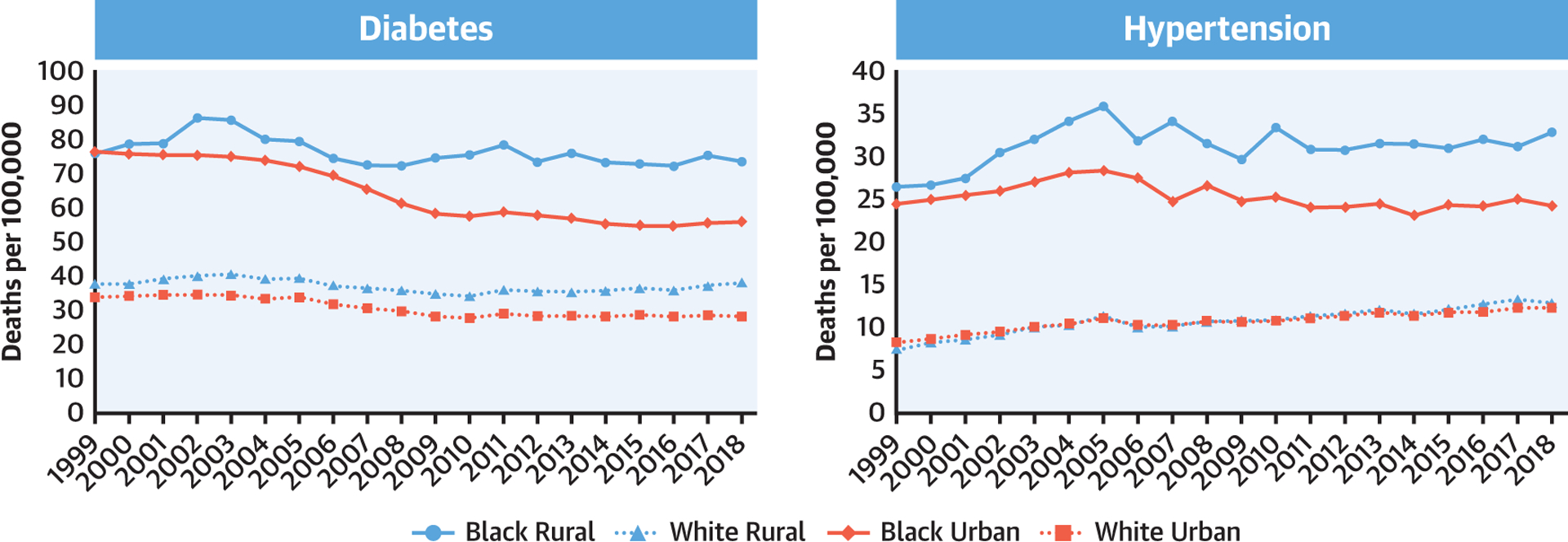
Annual mortality rates are shown for diabetes and hypertension (noncardiac causes) in both rural and urban areas. International Classification of Diseases-10th Revision codes were used to identify deaths: diabetes (E10 to E14) and hypertension (I10, I12, I15).
Over the last 2 decades, mortality rates of diabetes, hypertension, heart disease, and stroke have consistently been highest among Black adults living in rural parts of the United States. Diabetes- and hypertension-related mortality are 2 to 3 times higher for Black adults compared with White adults in rural areas. These marked racial disparities have improved minimally over the last 20 years, although more pronounced improvements have occurred in urban areas.
Although worse health outcomes in the rural United States have been attributed to higher rates of chronic disease, poverty, and fragmented health care (1), rural Black adults may be disproportionately affected by these factors. Hypertension-related deaths have increased across all populations, but this rise has been most pronounced among rural Black adults. Additionally, whereas urban Black adults have experienced a decline in diabetes-related mortality, these gains have not occurred among rural Black adults. The striking and persistent racial disparities for diabetes- and hypertension-related mortality in rural areas, relative to urban areas, may reflect structural inequities that impede access to primary, preventive, and specialist care for rural Black adults (4).
In contrast, racial disparities have narrowed for heart disease and stroke mortality in rural areas. These changes may reflect improvements in emergency services, the expansion of referral networks, the development of stroke and myocardial infarction care centers, and the implementation of time-to-procedure metrics (5).
Targeted public health initiatives are urgently needed to reduce racial inequities in cardiovascular health in rural areas of the United States.
Acknowledgments
Dr. Yeh has received research grants or served as a consultant for Abbott Vascular, AstraZeneca, Boston Scientific, and Medtronic, outside this submitted work. Dr. Wadhera receives research support from the National Heart, Lung, and Blood Institute (grant K23HL148525-1) at the National Institutes of Health; has previously served as a consultant for Regeneron, outside the submitted work. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
REFERENCES
- 1.Harrington RA, Califf RM, Balamurugan A, et al. Call to action: rural health: a presidential advisory from the American Heart Association and American Stroke Association. Circulation 2020;141:e615–44. [DOI] [PubMed] [Google Scholar]
- 2.Carnethon MR, Pu J, Howard G, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation 2017;136:e393–423. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC). CDC Wonder. 2020 2020. Atlanta, GA: CDC, 2020. Available at: https://wonder.cdc.gov/. Accessed January 26, 2021. [Google Scholar]
- 4.James CV, Moonesinghe R, Wilson-Frederick SM, Hall JE, Penman-Aguilar A, Bouye K. Racial/ethnic health disparities among rural adults — United States, 2012–2015. MMWR Surveill Summ 2017;66:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilcock AD, Zachrison KS, Schwamm LH, Uscher-Pines L, Zubizarreta JR, Mehrotra A. Trends among rural and urban Medicare beneficiaries in care delivery and outcomes for acute stroke and transient ischemic attacks, 2008–2017. JAMA Neurol 2020;77:863–71. [DOI] [PMC free article] [PubMed] [Google Scholar]


